Abstract
The potentially preventable readmission (PPR) method uses administrative data to identify hospital readmissions that may indicate problems with quality of care. The PPR logic determines whether the reason for readmission is clinically related to a prior admission, and therefore potentially preventable. The likelihood of a PPR was found to be dependent on severity of illness, extremes of age, and the presence of mental health diagnoses. Analyses using PPRs show that readmission rates increase with increasing severity of illness and increasing time between admission and readmission, vary by the type of prior admission, and are stable within hospitals over time.
Introduction
Hospital readmission rates have been proposed as an important indicator of quality of care (Friedman and Basu, 2004; Miller, 2007) because they may result from actions taken or omitted during the initial hospital stay. A readmission may result from incomplete treatment or poor care of the underlying problem, or may reflect poor coordination of services at the time of discharge and afterwards, such as incomplete discharge planning and/or inadequate access to care (Halfon et al., 2006; Kripalani et al., 2007). Readmissions are important not only as quality screens, but also because they are expensive, consuming a disproportionate share of expenditures for inpatient hospital care (Anderson and Steinberg, 1984). Readmissions can therefore focus attention on the critical time of an acute illness when the patient is in transition between inpatient and outpatient phases of treatment.
Another advantage is that, like measures such as mortality rates and complication rates, readmission rates can be generated from administrative data, and can therefore serve to screen large numbers of records and provide a basis for comparing hospital performance.
Several studies have documented the relationship between readmissions and quality of care. Ashton et al. (1997) concluded that an early readmission is significantly associated with the process of inpatient care and found that patients who were readmitted were roughly 55 percent more likely to have had a quality of care problem. Hannon et al. (2003) found that 85 percent of readmissions following coronary bypass surgery were associated with complications directly related to the bypass surgery.
The analysis of hospital readmissions is complicated by the fact that not all readmissions are preventable, even with optimal care. If readmission rates are to serve as a useful indicator of hospital quality and performance, it is necessary to identify those readmissions that are potentially preventable based on credible clinical criteria. This article addresses these challenges and describes a method for identifying potentially preventable hospital readmissions using computerized discharge abstract data.
Methods
The concept of a potentially preventable readmission was defined and a determination of which types of admissions were at risk of generating a readmission was made. A method for judging preventability was developed based on the relationship between the reason for the original admission and the reason for the readmission, and various factors that influenced the probability of occurrence of a preventable readmission were examined.
A readmission is considered to be clinically related to a prior admission and potentially preventable if there was a reasonable expectation that it could have been prevented by one or more of the following: (1) the provision of quality care in the initial hospitalization, (2) adequate discharge planning, (3) adequate postdischarge followup, or (4) improved coordination between inpatient and outpatient health care teams.
A readmission is defined as a return hospitalization to an acute care hospital that follows a prior acute care admission within a specified time interval, called the readmission time interval. The readmission time interval is the maximum number of days allowed between the discharge date of a prior admission and the admitting date of a subsequent admission.
If a subsequent admission occurs within the readmission time interval and is clinically related to a prior admission, it is considered a PPR. The hospitalization preceding a PPR is called an initial admission. Subsequent PPRs relate back to the care rendered during or following the initial admission.
Readmission chains are defined as sequences of one or more PPRs that are all clinically related to the same initial admission. In calculating PPR rates, readmission chains rather than individual readmissions were used as the numerator.
Stand alone admissions are defined as admissions that have neither a proceeding clinically related admission within the readmission time interval nor a subsequent clinically related admission within the readmission time interval. Candidate admissions are the combination of the stand alone admissions and the initial admissions and represent all admissions that are at risk of having a readmission occur. Candidate admissions are used as the denominator in calculating readmission rates.
Admissions that do not meet certain eligibility criteria are excluded from consideration as a PPR or candidate admission. Three types of exclusion criteria were identified: (1) admissions associated with major or metastatic malignancies, multiple trauma, burns, and certain chronic conditions such as cystic fibrosis, for which subsequent readmissions are often either not preventable or are expected to require significant followup care; (2) neonatal and obstetrical admissions and admissions for eye care, which have unique followup care requirements and only rarely are followed by related readmissions; and (3) admissions with a discharge status of “left against medical advice” because the intended care could not be completed. These excluded admissions are not eligible to be a PPR or a candidate admission and are not included in the calculation of readmission rates. Admissions with a discharge status of “transferred to another acute care hospital” can be a PPR, but are excluded as candidate admissions because under these circumstances the hospital has limited influence on the patient's subsequent care. Similarly, admissions with a discharge status of died can be a PPR, but are excluded as candidate admissions because the patient can obviously never be readmitted.
Defining PPRs
The selection of the readmission time interval has an important effect on the PPR rate. A longer readmission time interval, 30 versus 15 days for example, will identify more readmissions. Longer time intervals after the initial admission decrease the likelihood that a readmission was related to the clinical care or discharge planning in the initial admission and increase the relative importance of outpatient management of chronic illness (Hannan et al., 2003).
A readmission is considered to be clinically related to the initial admission if it belonged to one of five different categories:
A medical readmission for a continuation or recurrence of the reason for the initial admission, or for a closely related condition (e.g., a readmission for diabetes following an initial admission for diabetes).
A medical readmission for an acute decompensation of a chronic problem that was not the reason for the initial admission, but was plausibly related to care either during or immediately after the initial admission (e.g., a readmission for diabetes in a patient whose initial admission was for an acute myocardial infarction).
A medical readmission for an acute medical complication plausibly related to care during the initial admission (a patient with a hernia repair and a perioperative Foley catheter readmitted for a urinary tract infection 10 days later).
A readmission for a surgical procedure to address a continuation or a recurrence of the problem causing the initial admission (a patient readmitted for an appendectomy following an initial admission for abdominal pain and fever).
A readmission for a surgical procedure to address a complication resulting from care during the initial admission (a readmission for drainage of a post-operative wound abscess following an initial admission for a bowel resection).
A readmission that did not fit one of these categories was classified as a clinically unrelated readmission and therefore, not potentially preventable (i.e., not a PPR).
All Patient Refined Diagnosis Related Groups (APR DRGs) were used to classify patients according to their reason for admission and to establish the existence of a clinical relationship between an initial admission and the readmission (Averill et al., 2002). APR DRGs use data from computerized discharge abstracts to assign patients to 1 of 314 base APR DRGs that are determined either by the principal diagnosis, or, for surgical patients, the most important surgical procedure performed in an operating room.
In order to identify whether there was a clinical relationship between an initial admission and a readmission, a matrix in which there were 314 rows representing the possible base APR DRGs of the initial admission, and 314 columns representing the base APR DRG of the readmission was created. Each of the 98,596 cells in the matrix then represented a unique combination of a specific type of initial admission and readmission. A clinical panel consisting of two general internists and two pediatricians, supplemented as needed by specialists in pediatrics, medicine, obstetrics and surgery, applied the criteria for clinical relevance and preventability to the combination of base APR DRGs in each cell to determine if the base APR DRG of the readmission was clinically related to the base APR DRG of the initial admission. Each of the 98,596 cells went through at least two reviews by the physician panel after the initial classification. Of the 98,596 cells, 32,230 (33 percent) were considered to be clinically related. The categorical nature of the readmission matrix permitted a specification of clinical relationships at a level of precision that would not be possible by other methods such as regression based models.
Calculating a PPR Rate
The PPR rate was calculated using the number of readmission chains as the numerator rather than the total number of PPRs. As previously described, two or more PPRs can all be related to the same prior initial admission in some instances, and will form a readmission chain. If for a given PPR, the preceding admission is itself a PPR, then the most recent readmission is assessed to determine if it is clinically related to the initial admission, rather than to the readmission immediately preceding it. If clinically related, the most recent readmission becomes part of the readmission chain related to the initial admission that started the readmission chain.
In a readmission chain, the total time period encompassed can exceed the specified readmission time interval. For example, if the readmission time interval is 15 days and there are two readmissions each 14 days apart related to the same initial admission, the second readmission is still considered a readmission related to the initial admission even though it occurred 28 days after the initial admission.
The denominator consists of all candidate admissions, including those admissions that occurred within the readmission time interval following a prior admission, but were determined to be clinically unrelated to the initial admission and therefore recategorized as a candidate admission. The PPR rate therefore is the proportion of all candidate admissions that were followed by one or more PPRs.
Risk Adjustment Using APR DRGs
APR DRGs also served to stratify patients according to severity of illness. Each base APR DRG is divided into four severity of illness (SOI) levels, determined primarily by secondary diagnoses that reflect both comorbid illnesses and the severity of the underlying illness, creating the final set of 1,256 groups. APR DRGs SOI levels could then be used to stratify the probability that an initial admission would be followed by a PPR, in order to compare actual and expected readmission rates across hospitals.
Calculating Hospital Expected Readmission Rates
A statewide PPR rate was calculated for each base APR DRG and severity level. Then, using indirect rate standardization, for each APR DRG and SOI level within each hospital, the expected number of PPRs was calculated by multiplying the statewide PPR rate for each APR DRG and SOI level by the number of candidate admissions in the hospital in the corresponding APR DRG and SOI level. The expected number of PPRs overall for the hospital is the expected number of PPRs for each APR DRG and SOI level, summed over all APR DRG and SOI levels. Since a hospital PPR rate can be influenced by its mix of patient types (i.e., base APR DRGs) and patient severity of illness (i.e., SOI level) during the candidate admission, an expected number of PPRs computed in this manner produces a case mix and severity of illness adjusted expected number of PPRs for each hospital. By comparing the actual and expected number of PPRs the variation in readmission patterns across hospitals can be assessed.
Data Sources
From all 249 Florida inpatient hospitals for 2004 and 2005, 5.02 million admissions were analyzed. A total of 634,491 admissions that had not recorded the unique patient identifier, needed to link patients, were eliminated. Another 76,825 admissions were excluded from the analysis because they were treated in non-acute care hospitals (i.e., long-term care and rehabilitation facilities) or had inconsistent data elements, including error APR DRG assignment, age and sex discrepancies, hospitalizations with less than $200 or greater than $4 million in total charges, or admissions with a discharge date that preceded the admission date. A total of 4,311,653 admissions from 234 Florida hospitals remained in the final database used for this analysis.
Results
Computing Readmission Rates
Figure 1 illustrates the process of categorizing the 4,311,653 admissions into candidate admissions and readmissions and computing a PPR rate, using a 15-day readmission time interval for readmissions to any hospital. Of the 3,816,845 candidate admissions, 834,204 were eliminated by one or more of the exclusion criteria. Of the 494,808 readmissions, 80,317 met one or more of the exclusion criteria, and 113,474 were not clinically related to the prior admission. Of the non-clinically related readmissions, 4,732 had a discharge status of died and therefore could not be reclassified as candidate admissions. The remaining 108,742 non-clinically related readmissions were reclassified as candidate admissions resulting in a total of 3,091,383 candidate admissions. There were 301,017 readmissions that were clinically related and therefore designated as PPRs. Among all PPRs, 203,103 belonged to a PPR chain with only a single PPR, while the remaining 97,914 PPRs belonged to 39,888 PPR chains with two or more PPRs, for a total of 242,991 unique PPR chains. The PPR rate, defined as the proportion of candidate admissions that were followed by one or more PPRs was 7.86 percent.
Figure 1. Potentially Preventable Readmission (PPR) Analysis of Florida Data for Readmissions to Any Hospital With a 15-Day Readmission Time Interval.
PPR Characteristics
Table 1 contains overall results of the readmission analysis categorized into three alternative readmission time intervals (i.e., 7, 15, or 30 days), and by whether the readmission was to the same hospital or to any hospital. The number of PPRs and PPR chains increased when readmissions to any hospital were included and also increased as the time interval increased from 7 to 30 days. Subsequent analyses in this article will be based on readmissions to any hospital with a 15-day readmission time interval.
Table 1. Potentially Preventable Readmission (PPR) Rates, by Time Intervals and Whether the Readmission Was to the Same or Any Hospital.
| Readmission Time Interval | Readmission Hospital | Number of PPRs | Number of PPR Chains | PPR Chains as a Percent of Candidate Admissions |
|---|---|---|---|---|
| 7 Days | Same | 137,341 | 125,234 | 3.85 |
| Any | 185,182 | 161,655 | 5.05 | |
| 15 Days | Same | 223,864 | 191,493 | 6.04 |
| Any | 301,017 | 242,991 | 7.86 | |
| 30 Days | Same | 335,024 | 264,119 | 8.62 |
| Any | 444,042 | 326,096 | 11.03 |
NOTE: Number of candidate admissions is 3,091,383.
SOURCE: Florida inpatient hospital data, calendar years 2005-2006.
Table 2 contains the 10 APR DRGs for the medical and surgical candidate admissions with the largest number of PPR chains, by APR DRG severity level. Three of the top 10 medical initial admissions were for APR DRGs related to mental health. The top 10 medical APR DRGs contain 33.4 percent of all candidate admissions and 61.7 percent of all medical PPR chains. The top 10 surgical APR DRGs contain 39.4 percent of candidate admissions and 46.1 percent of surgical PPR chains.
Table 2. Top 10 APR DRGs for Medical and Surgical Candidate Admissions With the Largest Number of Potentially Preventable Readmission (PPR) Chains, by Severity of Illness (SOI) Level.
| APR DRG Number | Medical APR DRG Description | Number of PPR Chains/Rate | All Patients | SOI 1 | SOI 2 | SOI 3 | SOI 4 |
|---|---|---|---|---|---|---|---|
| 194 | Heart Failure | Chains | 15,053 | 1,304 | 8,151 | 4,675 | 923 |
| Rate | 12.5 | 8.9 | 11.7 | 15.0 | 19.4 | ||
| 140 | Chronic Obstructive Lung Disease | Chains | 8,271 | 1,737 | 3,745 | 2,416 | 373 |
| Rate | 9.7 | 7.3 | 9.3 | 12.7 | 17.3 | ||
| 750 | Schizophrenia | Chains | 7,592 | 3,382 | 3,931 | 251 | 28 |
| Rate | 17.7 | 17.1 | 18.1 | 20.8 | 16.8 | ||
| 139 | Other Pneumonia | Chains | 7,579 | 393 | 3,295 | 3,394 | 497 |
| Rate | 7.7 | 2.7 | 6.5 | 11.4 | 16.4 | ||
| 751 | Major Depressive Disorder | Chains | 5,608 | 1,814 | 3,391 | 339 | 64 |
| Rate | 10.9 | 8.3 | 12.6 | 16.5 | 10.8 | ||
| 198 | Angina Pectoris & Coronary Atherosclerosis | Chains | 5,151 | 1,414 | 2,685 | 982 | 70 |
| Rate | 5.6 | 3.7 | 6.2 | 9.9 | 17.3 | ||
| 753 | Bipolar Disorders | Chains | 4,830 | 2,366 | 2,260 | 179 | 25 |
| Rate | 14.0 | 12.7 | 15.3 | 18.8 | 11.6 | ||
| 720 | Septicemia & Disseminated Infection | Chains | 4,370 | 46 | 881 | 1,808 | 1,635 |
| Rate | 12.6 | 3.6 | 8.3 | 12.7 | 19.3 | ||
| 460 | Renal Failure | Chains | 4,288 | 92 | 471 | 3,250 | 475 |
| Rate | 12.8 | 11.0 | 10.6 | 12.5 | 21.1 | ||
| 201 | Cardiac Arrhythmia & Conduction Disturbance | Chains | 4,066 | 898 | 1,950 | 1,070 | 148 |
| Rate | 6.3 | 4.0 | 6.4 | 10.2 | 16.0 | ||
| All Other Medical APR DRGs | Chains | 41,412 | 8,036 | 15,942 | 13,011 | 4,423 | |
| Rate | 2.9 | 1.7 | 2.5 | 5.0 | 9.4 | ||
| Total Medical APR DRG | Chains | 108,220 | 21,482 | 46,702 | 31,375 | 8,661 | |
| Rate | 5.0 | 3.2 | 4.7 | 7.4 | 11.7 | ||
|
| |||||||
| APR DRG Number | Surgical APR DRG Description | Number of PPR Chains/Rate | All Patients | SOI 1 | SOI 2 | SOI 3 | SOI 4 |
|
| |||||||
| 175 | Percutaneous Cardiovascular Procedures Without AMI | Chains | 7,260 | 3,222 | 2,850 | 1,043 | 145 |
| Rate | 7.9 | 6.4 | 9.0 | 12.7 | 14.8 | ||
| 221 | Major Small & Large Bowel Procedures | Chains | 3,426 | 606 | 1,201 | 913 | 706 |
| Rate | 9.4 | 6.0 | 8.3 | 11.1 | 19.5 | ||
| 173 | Other Vascular Procedures | Chains | 3,186 | 627 | 1,140 | 1,075 | 344 |
| Rate | 11.3 | 6.9 | 10.2 | 16.9 | 23.7 | ||
| 174 | Percutaneous Cardiovascular Procedures With AMI | Chains | 3,115 | 791 | 1,288 | 648 | 388 |
| Rate | 9.8 | 6.4 | 10.0 | 14.4 | 18.5 | ||
| 165 | Coronary Bypass With Catheter or Percutaneous Procedure | Chains | 2,638 | 101 | 909 | 1,073 | 555 |
| Rate | 12.3 | 7.2 | 9.3 | 13.9 | 21.5 | ||
| 301 | Hip Joint Replacement | Chains | 2,870 | 1,123 | 1,106 | 445 | 196 |
| Rate | 6.2 | 5.1 | 6.0 | 8.9 | 21.4 | ||
| 308 | Hip/Femur Procedure Except Joint Replacement Due to Trauma | Chains | 2,395 | 234 | 1,115 | 835 | 211 |
| Rate | 8.0 | 4.9 | 6.9 | 10.6 | 19.5 | ||
| 302 | Knee Joint Replacement | Chains | 2,373 | 780 | 1,323 | 233 | 37 |
| Rate | 4.0 | 2.9 | 4.5 | 7.4 | 13.1 | ||
| 161 | Cardiac Defibrillator & Heart Assist Implant | Chains | 2,048 | 113 | 614 | 1,132 | 189 |
| Rate | 9.3 | 4.9 | 7.4 | 11.1 | 16.9 | ||
| 171 | Permanent Cardiac Pacemaker Without AMI, CHF, or Shock | Chains | 2,044 | 523 | 1,068 | 382 | 71 |
| Rate | 8.1 | 5.5 | 8.7 | 12.7 | 19.6 | ||
| All Other Surgical | Chains | 36,608 | 8,940 | 13,142 | 10,196 | 4,330 | |
| Rate | 6.1 | 3.2 | 6.2 | 12.4 | 18.6 | ||
| Total Surgical APR DRG | Chains | 67,963 | 17,060 | 25,756 | 17,975 | 7,172 | |
| Rate | 6.8 | 4.0 | 6.8 | 12.3 | 19.0 | ||
NOTES: APR DRG is All Patiënt Refined Diagnosis Related Group. AMI is acute myocardial infarction. CHF is congestive heart failure. Table shows readmission to any hospital with a 15-day readmission time interval.
SOURCE: Florida inpatient hospital data, calendar years 2005-2006.
The PPR rate increased consistently as the severity level increases. For readmissions to any hospital within 15 days the PPR rate increased more than threefold for medical patients and more than fourfold for surgical patients as severity increases from severity level 1 to 4.
Table 3 contains the top 10 medical and surgical APR DRGs ranked according to their readmission rate rather than numbers of readmissions. The number of readmissions for these APR DRGs tends to much smaller than those in Table 2.
Table 3. Top 10 Medical and Surgical APR DRGs With the Largest Percentage of Potentially Preventable Readmission (PPR) Chains.
| APR DRG | Description | Candidate Admissions | No. of PPR Chains | PPR Rate |
|---|---|---|---|---|
| Total Medical | 2,096,889 | 175,028 | 8.35 | |
| 196 | Cardiac Arrest | 389 | 81 | 20.82 |
| 279 | Hepatic Coma/Other Major Liver Disease | 4,381 | 848 | 19.36 |
| 890 | HIV with Multiple Major HIV Related Conditions | 2,366 | 456 | 19.27 |
| 130 | Mechanical Ventilation 96+ Hours | 6,621 | 1,182 | 17.85 |
| 750 | Schizophrenia | 42,868 | 7,592 | 17.71 |
| 812 | Poisoning Medicinal Agent | 20,618 | 3,628 | 17.60 |
| 892 | HIV with Major HIV Related Condition | 5,820 | 932 | 16.01 |
| 662 | Sickle Cell Anemia Crisis | 10,056 | 1,554 | 15.45 |
| 44 | Intracranial Hemorrhage | 6,941 | 1,053 | 15.17 |
| 280 | Alcoholic Liver Disease | 8,068 | 1,215 | 15.06 |
| All Other Medical | 1,988,761 | 156,487 | 7.87 | |
| Total Surgical | 994,494 | 67,963 | 6.83 | |
| 440 | Kidney Transplant | 1,613 | 332 | 20.58 |
| 740 | Mental Illness Diagnosis With Procedure | 270 | 53 | 19.63 |
| 162 | Cardiac Valve Procedure With Catheterization | 4,953 | 837 | 16.90 |
| 444 | Renal Dialysis Access Procedure Only | 5,352 | 859 | 16.05 |
| 710 | Infectious & Parasitic Diagnosis With Procedure | 5,184 | 829 | 15.99 |
| 405 | Other Procedure—Endocrine/Nutrition/Metabolic Diagnosis | 717 | 114 | 15.90 |
| 260 | Major Pancreas/Liver/Shunt Procedure | 1,843 | 287 | 15.57 |
| 163 | Cardiac Valve Procedure Without Catheter | 7,047 | 1,076 | 15.27 |
| 950 | Extensive Procedure Unrelated Diagnosis | 5,043 | 751 | 14.89 |
| 305 | Amputation Lower Limb Except Toe | 5,898 | 862 | 14.62 |
| All Other Surgical | 956,574 | 61,963 | 6.48 |
NOTES: APR DRG is All Patient Refined Diagnosis Related Groups. Table shows readmission to any hospital with a 15-day readmission time interval.
SOURCE: Florida inpatient hospital data, calendar years 2005-2006.
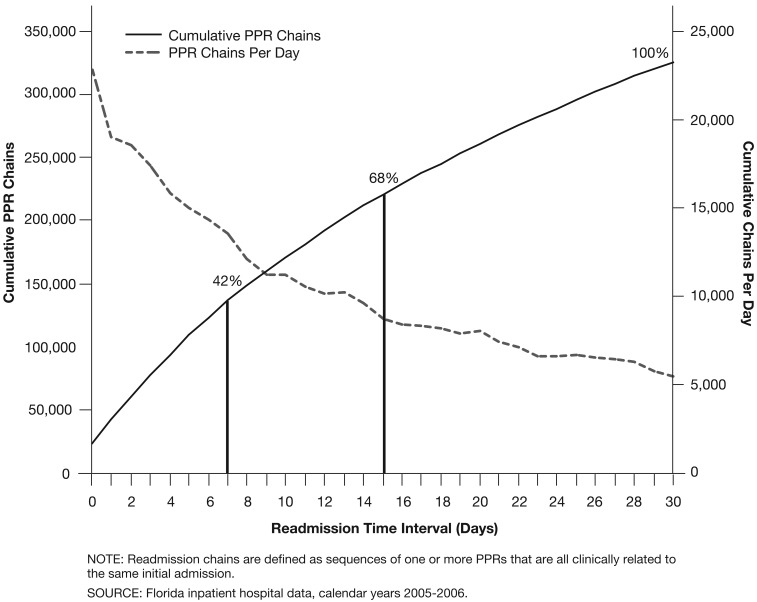
Figure 2 shows the number of PPR chains per day and the cumulative number of PPR chains for the 30 days following the initial admission. The number of the PPR chains per day declined rapidly until about the 10th day and then declined at a slower rate. A readmission time interval of 7 days accounted for 42 percent of the 30-day total number of PPR chains and a readmission interval of 15 days accounted for 68 percent of the 30-day total number of PPR chains.
Figure 2. Number of Potentially Preventable Readmission (PPR) Chains, by Readmission Time Interval up to 30 Days.
The large majority of PPR chains (83.6 percent) had only a single PPR, while 12.2 percent contained two PPRs and 2.7 percent contained three PPRs. Less than one-half of 1 percent of PPR chains had six or more PPRs. The distribution of the number of PPRs in a chain was roughly the same for medical and surgical initial admissions.
Table 4 compares the actual and expected length of stay (LOS) and charges for initial admissions that had a PPR chain. Expected values were calculated for each APR DRG and severity level based on pooled data from both years for all eligible initial admissions. For the subset of initial admissions that had a PPR chain, indirect rate standardization was used to compute the expected average LOS and charge. The actual LOS and charges were higher than expected in initial admissions with a PPR chain by 10.55 percent for LOS and 8.58 percent for charges. Although a possible cause of readmissions could be premature discharge (i.e., quicker and sicker), these results show that initial admissions that were followed by a PPR chain had a longer LOS and increased charges, suggesting a more difficult treatment course during the initial admission.
Table 4. Actual and Expected Average Length of Stay (ALOS) and Charges for Initial Admissions With a Potentially Preventable Readmission (PPR) Chain.
| Admissions, ALOS, and Charges | Initial Admission Type | ||
|---|---|---|---|
|
| |||
| Medical | Surgical | Total | |
| Number of Initial Admissions Without a PPR | 1,921,861 | 926,531 | 2,848,392 |
| Number of Initial Admissions With a PPR | 175,028 | 67,963 | 242,991 |
| Actual ALOS for Initial Admissions With a PPR | 6.19 | 8.38 | 6.80 |
| Expected ALOS for Initial Admissions With a PPR | 5.69 | 7.36 | 6.16 |
| Difference Between Actual and Expected ALOS for Initial Admissions With a PPR | 0.50 | 1.02 | 0.65 |
| Percent Difference Between Actual and Expected ALOS for Initial Admissions With a PPR | 8.78 | 13.86 | 10.55 |
| Actual Average Charge for Initial Admissions With a PPR | $25,792 | $72,432 | $38,837 |
| Expected Average Charge for Initial Admissions With a PPR | $23,758 | $66,697 | $35,768 |
| Difference Between Actual and Expected Average Charge for Initial Admissions With a PPR | $2,034 | $5,735 | $3,069 |
| Percent Difference Between Actual and Expected Average Charges for Initial Admissions With a PPR | 8.56 | 8.60 | 8.58 |
NOTE: Table shows readmission to any hospital with a 15-day readmission time interval.
SOURCE: Florida inpatient hospital data, calendar years 2005-2006.
Patterns of Clinical Relationship
Table 5 shows the pattern of clinically related and unrelated readmissions for 11 (5 medical and 6 surgical) of the most commonly occurring base APR DRGs. Unlike the other tables, the readmission rates reported here count each readmission separately rather than as members of a PPR chain. The overall rate of readmissions varied widely across these APR DRGs, ranging from a high of 23.3 percent for respiratory failure with mechanical ventilation to a low of 7.5 percent for hip joint replacement and for cellulitis and skin ulcers.
Table 5. Reasons for Readmission to Any Hospital With a 15-Day Readmission Time Interval for Eight Common Initial Discharges.
| APR DRGs for Initial Admissions | Medical | Surgical | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||||||||
| APR130 Respiratory Failure With Mechanical Vent | APR 140 COPD | APR 194 CHF | APR 380 & 381 Cellulitis and Skin Ulcers | APR 165 & 166 CABG With & Without Cardiac Cath | APR 174 & 174 Angioplasty With & Without AMI | APR 221 Major Small & Large Bowel Procedures | APR 301 Hip Joint Replacement | |||||||||
|
|
|
|
|
|
|
|
|
|||||||||
| Number of Initial Admissions | 6,621 | 85,026 | 120,062 | 65,341 | 34,098 | 123,388 | 36,296 | 46,354 | ||||||||
| Number of Readmissions Within 15 Days | 1,542 | 11,208 | 21,694 | 4,890 | 4,814 | 12,617 | 4,108 | 3,471 | ||||||||
| Percent | 23.3 | 13.2 | 18.1 | 7.5 | 14.1 | 11.3 | 11.3 | 7.5 | ||||||||
| Number | Percent | Number | Percent | Number | Percent | Number | Percent | Number | Percent | Number | Percent | Number | Percent | Number | Percent | |
| Reason for Readmission | ||||||||||||||||
| Medical Readmission for a Continuation or Recurrence of the Reason for the Initial Admission, or for a Closely Related Condition | 774 | 50.2 | 6,080 | 54.2 | 9,669 | 44.6 | 1,483 | 30.3 | 2,446 | 50.8 | 5,084 | 40.3 | 1,139 | 27.7 | 143 | 4.1 |
| Medical Readmission for an Acute Decompensation of a Chronic Problem that was not the Reasons for the Initial Admission, but was Plausibly Related to Care Either During or Immediately After the Initial Admission | 187 | 12.1 | 1,877 | 16.7 | 2,879 | 13.3 | 1,106 | 22.6 | 509 | 10.6 | 1,106 | 8.7 | 592 | 14.4 | 860 | 24.8 |
| Medical Readmission for an Acute Medical Complication Plausibly Related to Care During the Initial Admission | 423 | 27.4 | 1,906 | 17.0 | 5,447 | 25.1 | 1,189 | 24.3 | 1,011 | 21.0 | 1,759 | 13.9 | 1,590 | 38.7 | 1,259 | 36.3 |
| Readmission for a Surgical Procedure to Address a Continuation or a Recurrence of the Problem Causing the Initial Admission | 11 | 0.7 | 129 | 1.2 | 408 | 1.9 | 139 | 2.8 | 224 | 4.7 | 3,330 | 26.4 | 220 | 5.4 | 644 | 18.6 |
| Readmission for a Surgical Procedure to Address a Complication Resulting from Care During the Initial admission. | 11 | 0.7 | 22 | 0.2 | 176 | 0.8 | 95 | 1.9 | 269 | 5.6 | 381 | 3.0 | 245 | 6.0 | 147 | 4.2 |
| Unrelated | 136 | 8.8 | 1,194 | 10.7 | 3,115 | 14.4 | 878 | 18.0 | 356 | 7.4 | 957 | 7.6 | 322 | 7.8 | 417 | 12.0 |
NOTES: APR DRG is all-patient refined diagnosis related groups. COPD is chronic obstructive pulmonary disease. CHF is congestive heart failure. CABG is coronary artery bypass grafting. Cath is cardiac catheterization. AMI is acute myocardial infarction.
SOURCE: Florida inpatient hospital data, calendar years 2005-2006.
In all cases, the majority of readmissions were clinically related to the initial admissions. In none of these selected APR DRGs was the proportion of clinically unrelated readmissions over 18 percent. As previously noted, the majority of possible combinations of readmissions and initial admissions were not clinically related (67 percent). However, the types of readmissions that did occur tended to be readmissions that were clinically related to an initial admission. Indeed, the most common reason for a readmission was the same as the reason for the initial admission.
The pattern of categories of related readmissions varied across APR DRGs. As would be expected, there were very few readmissions for a surgical procedure to address a complication that resulted from an initial admission for medical reasons. Readmissions for a surgical procedure to address a continuation or recurrence of the problem in the initial surgical admission, or to address a complication arising from the surgery in the initial surgical admission were more common, but still responsible for only a minority of the clinically related readmissions. The rate of readmissions for procedures to address recurrences of the initial problem was highest for angioplasty with and without acute myocardial infarction (APR DRGs 174 and 175), where the rate of 26.4 percent reflects the common clinical scenario of the need for a repeat angioplasty.
Modifications to Expected Readmission Rates
Although severity levels within each base APR DRG were highly predictive of risk of readmission, additional factors that might influence readmission risk were examined. Both patient age and the presence of certain major mental health or substance abuse problems (e.g., schizophrenia) as a comorbid condition in the initial admission were found to increase the probability of a readmission, and had independent effects beyond the APR DRG predicted values. As shown in Table 6, patients with mental health or substance abuse problems were more likely to be readmitted, while younger patients were less likely and older patients more likely to be readmitted. These adjustments were added to the calculation of expected values for PPR rates for individual hospitals. The mental health/substance abuse adjustment was only applied to patients for whom the mental health or substance abuse problem is a comorbid condition in the candidate admission.
Table 6. Actual Versus Expected Potentially Preventable Readmission (PPR) Rates for Patients With and Without Substance Abuse Problems.
| Age Group | No Major Mental Health or Substance Abuse Diagnoses | Major Mental Health or Substance Abuse Diagnoses | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Number of Candidate Admissions | Actual PPR Rate | Actual/Expected Ratio | Number of Candidate Admissions | Actual PPR Rate | Actual/Expected Ratio | |
| 0-5 Years | 72,643 | 3.77 | 0.729 | 362 | 8.29 | 0.826 |
| 6-18 Years | 72,826 | 4.21 | 0.698 | 16,070 | 9.15 | 0.778 |
| 18-35 Years | 211,084 | 5.12 | 0.874 | 68,268 | 11.76 | 1.032 |
| 36-55 Years | 601,197 | 5.63 | 0.892 | 168,748 | 12.7 | 1.15 |
| 56-75 Years | 929,102 | 6.98 | 0.914 | 82,706 | 12.86 | 1.204 |
| 76-85 Years | 577,790 | 9.14 | 1.069 | 25,521 | 13.23 | 1.29 |
| 85 Years or Over | 255,705 | 11.15 | 1.216 | 9,402 | 14.48 | 1.426 |
| Total | 2,720,347 | 7.23 | 0.972 | 371,077 | 12.48 | 1.137 |
SOURCE: Florida inpatient hospital data, calendar years 2005-2006.
Hospital Performance
Calculation of the difference in the actual minus expected rate of PPRs for each of the Florida hospitals, using both years of data combined, yielded a range from -37.54 percent (better than expected) to 397.14 percent (worse than expected). 93 hospitals were classified as having PPR rates significantly lower than expected and 81 hospitals were classified as having significantly higher PPR rates than expected for either of the 2 years at a p value of <0.05 using the Cochran-Mantel-Haenszel statistical test (Agresti, 1990).
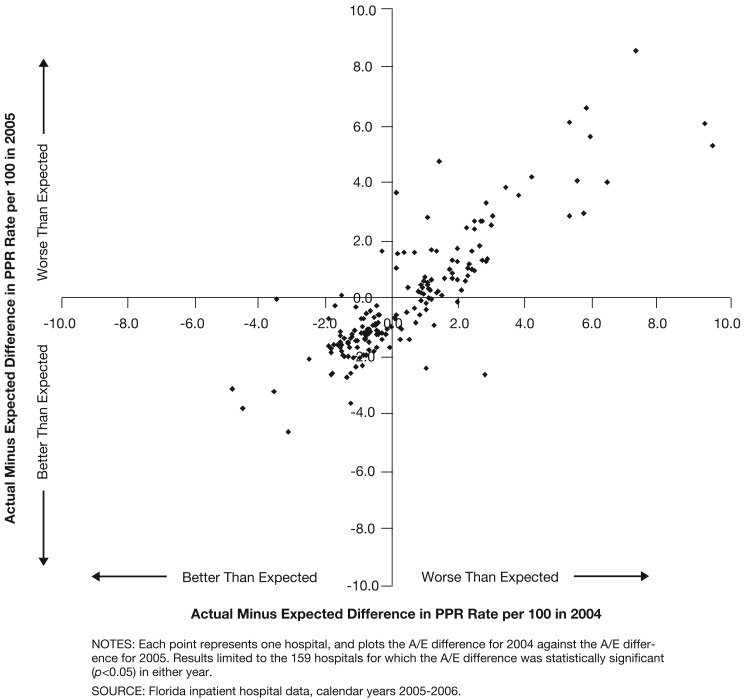
Figure 3 shows the actual minus expected PPR rate for 2004 and 2005 for each of the 174 hospitals that had a statistically significant difference in either of those years (76 of the 174 hospitals had a statistically significant difference in both years). The computation of the expected PPR rate includes the additional adjustments for age and the presence of mental health or substance abuse problems in the initial admission. The figure shows that although there seemed to be some amount of improvement from 2004 to 2005, hospitals tended to either perform worse than expected in both years, or to perform better than expected in both years. Only a relatively small group of hospitals changed from worse to better or vice versa over the 2-year span. Correlation between the 2 years as measured by the R2 value was 0.765.
Figure 3. Difference Between the Actual/Expected (A/E) Potentially Preventable Readmission (PPR) Rate at Each hospital.
Discussion
This article describes a method to identify potentially preventable hospital readmissions using administrative data and identifies several factors that influence the risk of readmission. This method builds on much previous work, and creates an approach that can be applied to a broad range of hospitalizations and readmissions. The PPR method recognizes that although readmissions can be associated with lower quality of care in the initial admission, many readmissions are not preventable. Those readmissions most likely to be preventable are those that have a plausible clinical relation to the initial admission, and occur relatively soon after the initial admission. The PPR method therefore creates specific links among all possible types of admissions and readmissions, as classified by APR DRGs, to determine which combinations can be considered potentially preventable.
The readmission time interval directly influences the level of confidence with which a readmission can be judged to be potentially preventable. For a shorter time interval there can be a greater degree of confidence that the readmission is causally linked to the clinical care or discharge planning process during the initial admission. For example, for a readmission for a urinary tract infection within 7 days following a admission for major bowel surgery, there is a high degree of confidence that urinary tract infection is causally related to the care rendered during the hospitalization for the bowel surgery, such as improper management of a urinary catheter. However, if the urinary tract readmission does not occur for 60 days following the bowel surgery the causal link is questionable.
Although 30 days after initial admission has been the most widely used readmission time interval for the definition of hospital readmissions (Hannan et al., 2003; Ashton et al., 1997), a shorter time readmission interval such as 15 or 7 days will have more appeal to hospital personnel because they have the greatest degree of control over the processes of care during the hospitalization and the discharge planning process and much less control of care beyond the immediate post discharge period.
The concept of a readmission chain is introduced in this article, which provides for a more precise specification of the readmission pattern associated with the care rendered during and following specific types of initial admissions. For example, an admission for CABG followed by a readmission for pneumonia, which is then followed by a readmission for a PTCA constitutes a readmission chain. Although the readmission for the PTCA is clinically unrelated to the prior admission for the pneumonia, both readmissions are most likely related to the CABG admission. Using the concept of a readmission chain, this patient, who would otherwise be characterized as a CABG admission with one readmission plus an unrelated admission for a PTCA, is more usefully characterized as coronary artery bypass grafting admission with two related readmissions.
These analyses demonstrate that the probability of a readmission is related to the reason for admission, severity of illness, the presence of comorbid mental health or substance abuse problems, and the patient's age at the time of the initial admission. Risk adjustment for each of these factors is therefore necessary in order to create fair evaluations of readmission rates. This analysis also shows that PPR rates increase with increasing time after the initial admission, and that the readmission rate is higher if readmissions to any hospital are considered rather than only readmissions to the same hospital where the initial admission took place. Furthermore, PPR rates for individual hospitals appear to be stable over time.
The PPR method relies on discharge abstract codes and is therefore limited by inherent problems in consistency and completeness of coding, and by the lack of clinical detail available for making judgments on the preventability of a readmission and the presence of a quality problem. PPRs will require various kinds of validation, ranging from consensus among clinicians about their clinical appropriateness and their ability to identify quality problems, to the ultimate test of their utility—whether they can contribute to performance-improving behavior change based on the identification of quality problems.
The examination of readmission rates should prove useful for internal quality review, allowing hospitals to identify the types of admissions that have higher than expected readmission rates. Readmission rates should also prove useful for comparing performance across hospitals and have the potential to become a useful tool for consumer information. The Florida Agency for Healthcare Administration (2008) has published comparative hospital readmission rates using PPRs. Eventually, public information campaigns that publish reliable outcome measures such as readmissions can both encourage and assist hospitals in examining the quality of care systems in their facilities, thus complementing pay-for-performance incentives based on these measures.
The increasing interest in pay-for-performance attempts to take advantage of the expanding availability of enhanced data sets, quality measures and guidelines, (MedPAC, 2003; 2008) and is, in part, a natural response to escalating health care costs. Because of their high cost, readmissions can be an important component of pay-for-performance efforts.
MedPAC (2008) has proposed that Medicare should reduce payments to hospitals with high readmission rates. From a policy perspective the key challenge is to establish the extent of the payment reduction for a readmission. For true medical errors that are clearly related to mistakes in the delivery of care (readmission to remove a foreign object left in after a prior surgery), not paying for the readmission may be justified. However, most readmissions are not so clearly linked to medical errors, and, although they may possibly relate to errors in judgment or lapses in execution that reflect poor quality care, they cannot be considered always preventable. Thus, a specific type of readmission will be preventable for some patients and not preventable for other patients (even after clinical exclusions for patients for whom the readmission is clearly not preventable). A balance between the relative preventability of a readmission and the extent of the payment reduction associated with the readmission needs to be achieved. The financial consequences of a readmission need to be significant enough to motivate hospitals to reduce readmission rates, without penalizing hospitals for events over which they have limited control.
MedPAC is essentially proposing that the extent of the payment reduction for a readmission be set separately for each hospital based on its risk-adjusted readmission rate. Since susceptibility to readmissions varies depending on the patient's severity of illness at the time of discharge, it is crucial that the determination of a hospital's risk-adjusted readmission rate adequately account for the patient's condition at the time of discharge. Under MedPAC's proposal, hospitals with the lowest riskadjusted readmission rates would have a small reduction in payment for readmissions, while hospitals with high readmission rates would have a larger reduction in payment. The advantage to this approach is that an estimate of the relative preventability of readmissions does not have to be made. Instead, the amount of the payment reduction is based on the relative overall performance of hospitals in terms of their risk-adjusted readmission rate.
Conclusion
Given the increasing pressure to control health care costs and improve quality, and increasing public and governmental scrutiny of both, financial incentives associated with quality measures in general, and hospital readmission rates in particular, will only increase. The effectiveness of these efforts will depend on the integrity of the data and the validity of the methods used in any performance-based payment systems. This study suggests that adequate risk stratification based on patient type and severity of illness as well as identification of those readmissions that are potentially preventable are critical to the fairness and usefulness of any evaluations and comparisons of hospital readmission rates.
Footnotes
Norbert I. Goldfield, M.D., Elizabeth C. McCullough, Richard F. Averill, and Ana M. Tang are with 3M Health Information Systems. John S. Hughes, M.D. is with Yale University School of Medicine. Beth Eastman is with the Florida Agency for Health Care Administration. Lisa K. Rawlins is with Broward Health, Broward County, Florida. The statements expressed in this article are those of the authors and do not necessarily reflect the views or policies of 3M Health Information Systems; Yale University School of Medicine; Florida Agency for Health Care Administration; Broward Health, Broward County, Florida; or the Centers for Medicare & Medicaid Services (CMS).
Reprint Requests: Norbert Goldfield, M.D., 3M Health Information Systems, 100 Barnes Road, Wallingford, CT 06492. E-mail: nigoldfield@mmm.com
References
- Agresti A. Categorical Data Analysis. John Wiley & Sons; New York, NY.: 1990. [Google Scholar]
- Anderson GF, Steinberg EP. Hospital Readmissions in the Medicare Population. New England Journal of Medicine. 1984 Nov 22;311(21):1349–1353. doi: 10.1056/NEJM198411223112105. [DOI] [PubMed] [Google Scholar]
- Ashton CM, Del Junco DJ, Souchek J, et al. The Association Between the Quality of Inpatient Care and Early Readmission: A Meta-Analysis of the Evidence. Medical Care. 1997 Oct;35(10):1044–1045. doi: 10.1097/00005650-199710000-00006. [DOI] [PubMed] [Google Scholar]
- Averill RF, Goldfield NI, Muldoon J, et al. A Closer Look at All-Patient Refined DRGs. Journal of AHIMA. 2002 Jan;73(1):46–50. [PubMed] [Google Scholar]
- Florida Agency for Healthcare Administration. Internet address: www.floridahealthfinder.gov (Accessed 2008)
- Friedman B, Basu J. The Rate and Cost of Hospital Readmissions for Preventable Conditions. Medical Care Research and Review. 2004 Jun;61(2):225–240. doi: 10.1177/1077558704263799. [DOI] [PubMed] [Google Scholar]
- Halfon P, Eggli Y, Pretre-Rohrbach I, et al. Validation of the Potentially Avoidable Hospital Readmission Rate as a Routine Indicator of the Quality of Hospital Care. Medical Care. 2006 Nov;44(11):972–981. doi: 10.1097/01.mlr.0000228002.43688.c2. [DOI] [PubMed] [Google Scholar]
- Hannan EL, Racz MJ, Walford G, et al. Predictors of Readmission for Complications of Coronary Artery Bypass Graft Surgery. JAMA. 2003 Aug 13;290(6):773–780. doi: 10.1001/jama.290.6.773. [DOI] [PubMed] [Google Scholar]
- Kripalani S, LeFevre F, Phillips CO, et al. Deficits in Communication and Information Transfer Between Hospital-Based and Primary Care Physicians. JAMA. 2007 Feb 28;297(8):831–841. doi: 10.1001/jama.297.8.831. [DOI] [PubMed] [Google Scholar]
- Medicare Payment Advisory Commission. Using Incentives to Improve the Quality of Care. Medicare Payment Policy. 2003 Jun; Report to Congress. [Google Scholar]
- Medicare Payment Advisory Commission. A Path to Bundled Payment Around a Hospitalization. Medicare Payment Policy. 2008 Jun; Report to Congress. [Google Scholar]
- Miller ME. Statement of Executive Director of the Medicare Payment Advisory Commission, before the Subcommittee on Health, Committee on Energy and Commerce. U.S. House of Representatives; Apr 18, 2007. [Google Scholar]