Abstract
Little is known about how work environment characteristics influence social services professionals' ability to deliver effective psychosocial services in skilled nursing facilities (SNFs) and how such influence translates into resident-centered outcomes. This study combines data from a survey of facility social services directors in Washington State with State inspection outcomes from the Online Survey Certification Reporting database. Logistic regression is used to examine how facility structure and facility culture impact receipt of a survey inspection deficiency in medically-related social services. Results indicate that non-metropolitan location and larger caseload size are the strongest predictors of receiving such a deficiency.
Introduction
Among social service professionals1 in SNFs, a relationship exists between work environment characteristics and employee-related outcomes such as job satisfaction, turnover intention (Gleason-Wynn and Mindel, 1999; Simons, 2006), and perceived decisionmaking power (Kruzich and Powell, 1995). However, less is known about how work environment characteristics influence social service professionals' ability to deliver effective psychosocial services and how such influence translates into resident-centered outcomes, such as State survey inspection results. Nursing home psychosocial care advocates assert that next step efforts to enhance quality of life and quality of care must include research that links social service delivery to resident outcomes (Vourlekis, Zlotnik, and Simons, 2005). As a component of a larger study of multilevel variables predicting State survey deficiencies in psychosocial care, the current study examines how facility receipt of a deficiency in medically-related psychosocial services varies by facility work environment characteristics. Combined data from a survey of SNF social service directors (SSDs) in Washington State and the Federal Online Survey Certification and Reporting database (OSCAR) are utilized to predict which SNFs received a deficiency in medically-related social services and which did not. Additional knowledge regarding how facility work environment factors influence such psychosocial care outcomes will enable policymakers, resident advocates, and facility personnel to tailor specific interventions to enhance quality of care.
Literature Review
Psychosocial needs refer to a range of SNF residents' needs that center on mental health, social services, and quality of life. According to standards developed by the National Association of Social Workers (2003), focal areas for psychosocial needs include:
The social and emotional impact of physical or mental illness or disability.
The preservation and enhancement of physical and social functioning.
The promotion of the conditions essential to ensure maximum benefits from long-term health care services.
The prevention of physical and mental illness and increased disability.
The promotion and maintenance of physical and mental health and an optimal quality of life.
Persons living in SNFs have extensive psychosocial needs, yet the services provided to address those needs appear insufficient. Indeed, substantial evidence indicates SNF residents' psychosocial needs are generally not met (Vourlekis, Gelfand, and Greene, 1992a; Tirrito, 1996; Parker-Oliver and Kurzejeski, 2003; U.S. Department of Health and Human Services, 2003). For example, a recent study conducted by the U.S. Office of Inspector General (OIG) revealed that out of 299 residents, 95 percent had at least one psychosocial need such as depression, anxiety, sad mood, or behavioral symptoms, yet 39 percent lacked care plans to address those needs. Furthermore, among residents with adequate care plans, 41 percent did not receive all services recommended by the plan and 5 percent received none of the recommended services (U.S. Department of Health and Human Services, 2003). These gaps in service delivery were evident in resident-centered outcomes: on inspection by State surveyors, 15 percent of the facilities received deficiencies in medically-related social services.
Several studies identify challenges SNF social service professionals face in providing quality psychosocial services to all residents who need them. The OIG study found that although 98 percent of facilities had social work staffing levels that met Federal requirements, 45 percent of social service professionals reported barriers to providing sufficient psychosocial care. Barriers included not having enough time, having too much paperwork, insufficient staff, and numerous responsibilities beyond providing psychosocial services. These responsibilities “…range[d] from running errands outside the facility to assisting with dining room arrangements to getting residents' eyeglasses fixed…” Nursing home administrators concurred that social work time constraints and paperwork demands were the primary obstacles to addressing residents' psychosocial needs.
Professionals in the field echo the OIG findings with reports of similar difficulties. O'Neill (2002) suggests SNF social service professionals tend to be assigned inappropriate jobs that “…draw [them] away from what they have been educated and trained to do…” Fiske (2003) found mountains of paperwork and other tasks reduced their availability to provide psychosocial services. Indeed, SNF social service professionals are described as practicing under severe time constraints (Parker-Oliver and Kurzejeski, 2003) and time studies reveal they have about 6 minutes per resident/per day to address all psychosocial needs, including assessment, care planning, and intervention (Harrington et al., 2000). Furthermore, the responsibility for ongoing completion of federally-mandated individualized assessments requires considerable time and may limit social service professionals' opportunity to provide psychosocial intervention (Parker-Oliver and Kurzejeski, 2003). One study illustrates the impact of such time constraints: disproportionate time allotted to psychosocial assessment relative to psychosocial intervention is associated with poorer outcomes in psychosocial care in contrast to a more equivalent investment of time in both assessment and intervention (Bonifas, 2008). Table 1 details common services in SNFs defined as medically-related social services.
Table 1. Medically-Related Social Services Provided in Skilled Nursing Facilities1.
|
American Health Care Association: The Long Term Care Survey. Washington, DC. 2006.
Along with presenting obstacles to the provision of psychosocial care, SNFs are challenging work settings for social service professionals in general. For example, the majority of SNF social service professionals are solo practitioners (Tirrito, 1996; Parker-Oliver and Kurzejeski, 2003), thus they practice in host environments where organizational missions and values are defined by other professions (Dane and Simon, 1991). Difficulties commonly encountered in host settings include managing value discrepancies among multiple disciplines, advocating with limited facility decisionmaking influence, negotiating conflict, and coping with role ambiguity combined with role strain. Host settings can also limit social service professionals' autonomy, yet autonomous practice is associated with increased job satisfaction and longevity in the field (Gleason-Wynn and Mindel, 1999) as well as higher levels of satisfaction among facility residents (Vourlekis, Zlotnika, and Simons, 2005). Similarly, when social service professionals are able to influence decisions, they typically influence decisions that impact residents' well-being (Kruzich and Powell, 1995). SNF social service professionals who receive support from supervisors, coworkers, and colleagues are better able to navigate the challenges inherent to host environments (Gleason-Wynn and Mindel, 1999; Parker-Oliver and Kurzejeski, 2003).
Given the previously mentioned issues, it is likely that important factors associated with outcomes in psychosocial care are linked to characteristics of the facility work environment. Indeed, among facilities identified as providing best practice psychosocial care, social service professionals report positive workplace attributes such as effective utilization of their expertise, highly satisfying roles and functions, integration of social services into the interdisciplinary team, and an overall value of social work skills and services (Vourlekis, Zlotnika, and Simons, 2005).
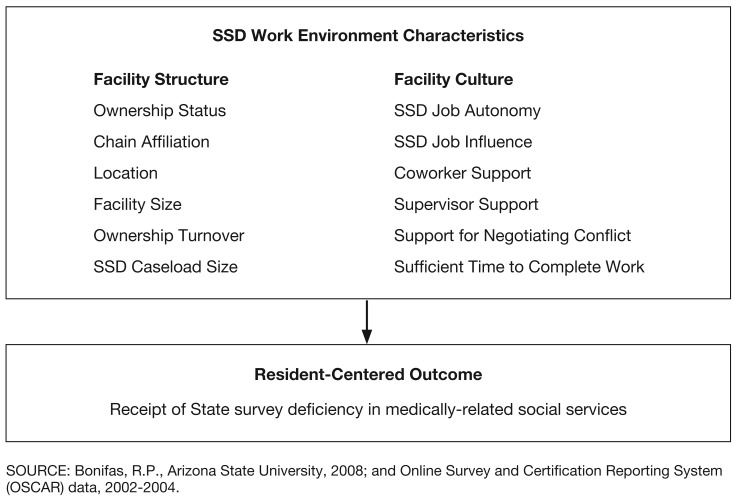
Work environment can be construed as a combination of facility structural factors and overall facility climate or culture. Facility structure refers to more inflexible characteristics of the work environment, such as its location or profit status; facility culture refers to more changeable characteristics influencing the work environment, for example, the level of supervisor support available or the extent of job autonomy offered by a given position. This study examines how facility structural factors and characteristics of the facility culture predict facility receipt of a State survey deficiency in medically-related social services. Facility structural factors include facility ownership turnover, facility ownership status, multi-chain affiliation, facility size, facility location, and the size of the social services professional's caseload. Facility culture characteristics include the social services professionals' level of job autonomy, supervisor support, coworker support, influence within the facility, and support for negotiating conflict, as well as the availability of sufficient time to complete his or her work responsibilities. The research hypothesis is that facility structural factors and facility cultural factors will both influence whether or not facilities receive a deficiency; however, facility structural factors are anticipated to have stronger predictive power relative to facility cultural factors.
Conceptual Model
The provision of medically-related social services is an aspect of overall quality of care and quality of life. Therefore, correlates of these broader definitions of quality offer important constructs for examining the impact facility work environment characteristics have on resident-centered outcomes. Myriad factors are associated with quality of care and quality of life in SNFs. Variables linked to higher scores on quality measures include, (1) lower levels of organizational change (Castle, 2001, 2005; Anderson, Corazzini, and McDaniel, 2004); (2) non-profit ownership status (Harrington et al., 2002; Anderson, Issel, and McDaniel, 2003; Castle and Myers, 2006); (3) not being affiliated with a multi-facility chain organization (Castle, 2001; Kruzich; 2005); (4) smaller facility size (Anderson, Issel, and McDaniel, 2003); (5) metropolitan facility location (Bravo et al., 1999); and (6) smaller caseload size (Kruzich and Powell, 1995; Harrington et al., 2000).
In addition, State survey inspection results provide meaningful resident-centered quality outcomes and have frequently been utilized in long-term care research. SNFs participating in the Medicare and/or Medicaid funding program(s) are held accountable to meet standards of quality specified in Federal and State regulations. Onsite evaluations of each facility are conducted by the State survey agency under contract with CMS at least once during a 15-month interval and may occur more often if a complaint needs to be investigated. The primary goal of evaluation is to ensure facility compliance with regulations stipulating the provision of quality care and resident safety (Harrington et al., 2000).
Annual survey results detail facility deficiencies issued by the State survey agency. Deficiencies represent the survey agency's evaluation of quality-related problems existing within the facility. If a facility fails to meet specific standards or regulations, a deficiency is issued. While measurement weaknesses have been identified in the survey investigative process in terms of interrater reliability for categorizing individual deficiencies, State survey results are commonly recognized as important indicators of facility quality (Lee, Gajewski, and Thompson, 2006). For example, State and Federal governments have used items from survey results to develop online nursing home report cards, including Nursing Home Compare, to support consumer choice in long-term care decisionmaking. Survey reliability is strongest when aggregate results are utilized (Lee, Gajewski, and Thompson, 2006), as is done in the current study.
There are several survey deficiency categories that potentially relate to psychosocial care; however one category is particularly relevant for the current study in that it examines the broadest range of psychosocial services and associated resident psychosocial needs: medically-related social services. This regulatory requirement dictates that facilities provide medically-related social services to attain or maintain the highest practicable physical, mental, and psychosocial well-being of each resident. As such, it provides a valuable proxy for capturing effective psychosocial care. The various services comprising medically-related social services are listed in Table 1. The overall model guiding this research study, featuring relevant independent variables, is depicted in Figure 1.
Figure 1. Conceptual Model: Relationship Between Work Enviroment Characteristics and Resident-Centered Outcomes.
Method
A cross-sectional research design was utilized and merged two sources of data, primary and secondary. Primary data associated with facility culture were collected via a self-administered questionnaire mailed to all SSDs in Washington State SNFs whose administrator authorized participation in the study. Primary data collection took place over an 8-week period in early 2006. Secondary data associated with facility structure and survey deficiencies in medically-related psychosocial services were obtained from the OSCAR for Washington State for the years 2002-2004. OSCAR is a computerized national database of State survey inspection results, facility staffing information, and facility characteristics that is considered to accurately reflect both survey deficiencies issued by State surveyors and actual problems existing within facilities (Harrington et al., 2000). A combined data set was created that consisted of each SSD's questionnaire responses linked to a 3-year history of his or her facility's State survey results, supporting analysis of differences across SSDs' self-reports and past facility performance. At least 3 years' worth of survey data is necessary to capture a facility's quality over time. As such, survey results utilized in this study correspond to inspections that occurred during a 3-year period from 1 to 4 years prior to collection of primary data via the SSD questionnaire. Data collected on SSDs' facility tenure enabled the author to temporarily exclude from analysis any SSDs with less than 1-year employment histories and facilitated examination of the implications posed by the 1-year time lag between the survey inspections recorded in OSCAR and primary data collection. (Limitations of this method are detailed in the discussion section.)
Measures
Facility Structure
Although data on facility-level changes, such as administrative turnover, are not a component of OSCAR, a measure of ownership turnover is included and provides an important measure of change occurring at the highest and most pervasive organizational level. Ownership turnover is a continuous variable and captures the number of times a facility has changed ownership (i.e., been sold) since first being licensed through the Medicare and/or Medicaid program(s). Research indicates facility acquisition by another nursing home chain can be detrimental to residents' quality of life, especially when poor-performing chains purchase poor-performing facilities (Banaszak-Holl et al., 2002). In addition, facilities that experience ownership changes have higher Medicaid occupancy rates, receive more survey deficiencies, and may house residents with greater physical and mental health care needs than facilities that do not undergo ownership change (Castle, 2005).
Facility ownership status refers to whether a facility is a for-profit or a non-profit organization, or a government-owned organization. Only two facilities in the sample were government-owned; these were incorporated into the non-profit category, a strategy that has been utilized in previous research (Castle and Myers, 2006). This measure was treated as a dichotomous variable, for-profit facilities were coded 1 and non-profit facilities were coded 0.
Multi-facility chain affiliation is also a dichotomous variable and refers to whether a facility is operated by a multifacility chain organization or not. Chain affiliated facilities were coded 1 and non-chain-affiliated facilities were coded 0.
Facility size was measured as a continuous variable representing the total number of licensed beds in the facility.
SSD caseload is a continuous variable and represents the ratio of social service professionals to facility residents. It was created by dividing the average number of residents in the facility, as recorded in OSCAR, by the number of social service professionals in the facility, as obtained from the SSD questionnaire.
Extrapolating from county and ZIP Code data obtained from OSCAR, facility location was determined using the rural-urban continuum codes available through the Economic Research Service (ERS) of the United States Department of Agriculture.2 ERS provides county rankings on a scale from 1 to 9 and employs three metropolitan codes and six non-metropolitan codes that account for each county's population and its proximity to an urban area. In this sample, several code categories contained few facilities, thus the nine rural-urban continuum codes were collapsed and facilities assigned to one of two categories to create a dichotomous variable: metropolitan, coded 1, and non-metropolitan, coded 0.
Facility Culture
Instrumentation
As a component of a larger study examining multilevel predictors of psychosocial care outcomes in SNFs, a self-administered survey instrument was developed utilizing questions derived from the literature and generated by the author. The questionnaire was designed to gather information related to facility organizational processes, social service professional characteristics, and the frequency of psychosocial service delivery; the current study focuses on results specific to SSD work environment characteristics and SSD demographics. Five researchers familiar with survey research and/or long-term care services assessed the content validity of the survey instrument, and it was pilot-tested by five master's level social workers employed in Washington State SNFs. To ensure the survey instrument was accessible to SSDs with diverse years of work experience, these five social workers represented practitioners whose practice experience ranged from several years to less than 1 year. Comments and suggestions from the researchers and practitioners were incorporated into the final instrument and some questions were modified from the original versions when recommended by the reviewers.
Variables of interest measured via the questionnaire include SSD job autonomy, supervisor support, coworker support, SSD influence in facility decisionmaking, the availability of sufficient time to complete work, and the level of support available to the SSD for negotiating conflict. All constructs are measured utilizing a 6-point Likert scale ranging from 1 “strongly agree” to 6 “strongly disagree” and, except where noted, are based on measures developed by Gleason-Wynn and Mindel (1999). These researchers employed the original questions with a reasonably representative sample of 329 social service professionals practicing in Texas SNFs and conducted confirmatory factor analysis to assess convergent validity of the results. Satisfactory model fit was found for all constructs. Scale scores represent the summation of individual items, which were then reverse-coded and converted to the original Likert measure to allow for meaningful comparisons across scales. As such, scores closer to 6 indicate stronger positive responses, while scores closer to 1 indicate stronger negative responses.
Social work job autonomy was measured via an eight-question scale that address the SSD's perception of concepts such as the clarity of his or her job responsibilities and the degree to which he or she is allowed to prioritize tasks independently. Factor loadings ranged from 0.567 to 0.822 for this construct.
Supervisor support was measured using a scale consisting of six questions that address concepts such as the SSD's perception of his or her supervisor's understanding of psychosocial service workload demands and the level of agreement between the SSD and his or her supervisor on psychosocial care priorities. Factor loadings ranging from 0.778 to 0.859 for this construct.
Coworker support was measured with a scale comprised of eight questions that assess such concepts as the SSD's perceptions regarding the level of emotional support provided by coworkers and the extent to which coworkers create a trusting work environment. Factor loadings ranged from 0.714 to 0.911 for this construct.
SSD influence was measured via a scale containing three questions that focus on the SSD's assessment of his or her ability to influence decisionmaking within the facility. Factor loadings ranges from 0.588 to 0.886 for this construct.
Sufficient time to complete work captures the extent that SSDs feel adequate time is available during the workday to accomplish necessary job tasks. It was measured by one question, “I have enough time to get everything done on my job.”
Support negotiating conflict captures the extent to which SSDs receive support for decisionmaking related to ethical dilemmas or when regulatory demands and/or resident rights are at odds. It is measured by one question developed by the author, “When I find myself in situations where State and/or Federal regulations or resident rights are in conflict, I receive support from others in my facility to guide my decision-making.”
Sampling
Facilities were identified via the Washington State Department of Social and Health Services' Web site directory of nursing homes.3 Freestanding (non-hospital based) facilities certified by Medicare and/or Medicaid were targeted for inclusion in the sample; 233 facilities were identified. An introductory letter that described the study and invited facility participation was sent to each facility administrator. Thirty-one administrators requested that their facility not be included in the study; questionnaires were not sent to these facilities, leaving a participating sample of 202. Statistical analysis via chi-square and ANOVA revealed no differences among non-respondent, participating, and non-participating facilities in terms of facility size, location, average number of residents, chain affiliation, ownership turnover, ownership status, number of State survey deficiencies, or the scope and severity of survey deficiencies.
Data Collection
The self-administered questionnaire was distributed to SSDs through a series of four mailings, as recommended by Dillman (2002). While larger facilities may have more than one social service professional on staff, directing the survey to SSDs promoted feasibility of the study and targeted data gathering efforts toward the social service professional most knowledgeable about psychosocial service practices throughout the facility. To maximize the response rate, pre-letters were sent introducing the study, describing its importance, and requesting the SSD's assistance in obtaining information. The survey instrument and informed consent documentation followed 1 week later, reiterating the study's importance and inviting participation. To encourage timely response a small financial incentive was offered to all participants who returned their survey postmarked within a 2-week time period. Followup contacts included two additional mailings. A 60-percent response rate was achieved, representing 121 SSDs.
Analysis
The Statistical Package for the Social Sciences (SPSS) version 11.5 was employed for all statistical procedures. The OSCAR data was screened for duplicates and accuracy as recommended by Castle (2001) and identified errors corrected prior to analysis. Then the sample was divided into two groups: (1) facilities that received deficiencies in medically-related social services (n = 34) and (2) facilities that did not receive deficiencies in medically-related social services (n = 87). Independent samples t-tests and chi-square analysis were run to compare differences between facilities in terms of facility structure and culture characteristics. Significant factors were then entered into two logistic regression models to assess the ability of these variables to predict deficiencies in medically-related psychosocial services. Logistic regression has one assumption to ensure that accurate results are obtained: equivalent probabilities must be maintained across all predictor values. Results are considered robust as long as the sample is random or observations are independent from each other (Peng, Lee, and Ingersoll, 2002); as such the assumption was met for this study given the independent nature of the observations.
Results
Tables 2 and 3 describe the sample in terms of SSD respondents and their corresponding facilities, respectively.
Table 2. Sample Description: Social Services Directors.
| Demographic | n | Percent |
|---|---|---|
| Sex | ||
| Female | 111 | 92.5 |
| Male | 9 | 7.5 |
| Ethnicity | ||
| Black/African American | 0 | 0 |
| Asian/Pacific Islander | 5 | 4.2 |
| Native American/Alaska Native | 0 | 0 |
| Latino | 5 | 4.2 |
| Caucasian | 106 | 88.3 |
| Other Ethnicity | 2 | 1.7 |
| Age | ||
| 25-34 Years | 35 | 29.4 |
| 35-44 Years | 23 | 19.3 |
| 45-54 Years | 28 | 23.5 |
| 55-64 Years | 33 | 27.7 |
| Declined to Respond | 2 | 1.7 |
| Income | ||
| $10,000 or Less | 1 | 0.8 |
| $10,001 - $20,000 | 4 | 3.3 |
| $20,001 - $30,000 | 16 | 13.3 |
| $30,001 - $40,000 | 39 | 32.5 |
| $40,001 - $50,000 | 39 | 32.5 |
| $50,001 or More | 15 | 12.5 |
| Declined to Respond | 6 | 5.0 |
| Education | ||
| MSW | 25 | 20.8 |
| BSW | 18 | 15 |
| Other Bachelors Degree | 44 | 36.7 |
| Other Masters Degree | 19 | 15.8 |
| No College Degree | 14 | 11.7 |
| Years of Experience | Mean | S.D. |
| Overall SNF | 10.79 | 7.81 |
| SNF Social Services | 7.92 | 5.64 |
| Current SNF | 5.23 | 5.22 |
| Current position | 4.95 | 4.45 |
n = 121.
NOTES: SNF is skilled nursing facility. S.D. is standard deviation.
SOURCE: Bonifas, R.P., Arizona State University, 2008; and Online Survey and Certification Reporting System (OSCAR) data, 2002-2004.
Table 3. Sample Description: Skilled Nursing Facilities.
| Demographic | n | Percent |
|---|---|---|
| Location | ||
| Metro | 103 | 85.1 |
| Non-Metro | 18 | 14.9 |
| Ownership Status | ||
| Non-Profit | 31 | 74.1 |
| Profit | 89 | 25.9 |
| Chain Affiliation | ||
| Chain | 74 | 61.7 |
| Non-Chain | 46 | 38.3 |
| Facility Size | ||
| < 60 Beds | 26 | 21.1 |
| 61-120 Beds | 59 | 54.6 |
| >120 Beds | 29 | 24.2 |
| Survey Deficiency in Medically-Related Social Services | ||
| Yes | 34 | 28.9 |
| No | 87 | 71.1 |
|
| ||
| Mean | S.D. | |
|
| ||
| Ownership Turnover | 2.11 | 2.5 |
| SSD Caseload | 72.79 | 33.51 |
n = 121.
NOTES: SSD is social service director. S.D. is standard deviation.
SOURCE: Bonifas, R.P., Arizona State University, 2008; and Online Survey and Certification Reporting System (OSCAR) data, 2002-2004.
Chi-square analysis and independent samples t-tests reveal several important differences between facilities that received a deficiency in medically-related social services and those that did not and provide partial support for the study's hypothesis. In terms of facility level factors, ownership status, facility location, SSD caseload, and the extent of ownership turnover differed significantly by deficiency status. Specifically, facilities that received deficiencies in medically-related social services were located in non-metropolitan areas (p < 0.01), were for-profit facilities (p < 0.01), had SSDs with larger caseloads (p < 0.05), and experienced greater ownership turnover (p < 0.05). There were no differences between facilities in terms of chain ownership status or facility size (Table 4).
Table 4. Survey Deficiencies in Medically-Related Social Services: Comparisons Across Facility Structural Variables.
| Received Deficiency | Did Not Receive Deficiency | χ2 | |||
|---|---|---|---|---|---|
| Facility Location | Metro | Non-Metro | Metro | Non-Metro | 15.570** |
|
|
|
|
|
|
|
| Number | 22 | 12 | 81 | 6 | — |
| Percent | 21.4 | 66.7 | 78.6 | 33.3 | — |
| Ownership Status | Non-Profit | For-Profit | Non-Profit | For-Profit | 7.164** |
|
|
|
|
|
|
|
| Number | 3 | 31 | 28 | 58 | — |
| Percent | 9.7 | 34.8 | 90.3 | 65.2 | — |
| Chain Affiliation | Non-Chain | Chain | Non-Chain | Chain | 1.597 |
|
|
|
|
|
|
|
| Number | 10 | 24 | 36 | 50 | — |
| Percent | 21.7 | 32.4 | 78.3 | 67.6 | — |
| Mean | S.D. | Mean | S.D. | t | |
|
|
|
|
|
|
|
| Facility Size | 99.00 | 34.46 | 94.00 | 40.69 | -0.63 |
| Ownership Turnover | 3.06 | 3.04 | 1.72 | 2.14 | -2.34* |
p<0.05.
p<0.01.
NOTES: S.D. is standard deviation; categorical IVs are facility location, ownership status, and chain affilication; continuous IVs are facility size and ownership turnover.
SOURCE: Bonifas, R.P., Arizona State University, 2008; and Online Survey and Certification Reporting System (OSCAR) data, 2002-2004.
In terms of facility culture, sufficient time to complete work, job influence, job autonomy, and support for negotiating conflict were significantly different between facilities that received deficiencies in medically-related social services and those that did not. Facilities that received deficiencies in medically-related social services had SSDs who reported not having sufficient time to complete necessary tasks (p < 0.05), having less influence in facility decisionmaking (p < 0.05), less autonomy in determining work priorities (p < 0.05), and less support in negotiating conflict (p < 0.05). There were no significant differences between facilities in terms of coworker support or supervisory support; however, results approached significance (p < 0.10) and it is possible that with a larger sample size, a statistically significant difference could be detected (Table 5).
Table 5. Survey Deficiencies in Medically-Related Social Services: Comparisons Across Facility Cultural Variables.
| Variable | Received Deficiency | Did Not Receive Deficiency | |||
|---|---|---|---|---|---|
|
| |||||
| Mean | S.D. | Mean | S.D. | t | |
|
|
|
|
|
|
|
| SSD Caseload | 87.60 | 33.46 | 66.49 | 31.69 | -3.20* |
| Sufficient Time to Complete Work | 1.00 | 1.18 | 1.60 | 1.42 | 2.36* |
| Support for Negotiating Conflict | 3.44 | .96 | 3.82 | .92 | 1.99* |
| Job Influence | 2.99 | 1.32 | 3.42 | 1.00 | 1.96* |
| Job Autonomy | 3.17 | .87 | 3.49 | .79 | 1.96* |
| Coworker Support | 3.44 | .92 | 3.73 | .62 | 1.70 |
| Supervisor Support | 3.22 | 1.11 | 3.61 | 1.10 | 1.76 |
p<0.05.
NOTE: SSD is social service director. S.D. is standard deviation.
SOURCE: Bonifas, R.P., Arizona State University, 2008; and Online Survey and Certification Reporting System (OSCAR) data, 2002-2004.
Building on significant relationships identified in the bivariate analysis, two logistic regression models were constructed to further test the study hypothesis, that both facility structural and cultural variables influence receipt of survey deficiencies in medically-related social services, but that structural factors have the strongest predictive power. Model 1 included facility structural variables (ownership turnover, facility location, ownership status, and SSD caseload size); model 2 included facility structural variables entered in at step 1 and facility culture variables (SSD job autonomy, SSD influence, sufficient time, and conflict support) entered in at step 2. Results reveal that both models fit the data better than the intercept-only model; however, model 2 demonstrates slightly improved fit over model 1 as evidenced by gains in model fit indices. In addition, both models overall significantly predict receipt of a deficiency in medically-related psychosocial services, but only two variables are significant predictors: SSD caseload and facility location. Consistent with the study hypothesis, these predictors are facility structural variables and offer partial support that these factors influence outcomes in psychosocial care. Indeed, the odds of receiving a deficiency in medically-related social services are 7.54 times greater for non-metropolitan facilities than for metropolitan facilities (p = 0.002). Results are shown in Table 6 for model 1 and Table 7 for model 2.
Table 6. Model 1 Logistic Regression Results: Facility Receipt of a Deficiency in Medically-Related Social Services by Facility Structural Variables.
| Variable | B | S.E. | Wald | df | P | Exp(B) Odds Ratio |
|---|---|---|---|---|---|---|
| Ownership Turnover | 0.12 | 0.1 | 1.432 | 1 | 0.231 | 1.128 |
| Facility Location | 1.953 | 0.618 | 10 | 1 | 0.002 | 7.049 |
| SSD Caseload | 0.019 | 0.008 | 6.092 | 1 | 0.014 | 1.019 |
| Ownership Status | 0.606 | 0.732 | 0.685 | 1 | 0.408 | 1.833 |
| Intercept | -3.435 | 0.79 | 18.922 | 1 | 0 | 0.032 |
NOTES: df is degrees of freedom. S.D. is standard error. Likelihood ratio test: χ2 [4, n = 121] = 108.827, p <0.000. Cox & Snell R2: χ2 [4, n = 121] = .211, p <.000. Nagelkerke R2 = 0.299. Hosmer and Lemeshow test: χ2[8, n = 121] = 4.782, p =0.781.
SOURCE: Bonifas, R.P., Arizona State University, 2008; and Online Survey and Certification Reporting System (OSCAR) data, 2002-2004.
Table 7. Model 2 Logistic Regression Results: Facility Receipt of a Deficiency in Medically-Related Social Services by Facility Structural Variables and Facility Culture Variables.
| B | S.E. | Wald | df | p | Exp(B) Odds Ratio | |
|---|---|---|---|---|---|---|
| Step 1: Facility Structure | ||||||
| Ownership Turnover | 0.111 | 0.108 | 1.064 | 1 | 0.302 | 1.118 |
| Facility Location | 2.020 | 0.654 | 9.540 | 1 | 0.002 | 7.540 |
| SSD Caseload | 0.018 | 0.008 | 5.319 | 1 | 0.021 | 1.018 |
| Ownership Status | 0.538 | 0.751 | 0.513 | 1 | 0.474 | 1.713 |
| Step 2: Facility Culture | ||||||
| SSD Job Autonomy | -0.043 | 0.094 | 0.206 | 1 | 0.650 | 0.958 |
| SSD Job Influence | -0.027 | 0.090 | 0.089 | 1 | 0.766 | 0.974 |
| Support for Negotiating Conflict | 0.049 | 0.081 | 0.366 | 1 | 0.545 | 1.050 |
| Sufficient time to complete work | -0.285 | 0.256 | 1.241 | 1 | 0.265 | 0.752 |
| Intercept | -3.339 | 2.235 | 2.231 | 1 | 0.135 | 0.035 |
NOTES: df is degrees of freedom. S.D. is standard error. SSD is social service director. Likelihood ratio test: χ2 [4, n = 121] = 105.122, p <0.000. Cox & Snell R2: χ2 [4, n = 121] =0.237, p =0.000. Nagelkerke R2 = 0.336. Hosmer and Lemeshow Test: χ2[8, n = 121] = 6.006, p =0.640.
SOURCE: Bonifas, R.P., Arizona State University, 2008; and Online Survey and Certification Reporting System (OSCAR) data, 2002-2004.
Discussion
Limitations
These findings need to be interpreted in light of limitations. Given the cross-sectional nature of the study design, causation cannot be inferred; thus, the direction of the relationships underlying the previously mentioned group differences are unclear. For example, it cannot be determined from this analysis whether lower job autonomy and influence contribute to negative psychosocial care outcomes or negative psychosocial care outcomes contribute to SSDs having lower job autonomy and influence. Further research is needed to clarify the direction of these relationships and to delineate the exact sources of influence.
An additional limitation is posed by the time lag between the collection of facility inspection data for OSCAR and the collection of SSD data via the questionnaire. Data for State survey investigations utilized in this research were collected between January 2002 and December 2004; data for the SSD questionnaire were collected early in 2006. Due to this discrepancy, a portion of the sample was not employed by their corresponding facilities when the State survey investigations took place. Indeed, 25 percent of the sample fall into this category, reporting hire dates after December 2004, which brings into question the true strength of the group differences identified. In further support of these findings, however, repeat analysis excluding respondents hired before December 2004 generated the same statistical results.
Implications
These findings provide preliminary evidence from one State that work environment factors affect the quality of social service provision in SNFs as measured by survey deficiencies in medically-related social services. SSDs working in non-metropolitan facilities and those with larger caseloads appear to experience the most difficulty providing effective psychosocial care. Addressing these issues will require a combination of interventions at the regulatory level and at the individual facility level.
This study found that during a 3-year period, 34 out of 121 SNFs, or 28 percent, received deficiencies in medically-related social services. However, this may be a finding specific to Washington State as other researchers using multi-State samples have found lower levels of deficiencies in psychosocial service related areas. For example, the previously mentioned U.S. Department of Health and Human Services (2003) study found only 15 percent of facilities received deficiencies in psychosocial services and such deficiencies represented just 4 percent of deficiencies overall. Indeed, State surveyors reported that they do not routinely assess facility compliance in all areas of psychosocial services (U.S. Department of Health and Human Services, 2003). Given that medically-related psychosocial services tend to be underscrutinized by State surveyors, one method to address the concerns generated by the current study is to instruct State survey staff to give more attention to this area, especially in facilities at high risk for negative outcomes, such as those in non-metropolitan areas and those with SSDs who have a large caseload (more than 73 residents). A caution is warranted here, however, in that care must be taken to ensure that individual SSDs do not become scapegoats for system-level problems. Rather, surveyors need to stipulate that facility plans of correction focus on facility cultural change. For example, SSD job descriptions could be revised to maximize the time devoted to the provision of psychosocial services that target commonly unmet resident needs. Such unmet needs often occur in more clinically-related areas such as depression, behavioral symptoms, and adjustment to role changes (DHHS, 2003); additional blocks of time might be shifted toward psychosocial services by limiting social service professionals' involvement in non-clinical tasks that other professionals are positioned to handle. For example, business office personnel might assist residents and families with Medicaid and Medicare procedures and housekeeping professionals might assist residents in locating missing possessions or obtaining personal items.
The negative influence of larger caseload size could also be addressed via regulatory change. Current Federal regulations stipulate that facilities with 120 beds or more must employ a qualified full time social worker4; facilities with fewer beds are still required to provide medically-related social services, but do not have to employ a qualified social worker full time. Given that 70 percent of SNFs in the U.S. have less than 120 beds, Federal regulations regarding the 120-bed rule have been described as insufficient and are considered a factor contributing to unmanageable caseload size (Vourlekis et al., 1992a; Gleason-Wynn and Mindel, 1999; Parker-Oliver and Kurzejeski, 2003; Simons, 2006). Yet, convincing evidence linking social work staffing levels to resident outcomes that would support revision of the 120-bed rule have not been available (Vourlekis, Zlotnik, and Simons, 2005; Simons, 2006). This study's findings offer preliminary support for revising the 120-bed rule since results indicate that, at least in one State, larger caseload size (more that 73 residents) is associated with facility receipt of a deficiency in medically-related social services. Additional research is needed using multi-State samples to assess the generalizability of these results.
In terms of facility location, a combination of regulatory enhancements and facility cultural change efforts are indicated. For example, facilities that have greater access to and utilize community collaborators, such as mental health agencies, score higher on measures of quality (Bravo et al., 1999). Due to their remote location, facilities in non-metropolitan areas have less access to collaborative resources. As such, intervention efforts focused on enhancing access to collaborative opportunities could extend social service professionals' ability to provide medically-related psychosocial services. Such intervention might take the form of devising regulatory incentives for mental health agencies and individual clinicians to provide services to rural facilities or targeting well elders in the community to serve as sources of informal support for facility residents under the supervision of the SSD. Similarly, collaboration could be fostered in-house by nurturing stronger partnerships across disciplines, for example, between social service professionals and activity professionals to incorporate therapeutic-centered groups into regular facility event schedules.
Footnotes
Not all persons providing psychosocial services in SNFs have formal education in social work; thus this article refers to these individuals as social service professionals.
The author is with Arizona State University. The research in this article was supported by a grant from the John A. Hartford Foundation (Grant Number 800584). The statements expressed in this article are those of the author and do not necessarily reflect the views or policies of Arizona State University, the John A. Hartford Foundation, or Centers for Medicare & Medicaid Services (CMS).
Additional information is available at: http://www.ers.usda.gov/data/RuralUrbanContinuumCodes/
Additional information is available at: http://www.adsa.dshs.wa.gov/Professional/NFDir/directory.asp
A qualified social worker is defined as someone with a bachelor's or masters degree in social work or a related field and at least 1-year of experience in a health care setting.
Reprint Requests: Robin P. Bonifas, Ph.D., M.S.W., Arizona State University, College of Public Programs/School of Social Work, 411 N Central Ave. #800, Phoenix, AZ 85004. E-mail: robin.bonifas@asu.edu
References
- Aaronson WE, Zinn JS, Rosko MD. Do For-Profit and Not-for-Profit Nursing Homes Behave Differently? The Gerontologist. 1994;34(6):775–786. doi: 10.1093/geront/34.6.775. [DOI] [PubMed] [Google Scholar]
- Anderson RA, Corazzini KN, McDaniel RR. Complexity Science and the Dynamics of Climate and Communication: Reducing Nursing Home Turnover. The Gerontologist. 2004;44(3):378–388. doi: 10.1093/geront/44.3.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson RA, Issel LM, McDaniel RR., Jr Nursing Homes as Complex Adaptive Systems: Relationship Between Management Practice and Resident Outcomes. Nursing Research. 2003;52(1):12–21. doi: 10.1097/00006199-200301000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banaszak-Holl M, Berta WB, Bowman DM, et al. The Rise of Human Service Chains: Antecedents to Acquisitions and Their Effects on the Quality of Care in U.S. Nursing Homes. Managerial and Decision Economics. 2002;23(4/5):261–282. [Google Scholar]
- Bonifas RP. Multi-Level Factors Related to Deficiencies in Psychosocial Care in Washington State Skilled Nursing Facilities. Dissertation Abstracts International Section A: Humanities and Social Sciences. 2008;68(8-A):3588. [Google Scholar]
- Bravo G, DeWals P, Dubois M, et al. Correlates of Care Quality in Long-Term Care Facilities: A Multilevel Analysis. Journals of Gerontology. 1999;54B(3):180–188. doi: 10.1093/geronb/54b.3.p180. [DOI] [PubMed] [Google Scholar]
- Castle NG. Administrator Turnover and Quality of Care in Nursing Homes. The Gerontologist. 2001;41(6):757–767. doi: 10.1093/geront/41.6.757. [DOI] [PubMed] [Google Scholar]
- Castle NG. Nursing Home Closures, Changes in Ownership, and Competition. Inquiry. 2005;42(3):281–292. doi: 10.5034/inquiryjrnl_42.3.281. [DOI] [PubMed] [Google Scholar]
- Castle N, Myers S. Mental Health Care Deficiency Citations and Nursing Home Staffing. Administration and Policy in Mental Health and Mental Health Services Research. 2006;33(2):215–225. doi: 10.1007/s10488-006-0038-2. [DOI] [PubMed] [Google Scholar]
- Dane BO, Simon BL. Resident Guests: Social Service Professionals in Host Settings. Social Work. 1991;36(3):208–213. [Google Scholar]
- Dillman DA. Mail and Internet Surveys: The Tailored Design Method. 2nd Edition. John Wiley and Sons, Inc.; New York: 2000. [Google Scholar]
- Fiske H. Nursing Home Social Work: Turnover Turmoil. Social Work Today. 2002;2(19):10–12. [Google Scholar]
- Gleason-Wynn P, Mindel H. A Proposed Model for Predicting Job Satisfaction Among Nursing Home Social Service Professionals. Journal of Gerontological Social Work. 1999;32(3):65–79. [Google Scholar]
- Harrington C, Woolhandler S, Mullan J, et al. Does Investor-Ownership of Nursing Homes Compromise the Quality of Care? International Journal of Health Services. 2002;32(2):315–325. doi: 10.2190/EBCN-WECV-C0NT-676R. [DOI] [PubMed] [Google Scholar]
- Harrington C, Zimmerman D, Karon SL, et al. Nursing Home Staffing and Its Relationship to Deficiencies. Journal of Gerontology. 2000;55B(5):S278–S287. doi: 10.1093/geronb/55.5.s278. [DOI] [PubMed] [Google Scholar]
- Kruzich J. Ownership, Chain Affiliation and Administrator Decision-Making Autonomy in Long-Term Care Facilities. Administration in Social Work. 2005;29(1):5–24. [Google Scholar]
- Kruzich JM, Powell WE. Decision-Making Influence: An Empirical Study of Social Service Professionals in Nursing Homes. Health and Social Work. 1995;20(3):215–222. doi: 10.1093/hsw/20.3.215. [DOI] [PubMed] [Google Scholar]
- Lee RH, Gajewski BJ, Thompson S. Reliability of the Nursing Home Survey Process: A Simultaneous Survey Approach. The Gerontologist. 2006;46(6):772–780. doi: 10.1093/geront/46.6.772. [DOI] [PubMed] [Google Scholar]
- O'Neill J. NASW News. Washington D.C.: Apr, 2002. Inappropriate Tasks, Lax Reinforcement, High Turnover: Nursing Home Social Work in Doldrums. National Association of Social Service Professionals. [Google Scholar]
- National Association of Social Workers. Standards for Social Work Services in Long-Term Care. National Association of Social Workers; Washington, D.C.: 2003. [Google Scholar]
- Parker-Oliver D, Kurzejeski LS. Nursing Home Social Services: Policy and Practice. Social Work. 2003;42(2):37–50. [Google Scholar]
- Peng CJ, Lee KL, Ingersoll GM. An Introduction to Logistic Regression Analysis and Reporting. The Journal of Education Research. 2002;96(1):3–14. [Google Scholar]
- Simons KV. Organization Characteristics Influencing Nursing Home Social Services Directors' Qualifications: A National Study. Health and Social Work. 2006;31(4):266–274. doi: 10.1093/hsw/31.4.266. [DOI] [PubMed] [Google Scholar]
- Tirrito T. Mental Health Problems and Behavioral Disruptions in Nursing Homes: Are Social Service Professionals Prepared to Provide Needed Services? Journal of Gerontological Social Work. 1996;27(1/2):73–86. [Google Scholar]
- U.S. Department of Health and Human Services, Office of Inspector General. Psychosocial Services in Skilled Nursing Facilities. 2003 Internet address: http://www.oig.hhs.gov/oei/reports/oei-02-01-00610.pdf (Accessed 2009.)
- Vourlekis BS, Gelfand DE, Greene RR. Psychosocial Needs and Care in Nursing Homes: Comparison of Views of Social Service Professionals and Home Administrators. The Gerontologist. 1992a;32(1):113–119. doi: 10.1093/geront/32.1.113. [DOI] [PubMed] [Google Scholar]
- Vourlekis BS, Greene RR, Gelfand DE, et al. Searching for the Doable in Nursing Home Social Work Practice. Social Work in Health Care. 1992b;17(3):45–70. doi: 10.1300/J010v17n03_04. [DOI] [PubMed] [Google Scholar]
- Vourlekis B, Zlotnik JL, Simons K. Evaluating Social Work Services in Nursing Homes: Toward Quality Psychosocial Care and Its Measurement. A Report to the Profession and Blueprint for Action. Institute for the Advancement of Social Work Research; Washington D.C.: 2005. [Google Scholar]