Abstract
The Medical Expenditure Panel Survey (MEPS) and National Health Expenditure Accounts (NHEA) are often used for health care policy analysis and simulations because they contain comprehensive estimates of national health care expenditures. The NHEA are primarily based on aggregate provider revenue data, while MEPS is based on person-level data on health care expenditures. This article compares MEPS and NHEA expenditure estimates for 2002 and discusses the differences. When MEPS and the NHEA are adjusted to be on a consistent basis, their expenditure estimates differ by 13.8 percent.
Introduction
NHEA and MEPS provide two of the most comprehensive sources of estimates of health care spending in the U.S. The NHEA cover the entire U.S. population and a full range of health care expenditures, including public health services and research. MEPS is designed to provide researchers and policymakers with detailed, person-level information on health expenditures from a nationally representative sample of households in the civilian, non-institutionalized population. Although each source provides a measure of total national spending on personal health care (PHC), at first glance the estimates may appear to diverge significantly. Once adjustments are made to account for the differences between NHEA and MEPS in terms of population, covered services, and other measurement concepts, the concordance is greater. In this article we describe the adjustments made to reconcile the estimates so that they measure the same concept. We then compare the NHEA and MEPS estimates for 2002 and discuss potential reasons for the differences.
Reconciling MEPS and NHEA serves two important purposes. First, it is an important quality assurance exercise for improving and ensuring the integrity of each source's estimates. The best way to identify potential weakness in data or assumptions is by comparing estimates to other sources. Second, the reconciliation is important because it provides a consistent baseline of health expenditure data for policy simulations, such as assessing the costs of expanding coverage to the uninsured. MEPS is often used in developing microsimulation models because it contains person-level expenditure, insurance coverage, and demographic data. Analysts adjust MEPS to be consistent with the NHEA so that the projected costs as well as budgetary and tax implications of any policy change are consistent with national health spending estimates.
In the next sections of this article we describe the MEPS and NHEA and summarize the adjustments needed to modify the NHEA so that they are as consistent as possible with MEPS. We conclude with a discussion of the reasons for the differences between the adjusted NHEA and MEPS estimates and how they changed since the previous reconciliation (Selden et al., 2001).
NHEA
NHEA measure total health spending in the U.S. and provide a structure to look at the relationship between payers and providers of goods and services over time. Since the structure adheres to national accounting principles, it can also be used to examine the relationship in health spending and overall economic growth, as measured by gross domestic product (GDP) and health spending in other countries. In this article we focus on the PHC sector, which includes the therapeutic goods and services rendered to treat or prevent a specific disease or condition (Centers for Medicare & Medicaid Services, 2006). NHEA estimates are produced annually in the U.S. by the Office of the Actuary at CMS.
The Office of the Actuary develops NHEA estimates from aggregate provider-based data sources, such as the U.S. Census Bureau's Economic Census and Service Annual Survey, the American Hospital Association, IMS Health (a market research firm that monitors drug sales from pharmacies) and government administrative data. The 2002 NHEA estimate for PHC spending is $1.3 trillion (Smith et al., 2006). Table 1 presents NHEA estimates for 2002 by service and source of payment categories.
Table 1. Unadjusted National Health Accounts for Personal Health Care, 20021.
| Type of Service | Out-of-Pocket | Private Health Insurance | Medicare | Medicaid | Defense | Veterans' Affairs | Workers' Compensation | Other Federal | Other State | Private Non-Patient | Type of Service Totals |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Hospital | $15.5 | $171.3 | $146.7 | $84.4 | $10.7 | $15.2 | $6.3 | $3.4 | $13.7 | $21.4 | $488.6 |
| Physician and Clinical Services | 35.2 | 162.7 | 67.7 | 23.8 | 3.8 | 1.8 | 11.2 | 6.2 | 1.1 | 24.4 | 337.9 |
| Dental | 32.4 | 36.6 | 0.1 | 3.5 | 0.0 | 0.0 | 0.0 | 0.5 | 0.2 | 0.1 | 73.3 |
| Other Professional Services | 11.9 | 16.1 | 8.6 | 2.4 | 0.0 | 0.0 | 3.3 | 0.2 | 0.4 | 2.7 | 45.7 |
| Home Health | 4.9 | 5.1 | 11.7 | 10.0 | 0.0 | 0.1 | 0.0 | 0.0 | 1.6 | 0.8 | 34.3 |
| Other Non-Durable Medical Products | 29.3 | 0.0 | 1.6 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 30.9 |
| Prescription Drugs | 40.0 | 78.7 | 2.4 | 27.8 | 1.8 | 1.8 | 2.0 | 0.7 | 2.6 | 0.0 | 157.9 |
| Durable Medical Equipment | 12.2 | 2.6 | 5.5 | 0.0 | 0.0 | 0.0 | 0.3 | 0.1 | 0.1 | 0.0 | 20.8 |
| Nursing Home | 29.5 | 8.6 | 14.1 | 47.1 | 0.0 | 2.2 | 0.0 | 0.0 | 0.2 | 4.0 | 105.7 |
| Other Personal Health Care | 0.0 | 0.0 | 0.0 | 31.6 | 1.3 | 1.4 | 0.0 | 3.5 | 3.9 | 4.7 | 46.3 |
| Source of Payment Totals | 210.8 | 481.8 | 258.2 | 230.7 | 17.7 | 22.5 | 23.1 | 14.6 | 23.9 | 58.2 | 1,341.4 |
In billions of 2002 U.S. dollars.
SOURCE: Centers for Medicare & Medicaid Services, Office of the Actuary: Data from the National Health Accounts, 2002.
Total expenditures by type of service are constructed primarily from estimates of provider revenues. Hospital expenditures are defined as hospital revenues from all sources, including net patient revenue (gross charges less contractual adjustments, bad debts, and charity care), non-patient revenue (such as parking lot revenue), non-operating revenue, and government tax appropriations. Expenditures for all services and goods that are sold in the hospital, such as hospital-based nursing homes, hospital-based home health care, and prescription drug sales, are counted as hospital revenues.
Expenditures for physician and clinical, dental, other professional, home health, and nursing home services are obtained from providers through the Service Annual Survey (U.S. Census Bureau, 2004b) and quinquennial Economic Census (U.S. Census Bureau, 2004a).
PHC expenditures by source of payment are estimated as follows. First, government spending on health care by source of payment is computed with data from government programs such as Medicare and Medicaid. Next, private expenditures are calculated as the residual of total expenditures minus government expenditures. The allocation of private expenditures across out of pocket, private health insurance, and other private sources is based on source of payment distributions from the Service Annual Survey, American Hospital Association (2002), and MEPS.
MEPS
In contrast to the NHEA, MEPS is a household-based survey that contains individual and household-level estimates of health expenditures and use, health insurance coverage, health status, employment, demographic and socioeconomic characteristics, and more. It is based on a nationally representative sample of the non-institutionalized, civilian population of the U.S. MEPS is the only comprehensive source of individual and household-level information regarding the amount and distribution of health expenditures by various demographic or socioeconomic characteristics (Cohen et al., 1996; Cohen, 1997). MEPS is also used to model or simulate individual or household-level behavior in response to policy changes, such as an expansion in health insurance coverage. It is produced by AHRQ and the National Center for Health Statistics.
MEPS expenditure data combine household-reported information primarily associated with medical care events with expenditure information obtained from providers through a followback survey. The household survey uses an overlapping panel design in which data are collected through five rounds of personal interviews during a 2.5 year period to cover use and expenditures over 2 calendar years. For the 2 most recent years for which MEPS data are publicly available, the MEPS sample includes data from 37,418 individuals with a positive sampling weight in calendar year 2002 and 32,681 individuals in 2003.1
MEPS estimates expenditures that are directly linked to patient care events. It excludes expenditures that are not directly linked to individual patients, such as maternal and child health grants for public and other community health clinics, Medicaid disproportionate share payments, and retrospective adjustments.
In addition, MEPS seeks to measure actual payments for health care services rather than charges, which are often higher. In general, if no payment occurred for a health care event, the MEPS expenditure total for that event is zero.
Like any survey database, MEPS estimates fluctuate from year to year in part due to random sampling variation (Machlin, Zodet, and Nixon, 2003). Using pooled data from 2002 and 2003 to smooth sampling variation, Table 2 presents MEPS expenditure estimates for the civilian non-institutionalized population by type of service and source of payment in 2002 dollars. Data from 2002 and 2003 were pooled by reweighting 2003 data to reflect 2002 population levels and expressing 2003 expenditures in constant 2002 dollars using the GDP price index.2 The total expenditure estimate for this population is $833 billion.
Table 2. Expenditure Estimates from the Medical Expenditure Panel Survey (MEPS), by Type of Service and Source of Payment: 20021.
| Type of Service | Out-of-Pocket | Private Health Insurance | Medicare | Medicaid | Defense | Veterans' Affairs | Workers' Compensation | Other Public | Other Sources | Type of Service Totals |
|---|---|---|---|---|---|---|---|---|---|---|
| Hospital | $11.1 (0.6) |
$146.0 (8.5) |
$108.9 (5.5) |
$29.9 (2.7) |
$3.3 (1.6) |
$9.6 (1.5) |
$12.0 (6.5) |
$1.3 (0.3) |
$2.2 (0.4) |
$324.3 (14.3) |
| Physician | 23.7 (0.8) |
93.2 (3.1) |
40.3 (1.4) |
16.3 (0.8) |
1.5 (0.2) |
3.4 (0.3) |
4.3 (0.4) |
2.0 (0.2) |
2.6 (0.3) |
187.3 (5.2) |
| Dentist | 31.3 (1.0) |
27.7 (1.1) |
0.2 (0.1) |
2.5 (0.2) |
0.2 (0.03) |
0.3 (0.05) |
0 (0.02) |
0.3 (0.06) |
1.6 (0.2) |
64.1 (2.2) |
| Other Providers | 10.8 (0.6) |
21.1 (0.9) |
7.8 (0.6) |
3.1 (0.3) |
0.4 (0.07) |
1.2 (0.2) |
1.7 (0.2) |
0.4 (0.1) |
1.3 (0.1) |
47.9 (1.9) |
| Home Health | 4.2 (1.1) |
2.1 (0.3) |
10.0 (0.9) |
12.2 (1.5) |
0 (0) |
0 (0) |
0 (0) |
2.4 (0.3) |
0 (0) |
31.0 (2.4) |
| Prescription Drugs | 70.0 (2.0) |
57.1 (1.9) |
6.0 (0.5) |
20.0 (1.0) |
1.5 (0.2) |
5.0 (0.3) |
0.1 (0.05) |
0.6 (0.2) |
0 (0.0) |
160.2 (4.2) |
| Other Medical Equipment | 10.6 (0.4) |
3.6 (0.2) |
1.4 (0.1) |
1.5 (0.1) |
0.3 (0.2) |
0.7 (0.1) |
0 (0) |
0.1 (0.04) |
0.3 (0.08) |
18.4 (0.7) |
| Source of Payment Totals | 161.6 (4.4) |
350.8 (12.4) |
174.6 (7.4) |
85.5 (4.1) |
7.2 (1.8) |
20.2 (1.8) |
18.2 (6.6) |
7.1 (0.6) |
8.0 (0.6) |
833.2 (23.3) |
In billions of 2002 U.S. dollars, computed by pooling MEPS expenditures from 2002 and 2003. MEPS expenditures from 2003 are expressed in 2002 dollars by reweighting the 2003 MEPS sampling weights to be consistent with 2002 population levels, and by converting 2003 expenditures into constant 2002 dollars using the gross domestic product deflator.
NOTE: Standard errors are in parentheses.
SOURCE: Agency for Healthcare Research and Quality, Center for Financing, Access, and Cost Trends: Data from the Medical Expenditure Panel Survey Household Component, 2002 and 2003.
NHEA and MEPS Differences
The NHEA and MEPS differ with respect to their included populations, included services, and service category definitions. The NHEA includes expenditures for active duty military personnel, foreign visitors to the U.S., and people in institutions such as nursing homes, all of whom are out of scope for MEPS. NHEA also includes expenditures for long-term hospital stays of 45 days or more which MEPS excludes as out-of-scope.
In terms of services, MEPS excludes private non-patient care revenues, such as revenues from philanthropic giving, cafeterias, and investment income. In addition, MEPS does not capture data on non-prescription non-durable goods (such as over-the-counter medications) and other PHC services. The NHEA category of other PHC services covers health services such as vaccines and health screening delivered in non-health establishments such as the work place and schools. These expenditures are not technically out of scope for MEPS, but it is highly unlikely that such visits would be reported. The largest public component of other PHC consists of Medicaid spending on home and community-based waivers. Personal care services are deemed out-of-scope for MEPS because they are primarily personal care services provided to individuals who are out-of-scope for MEPS.
In addition, the NHEA and MEPS group services differently. NHEA service categories are defined according to the type of establishment that collected the revenue, while MEPS service categories are defined according to the type of service provided to an individual. For instance, NHEA hospital expenditures are based on all revenue received by hospitals. This includes expenditures for inpatient care, which are also in the MEPS hospital category, as well as expenditures for hospital-based home health services, which are in the MEPS home health category.
Adjusting the NHEA
Adjustments to the NHEA to make it consistent with MEPS can be roughly grouped into three broad categories:
Aligning service categories.
Adjusting the scope of included population.
Adjusting for non-patient care revenues.
The adjustments we make to the NHEA are summarized in Tables 3 and 4. Table 3 summarizes some of the adjustments we make to align NHEA service categories with MEPS. Table 4 summarizes the subtractions we make from the NHEA to make the included population and patient care expenditures consistent with MEPS. These adjustments require detailed estimates for expenditure categories and population subsets that are often difficult to measure accurately. Most of the adjustments are based on published data. Because there are no detailed survey data that measure these expenditures, our estimates of the acute care expenditures for the institutionalized population and for people receiving long-term care from Veterans' Administration (VA) providers are based on authors' calculations developed in consultations with experts. Estimates of acute care expenditures for the institutionalized are developed in conjunction with the Actuarial Research Corporation. Estimates of long-term health care provided by the VA are based on analyses conducted by their researchers (Burgess, 2005).
Table 3. Selected Adjustments to Align National Health Expenditure Accounts (NHEA) Service Categories with the Medical Expenditure Panel Survey.
| Amount Shifted1 | Initial NHEA Category | New Category |
|---|---|---|
| $13.3 | Hospital | Home Health |
| Hospital-Based Home Health | ||
| $3.4 | Hospital | Prescription Drug |
| Hospital-Based Pharmacy Sales | ||
| $1.6 | Hospital | Other Personal Care |
| Hospital-Based Personal Care | ||
| $11.2 | Physician and Clinical Services | Other Professional Services |
| Outpatient Mental Health ($4.6) | ||
| Kidney Dialysis Providers ($1.3) | ||
| Other Providers ($5.3) | ||
| $5.2 | Physician and Clinical Services | Prescription Drugs |
| Prescription Drugs | ||
| $2.2 | Physician and Clinical Services | Other Medical Equipment |
| Durable Medical Equipment | ||
| $22.5 | Physician and Clinical Services | Other Professional Services |
| Independently-Billed Laboratory |
In billions of 2002 U.S. dollars.
SOURCES: Calculations based on the Medical Expenditure Panel Survey, NHEA, and other data sources, 2002-2005.
Table 4. Subtractions from the National Health Expenditure Accounts (NHEA) to Make It Consistent with the Medical Expenditure Panel Survey (MEPS).
| Amount Subtracted1 | Health Care Service or Type of Expenditure |
|---|---|
| Long-Term Care Facility Expenditures | |
| $15.2 | Hospital (Non-Community) |
| $127.0 | Nursing Home |
| $3.3 | Hospital (Veterans' Administration) |
| $0.4 | Physician (Veterans' Administration) |
| Acute Care Expenditures of Institutionalized | |
| $52.0 | Acute Care Services for People in Institutions |
| Expenditures for Active Duty Military and Foreign Visitors | |
| $10.2 | Active Duty Military Expenditures |
| $1.7 | Services for Foreign Visitors to U.S. |
| Patient Care Services Not Captured In MEPS | |
| $31.0 | Non-Durable Medical Products (e.g., Aspirin and Bandages) |
| $58.5 | Other Personal Health Care (e.g., Housekeeping Services) |
| Non-Patient Care Revenues Not Included in MEPS | |
| $37.5 | Private Non-Patient Services (e.g., Gift Shop Revenue) |
| $21.0 | Replace NHEA Other Public Expenditures with MEPS Other Public Expenditures |
| $17.0 | Disproportionate Share Hospital and Graduate Medical Education |
| Previously Paid Expenditures | |
| $2.5 | Lab Services and Tests Paid by Other Providers |
| Total | |
| $377.3 | Total Subtractions |
In billions of 2002 U.S. dollars.
SOURCES: Available on request from: Merrile Sing, Ph.D., Agency for Healthcare Research and Quality, 540 Gaither Road, Rockville, MD 20850. E-mail: merrile.sing@ahrq.hhs.gov
To obtain adjusted NHEA estimates that are consistent with MEPS, we adjusted the NHEA service and source of payment category totals in Table 1, as well as the more detailed distributional estimates by type of service and source of payment. We made the adjustments across source of payment categories in proportion to the corresponding NHEA category's source of payment distribution because all adjustments (except one) were made to the NHEA. Although the NHEA service and source of payment totals are official estimates, the adjustments we present in Tables 3 and 4 should not be deemed official.
Comparison of the Adjusted NHEA and MEPS
The adjusted NHEA estimate for 2002 is $964 billion (Table 5), compared with the unadjusted NHEA estimate of $1,341 billion (Table 1). Thus, our reconciliation removes approximately $377 billion from the NHEA. We adjust the total MEPS expenditure estimate of $833 billion (Table 2) by removing approximately $2 billion in massage therapy and non-Medicare ambulance services that are not in the NHEA. The total adjusted MEPS expenditure estimate is $831 billion, with a 95-percent confidence interval of $785 billion to $877 billion. The adjusted MEPS is $133 billion (13.8 percent) less than the adjusted NHEA total (Table 6).
Table 5. National Health Expenditure Accounts (NHEA) Adjusted to be Consistent with the Medical Expenditure Panel Survey: 20021.
| Type of Service | Out-of-Pocket | Private Health Insurance | Medicare | Medicaid | Defense | Veterans' Affairs | Workers' Compensation | Other Public | Other Sources | Type of Service Totals |
|---|---|---|---|---|---|---|---|---|---|---|
| Hospital | $12.1 | $149.6 | $112.6 | $55.8 | $1.1 | $10.7 | $5.8 | $1.3 | $2.2 | $351.2 |
| Physician | 23.8 | 131.8 | 44.7 | 17.1 | 3.8 | 1.1 | 9.3 | 2.0 | 2.6 | 236.3 |
| Dentist | 31.9 | 34.8 | 0.1 | 3.5 | 0.0 | 0.0 | 0.0 | 0.3 | 1.6 | 72.2 |
| Other Providers | 13.6 | 30.4 | 11.8 | 4.1 | 0.0 | 0.1 | 4.9 | 0.4 | 1.3 | 66.5 |
| Home Health | 4.7 | 9.8 | 14.0 | 9.9 | 0.3 | 0.6 | 0.2 | 2.4 | 0.0 | 41.9 |
| Prescription Drugs | 39.7 | 83.7 | 2.3 | 34.6 | 1.9 | 1.9 | 2.1 | 0.6 | 0.0 | 166.8 |
| Other Medical Equipment | 17.5 | 2.6 | 8.3 | 0.0 | 0.0 | 0.0 | 0.3 | 0.1 | 0.3 | 29.0 |
| Source of Payment Totals | 143.4 | 442.7 | 193.8 | 125.0 | 7.2 | 14.3 | 22.7 | 7.1 | 8.0 | 964.0 |
In billions of 2002 U.S. dollars.
SOURCE: Calculations based on the Medical Expenditure Panel Survey, NHEA, and other data sources, 2002-2005.
Table 6. Selected Differences Between Adjusted Medical Expenditure Panel Survey (MEPS) and Adjusted National Health Expenditure Accounts (NHEA): 20021.
| Type of Service | Out-of-Pocket | Private Health Insurance | Medicare | Medicaid | Defense | Veterans' Affairs | Workers' Compensation | Type of Service Totals | Differences as Percentage of Adjusted NHEA |
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Percent | |||||||||
| Hospital | -1.1 | -3.5 | -3.7 | -26.0 | 2.2 | -1.1 | 6.2 | -26.9 | -8.0 |
| Physician | -0.1 | -38.6 | -4.4 | -0.8 | -2.4 | 2.3 | -5.0 | -49.0 | -21.0 |
| Dentist | -0.6 | -7.1 | 0.2 | -1.0 | 0.2 | 0.3 | 0.0 | -8.1 | -11.0 |
| Other Providers | -3.4 | -9.3 | -4.0 | -1.0 | 0.4 | 1.1 | -3.2 | -19.4 | -29.0 |
| Home Health | -0.6 | -7.7 | -4.0 | 2.4 | -0.3 | -0.5 | -0.2 | -10.9 | -26.0 |
| Prescription Drugs | 30.3 | -26.7 | 3.7 | -14.6 | -0.4 | 3.1 | -2.0 | -6.6 | -4.0 |
| Other Medical Equipment | -7.5 | 0.4 | -6.9 | 1.5 | 0.3 | 0.7 | -0.3 | -11.8 | -41.0 |
| Source of Payment Totals | 17.0 | -92.5 | -19.2 | -39.5 | 0.0 | 5.9 | -4.5 | -132.8 | -13.8 |
| Differences as Percentage of Adjusted NHEA | 12.1 | -21.0 | -10.0 | -32.0 | 0.0 | 41.0 | -20.0 | -13.8 | — |
In billions of 2002 U.S. dollars.
NOTES: MEPS was adjusted to remove two services that are not included in the NHEA: massage services (approximately $0.8 billion) and non-Medicare ambulance services (approximately $1.2 billion). The difference between the adjusted MEPS and NHEA estimate for each service and source of payment category cell in this table is computed by subtracting the adjusted NHEA estimate from the adjusted MEPS estimate. The percentage differences are computed by dividing this difference by the adjusted NHEA estimate.
SOURCES: Calculations based on the Medical Expenditure Panel Survey, NHEA, and other data sources, 2002-2005.
1996 Reconciliation
The NHEA-MEPS difference of 13.8 percent is substantially larger than the adjusted difference of 6.7 percent found in a previous reconciliation of the 1996 NHEA and MEPS (Selden et al., 2001), and might suggest a substantial widening of the gap between NHEA and MEPS over time. A detailed comparison of the 1996 and 2002 reconciliations, however, finds that much of the difference can be traced to methodological changes and data improvements in the adjustments to better match the two sets of estimates. This includes a basic change in approach as well as important improvements in data quality.
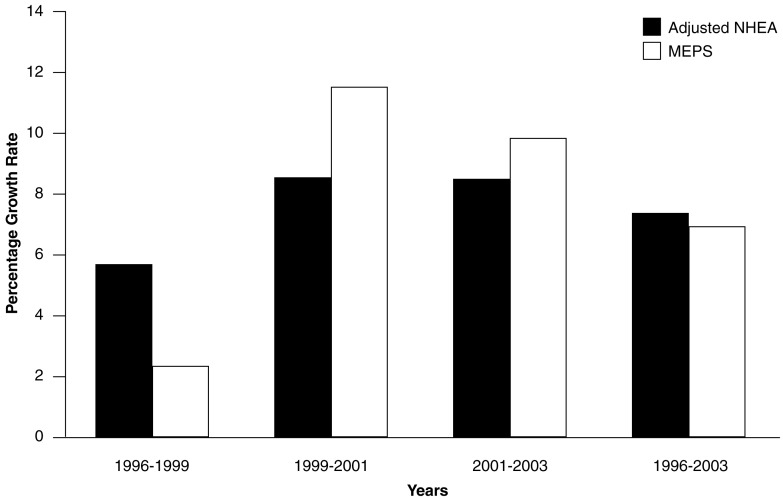
As a starting point for thinking about NHEA and MEPS over time, Figure 1 presents the results of a simplified reconciliation using methods applied consistently over time. To construct this figure, we focused on NHEA expenditures in four categories: (1) out of pocket, (2) PHI, (3) Medicare, and (4) Medicaid. We also adjusted the scope of goods and services in NHEA solely by removing nursing home facility costs, non-Federal non-community hospitals, non-prescription non-durable medical products, and other PHC. As Figure 1 shows, MEPS grew more slowly than the adjusted NHEA between 1996 and 1999, and grew more rapidly than the adjusted NHEA in the latter two periods. Over the entire 1996-2003 period, the average annual growth rate in the NHEA was 7.3 percent, compared with 7.0 percent in MEPS. These annual growth rates translate into a cumulative growth over the 1996 to 2003 period of 63.5 percent in the NHEA, compared with 60.4 percent in MEPS. The growth rates in this figure should be interpreted with caution, because they are based on only a partial reconciliation. However, the fact that growth in the adjusted NHEA outpaced MEPS by a cumulative total of only 3.1 percentage points in this analysis suggests that much of the reason for the widening gap between 1996 and 2003 stems from changes in the reconciliation methodology.
Figure 1. Annual Nominal Growth Rates in Partially-Adjusted National Health Expenditure Accounts (NHEA) and Medical Expenditure Panel Survey (MEPS)1: 1996-2003.
1 Based on a simplified, but consistently-applied reconciliation of out of pocket, private health insurance, Medicare, and Medicaid payments in NHEA and MEPS.
SOURCES: Calculations based on the MEPS, NHEA, and other data sources, 1996-2003.
The first and by far the largest improvement in data quality concerns estimates of acute care spending of the institutionalized. Because no national survey provides acute care expenditure estimates for the institutionalized, any effort to develop estimates requires the use of numerous data-sets and strong assumptions. The 1996 reconciliation subtracted $57 billion (1996 dollars) for residents in nursing homes and assisted living, while the 2002 reconciliation subtracts a smaller nominal amount ($52 billion in 2002 dollars) to account for the acute care expenditures of residents in nursing homes, assisted living facilities, intermediate care facilities for the mentally retarded, and other long-term care settings. We now believe that the 1996 adjustments were too large. As one example, in the 1996 reconciliation the authors used scaled down industry estimates for the assisted living population. Recently available data show that these scaled down estimates appear to be too high by a factor of nearly two (Spillman and Black, 2005). Another change is that the most recent methodology yields lower estimates of acute care spending per person in the institutionalized population in 2002 compared with 1996.
A second improvement in data quality is that the 1996 reconciliation was based on provider revenue data for industries based on the Standard Industrial Classification (SIC), whereas the 2002 reconciliation is based on industry data disaggregated using the North American Industry Classification System (NAICS). NAICS represents a substantial improvement over SIC for our purposes, because NAICS allows for a more precise distinction between revenues that are in-scope versus out-of-scope for MEPS. In light of the NAICS data, we suspect that SIC-based adjustments in 1996 narrowed the NHEA-MEPS gap by perhaps 1-2 percentage points more than warranted.
In addition to improvements in data quality, we also made several methodological changes that hold MEPS to a more rigorous standard. In the 1996 reconciliation, expenditure types that were deemed too costly for MEPS to collect in detail were excluded from NHEA, even if they were technically in-scope for MEPS. For the current reconciliation, we chose to reduce or eliminate these adjustments. For example, the 1996 reconciliation adjusted NHEA for all expenditures at family planning clinics, even though some were in-scope, because MEPS is not designed to measure such expenditures accurately. In the current reconciliation, only a portion of such expenditures are removed from the NHEA, thereby adhering to a more rigorous definition of what MEPS should in principle capture.
This change in approach affects not only the overall comparison of NHEA and MEPS, but also comparisons by type of service. For instance, in the 1996 reconciliation, some NHEA physician and clinic expenditures were shifted to the hospital category in view of the difficulty some MEPS respondents may face in distinguishing whether outpatient clinics are affiliated with hospitals. This adjustment was discontinued for the 2002 reconciliation, thereby tending to increase the apparent gap between NHEA and MEPS physician and clinic estimates while narrowing the apparent gap for hospital expenditures.
For these reasons, we caution the reader against drawing strong conclusions from comparisons of the 1996 and 2002 results. In the rest of this section we discuss the differences between MEPS and NHEA expenditure estimates by type of service and source of payment, focusing on the largest service and source of payment categories.
Service Category
The adjusted NHEA expenditure estimates are greater than those from MEPS for every service category (Table 6). Whereas we observe a relatively narrow gap for hospital expenditures, the largest difference in expenditures is for the physician sector, where MEPS is $49 billion (21 percent) lower than the NHEA. As previously discussed, a portion of this gap may reflect differences in how NHEA and MEPS treat the nearly $30 billion in outpatient clinic expenditures. Shifting a portion of this outpatient clinic total either from physicians to hospitals in the NHEA (as done in 1996) or vice versa in the MEPS would help to even out the apparent NHEA-MEPS differences for these two categories. This illustrates the caution needed when making direct comparisons between NHEA and MEPS based on data in Table 6.
MEPS treats hospitalizations longer than 45 days as out-of-scope, and comparisons between MEPS and PHI claims data from MarketScan3 suggest that this may reduce MEPS hospital expenditures by over 5 percent (and perhaps more in the Medicare and Medicaid populations). Also, MEPS may inadvertently miss some high-cost hospital and physician expenditures that occur just before sampled persons die or are placed in a nursing home if MEPS interviewers have difficulty locating someone to report on their use and expenditures. Furthermore, while hospitalizations may be more easily recalled by MEPS respondents than physician visits, the 2002 MEPS estimate of physician office visits (977 million) is about 10 per-cent higher than the estimate of physician office visits from the National Ambulatory Medical Care Survey (NAMCS) (Woodwell and Cherry, 2004; Agency for Healthcare Research Quality, 2004).4
For these reasons, it is perhaps more accurate to view the hospital and physician estimates together. This is particularly true when looking at sources of payment (Table 6). The NHEA-MEPS difference for physician expenditures is heavily concentrated in the PHI payer category, whereas the PHI difference for hospital expenditures is small. In contrast, for Medicaid we observe a much smaller difference for physician expenditures and a much larger difference for hospital expenditures. This may, in part, be a function of the NHEA methodology used to distribute premiums associated with managed care plans. Currently NHEA distributes these expenditures (about 14 percent of total Medicaid expenditures) using the fee-for-service expenditure distributions by State with some adjustments for carve-out plans. This may allocate too much spending to the hospital sector and not enough to the physician sector, because fee-for-service enrollees are more likely to include the elderly and disabled, while managed care enrollees are more likely to include children and their parents. In addition, this method will affect the private spending estimates within each service category, since private expenditures are estimated as a residual after public expenditures are estimated. As a sensitivity analysis, we used the MEPS type of service distribution for Medicaid managed care to reallocate these NHEA Medicaid expenditures. Based on this analysis, perhaps as much as $8-10 billion could be shifted from the adjusted NHEA Medicaid hospital cell to other types of services, entailing offsetting adjustments in NHEA estimates of PHI and out-of-pocket expenditures.
Part of the MEPS-NHEA physician difference may also stem from the complex financial arrangements in the U.S. health care system, which include duplicative provider payment flows and provider payments (such as bonuses) that are not directly linked to specific patient care events. Provider payments that are not linked to events pose a potential problem for MEPS, which relies on payments linked to events, while duplicative payments pose a potential problem for NHEA estimates because NHEA relies on data collected at the office or clinic level (Zuvekas and Hill, 2004). Nearly $4 billion is subtracted from the NHEA to avoid double-counting payments that physician offices and clinics receive from hospitals, since these payments are already included in the NHEA hospital estimates.
Prescription drug spending is 10 percent higher in the NHEA than the MEPS. Underreporting may be an issue with the MEPS estimate; a recent study suggests that Medicare beneficiaries underreport prescription drug expenditures by 17 percent (Poisal, 2003-2004). There are also large differences between payers for prescription drugs, particularly between out of pocket (where MEPS is 30 percent higher than the NHEA) and PHI spending (where MEPS is 27 percent lower). Part of these differences may be explained by the NHEA methodology for allocating revenue to PHI and out of pocket as well as response rates in the MEPS followback survey to pharmacies (Centers for Medicare & Medicaid Services, 2006).
Another large difference between MEPS and the adjusted NHEA occurs in the other provider category, for which the adjusted NHEA estimate is $19 billion (29 percent) larger than MEPS. Part of this difference is likely due to underreporting of independently billed laboratory tests in MEPS. Whereas the adjusted NHEA contains $22 billion in independently billed laboratory tests, event-level reporting by households in the 2002 MEPS identified only $6.6 billion in laboratory tests billed separately from the associated physician events. MEPS does not field a provider followback survey to independent medical labs, diagnostic, and testing facilities.
Source of Payment
Three of the four largest source of payment categories from the adjusted NHEA are greater than those from MEPS: (1) adjusted NHEA estimates are 32 percent greater for Medicaid, (2) 21 percent greater for PHI, (3) 10 percent greater for Medicare, and (4) 12 percent less for out of pocket (Table 6).
Some of the difference in the Medicaid expenditure estimates can be explained by MEPS underestimating persons with Medicaid coverage. Banthin and Sing (2006) found that estimates of Medicaid enrollees from MEPS are approximately 12 percent below enrollment counts from administrative data.
In addition, the NHEA expenditure estimates for Medicaid and Medicare may be higher relative to MEPS due to undetected fraudulent billing practices (e.g., cases in which billed care was never provided) (Levinson, 2005). The NHEA expenditure estimates are adjusted for fraudulent billing that has been detected and quantified. Since the source of funding estimates in the NHEA are consistent with budget data for public programs such as Medicare and Medicaid, estimates of fraudulent billings would be inherent in the data and exceedingly difficult to estimate and remove, whereas they would likely not be reported in MEPS.
The out-of-pocket expenditures estimate from MEPS is 12 percent greater than the estimate from NHEA. Since MEPS collects data on out-of-pocket expenditures directly from households, out-of-pocket estimates are considered to be one of MEPS' strengths. As previously noted, out-of-pocket payments and PHI are residual source-of-payment categories in the NHEA, and the allocation of expenditures between them is sensitive to the underlying assumptions.
We estimate a 21-percent difference between the MEPS and NHEA estimates for PHI that is difficult to explain. On one hand, MEPS service-use measures, such as physician office visits, benchmark well to the NAMCS. On the other hand, aggregate PHI estimates from NHEA for 2002 are within 5 percent of estimates of PHI spending generated from the MEPS Insurance Component, an annual survey of employers.
Similar to the 21 percent difference we find in PHI, Zuvekas and colleagues (2005) find that MEPS estimates of mean health expenditures for PHI enrollees covered through large employers are approximately 21 percent lower than expenditures estimated with MarketScan data. They estimate that approximately 60 percent of this difference is due to missing expenditure data because people with more than $100,000 in total annual health expenditures are underrepresented in MEPS. MEPS may be missing some expenditures for these high-cost cases because some MEPS sample members underreport these expenditures, some MEPS sample members die or enter an institution before these data are collected, or some high-cost cases (such as people in an institution for the entire year) are never in-scope for MEPS.
Discussion
We estimate that total health care expenditure estimates in 2002 differ between MEPS and NHEA by $133 billion, or 13.8 percent. The reader should bear in mind that the true difference between the adjusted NHEA and MEPS estimates could be different from this estimate. It is important to emphasize that aligning the two estimates entails numerous assumptions, and the adjustments we implement are subject to error. It would be difficult to test the sensitivity of all the assumptions underlying the many steps involved in reconciling the two sources of data. One optimistic finding from this analysis is that if the 1996 and 2002 reconciliations are done using similar data and methodologies, there does not appear to be a large increase in the estimated gaps between the two data sources.
Looking across service types and sources of payment, it appears that measurement issues in MEPS and NHEA may contribute to the gaps we observe. For MEPS, although utilization measures align quite closely with provider utilization data, the gaps we find for physician and hospital expenditures highlight the merit of improving data collection from high-expenditure cases. The reconciliation also highlights the importance of ongoing AHRQ research aimed at evaluating and improving strategies to improve corrections for survey attrition, a potential problem with any longitudinal survey. For NHEA, measurement issues may also contribute to the gap. Part of the large gaps in PHI and out-of-pocket expenditures may arise because private expenditures in NHEA are calculated as a residual, and are thus subject to measurement issues associated with provider surveys as well as public program data. Also contributing to the overall gap might be NHEA measurement issues surrounding provider-to-provider payment flows.
We hope this reconciliation allows users of MEPS and NHEA to better understand why these data sources yield different expenditure estimates. This reconciliation will help AHRQ and CMS focus future research efforts in the appropriate areas to improve expenditure estimates from MEPS and the NHEA.
Acknowledgments
The authors would like to thank Katherine Levit, David McKusick, D.E.B. Potter, Joel Cohen, Samuel Zuvekas, Steven Machlin, Stephen Heffler, Steven Cohen, and James Burgess.
Footnotes
Merrile Sing, Jessica S. Banthin, and Thomas M. Selden are with the Agency for Healthcare Research and Quality (AHRQ). Cathy A. Cowan and Sean P. Keehan are with the Centers for Medicare & Medicaid Services (CMS). The statements expressed in this article are those of the authors and do not necessarily reflect the views or policies of AHRQ or CMS.
The total MEPS sample includes some people who are out-of-scope for MEPS, but have family member(s) that are in-scope for MEPS. Out-of-scope MEPS sample members have zero sampling weights.
We use the GDP price index because it includes government purchases and investment goods, which are omitted from the consumer price index.
The data from MarketScan contain service-level medical claims and encounter data of health care cost obtained from employers and health plans.
Comparisons between MEPS and NAMCS are complicated by differences in how events are defined and populations covered (Machlin, Valluzi, Chevarly, et al., 2001).
Reprint Requests: Merrile Sing, Ph.D., Agency for Healthcare Research and Quality, 540 Gaither Road, Rockville, MD 20850. E-mail: merrile.sing@ahrq.hhs.gov
References
- Agency for Healthcare Research and Quality. Full Year Consolidated Data File (HC-070) 2004 Dec; Medical Expenditure Panel Survey Household Component Data Generated Using MEPSnet/HC. Internet address: http://www.meps.ahrq.gov (Accessed 2006.)
- American Hospital Association. Chicago, IL.: 2002. Annual Survey. Internet address: http://www.aha.org (Accessed 2006.) [Google Scholar]
- Banthin JS, Sing M. How Medicaid Enrollment Estimates from MEPS Compare with Administrative Totals. Agency for Healthcare Research and Quality; Rockville, MD.: 2006. Working paper. [Google Scholar]
- Burgess J. Management Science Group, personal communication. U.S. Department of Veterans Affairs; Sep, 2005. [Google Scholar]
- Centers for Medicare & Medicaid Services. Office of the Actuary; Jan, 2006. National Health Expenditure Accounts: Definitions, Sources, and Methods Used in the NHEA, 2004. Internet Address: http://new.cms.hhs.gov/NationalHealthExpendData/ (Accessed 2006.) [Google Scholar]
- Cohen JW, Monheit AC, Beauregard KM, et al. The Medical Expenditure Panel Survey: A National Health Information Resource. Inquiry. 1996 Winter;33(4):373–389. [PubMed] [Google Scholar]
- Cohen SB. Sample Design of the 1996 Medical Expenditure Panel Survey Household Component. U.S. Government Printing Office; Washington, DC.: 1997. MEPS Methodology Report No. 2. Pub. No. 97-0027. Agency for Health Care Policy and Research. [Google Scholar]
- Levinson DR. Testimony of the Inspector General, U.S. Department of Health and Human Services. 2005 Jun 28; Hearing before the Senate Committee on Finance. Internet address: http://oig.hhs.gov/testimony/docs/2005/50628-levinson-fin.pdf (Accessed 2006.)
- Machlin S, Zodet M, Nixon J. Estimates of Medical Expenditures from the Medical Expenditure Panel Survey: Gains in Precision from Combining Consecutive Years of Data. Proceedings of the American Statistical Association, Section on Survey Research Methods; Alexandria, VA.: American Statistical Association; 2003. [Google Scholar]
- Machlin SR, Valluzi JL, Chevarly M, et al. Measuring Ambulatory Health Care Use in the United States: A Comparison of 1996 Estimates Across Four Federal Surveys. Journal of Economic and Social Measurement. 2001;27(1-2):57–69. [Google Scholar]
- Poisal JA. Reporting of Drug Expenditures in the MCBS. Health Care Financing Review. 2003-2004 Winter;25(2):23–36. [PMC free article] [PubMed] [Google Scholar]
- Selden T, Levit K, Cohen J, et al. Reconciling Medical Expenditure Estimates from the MEPS and NHA, 1996. Health Care Financing Review. 2001 Fall;23(1):161–178. [PMC free article] [PubMed] [Google Scholar]
- Sing M, Selden T, Banthin J. Using MEPS Expenditure Data for Policy Simulation Studies. Agency for Healthcare Research and Quality; 2007. Working paper, forthcoming. [Google Scholar]
- Smith C, Cowan C, Heffler S, et al. National Health Expenditures in 2004: Recent Slowdown Led by Prescription Drug Spending. Health Affairs. 2006 Jan-Feb;25(1):186–196. doi: 10.1377/hlthaff.25.1.186. [DOI] [PubMed] [Google Scholar]
- Spillman B, Black K. The Size of the Long-Term Care Population in Residential Care: A Review of Estimates and Methodology. U.S. Department of Health and Human Services; Washington, DC.: Feb, 2005. Office of Disability, Aging, and Long-Term Care. [Google Scholar]
- U.S. Census Bureau. U.S. Department of Commerce; 2004a. Economic Census 2002, Health Care and Social Assistance Industry Series. Internet address: http://www.census.gov (Accessed 2006.) [Google Scholar]
- U.S. Census Bureau. U.S. Department of Commerce; Feb, 2004b. Service Annual Survey: 2002, Current Business Reports. Internet address: http://www.census.gov (Accessed 2006.) [Google Scholar]
- Woodwell DA, Cherry DK. Centers for Disease Control and Prevention, National Center for Health Statistics; Aug 26, 2004. National Ambulatory Medical Care Survey: 2002 Summary. Advance Data from Vital and Health Statistics, Number 346. Internet address: http://www.cdc.gov/nchs/about/major/ahcd/ahcd1.htm (Accessed 2006.) [Google Scholar]
- Zuvekas S, Cohen J, Pylypchuk Y. Comparison of MEPS and MarketScan Health Care Expenditure Estimates. Internal Agency for Healthcare Research and Quality memorandum; Rockville, MD.: Fall. 2005. [Google Scholar]
- Zuvekas S, Hill S. Does Capitation Matter? Impacts on Access, Use, and Quality. Inquiry. 2004 Fall;41(3):316–335. [PubMed] [Google Scholar]