Abstract
This article examines the investment of patient care information technology (IT) systems by a nationwide sample of U.S. short-term acute care hospitals and the resulting impact these systems have in the productivity of institutions from 1990-1998. Of particular interest is the extent to which for-profit and not-for-profit hospitals obtain different results from the adoption of IT systems. We find that the marginal effect of IT on for-profit hospital productivity is to reduce the number of days supplied, while in not-for-profit hospitals the marginal effect of IT is to increase the quantity of services supplied. This resulting effect is consistent with the differing objectives of not-for-profit and for-profit hospitals and demonstrates the positive marginal value of IT as a sustainable and prudent investment.
Introduction
In recent years, policymakers, insurers, reform coalitions, such as The Leapfrog Group, and the Institute of Medicine (IOM) have advocated for greater use of clinical IT to improve the quality and efficiency of medical care (Institute of Medicine, 2001). In 2004, The Office of the National Coordinator (ONC) of Health Information Technology (HIT) was formed as the result of an Executive order from the President. This office is now pursuing an aggressive policy agenda to establish a national interoperable health information infrastructure. Since 2004, ONC has sponsored a national dialogue by industry leaders on value of HIT as a key enabler reformed, high-performance health economy. The empirical evidence cited by ONC supporting action was drawn by reported clinical and financial successes from local or firm-specific HIT initiatives. Additional evidence framed the need for HIT as a solution to the patient safety problem (Institute of Medicine, 1999). Furthermore, the use of computerized patient order entry systems was advocated by the IOM (2001) as a HIT solution to directly improve quality of care and patient safety. More recently, studies have speculated on the potential cost savings as hundred of billions of dollars over several years (Hillestad et al., 2005).
Despite a lot of speculation about the utility of IT investments, there is a shortage of studies that demonstrate what the payback from IT investments is. And while the results from the existing studies mentioned by IOM and ONC have proved compelling, they have not utilized a national panel of providers to demonstrate the value of HIT investments. In this study, we utilize nearly a decade of data (1990-1998) and several national data sources to provide the first evidence of the marginal value of hospital IT investment. Specifically, we investigate whether hospital IT investments meet the underlying, but different, economic goals of for-profit and not-for-profit hospitals. To meet their goals, we would expect the marginal effect of IT on for-profit hospital productivity is to reduce the number of days supplied, while in not-for-profit hospitals the marginal effect of IT is to increase the quantity of services supplied. If hospitals' IT investments have met their objectives, then future calls for expensive IT investments will be far more compelling and sustainable over time.
Background
Earlier empirical studies have examined the potential return on investment from implementing clinical IT systems. Lee and Wan (2002) used structural equation modeling to examine the relationships among clinical integration, efficiency, and patient outcomes for a sample of 358 U.S. hospitals. IT represents one of four identified dimensions of clinical integration and is measured as the number of applications in each of the administrative, management, and clinical functional areas. The source of the IT data is the Dorenfest IHDS+Database™. The authors looked at deaths for hysterectomy, spinal fusion, cholecystectomy, transurethral prostatectomy, hip replacement, and knee replacement. Additionally, nine surgical complication types after major surgery were aggregated. The authors found a positive relationship between structural clinical integration and average total charge; a positive relationship between average total charge and the complication ratio; a positive relationship between hospital size and clinical integration; and a positive relationship between health maintenance organization penetration and average total charges.
Burke et al. (2002) provided a descriptive analysis to understand the organizational factors associated with hospital adoption of IT for clinical, administrative, and strategic purposes. They found that hospital size, urban location, and being located in more competitive markets were positively associated with higher adoption rates overall. Borzekowski (2003) examined the influence of health care finance on the adoption of hospital information systems during the 1970s and 1980s, specifically focusing on the effect of Medicare's prospective payment system (PPS), State-level policies, and general market conditions. He found that larger hospitals were fastest to adopt, indicating economies of scale, and rural hospitals were slower to adopt. He also found little effect of health maintenance organization penetration and certificate of need regulation on IT adoption.
Conceptual Model of Hospital IT Investment
We assume that for-profit hospitals attempt to maximize their profits and returns to shareholders, while not-for-profit hospitals attempt to maximize some combination of quantity and quality of their services subject to a constraint that retained earnings be positive. They operate in local hospital markets that are oligopolistic, meaning there are few competitors, hospitals have some latitude to set prices for private payors, and their decisions directly affect the fortunes of their competitors. In this environment, hospitals (irrespective of profit status) try to gain a competitive advantage in the marketplace by having lower costs or by offering a product that is differentiated in the minds of purchasers so that it can be sold at a premium, or attract more customers at any given price.
Brynjolfsson and Hitt (1996;1998) argue that IT, in general, will affect a firm's productivity and profitability (Hitt and Brynjolfsson, 1997). IT investments, such as electronic accounting systems to replace paper-based ledgers, or barcoding products as opposed to manually writing down patient tracking information will yield labor savings for any industry. IT will improve profits if the firm operates in an industry with high barriers to entry, such as the U.S. hospital industry. Even before the advent of the digital age, Arrow (1963) noted the knowledge information asymmetry between provider and non-provider as a barrier to entry. Improved HIT can provide the information to address the information asymmetry problem Arrow discussed. In particular, new innovations from HIT can improve consumer access to medical provider quality, price, and technology effectiveness information.
From the perspective of the provider, the general model of a firm's IT investment objectives of increased profitability, most likely through efficiency gains, and productivity, can apply to hospitals. For example, if IT can lower the cost of treating a hospitalized patient for the same reimbursement price through prospective payment, a more profitable admission will result. The preceding example illustrates the cost-minimizing side of improving profitability. Increases in revenue driven by advertising or overly enthusiastic referral practices for inpatient care, using the same cost structure, can also yield higher profitability.
With respect to productivity, IT investments in computerized order entry could decrease nursing staff time related to administrative tasks, thus increasing time for clinical tasks. Technologies designed to reduce paperwork and redundant processes can help reduce the amount of down time between diagnostic testing and the interpretation of test results in order to proceed to the next step in a care process. These technologies can increase the overall clinical capacity of a hospital. The end result could be increased inpatient volume, assuming no decrease in the demand for hospital admissions.
For-Profit Gains from HIT
The U.S. market of short-term acute care hospitals is made up of for-profit and not-for-profit hospitals. Not-for-profit hospitals have over an 80 percent majority of hospital market share. While it is assumed that for-profit hospitals maximize profits, the objectives of not-for-profit or public hospitals are not as clear to economists (Newhouse, 1970; Pauly and Redisch, 1973; Philipson and Lakdawalla, 2001; Sloan, 1998). We assume for-profit hospitals seek to return their residual surplus at the end of the year to the investors of the hospital. Further, we assume not-for-profit hospitals return their residual surplus to the community in which they operate by providing more services to patients. The differing objectives of for-profit and not-for-profit hospitals provide an opportunity to test whether expensive IT investments fit the goals of these two types of institutions.
By maximizing profits, we assume for-profit hospitals invest in HIT also to minimize their costs of production. We apply the assumption of the duality between profit-maximizing and cost-minimizing behavior. Under some conditions, the production, cost, and profit functions have been shown to be dual to each others, particularly in competitive markets. Cost minimizing behavior can be manifested in a reduction in average length of stay (LOS) when reimbursed through a PPS, such as the commonly applied diagnosis-related group payment reimbursement mechanism used by Medicare and several private insurers. We assume that not-for-profit hospitals invest in IT to minimize costs in order to see more patients and thus better meet their mission to serve through higher patient admission volume. We use this conceptual framework for our empirical analysis of the relationship between IT investment and hospital financial performance.
There are several practical ways IT systems can affect a hospital's production and costs. First, these systems can reduce time lags with respect to patient care. For example, an admitted patient could wait hours, if not overnight, for results before the next action is taken. Electronic messaging of laboratory results would accelerate the process. Second, HIT can reduce probability of adverse events and their associated costs as documented by the two IOM studies on patient safety. Third, HIT can reduce unnecessary resource use by providers. Finally, the technology could increase probability of substitution of IT for labor inputs.
HIT Tenure Effects
Computers and their related databases and decision-support algorithms alone can not make a patient better. IT investments need to be coupled with clinical and administrative staff practices within a hospital to produce a return on investment. This may mean a change in work processes for hospital staff that become more efficient because they are IT enabled. Changes in work processes typically take time to execute. For this reason, we believe that IT investments must be measured over time and that the tenure of an IT investment at a hospital must be considered. As a result, we propose that those hospitals with more years of experience with IT will be more likely to yield a positive return on investment. This specification can be supported by the recent growth in change management services. Stated simply, HIT can be imposed at a hospital by command. It takes time for the system to be trusted and adopted. Increasingly, change management has arrived as a new consulting practice for any hospital to encourage HIT adoption by having IT champions working directly with medical providers to facilitate a change in work flow and processes (Schoenman et al., 2006). During our decade earlier study period, champions were also necessary to implement HIT and the process took time. As a result, the IT tenure variable really represents an IT exposure variable and perhaps a time of survival if the champion tried for several years and then failed.
Data and Methods
Data from two sources contributed to this study, the Healthcare Information and Management Systems Society (HIMSS) HIMSS/Dorenfest database™ and the Medicare cost reports. The HIMSS/Dorenfest Database™ provides information on IT investments of approximately 3,000 U.S. hospitals annually. The hospitals surveyed account for most general hospitals with greater than 100 beds as of 1986. For this study, 1990-1998 HIMSS/Dorenfest Database™ data were used. Included in the database is a list of the type of HIT applications as well as the vendor providing the application (if it is not home grown). We restricted our attention for the purposes of this analysis to patient care systems.
Using a Medicare institutional provider database with address information, we were able to match 2,781 hospitals in the HIMSS/Dorenfest Database™. We matched on ZIP Code, name, and street address (when necessary). To account for the impact of hospital mergers and closures we used data developed by Connor and colleagues (1998), to match hospitals that had merged and either flag them for further analysis or eliminate them from the sample. Our match rate was not uniform throughout the Nation. Our best match rates were with hospitals east of the Mississippi and on the west coast. The HIMSS/Dorenfest Database™ identified the major types of information systems purchases by hospitals. We chose to focus on patient care systems and ignore financial reporting systems and personnel system, both of which were very common IT investments during this period when we examine adoption rates.
Patient care systems are the largest and most significant types of systems in which a hospital may invest. Clinical IT systems are designed to support the delivery of patient care and can be broadly grouped according to their applications, including medical records, decision support, ancillary, and nursing applications. From the HIMSS/Dorenfest Databases™, we identified the presence of master patient indices, clinical decision support systems, computerized physician order entry (CPOE) systems, pharmacy and laboratory systems, and electronic medical records as investments in clinical IT.1 Although this is a much broader definition of clinical IT than used by other groups, such as the Leapfrog Group, these investments do provide the foundation for enhanced IT-enabled work processes. For example, the CPOE systems advocated by the Leapfrog Group rely on the more primitive master patient indexing system so that one common identifier is used to follow a patient throughout their stay for billing and clinical data collection. For this analysis we construct two measures: (1) whether a hospital has the clinical IT system in a given year, and (2) the total number of years the IT system has been in place.
Following the creation of common linking Medicare hospital identification variable, we combined the HIMSS/Dorenfest Database™ data with the Medicare cost report data to create a 9-year panel of data. The cost reports provide detailed annual financial performance and operating characteristics of the hospitals. Approximately 70 percent of available hospitals from the HIMSS/Dorenfest Database™ could be matched successfully with the Medicare cost report information. We further restricted our sample to include hospitals for which we have a complete 9-year series of data and dropped hospitals that closed or ceased their Medicare certification between 1990 and 1998. We further limited our sample to short-term, acute care, nongovernment hospitals with greater than 50 beds. Typically, a hospital with less than 50 beds could not afford a clinical information system unless it was part of a chain of hospitals. In addition, hospitals in the sample had to have operating earnings between a positive and negative $50 million and a return on asset (ROA) ratio from operations between -0.5 and 0.5. We made these financial restrictions to eliminate outliers from our sample who likely had issues affecting their financial performance other than HIT. From the Medicare cost data we focused on two key annual outcome variables: inpatient bed days and the number of discharges.
To identify the marginal value of HIT, we used a multivariate statistical analysis and an economic production function structure. Specifically, we used a translog production function. This form of production function was estimated for both total inpatient days as well as total discharges, and was estimated separately for both for-profit and not-for-profit hospitals. These specifications are most akin to the translog production functions of Jensen and Morrisey (1986). The objective here was to evaluate the full impact of IT on hospital production, allowing for the complementary and substitute effects IT may have for labor and hospital capacity. We computed the total marginal effect of IT by taking the derivative of the production function with respect to IT tenure and computing the effect at the mean value of the covariates considered. Our approach is similar to that of Menon and Lee (2000) who focused on hospitals in Washington from 1976-1994 to estimate a translog cost function. The inputs to their production function are medical labor, medical capital, IT labor, and IT capital. They are focused on the impact of prospective payment in 1983 on production, to examine the substitution and complementarity effects of IT with labor.
There are several other econometric specification issues we needed to address. First, there are repeated measures from the same hospitals over time (the 9 years we have in our data). As a consequence, the standard errors of the parameter estimates needed to be estimated in a way that accounts for this lack of independence. To do this, we employed a hospital fixed approach. This also provided a control for long-term case-mix difference between hospitals based on location and medical staffing, both of which are long-term factors. A time dummy variable is used to control for differences in annual financial incentives from different private and public insurer initiatives (e.g., managed care growth, and the 1998 Balanced Budget Act). This fixed-effects translog model has been used extensively in previous studies (Granneman, Brown, and Pauly 1986; Bamezai et al., 1999; Zwanziger, Melnick, and Bamezai, 2000). To the extent that the unobserved characteristics in the provider market remain stable over time, the hospital fixed-effects model would eliminate this potential selection bias.
Second, we are concerned about functional form issues. It is well known that patient bed days tend to be positively skewed, rather than normally distributed. As such, transformation of the dependent variable by taking the natural log is appropriate. In our empirical analysis, we also tested for the presence of non-linear relationships between our explanatory variables and LOS, as well as for the presence of interaction effects between explanatory variables. We found IT was not the only interaction effect of interest, but since it was our focus, only IT interaction effects were used in the regressions in order to calculate the marginal effect on IT.
Third, the data may not be identically distributed. The hospitals in our data are of widely varying sizes and attributes. It is therefore likely that the errors are also heteroskedastic. We formally tested for the presence of heteroskedasticity using White's test, and correct for it using White's correction (StataCorp LP, 2003) for heteroskedasticity of unknown form. We found that the model could be improved if we developed a more complete production function with additional patient attributes as well, but at this time could not empirically test that model without complementary inpatient data for all hospitals in our sample from 1990-1998.
Consistent with organizational objectives, we would expect for-profit hospitals to minimize LOS and not-for-profit hospitals to maximize patient volume. These outcome measures are the end result of a hospital's production capacity. HIT is proposed as the enabler to reach these objectives, with HIT enabling increases in a hospital's potential medical care production.
The hospitals' production inputs includes hospital beds to represent non-IT capital inputs and full time employees (FTE) for labor inputs. We introduce a linear time trend variable to account for underlying macroeconomic changes in the hospital markets that could affect financial performance (e.g., widespread growth of managed care plans in the 1990s). IT investment is measured as IT tenure representing the number of years of clinical IT investment, and IT tenure was interacted with capital and labor inputs. Since we suspected the relationships between capital and labor to be non-linear, we used squared terms for their inputs. In summary, this specification provides an empirical approach to measure the marginal effect of IT. Economists will recognize that this is clearly a reduced form estimation which does not incorporate other important dimensions of hospital inputs and organizational attributes. Our goal was to complete this early stage analysis and then use the insights provided to develop a formal structural model of production for future analyses.
Table 1 provides a set of descriptive statistics for the attributes, as well as outcome measures, for the hospitals included in our analysis. For-profit and not-for-profit hospitals have some significant differences. Not-for-profit hospitals were larger in terms of beds, FTEs, total assets and patient volume. For-profit hospitals displayed better financial performance, and lower LOS. Interestingly, both types of hospitals had similar median costs per day and per admission.
Table 1. Descriptive Statistics for Type of Hospital, by Variables and Outcome Measures: 1990-1998.
| Variable | Hospital | |||
|---|---|---|---|---|
|
| ||||
| Not-for-Profit | For-Profit | |||
|
|
|
|||
| Mean | Median | Mean | Median | |
| Observations | 7,688 | 7,688 | 1,513 | 1,513 |
| Percent with Patient Care IT System | 0.70 | 1.00 | 0.66 | 1.00 |
| Mean IT Tenure | 2.96 | 2.00 | 2.88 | 2.00 |
| Total Inpatient Days | 52,894 | 41,603 | 34,586 | 26,883 |
| Total Hospital Discharges | 9,485 | 7,832 | 6,637 | 5,402 |
| Total Beds | 247 | 211 | 208 | 172 |
| Total Assets | 104,061,117 | 69,189,243 | 55,102,656 | 40,939,255 |
| Length of Stay | 5.73 | 5.25 | 5.27 | 5.04 |
| Medicaid Percentage | 0.09 | 0.08 | 0.1 | 0.07 |
| Medicare Percentage | 0.45 | 0.46 | 0.43 | 0.43 |
| Case-Mix Adjustment Cost Per Day | 3,086 | 1,103 | 1,208 | 1,121 |
| Case-Mix Adjustment Cost Per Admission | 8,225 | 5,839 | 6,024 | 5,577 |
| Return on Asset from Operations | 0.00 | 0.00 | 0.07 | 0.07 |
NOTES: The information technology (IT) system variables are obtained from the HIMSS/Dorenfest™ Database annual survey of hospital IT. All other variables are computed from the Medicare Cost Reports for 1990-1998.
SOURCE: Parente, S.T., University of Minnesota, Van Horn, R.L., Vanderbilt University, 2006.
Results
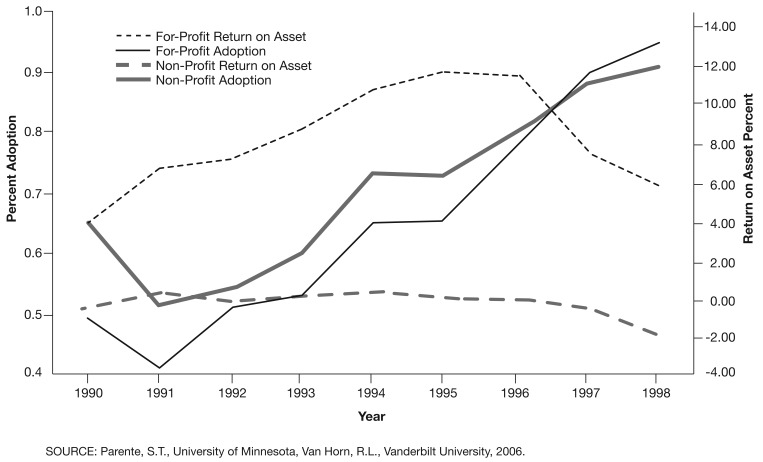
Figure 1 presents the adoption curve for IT systems by for-profit and not-for-profit hospitals along with a plot of the mean ROA by hospital type. Throughout most of the study period the percentage of not-for-profit hospitals with the patient care IT system was greater than in the for-profit hospitals. Clearly, not-for-profit hospitals appear to be early adopters of the technology. It is also noteworthy that at this very general level there does not appear to be a relation between the financial performance of the hospital and adoption of the IT system. Throughout most of the 1990s, not-for-profit hospitals had negative operating ROA, yet they invested in these expensive IT systems. It is noteworthy that both not-for-profit and for-profit hospital financial performance suffers materially from 1997 onward, largely the result of the 1997 Balanced Budget Act.
Figure 1. Time Series Cumulative Adoption of Patient Care Information Technology Systems, by Hospital Type: 1990-1998.
To better understand the factors affecting the adoption of the IT systems by these hospitals, we performed a logistic regression of adoption on organizational attributes. The results (Table 2) suggest that for-profit hospitals are less likely to have an IT system, and when they do, it is positively influenced by the financial position of the hospital. Not-for-profit hospitals, on the other hand, are more likely to have an IT system, to adopt the system earlier (negative coefficient on the time trend), and are more likely to make the investment when they have poor financial performance. FTE employees per hospital bed (a crude measure of efficiency) were not related to whether the IT system was purchased. Hospitals which had a higher case mix were more likely to invest in IT. Although the explanatory power of the logistic regression was fairly low, these results largely confirm what is depicted in Figure 1, and provide some insight into the relationship between IT adoption and financial performance.
Table 2. Logistic Regression of Information Technology (IT) Adoption.
| Variable | Parameter | t-Statistic |
|---|---|---|
| Intercept | 0.041 (0.393) |
0.105 |
| For-Profit Dummy | -2.476 (0.472) |
5.250 |
| Operating Return on Assets | -1.874 (0.618) |
3.031 |
| For-Profit Operating Return on Assets | 2.139 (0.903) |
2.369 |
| Full-Time Equivalent per Hospital Bed | -0.001 (0.005) |
0.296 |
| Time Trend | -0.262 (0.024) |
9.287 |
| For-Profit Time Trend | 0.262 (0.052) |
5.078 |
| Medicaid Percentage | -2.807 (0.540) |
5.201 |
| Medicare Percentage | -0.624 (0.340) |
1.833 |
| Medicare Case-Mix Index | 1.269 (0.176) |
7.221 |
| Pseudo R2 | 0.056 | — |
| Observations | 3,494 | — |
| Events | 1,077 | — |
NOTES: The dependent variable is equal to 1 if the hospital in a given year had a newly acquired patient care IT system and zero in the preceding years. All hospital years after adoption have been removed. The IT variable is obtained from the HIMSS/Dorenfest™ Database data, all other variables are obtained from the Medicare Cost Report data for 1990-1998. Standard errors are in parentheses.
SOURCE: Parente, S.T., University of Minnesota, Van Horn, R.L., Vanderbilt University, 2006.
Table 3 shows the results of an estimation of the marginal value of IT using production function estimation for for-profit and not-for-profit hospitals. The marginal effect of health IT is quite different between not-for-profit and for-profit hospitals. IT increases the discharges of not-for-profit hospitals by a statistically significant 0.6 percent, which is consistent with their functional objective to maximize the volume of services provided within a community. For for-profit hospitals, IT has a statistically significant negative effect on the number of patient bed days and the costs associated with staffing beds for those days. Specifically, the marginal value of 1 year of IT is associated with a 1.1-percent reduction in patient bed days. Given the economic duality of cost-minimization and profit-maximization, these results suggest for-profit hospitals are maximizing profits by using IT to reduce inpatient days, holding constant their labor and capital capacity. This response is effectively equivalent to for-profit hospitals minimizing LOS which, given a largely PPS for hospital reimbursement, is a cost-minimizing behavior. Alternatively, the marginal value of IT has no significant effect on the LOS for not-for-profit hospitals or the volume of admissions within for profit hospitals.
Table 3. Translog Production Functions Estimated for Total Inpatient Hospital Days and Total Hospital Discharges Separately for Not-for-Profit and For-Profit Hospitals: 1990-1998.
| Variable | Hospital | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Not-for-Profit | For-Profit | |||||||
|
|
|
|||||||
| Log Days | Log Discharges | Log Days | Log Discharges | |||||
|
| ||||||||
| Parameter | t-Statistics | Parameter | t-Statistics | Parameter | t-Statistics | Parameter | t-Statistics | |
| Intercept | 2.4886 (0.178) |
13.97 | -0.7438 (0.183) |
-4.07 | -0.4729 (0.993) |
-0.48 | -0.3246 (1.003) |
-0.32 |
| Time Trend | -0.0333 (0.002) |
-18.16 | -0.0047 (0.002) |
-2.51 | -0.0305 (0.005) |
-5.66 | -0.0024 (0.005) |
-0.44 |
| Log FTE Hospital | 0.4714 (0.069) |
6.79 | 0.7783 (0.071) |
10.91 | 0.6229 (0.434) |
1.44 | 0.6662 (0.438) |
1.52 |
| Log FTE Hospital IT Tenure | -0.2697 (0.021) |
-12.98 | -0.2707 (0.210) |
-12.68 | -0.0852 (0.114) |
-0.75 | -0.0971 (0.115) |
-0.85 |
| Log Hospital Bed | 1.3179 (0.097) |
13.54 | 1.5366 (0.100) |
15.37 | 2.2903 (0.607) |
3.77 | 1.5835 (0.613) |
2.58 |
| Log Hospital Bed IT Tenure | 0.3425 (0.026) |
13.07 | 0.3389 (0.027) |
12.59 | 0.0747 (0.136) |
0.55 | 0.8620 (0.137) |
0.63 |
| Log FTE Hospital ^2 | 0.0641 (0.004) |
15.41 | 0.0621 (0.004) |
14.52 | -0.0654 (0.041) |
-1.61 | -0.1180 (0.041) |
-2.87 |
| Log FTE Hospital ^2 IT Tenure | -0.0092 (0.001) |
-9.78 | -0.0089 (0.001) |
-9.17 | 0.0489 (0.011) |
4.38 | 0.0635 (0.011) |
5.63 |
| Log Hospital Bed ^2 | 0.0376 (0.015) |
2.43 | 0.0325 (0.016) |
2.05 | -0.2643 (0.106) |
-2.50 | -0.2674 (0.107) |
-2.51 |
| Log Hospital Bed ^2 * IT Tenure | -0.0753 (0.005) |
-15.25 | -0.0716 (0.005) |
-14.13 | 0.0514 (0.028) |
1.85 | 0.0678 (0.028) |
2.41 |
| Log FTE Hospital Log Hospital Bed | -0.1582 (0.014) |
-11.27 | -0.2065 (0.014) |
-14.32 | 0.1539 (0.111) |
1.39 | 0.2591 (0.112) |
2.31 |
| Log FTE Hospital Log Hospital Bed IT Tenure | 0.0710 (0.004) |
16.84 | 0.0685 (0.004) |
15.83 | -0.0976 (0.031) |
-3.13 | -0.1280 (0.032) |
-4.07 |
| Marginal Effect of IT | 0.0011 (0.002) |
0.55 | 0.0060 (0.002) |
2.83 | -0.0111 (0.006) |
-1.86 | -0.0005 (0.006) |
-0.09 |
| Observations | 7,682 | 7,681 | — | — | — | — | — | — |
| Adjusted R2 | 0.8839 | 0.8593 | — | — | — | — | — | — |
NOTES: FTE is full-time equivalent. The marginal effect of information technology (IT) is computed as the derivative of the production function with respect to IT. The IT variable employed is the number of years the patient care information system has been in place in the hospital. Standard errors are in parentheses.
SOURCE: Parente, S.T., University of Minnesota, Van Horn, R.L., Vanderbilt University, 2006.
Other relationships between IT investment and hospital labor and capital were also considered. The main effect of IT on the productivity of labor is negative in both for-profit and not-for-profit hospitals. The tenure of the IT system serves to reduce the productivity of labor. Conversely, the marginal effect of IT on hospital capacity is positive in all models, suggesting that IT increases the marginal product of hospital beds.
Discussion
This analysis is the first to identify the marginal value of HIT investment consistent with the hypotheses that for-profit hospitals will invest in IT to maximize profits/minimize costs, and that not-for-profit hospitals will invest in IT systems to maximize volume. These results, obtained by using an estimated production function in a manner consistent with earlier empirical work focused on the hospital industry, could provide a foundation for future examinations.
Our findings contribute to the existing literature on the national valuation of HIT. Previous analyses by Kimberly and Evanisko (1981), Burke et al. (2002), and Borzekowski (2003) focused on the factors contributing to HIT adoption. All three studies found, as do we, that large hospitals are more likely to adopt. However, our analysis also suggests a dynamic relationship between adoption and financial status as well as governance structure. Specifically, we observed a contrary finding when for-profit hospitals, which are typically smaller than not-for-profit hospitals, achieved a more rapid adoption rate of patient care systems in the later 1990s.
A national cross-sectional exploratory analysis by Parente and Dunbar (2001), based on data from a 1993 survey, found clinical information systems were associated with higher total margins, but with no difference in operating margins. These results suggested a reverse causality relationship where wealthier hospitals were more likely to purchase HIT, but the investment in it did not increase their operating margins. Our study improves on this analysis by providing a more recent time series and specifically identifying the inputs that would drive improvements in operational efficiencies needed to have an effect on hospital margins.
Similar to our production analysis approach, Menon and Lee (2000) used data on hospitals in Washington from 1976-1994 to estimate a translog cost function. The inputs to production were medical labor, medical capital, IT labor, and IT capital. Their output measure was also patient days. They focused on the impact of Medicare's prospective payment on production and technical change, as well as measurement of substitution and complementary effects. Similar to our own findings, the authors found that while IT labor expense rose at an increasing rate due to regulatory effects, hospitals were able to achieve some degree of cost containment through IT.
This analysis has three limitations. First, the analysis focuses on a time period prior to the introduction of the Health Insurance Portability and Accountability Act (HIPAA), the IOM reports on patient safety, and The Leapfrog Group initiative. While not the most current period available for study, the finding that clinical IT applications contribute positively to hospital's objectives prior to legislative mandates and highly structured voluntary efforts, such as Leapfrog, should help substantiate the case for investment beyond the argument of “…it's the right thing to do to cross the quality chasm.” Furthermore, our IT tenure results show that the impact of IT may take years to realize. At the very least, our analysis provides a set of pre-HIPAA findings on the value of HIT that will hopefully only increase as the quality and capabilities of IT systems improve through the use of technologies not present in the first half of the 1990s, such as enterprise wide networking and graphical user interfaces (i.e., Microsoft® Windows as opposed to Microsoft® DOS).
Our second limitation is not matching all hospitals between the HIMSS/Dorenfest Database™ and Medicare database. However, we do know which hospitals did not match and can gauge some of the direction of the bias caused by this result. Since the analysis focuses only on hospitals with greater than 100 beds that were financially solvent through the 1990s, it may be that our subset is biased toward larger hospitals better able to invest in HIT. It is unfortunate that our analysis does not consider the recent impact of HIT on smaller rural hospitals where evidence has suggested significant potential returns on IT investment (Schoenman et al., 2006).
A third limitation may be that case mix is absent from the production function. We have deliberately left it out at this stage of the analysis to develop a pure specification of production with only inputs. While case mix could be considered a technology determinant of the hospital, we fear it could be correlated to other inputs in the translog function as currently specified, particularly HIT as seen from the logistic regression analysis.
Even with these limitations, the HIMSS/Dorenfest Database™ is a unique resource that can be refined for future empirical analysis. For example, one major new HIT application will be the use of hospital-wide CPOE systems endorsed by The Leapfrog Group. The HIMSS/Dorenfest Database™ data have the potential to track not only hospital investments in these systems, but also the physician and long-term care affiliates' adoption of CPOE within an integrated delivery hospital system.
One enhancement to our production model specification was to allow for a multidimensional output space including measures of quality, such as mortality. As part of this analysis, we explored using Cobb-Douglas and Data Envelopment Analysis approaches to get a more robust specification of production with varying levels of success. We hope to employ a specification similar to Hofler and Folland's (1995) use of a stochastic frontier estimation to evaluate the efficiency of U.S. hospitals based on visits or admissions in five patient categories taken from the 1985 American Hospital Association Survey. Additional explorations that could provide an opportunity to include case mix will be examined. We also plan to investigate the use of incorporating random effects to account for the correlated error structure.
Our analysis provides evidence to address the business case for investing in new HIT systems within for-profit and not-for-profit hospitals. While we see this analysis as a first step in the path of future analyses, it does present a novel example of where the marginal effect of a common technology adoption in hospitals and the corresponding effect on productivity were considered. The finding that for-profit and not-for-profit hospitals successfully maximize their production objectives, though in different ways, should focus investment decisions of hospital managers and enable them to make the case that higher quality or HIPAA-compliance will be achieved, as well as improved financial performance.
Acknowledgments
The authors wish to thank William Vogt, Jim Burgess, Jon Christianson, Ruth Taylor, Jean Abraham, Martin Gaynor, Roger Feldman, and Lisa Schloff for comments on earlier drafts of the article. We would also like to thank Sanjog Misra for his econometrics expertise.
Footnotes
Stephen T. Parente is with the University of Minnesota. R. Lawrence Van Horn is with Vanderbilt University. The research in this article was supported by the University of Minnesota. The statements expressed in this article are those of the authors and do not necessarily reflect the views or policies of the University of Minnesota, Vanderbilt University, or the Centers for Medicare & Medicaid Services (CMS).
In some instances hospitals would adopt a system and then abandon it. We recorded in the data the presence of systems year by year for our analysis. This way, the greater the exposure to the system the greater the marginal effect of HIT on hospital performance.
Reprint Requests: Stephen T. Parente, Ph.D., Department of Finance, Medical Industry Leadership Institute, Carlson School of Management, 321 19th Avenue South, Room 3-279, Minneapolis, MN 55455. E-mail:sparente@csom.umn.edu
References
- Arrow K. Uncertainty and the Welfare Economics of Medical Care. American Economic Review. 1963;53:941–973. [Google Scholar]
- Bamezai A, Zwanziger J, Melnick G. Price Competition and Hospital Cost Growth in the United States (1989-1994) Health Economics. 1999 May;8(3):233–245. doi: 10.1002/(sici)1099-1050(199905)8:3<233::aid-hec406>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- Brynjolfsson E, Hitt LM. Beyond the Productivity Paradox. Communications of the ACM. 1998 Aug;41(8):49–55. [Google Scholar]
- Brynjolfsson E, Hitt LM. Paradox Lost? Firm-Level Evidence on the Returns to Information Systems. Management Science. 1996 Apr;42(4):541–558. [Google Scholar]
- Burke D, Wang B, Wan T, et al. Exploring Hospitals' Adoption of Information Technology. Journal of Medical Systems. 2002;26(4):349–355. doi: 10.1023/a:1015872805768. [DOI] [PubMed] [Google Scholar]
- Borzekowski R. Measuring the Cost Impact of Hospital Information Systems: 1987-1994. Board of Governors of the Federal Reserve System; Washington, DC.: 2003. Finance and Economics Discussion Series 2002-2042. [Google Scholar]
- Connor R, Feldman R, Dowd B. The Effects of Market Concentration and Horizontal Mergers on Hospital Costs and Prices. International Journal of the Economics of Business. 1998 Jul;5(2):159–180. [Google Scholar]
- Granneman T, Brown R, Pauly M. Estimating Hospital Costs: A Multiple-Output Analysis. Journal of Health Economics. 1986;5:107–127. doi: 10.1016/0167-6296(86)90001-9. [DOI] [PubMed] [Google Scholar]
- Hillestad R, Bigelow J, Bower A, et al. Can Electronic Medical Record Systems Transform Health Care? Potential Health Benefits, Savings, and Costs. Health Affairs. 2005 Sep-Oct;24(5):1103–1117. doi: 10.1377/hlthaff.24.5.1103. [DOI] [PubMed] [Google Scholar]
- Hitt LM, Brynjolfsson E. Information Technology and Internal Firm Organization: An Exploratory Analysis. Journal of Management Information Systems. 1997 Fall;14(2):81–101. [Google Scholar]
- Hofler RA, Folland ST. On the Technical and Allocative Efficiency of United States Hospitals: A Stochastic Frontier Approach. 1995. Working Paper. [Google Scholar]
- Institute of Medicine. To Err is Human. National Academy of Science Press; Washington, DC.: 1999. [Google Scholar]
- Institute of Medicine. Crossing the Quality Chasm. National Academy of Science Press; Washington, DC.: 2001. [Google Scholar]
- Jensen G, Morrisey M. The Role of Physicians in Hospital Production. The Review of Economics and Statistics. 1986;68(3):432–442. [Google Scholar]
- Kimberly JR, Evanisko MJ. Organizational Innovation: The Influence of Individual, Organizational, and Contextual Factors on Hospital Adoption of Technological and Administrative Innovations. Academy of Management Journal. 1981;24(4):689–713. [PubMed] [Google Scholar]
- Lee K, Wan T. Effects of Hospitals' Structural Clinical Integration on Efficiency and Patient Outcome. Health Services Management Research. 2002 Nov;15(4):234–244. doi: 10.1258/095148402320589037. [DOI] [PubMed] [Google Scholar]
- Menon NM, Lee B. Productivity and Efficiency of Information Systems in the Healthcare Industry. Information Systems Research. 2000;11(1):83–92. [Google Scholar]
- Newhouse J. Toward a Theory of Nonprofit Institutions: An Economic Model of a Hospital. The American Economic Review. 1970;60(1/2):64–74. [Google Scholar]
- Parente ST, Dunbar JL. Is Health Information Technology Investment Related to the Financial Performance of U.S. Hospitals? An Exploratory Analysis. International Journal of Healthcare Technology and Management. 2001;3(1):48–58. [Google Scholar]
- Pauly M, Redisch M. The Not-for-Profit Hospital as a Physician's Cooperative. The American Economic Review. 1973 Mar;63(1):87–99. [Google Scholar]
- Philipson T, Lakdawalla D. Medical Care Output and Productivity in the Nonprofit Sector. In: Cutler D, Berndt E, editors. Medical Care Output and Productivity. Vol. 62. University of Chicago Press; Chicago, IL.: 2001. NBER Studies in Income and Wealth. [Google Scholar]
- Schoenman JA, Keeler J, Moiduddin A, et al. Roadmap for the Adoption of Health Information Technology in Rural Communities. NORC Walsh Center for Rural Heath Analysis; Bethesda, MD.: 2006. [Google Scholar]
- StataCorp LP. Stata®8. College Station, TX.: 2003. [Google Scholar]
- Sloan F Commercialism in Nonprofit Hospitals. In: To Profit or Not to Profit: The Commercial Transformation of the Nonprofit Sector. Weisbrod B, editor. Cambridge University Press; Cambridge, England: 1998. [Google Scholar]
- Zwanziger J, Melnick GA, Bamezai A. The Effect of Selective Contracting on Hospital Costs and Revenues. Health Services Research. 2000;35(4):849–867. [PMC free article] [PubMed] [Google Scholar]