Abstract
We examine the impact of the first wave of Medicare health maintenance organization HMO withdrawals. With data from CMS and United Health Group, we estimate use and expenditure changes between 1998 and 1999 for HMO enrollees who were involuntarily dropped from their plan and returned to fee-for-service (FFS) Medicare using a difference-in-difference model. Compared to those who voluntarily left an HMO, involuntarily disenrolled beneficiaries had higher out-of-pocket expenditures, an 80 percent decrease in physician visits, 38 percent higher emergency room (ER) use and a higher probability of dying. The results suggest beneficiaries face significant costs and reduced health outcomes from unstable Medicare managed care markets.
Introduction
On January 1, 1999, approximately 407,000 Medicare beneficiaries (nearly 7 percent of all Medicare HMO enrollees) were forced to leave their current Medicare risk-plan HMO because their health insurers chose not to enter into a new Medicare+Choice contract; or decided to reduce their current service area (Gold et al., 1999;U.S. Department of Health and Human Services, 2000; Gold and Justh, 2000; U.S. General Accounting Office, 1999). Plans have cited the payment and regulatory changes legislated by the Balanced Budget Act of 1997, combined with often intense market competition, as the reason for their withdrawal from the Medicare market (Harrison, 2002). Since 1999, Medicare managed care plan withdrawals continue to have significant consequences to Medicare beneficiaries (Booske, Lynch, and Riley, 2002). With the passage of the Medicare Prescription Drug, Improvement, and Modernization Act of 2003 (MMA), which provides new incentives to private health insurers to re-enter the market by 2006, and offer extended health care and prescription drug coverage to beneficiaries, understanding the impact of Medicare HMO withdrawals at the beneficiary level remains relevant.
Prior studies completed at the beneficiary level used survey data to gauge the impact of Medicare HMO withdrawals on cost and utilization (Booske, Lynch, and Riley, 2002; Laschober et al., 2000). While these studies have identified significant deleterious effects for beneficiaries associated with involuntary disenrollment from a Medicare HMO, such as increased out-of-pocket expenditures for prescription drugs, higher premium prices for supplemental coverage, and disruptions in their usual source of care, they have not provided an account of the utilization and expenditure impact. Also, none of these studies used a comparison group to determine whether the effects reported by disenrollees differed from underlying trends in the Medicare market.
Using 1998 and 1999 claims and enrollment data from Medicare and United Health Group (UnitedHealth), we examine the utilization and cost impact of plan changes at the beneficiary level. We report the results of an analysis comparing the utilization, out-of-pocket cost sharing, and reimbursement differences among three groups of enrollees: (1) beneficiaries involuntarily dropped from their plan and returned to FFS Medicare, (2) beneficiaries who remained enrolled in the same HMO throughout the period, and (3) beneficiaries in an UnitedHealth HMO in 1998 who voluntarily left the plan to return to FFS in 1999.
The focus of our analysis is the beneficiary level consequences of an involuntary disenrollment from a Medicare HMO from 1998 to 1999, the first period of widespread closures. This period represents a time when alternative Medicare managed care plan choices were still abundant to the beneficiary facing an HMO market withdrawal. For example, a survey of UnitedHealth Medicare seniors found that over 82 percent of those forced to leave their UnitedHealth plan in 1998 found a new managed care plan by January 1, 1999 (Schoenman et al., 2005). The implications of this research could help identify the impact of 2003 MMA failing to provide a long-term stable market-based Medicare HMO set of plan choices in 2006.
Methods
Study Setting
This study focuses on the utilization consequences of the first large-scale wave of withdrawals of HMOs from the Medicare market, which went into effect in January 1999. A unique feature of our research is the use of claims data made available by UnitedHealth as a collaborative research partner. Effective January 1999, UnitedHealth ended HMO coverage for 59,017 Medicare beneficiaries in 15 markets nationwide. Of these markets, UnitedHealth had claims and enrollment data for 9 markets comprised of 31,189 beneficiaries. Table 1 lists UnitedHealth's 1998 operational markets corresponding to 92 counties for which we have enrollment.1 In the table, the 49 counties correspond to the markets dropped by UnitedHealth are identified. All beneficiaries enrolled in these plans were forced to make a decision to choose another HMO offered in their county of residence or return to the Medicare FFS. What makes this an interesting experiment is that we are able to observe the utilization and expenditures of the dropped population if they returned to FFS. However, there is one cohort of significance with missing data—the dropped population that chose another HMO in 1999. For these beneficiaries, we used two other survey instruments to record their general experiences. We present these findings in a separate analysis (Schoenman et al., 2005).
Table 1. UnitedHealth Group Medicare+Choice Markets in Operation 1998 and their Status in 1999.
| Markets | Counties Served | Complete Withdrawal | Partial Withdrawal |
|---|---|---|---|
| Remaining in 1999 | |||
| Tampa, FL | 7 | No | Yes |
| St. Louis, MO | 9 | No | No |
| Pensacola, FL | 2 | No | No |
| Omaha, NE | 2 | No | No |
| New York | 4 | No | Yes |
| Dayton, OH | 2 | No | No |
| Columbus, OH | 2 | No | Yes |
| Cleveland, OH | 3 | No | Yes |
| Cincinnati, OH | 2 | No | No |
| Boston, MA | 4 | No | No |
| Atlanta, GA | 6 | No | Yes |
| Total | 43 | — | — |
| Withdrawn in 1999 | |||
| Tampa, FL | 2 | No | Yes |
| Orlando, FL | 5 | Yes | No |
| New York | 6 | No | Yes |
| New Jersey | 7 | Yes | No |
| Dallas, TX | 8 | Yes | No |
| Columbus, OH | 2 | No | Yes |
| Colorado, CO | 8 | Yes | No |
| Cleveland, OH | 3 | No | Yes |
| Atlanta, GA | 8 | No | Yes |
| Total | 49 | — | — |
SOURCE: Robert Wood Johnson Foundation: Data from the 1999 Medicare Health Maintenance Organization Closure Study.
Data
Enrollment and claims data used in this analysis were from 1998 and 1999. This pre/post-closure analysis was completed with the use of de-identified claims and enrollment data from CMS and UnitedHealth. CMS provided demographic, eligibility, and enrollment data for beneficiaries in our study group. All dropped HMO beneficiaries residing in markets UnitedHealth chose to exit in 1999 had the option of enrolling in another HMO, the majority (82 percent) did (Schoenman et al., 2005). UnitedHealth did not make the decision of which markets to withdraw from at random. Although, many of the markets designated for exit by UnitedHealth were less than 3-5 years old; the usual startup period were managed care organizations, and the providers build sufficient claims experience to develop predictable expenditure patterns. While UnitedHealths' choice to exit certain markets was made with some lead time, the beneficiary was unaware of UnitedHealth strategic decisionmaking and experienced an exogenous shock to either return to FFS or find another Medicare HMO in their county.
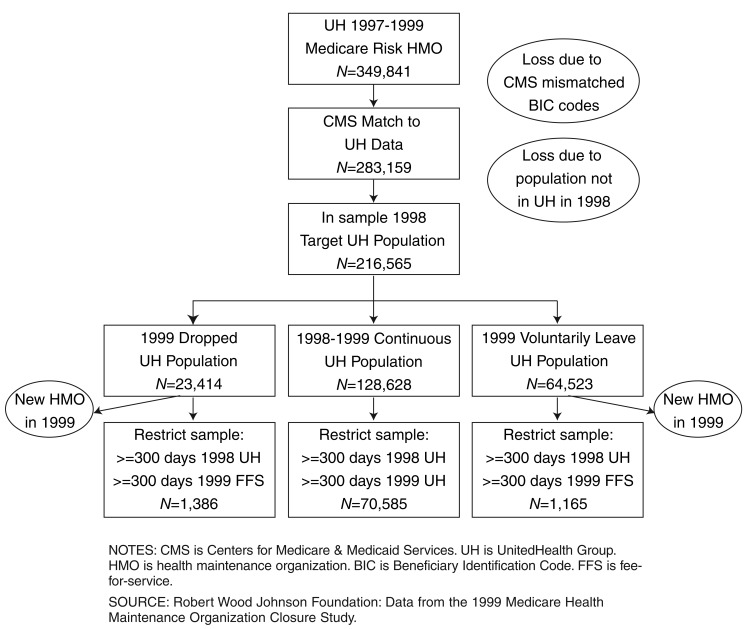
Combining the Medicare data with claims and administrative files from UnitedHealth was challenging due to structural differences in the two sources of data and timing of the data requests to complete the study. Figure 1 describes the selection of the study comparison population. The following are the four population development steps.
Figure 1. CMS and UnitedHealth Group Combined Study Population Development: 1998-1999.
In step one, UnitedHealth identified all Medicare HMO enrollees with any participation in a UnitedHealth HMO in 1997-1999 and created a finder file for CMS. This step yielded a starting population of 349,841 enrollees.
In step two, they sent a finder file with the enrollees to obtain CMS denominator file information, managed care enrollment data, and claims data for the beneficiary for the period 1997-1999. The resulting denominator file from CMS could only match 283,159 beneficiaries, a loss of 19 percent of the potential sample population. This loss was due to an inconsistency between the older way UnitedHealth was recording Beneficiary Identification Codes (BICs) and CMS's recently changed approach. A closer examination revealed the systematic under matching of female spouses and widowers on the data. Unfortunately, the source of the mismatch was discovered well after the data request to UnitedHealth and CMS. While this mismatch introduces a potential bias to our results, it is a consistent bias throughout the remainder of our study.
Step three identified UnitedHealth beneficiaries who were: enrolled in 1998, in the 1997-1999 population, and those age 65 or over. This step reduced the sample from 283,159 to 216,565, a reduction of 23.6 percent. This number became our starting “in sample” population for which we have adequate data for an evaluation. As part of this step we identify three different populations. The first group (23,414) is of greatest policy interest since they were to be involuntary disenrolled from a UnitedHealth health plan in 1999. The second group (128,628) remained enrolled in a UnitedHealth health plan in 1999 after enrollment in 1998. The third group (64,523) voluntarily disenrolled from UnitedHealth at the start of 1999. We identify voluntary disenrollment by observing the beneficiaries' county of residence of remaining UnitedHealth markets.
In the final step of our study population development, we made a restriction of 300 days of enrollment in a UnitedHealth managed care plan in 1998 and 300 days of enrollment in either CMS's FFS or a managed care plan. This significantly reduced our sample in voluntary and involuntary disenrollment from UnitedHealth populations because over 80 percent of beneficiaries enrolled in another HMO in the area. In addition, the 300-day restriction on UnitedHealth enrollment in 1998 and 1999 reduced the continuously enrolled population to 55 percent of its original size from 128,628 to 70,585. Due to minimal restriction in seniors' enrollment and disenrollment from the plans, a fairly transient managed care population is observed. We used the 300-day restriction to ensure we had consistent data for case-mix adjustment and cost and utilization measurement. In 1999, the median enrollment in FFS was 300 days, roughly the 60th percentile of UnitedHealth enrollment in 1998, and was considered a sufficient enrollment period to examine annual cost and utilization data. While we could have used per member per month (PMPM) calculations for cost and reduced the 300-day restriction, the case-mix adjustment procedure could not be as easily attenuated as PMPM to provide an accurate reflection of illness burden. The reduction of seniors from 23,414 to 1,386 within the involuntary withdrawal population who returned to FFS is quite substantial. However, this reduction is consistent combined combination of the probability of the population opting for a new HMO in 1999, the annual 300-day enrollment restrictions and the annual mortality rate of the Medicare population. A similar combination of factors reduced the sample size of the voluntary disenrollment potential population from 64,522 seniors to the study comparison group population of 1,165 seniors. Of these 64,522 beneficiaries, 8,851 participated in FFS, but the majority of this group had partial HMO enrollment of greater than 65 days.
After the four study population development steps, we identified three groups of enrollees for analysis:
HMO-HMO—In UnitedHealth continuously for 1998 and 1999.
HMO-FFS (ID)—The treatment group. People who moved from a UnitedHealth HMO in 1998 to FFS in 1999 after involuntary disenrollment in 1999.
HMO—FFS (V)-Voluntarily left UnitedHealth in 1998 and enrolled in FFS.
With these three cohorts, we are able to provide more information on the consequence of the withdrawal beyond earlier survey-based analyses. These three study cohort populations total 73,136 beneficiaries. The largest cohort (N=70,585), HMO-HMO, represents a comparison population of continuous UnitedHealth enrollees from 1998 to 1999. The treatment population (N=1,386) consisted of enrollees who were enrolled in UnitedHealth in 1998, involuntarily disenrolled from the HMO and FFS in 1999. We refer to this group as HMO-FFS (ID). The third group, labeled as, HMO-FFS (V), (N=1,165) was comprised of beneficiaries enrolled in UnitedHealth in 1998 who voluntarily returned to FFS in 1999.
For each study population we extracted the claims data for their annual period of enrollment from CMS and UnitedHealth. From these data we generated a series of dependent variables and explanatory variables at the beneficiary level for 1998 and 1999 experience using UnitedHealth and Medicare claims. Key outcome measures generated were: physician visits, inpatient stays, ER visits, outpatient hospital services, and laboratory tests. Key expenditure measures were: total, physician visit, outpatient hospital, and inpatient allowed charges, and out-of-pocket expenses. Allowed charges were calculated as the amount paid to the provider plus any coinsurance, copayment or deductibles paid by the beneficiary. The total out-of-pocket expenditures for both CMS and UnitedHealth were the union of deductible, coinsurance, and copayment measures. No pharmaceutical claims data was used in the analysis since there was not FFS equivalent in the Medicare Program due to obvious benefit design differences that predicated the MMA (2003) legislation. In addition to cost and utilization measures, we also include mortality as an outcome measure.
Age, sex, race, and illness burden variables were developed to account for differences in medical care demand. A vector of categorical ambulatory diagnostic groups (ADGs) was generated using claims data to identify illness burden (Weiner et al., 1991).2 Many of these variables were used to help identify the compatibility of comparing populations, rather than as actual control variables.
In Table 2, we report the sample 1998 means of the three study groups. The two return to FFS in 1999 groups, HMO-FFS (ID) and HMO-FFF (V) are similar in age, sex, and race characteristics. However, the populations are also dissimilar. For example, the HMO-FFS (ID) group tended to be healthier, 9.7 percent of beneficiaries had no ADGs, compared to 5.2 percent in the HMO-FFS (V) sample. Conversely, 18.7 percent of the HMO-FFS (V) population had 18.7 percent more beneficiaries with 6-10 ADGs than the treatment population. However, there was no statistically significant difference between these two populations in the largest illness burden category of greater than 10 ADGs. A greater share of the HMO-FFS (ID) population with no illness burden largely made up the difference in illness burden between the two populations.
Table 2. Sample Characteristics for Forced Choice Return to Fee-for-Serice (FFS) Treatment Population Compared to Continuous Health Maintenance Organization (HMO) and Voluntary Return to FFS: 1998.
| Characteristic | Forced Withdrawal Return to FFS | Continuous HMO | Voluntary Return to FFS |
|---|---|---|---|
| Observations | 1,386 | 70,585 | 1,165 |
| Percent | |||
| Average Age | 72.2 | 72.8 -(2.20) |
72.5 -(0.02) |
| 65-70 Years | 0.400 | 0.353 (3.40) |
0.404 -(0.38) |
| 70-75 Years | 0.272 | 0.300 -(2.19) |
0.257 (0.87) |
| 75-85 Years | 0.281 | 0.297 -(1.35) |
0.292 -(0.62) |
| 85 Years or Over | 0.050 | 0.050 -(0.02) |
0.046 (0.40) |
| Male | 0.523 | 0.493 (2.25) |
0.505 (0.88) |
| White Persons | 0.882 | 0.889 -(0.80) |
0.873 (0.67) |
| Average Number of Ambulatory Diagnostic Groups | 5.32 | 4.62 (7.88) |
5.85 -(3.77) |
| None | 0.097 | 0.092 (0.59) |
0.052 (4.21) |
| 1-5 | 0.462 | 0.555 -(6.90) |
0.439 (1.17) |
| 6-10 | 0.352 | 0.300 (4.16) |
0.418 -(3.42) |
| > Than 10 | 0.089 | 0.053 (5.98) |
0.091 -(0.13) |
NOTES: In parentheses are the t-statistics for comparison of means between the treatment population and the two comparison populations.
SOURCE: Robert Wood Johnson Foundation: Data from the 1999 Medicare Health Maintenance Organization Closure Study.
The HMO-HMO group was younger, healthier, and had slightly more female beneficiaries than the two return to FFS samples. There was no difference in race between the two groups. The results in Table 2 indicate that the three samples are fairly similar and that the treatment group might be categorized as having slightly favorable selection in terms of a proportionately less sick population than the HMO-FFS (V) group. However, we also found the HMO-HMO population to be even healthier than the forced return to FFS population. Thus, the group that was forced to leave UnitedHealth was associated with an illness burden in the middle of the case-mix distribution between the two other study populations.3
Statistical Method
Empirically, we used a regression model with individual fixed effects to estimate the impact of being involuntarily dropped from an HMO, and return to FFS, on health care use, cost, and mortality. In this difference-in-difference framework, we use beneficiaries continuously enrolled in HMOs to identify the time path of utilization that would have occurred in the absence of the intervention. The fixed-effects model allows us to control for permanent differences in utilization across people and market characteristics and allows for the real possibility that those who were involuntarily dropped and returned to FFS may have different levels of health care use than those continuously enrolled in HMO. Similar approaches have been used in other policy evaluations, for example, Liu et al. (1999) used a differences approach when analyzing the impact of a Medicaid managed care initiative on outpatient mental health utilization. More recently, Dranove et al. (2003) examined the difference in resource use and quality from the introduction of physician report cards for cardiac surgery in Pennsylvania and New York.
To control for some statistically significant case-mix differences between the two populations, in our regressions we included a vector of year-specific ADGs, where each of the 34 can take the value of 0 or 1, as well as the age of the beneficiary. While this also significantly improves our model fits, all regression-adjusted R2s were over 50 percent prior to adjustment. We also include a year categorical variable for 1999 to pick up any systematic trend differences. Race and sex are not included in the regressions since these variables are captured by the individual fixed effects.
For each outcome, we ran two models. First, we estimated the impact of moving to FFS from an HMO for those involuntarily disenrolled from an HMO using the HMO-HMO cohort as a comparison group. In a second model, we use the HMO-FFS (V) group as a second treatment group and compare their outcomes over time to the HMO-HMO group. These results show the differing impacts of forced versus voluntary withdrawal from an HMO to FFS health plan. For the dependent variable, mortality in 1999, we use a logistic regression on only the 1999 data and report the odds ratios associated with population cohort categorical variable as well as age, age squared, sex, race, and prior year categorical variables. From the regression models, we interpret the effect of forced withdrawal on beneficiaries or the CMS FFS program as a statistically significant difference for that population's outcome results.
Results
Table 3 presents the mean of the dependent variables for the three study populations in 1998, the year before our treatment group was involuntarily disenrolled from their HMO. The numbers in parentheses are the t-tests on the difference in mean between the HMO-FFS (ID) population and the other group. The treatment population had significantly higher utilization and expenditure in 1998 than the HMO-HMO population in nearly every outcome. Mortality rates in 1999 were nearly 40 percent higher in the treatment population than the HMO-HMO population. Alternatively, the HMO-FFS (V) population had significantly higher utilization and out-of-pocket expenditures than the treatment population. The average allowed expenditures between these two populations are not statistically different.
Table 3. Sample Characteristics for Outcomes, Treatment, Continuous Health Maintenance Organization (HMO), and Voluntary Return to Fee-for-Service (FFS) Samples: 1998.
| Characteristic | Forced Withdrawal Return to FFS | Continuous HMO | Voluntary Return to FFS |
|---|---|---|---|
|
| |||
| Percent | |||
| Physician Visits | |||
| Beneficiary Probability of Any Visit | 0.817 | 0.779 (3.41) |
0.867 -(3.40) |
| Beneficiary Average Visits | 4.10 | 3.259 (6.40) |
4.693 -(2.11) |
| Inpatient Stays | |||
| Beneficiary Probability of Any Stay | 0.154 | 0.137 (1.82) |
0.177 -(2.04) |
| Beneficiary Average Stays | 0.258 | 0.221 (1.98) |
0.324 -(1.52) |
| Emergency Room Visits | |||
| Beneficiary Probability of Any Visit | 0.133 | 0.078 (7.38) |
0.161 -(2.04) |
| Beneficiary Average Visits | 0.207 | 0.112 (7.41) |
0.263 -(1.89) |
| Any Outpatient | 0.604 | 0.473 (9.64) |
0.586 (0.90) |
| Average Lab Tests | 4.75 | 4.74 (0.05) |
5.802 -(2.69) |
| Average Out-of-Pocket Expenses | |||
| All Services | $79.93 | $73.57 (1.66) |
$111.58 -(4.64) |
| Physician Visits | $58.59 | $51.16 (3.72) |
$69.15 -(3.20) |
| Inpatient Stays | $6.08 | $12.82 (-2.69) |
22.54 -(4.20) |
| Outpatient | $15.26 | $9.59 (2.60) |
$19.89 -(1.47) |
| Average Allowed Charge | |||
| All Services | $4,484.61 | $3,176.45 (5.82) |
$4,439.03 (0.10) |
| Physician Visits | $1,792.62 | $1,309.03 (5.88) |
$1,736.73 (0.35) |
| Inpatient Stays | $1,825.22 | $1,388.55 (2.72) |
$2,034.34 -(0.74) |
| Outpatient | $866.77 | $478.87 (8.97) |
$667.97 -(1.47) |
| Mortality Rate in 1999 | 0.028 | 0.018 (2.65) |
0.013 (2.67) |
NOTE: In parentheses are the t-statistics for comparison of means between the treatment population and the two comparison populations.
SOURCE: Robert Wood Johnson Foundation: Data from the 1999 Medicare Health Maintenance Organization Closure Study.
Table 4 presents the effects of the closures on the treatment group, regression estimates for utilization, expenditure, and mortality variables of treatment population compared to the HMO-HMO population, and the marginal effect of the closure on each variable for the voluntary return to FFS population compared to the HMO-HMO population.
Table 4. OLS Estimates of Impact of Health Maintenance Organization (HMO) Closure on Outcomes and Impact of Moving From an HMO to Fee-for-Service (FFS): 1999.
| Characteristic | OLS Estimates of Forced Withdrawal Effect | OLS Estimates of Voluntary Return to FFS Effect | 1999 Mean Continuous HMO Populatio |
|---|---|---|---|
| Physician Visits | |||
| Beneficiary Probability of Any Visit | -0.042 (-4.22) |
-0.068 (-6.28) |
0.877 |
| Beneficiary Average Visits | -0.616 (-3.51) |
-0.342 (-1.78) |
6.507 |
| Inpatient Stays | |||
| Beneficiary Probability of Any Stay | 0.018 (1.68) |
0.019 (1.64) |
0.155 |
| Beneficiary Average Stays | 0.048 (2.31) |
0.017 (0.76) |
0.246 |
| Emergency Room Visits | |||
| Beneficiary Probability of Any Visit | 0.073 (7.35) |
0.053 (4.89) |
0.125 |
| Beneficiary Average Visits | 0.405 (20.92) |
0.265 (12.72) |
0.205 |
| Any Outpatient | 0.040 (2.73) |
0.098 (6.24) |
0.498 |
| Average Lab Tests | 0.786 (2.29) |
0.788 (2.11) |
10.546 |
| Average Out-of-Pocket Expenses - Percent Change | |||
| All Services | 168 (44.73) |
156 (38.40) |
$90.28 |
| Physician Visits | 134 (37.93) |
127 (33.45) |
$63.11 |
| Inpatient Stays | 94 (22.16) |
84 (18.22) |
$15.47 |
| Outpatient | 224 (46.49) |
215 (41.05) |
$11.70 |
| Average Allowed Charge - Percent Change | |||
| All Services | 1 (0.12) |
3 (0.54) |
$3681.41 |
| Physician Visits | 0 (0.00) |
-9 (-1.70) |
$1521.37 |
| Inpatient Stays | -1 (-0.06) |
-13 (-1.17) |
$1629.16 |
| Outpatient | -1 (-0.07) |
42 (4.22) |
$530.89 |
| Mortality - Odds Ratio | 1.410 | 0.602 | 0.018 |
| 95 Percent Odds Ratio Confidence Interval | 1.013 to 1.962 | 0.358 to 1.011 | — |
NOTES: OLS is ordinary least squares. In parentheses are the t-statistics for the OLS estimates.
SOURCE: Robert Wood Johnson Foundation: Data from the 1999 Medicare Health Maintenance Organization Closure Study.
With respect to physician visits, in the treatment population, we observe a smaller decrease in the propensity for a visit following a return to FFS (-4.2 percentage point) compared to the HMO-FFS (V) population (-6.8 percentage point), but an 80 percent larger decrease in average number of physician visits. In other words, more patients in the treatment population went to the doctor after they returned to FFS than the HMO-FFS (V) population, but once they had used these services, they had less physician encounters. For inpatient stays we see the opposite effect; although the effect on incidence has marginal precision (t-statistics: 1.68, 1.64), there is a 1.8 percentage point to 1.9 percentage point increase in incidence of admissions for both return to FFS populations, and the per capita frequency of admissions is significantly higher statistically in the treatment population compared to the HMO-HMO population.
In the case of ER visits, both return to FFS populations had an increased probability of using the service and, once they were users of the ER, a greater frequency of visits than the continuous population. These results are statistically significant in both populations. Comparing the marginal effects between the two return to FFS populations, the treatment group had 38 percent higher incidence and 51 percent higher utilization than the HMO-FFS (V) group. The treatment and HMO-FFS (V) populations had, respectively, a 4.0 percentage point and 9.8 percentage point greater probability of hospital outpatient services than the continuous population. Laboratory test utilization for the return to FFS population was nearly identical, (roughly 0.78 tests per person higher) to the continuous population.
The most significant financial impact on both returns to FFS populations was out-of-pocket expenditures, both in terms of statistical significance and magnitude. While the difference in average per person out-of-pocket expenditures at baseline was statistically insignificant between the treatment and continuously enrolled HMO populations, the treatment population faced total out-of-pocket medical expenditures which were 168 percent greater in 1999 than the continuous population. Much of this increase appears to be associated with physician (168 percent) and hospital outpatient (224 percent) expenditures. Treatment group inpatient expenditures were 94 percent greater than the continuously enrolled HMO population. The HMO-FFS (V) population faced increases very similar to the treatment population, when compared to the HMO-HMO population. These results suggest the out-of-pocket impact following a return to FFS is not substantially different for those who had to find a new plan in 1999—and then chose FFS—as opposed to beneficiaries who voluntarily chose FFS in 1999.
With regard to total allowed charges, we found no statistically significant difference at all, with one exception. For the HMO-FFS (V) population, outpatient expenditures were 42 percent higher than the HMO-HMO population. However, the forced choice population had no difference in outpatient expenditure. This result appears to be largely utilization driven from the previous results.
The odds ratio presented is interpreted as the chance of dying in 1999 in either a treatment or voluntary return to FFS scenario compared to being continuously in the HMO. The odds ratio of dying in a forced return situation equals 1.410, indicating a significantly higher chance of mortality than remaining in an HMO continuously. Alternatively, the probability of dying when voluntarily returning to FFS is less than remaining continuously enrolled in the HMO, but is not statistically significant. Our evidence suggests those who were forced to choose, and chose FFS, fared the worst in terms of health outcomes as measured by higher ER, inpatient use, and increased probability in mortality.
Discussion
This study provides the first comprehensive analysis of the impact of Medicare HMO closures on use-of-services and out-of-pocket costs of beneficiaries. While previous studies found similar results, with respect to increased out-of-pocket expenditure for beneficiaries facing involuntary withdrawal from a Medicare HMO, the results were very general and did not separate out-of-pocket medical expenses, (as we report), from out-of-pocket pharmacy expenses, which we assume to be an additional financial burden on beneficiaries in our treatment group.
Using claims data, we offer new findings with respect to Medicare HMO market exit. First, out-of-pocket expenditures increased significantly for HMO disenrollees for all types of services. Based on prior research from Laschober et al. (1999); and Booske, Lynch, and Riley (2002), we expected to see some increase in out-of-pocket expenditures. While this effect can also be interpreted as simply a result of returning to a benefit structure with higher cost sharing, we found that the increase in out- of-pocket expenditures was always proportionally higher for the treatment population than the HMO-FFS (V) population. Second, treatment beneficiary movement from an HMO to FFS Medicare was associated with an 80 percent higher decline in physician visits per person during the year than a voluntary choice to enroll in FFS. This result could be interpreted as the shock of the treatment population facing the Medicare Part B deductible and deciding to not seek care due to a beneficiary's budget constraint. Third, the marginal effect on probability of having an ER visit was 38 percent higher in the treatment population than the HMO-FFS (V) population and the difference in marginal effect on per capita utilization was 53 percent higher in the treatment population. This result may be an indicator of a beneficiary delaying care, as suggested with the earlier result, to the point where ER level attention is now required. At this point, the demand for some medical intervention may have reached a point of urgency and price inelasticity; even the Part B deductible for ER services is no longer considered a barrier to seeking services. Fourth, the treatment population had the highest rate of mortality of all the populations examined. The treatment population had a case mix adjusted mortality rate that was roughly 1 percentage point over all other groups. This result suggests, but cannot prove, that being forced to consider returning to FFS—and then making that choice—led to a substantial adverse outcome that seems plausible given the combination of reduced physician access, higher ER use and higher inpatient use, following case mix adjustment. Prior studies have demonstrated an adverse impact on the financial burden of seniors facing withdrawal, but the degree of the adversity could not be measured.
This study has four limitations. The first limitation is our inability to observe one counterfactual continuous population: claims data for those that switched to another HMO. Unfortunately, it is beyond the scope of our research to secure claims data from other health plans. Access to this type of data could have provided another continuous population and possibly better insight into continuity of care issues, as well as a more accurate assessment of the validity of our mortality results.
Our second limitation is that our conclusions regarding the effect of HMO are drawn from an approximately 15 percent minority of the forced disenrollment population. Although we can't observe outcomes for those who went to another HMO for the aforementioned limitation, we were able to compare the baseline demographics of our two populations and found that they were dissimilar in terms of prior utilization and case mix in 1998. The treatment population that chose to find another HMO had a higher illness burden and higher utilization of physician services. There was no difference in prior inpatient service utilization. While we recognize the likelihood of selection bias, our sensitivity analysis suggested that the population we examined who returned to FFS had favorable selection compared to those who found another HMO. This makes our treatment population ER, out-of-pocket expenditures, and mortality results more interesting since the direction of the bias suggests the adverse effects we observed could be underestimates of the impact of an HMO market exit.
Our third limitation is the original bias introduced by the mismatched BIC codes. We are fairly certain the result of the mismatch was an overrepresentation of males. Given that males tend to live shorter lives than females our expenditure, utilization, and mortality results may be biased upward due to a greater share of higher end of life expenditures in a managed care market typically characterized as being younger than FFS. However, we can not say conclusively how we expect the bias to effect our results. In defense of the result, the bias is consistent throughout the analysis.
Finally, 1 year may be too short of a time period to gauge the impact of the closures. Specifically, our results could be affected by regression to the mean. However, given the highly transient population we have already observed it is likely a 2-year FFS and HMO cohort with 300-day enrollment would greatly reduce the size of our sample and possibly affect its power for hypothesis testing.
Another explanation of our findings of higher expenditure and use for the treatment population may be the population was simply sicker to begin with in 1998 when compared to the continuous HMO population. However, the sickest population of the three groups examined in 1998 was the voluntary return to FFS group. If prior illness burden were the only explanation for higher cost and use impacts, than the HMO-FFS (V) population should have greatest impact. In contrast we find the greatest cost and use impact associated with HMO-FFS (ID) that suggests a unique adverse effect on the involuntary choice faced by beneficiary after an HMO market withdrawal.
Future Medicare managed care designers can use these results to highlight the costs of seniors involuntarily switching between HMO and FFS to help design an effective safety-net for beneficiaries to mitigate the adverse consequences that we discovered in our research. Because our population is, by its own plan selection in 1998, a more likely adopter of a managed care plan, these results provide insights into the downside of discontinuous enrollment in a Medicare financed managed care plan.
Acknowledgments
The authors would like to thank Kelly Merriman for her technical advice, Mona Shah, and Tom Horstman for facilitating all data creation from UnitedHealth Group; Lan Zhao for the SAS programming; and Gerald Riley of CMS. Special thanks to David Colby for his support of this project.
Footnotes
Stephen T. Parente is with University of Minnesota. William N. Evans is with University of Maryland. Julie A. Schoenman is with NORC at the University of Chicago. Michael D. Finch is with UnitedHealth Group. The statements expressed in this article are those of the authors and do not necessarily reflect the views or policies of the University of Minnesota, University of Maryland, NORC, UnitedHealth Group, or the Centers for Medicare & Medicaid Services (CMS).
The five dropped UnitedHealth markets we did not have data for were: Northern and Southern California, Chicago, Louisiana, and Maryland. Many of these plans were either new to UnitedHealth through acquisition or had not completed the integration of their data into the UnitedHealth national claims database.
ADGs are one of several comparable case mix adjustment systems that could be used for the Medicare population including episode treatment groups (ETGs) from Ingenix and DxCGs from Boston University. ADGs were chosen because of the authors familiarity with the adequacy of the ability of the algorithm from previous analyses (Parente et al., 1996; Parente, Salkever, and Davanzo, 2005). Additional information on ACGs can be found at http://www.acg.jhsph.edu/.
We did consider as another comparison population, the continuous FFS population using the 5-percent Medicare sample. This population had statistically significant different demographic and utilization patterns than the treatment population.
Reprint Request: Stephen T. Parente, Ph.D., University of Minnesota, Department of Finance, Carlson School of Management, 321 19th Avenue South, Suite 3-149, Minneapolis, MN 55455. E-mail: sparente@csom.umn.edu
References
- Booske B, Lynch C, Riley G. Impact of Medicare Managed Care Market Withdrawal on Beneficiaries. Health Care Financing Review. 2002 Fall;24(1):95–115. [PMC free article] [PubMed] [Google Scholar]
- Dranove D, Kessler D, McClellan M, et al. Is More Information Better? The Effects of Report Cards on Health Care Providers. Journal of Political Economy. 2003 Jun;111(3):555–588. [Google Scholar]
- Gold M, Justh N. Trends Reflect Fewer Choices. Monitoring Medicare+Choice Fast Facts. Mathematic Policy Research. 2000 Sep;(Number 4) [Google Scholar]
- Gold M, Smith A, Cook A, et al. Medicare Managed Care: Preliminary Analysis of Trends in Benefits and Premiums, 1997-1999. Mathematic Policy Research; Washington, DC.: 1999. [Google Scholar]
- Harrison S. New Developments in Medicare+Choice. Presentated at Medicare Payment Assessment Commission Meeting; Washington, DC.. October 2002. [Google Scholar]
- Laschober MA, Neuman P, Kitchman MS, et al. Medicare HMO Withdrawals: What Happens to Beneficiaries? Health Affairs. 1999 Nov-Dec;18(6):150–158. doi: 10.1377/hlthaff.18.6.150. [DOI] [PubMed] [Google Scholar]
- Liu CF, Manning WG, Christianson JB, et al. Patterns of Outpatient Use of Mental Health Services for Medicaid Beneficiaries Under a Prepaid Mental Health Carve-Out. Administration and Policy in Mental Health. 1999;26(6):401–15. doi: 10.1023/a:1021329722847. [DOI] [PubMed] [Google Scholar]
- Parente S, Weiner J, Garnick D, et al. Profiling Medicare Beneficiary Resource Use by Primary Care Practices: Implications for a Managed Medicare. Health Care Financing Review. 1996 Summer;17(4):23–42. [PMC free article] [PubMed] [Google Scholar]
- Parente S, Salkever D, DaVanzo J. The Role of Consumer Knowledge on the Demand for Preventive Health Care Among the Elderly. Health Economics. 2005 Jan;14(1):25–38. doi: 10.1002/hec.907. [DOI] [PubMed] [Google Scholar]
- Schoenman JA, Parente ST, Feldman JJ, et al. Impact of HMO Withdrawals on Vulnerable Medicare Beneficiaries. Health Care Financing Review. 2005 Spring;26(3):5–30. [PMC free article] [PubMed] [Google Scholar]
- U.S. General Accounting Office. Medicare Managed Care Plans: Many Factors Contribute to Recent Withdrawals; Plan Interest Continues. U.S. Government Printing Office; Washington, DC.: Apr, 1999. GAO/HEHS-99-91. [Google Scholar]
- U.S. Department of Health and Human Services. HMO Withdrawals: Impact on Medicare Beneficiaries. U.S. Government Printing Office; Washington, DC.: Aug, 2000. [Google Scholar]
- Weiner JP, Starfield B, Steinwach D, et al. Development and Application of a Population-Oriented Measure of Ambulatory Care Case-Mix. Medical Care. 1991 May;29(5) doi: 10.1097/00005650-199105000-00006. [DOI] [PubMed] [Google Scholar]