Abstract
In 2006, Florida's Medicaid reform required some Medicaid consumers to enroll in health plans that differed in terms of cost-sharing requirements and benefit limitations. In focus groups we found enthusiasm among Medicaid consumers for having choices among health plans; however, enthusiasm did not translate into comparison shopping for health plans. Survey findings suggested that Medicaid consumers had difficulty comprehending Medicaid healthplan comparison information, particularly if they were lower in numeracy or literacy skills. Given the number of plans offered and the numerous ways they differed, our efforts to simplify the comparison chart resulted in slightly higher comprehension, but only among those with higher skill levels. Our study suggests that policymakers should seek to simplify Medicaid Program information and design to encourage informed decisionmaking.
Introduction
To spend Medicaid dollars more efficiently, CMS has encouraged Medicaid directors to adopt value-driven health care (VDHC) initiatives. These initiatives include improving informational systems, providing health care cost and quality information to consumers, and developing incentives to encourage consumers to make high value health care choices (Smith, 2007). The intent is to catalyze Medicaid consumers to make cost-effective decisions to best meet their individual health care needs and preferences, which, in turn, is expected to control health care costs and raise quality.
Florida's Medicaid Program was one of the first to comprehensively embrace VDHC principles with its 2006 reform, although elements of this policy direction had already been implemented in other Medicaid Programs (Felt-Lisk et al., 2007; Greene, 2007; Milligan et al., 2006). One key component of Florida's reform was requiring beneficiaries to enroll in health plans that offered different additional benefits. For non-pregnant adults these plans additionally differed in terms of cost-sharing requirements and benefit limitations.1 A Medicaid agency document explained: “The standard state plan package is no longer considered the perfect fit for every Medicaid beneficiary, and the beneficiaries are getting new opportunities to engage in decision-making responsibilities relating to their personal health care” (Agency for Health Care Administration, 2008).
Inherent in Florida's Medicaid reform, and in the larger VDHC policy direction, is the assumption that, when consumers are provided with comparative information and differentiated choices, they will make more informed health care decisions. In the context of Florida's Medicaid reform, consumers are expected to weigh the differences in health plan benefits and costsharing requirements in order to select the health plan that best meets their needs. In the first year of the program, which operated in two counties, this meant choosing from among 13 and 7 plans in Broward and Duval Counties, respectively.
Some have questioned how well equipped vulnerable populations like Medicaid consumers are to take advantage of health care report cards (Davies, Washington, and Bindman, 2002; Rice, 2003). According to the 2003 National Assessment of Adult Literacy, Medicaid consumers have health literacy levels approximately 80 percent the level of those with employer-sponsored health insurance (Kutner et al., 2006). Most Medicaid consumers (60 percent) have either basic or below basic health literacy, which means they are not able to use charts and graphs for tasks such as determining the healthy weight range for someone given their height, or the age at which a child should receive a vaccine.
Not surprisingly, there is a linkage between skills in literacy, numeracy (the ability to reason with numbers and other mathematical concepts), or health literacy (which combines literacy and numeracy in a health context) and consumers' ability to comprehend health-related information and make informed choices. Studies have found, for example, that those with lower skill levels were less likely to comprehend quality differences between hospitals, to understand prescription drug warning labels, and to distinguish the differences between a health savings account plan and a traditional health plan (Davis et al.; 2006, Greene, Hibbard, and Tusler, 2005; Greene et al., 2008; Hibbard et al., 2007; Peters et al., 2007).
Little research has focused specifically on how well Medicaid consumers make informed health care choices. One study found that Medicaid consumers were less likely to use comparative plan information than those with private coverage (63 versus 80 percent) and that they were considerably less sure of their health plan choice (Farley Short et al., 2002). In two fieldbased experiments, researchers found that sending quality health plan report cards did not influence Medicaid consumer health plan choices (Farley et al., 2002a; Farley et al., 2002b). In one of the studies, those consumers who reported reading the quality report did, however, make higher quality plan choices.
Recent evidence from Florida's Medicaid reform suggests that Medicaid consumers had very low awareness and knowledge of the Medicaid reform program early in the program's implementation (Coughlin et al., 2008). More than one-quarter (29 percent) of those surveyed soon after enrollment were not aware that they were enrolled in a Medicaid Reform health plan. Of those aware, almost one-quarter (22 percent) reported that the State assigned them to a plan because they did not choose one themselves. The majority (55 percent) agreed with the statement that it was “hard to understand information about plans” and very few (less than 1 in 10) knew even approximately how many health plans were offered to them.
This mixed mode study, combining qualitative and quantitative research, builds on this prior research, investigating in greater detail consumers' health plan decisionmaking process and identifying factors that inhibited informed decisionmaking. Using qualitative methods, we explored the factors consumers considered in selecting a health plan and the reasons why so many did not make a health plan choice. Using quantitative methods we examined three possible factors that may have inhibited informed decisionmaking. The first two were the role of literacy and numeracy in influencing comprehension of the Florida Medicaid reform health plan comparison chart. We hypothesized that higher numeracy scores would be associated with greater comprehension in this relatively low-education Medicaid sample after controlling for literacy. We also hypothesized the higher literacy scores would be associated with greater comprehension, adjusting for differences in numeracy.
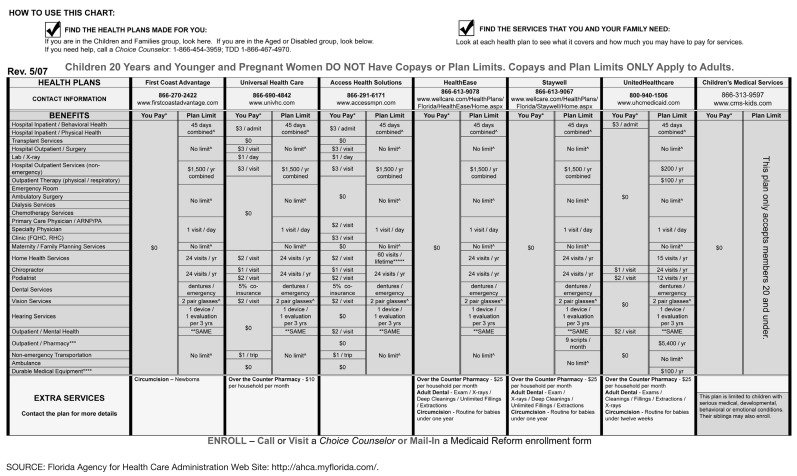
The third factor was the complexity of the Medicaid health plan comparison chart. The official Medicaid health plan comparison chart in Duval County (includes the City of Jacksonville) was complex, with seven plans compared across 27 attributes. The font size in the chart was smaller than is recommended by low literacy guidelines and the structure was complex with information on copayments and benefit limitations nested in two columns under each plan (Figure 1) (Doak, Doak, and Root, 1996). Prior experimental studies have found that providing simpler information can result in higher consumer comprehension and more high value choices (Gerteis et al., 2007; Hibbard et al., 2001; Hibbard et al., 2002; Peters et al., 2007). We sought to simplify the presentation based on low literacy principles in order to test whether a revised version containing the same information would result in higher comprehension levels. We hypothesized that a less complex chart would result in greater comprehension of information, however, we were unsure whether the complexity reduction would be sufficient to help the less skilled or whether it might only help the higher skilled enrollees.
Figure 1. Actual Medicaid Reform Plan Comparison Chart for Duval County, Florida.
Methods
Qualitative Methods
The qualitative component examined consumer attitudes and experiences with Medicaid reform health plan informed decisionmaking. A total of six focus groups were conducted (n=59) with Medicaid consumers, who either were adult Medicaid beneficiaries themselves or had children who received Medicaid. Participants were recruited through flyers at public and nonprofit housing organizations for low income families in Duval County, Florida (one of the two counties that initiated Medicaid reform in 2006).
The focus group discussions centered on participants' health plan decisionmaking process, their attitudes toward health plan choice, and for those who did not select a plan—the reasons for not making a selection. The sessions were conducted in June, 2007, which was 10 months after Medicaid reform began its incremental enrollment process. Each session lasted 1 hour, and individuals received $15 for participating in a focus group.
The focus groups were audiotaped and fully transcribed. The transcribed interviews were each reviewed several times by the first author in order to identify themes derived from the data. Verbatim text blocks that corresponded to each theme were identified. These text blocks were then subsequently reviewed to identify subthemes and to refine concepts. We did not attempt to analyze differences in responses by subgroups.
Quantitative Methods
We used an experimental survey design to test whether simplifying the official Medicaid comparison chart improved comprehension, and to examine how important literacy and numeracy skills were for comprehension. We recruited a convenience sample of 122 participants through posting flyers at public and non-profit housing organizations in Duval County, Florida. This group included most, but not all of the focus group participants.2 In order to participate, consumers had to be at least age 18 and had to either receive Medicaid themselves or have children receiving Medicaid. Participants completed a paper and pencil survey, which took approximately 20 minutes, and they received $8 for participation.
Respondents were given one of two versions of the Medicaid health plan comparison chart. We alternated which version was distributed to assure randomization. With randomization, differences in comprehension on the two versions of the comparison chart could be attributed to the charts, and not to differences in time of day or similarity among individuals who arrived together. One-half of the participants received a black and white copy of the actual chart used by Florida Medicaid in Duval County (version 5/2007), which compared 7 health plans. The comparison chart, shown in Figure 1, compares the plans' health coverage benefits across 27 different areas (e.g. primary care physician, hospital inpatient, emergency room, and extra services). Benefit information for each plan was nested in two columns, one for cost-sharing requirements and the other for benefit limitations. Plan contact information was also listed. The font size for the comparison chart is 7. The official plan comparison chart was assessed as being appropriate for people with 15 years of education or more according to the Mosenthal and Kirsch's (1998) document complexity assessment. This readability assessment examines a chart's structure for complexity (i.e., whether the information is in one column, multiple columns, intersected columns and rows, or a nested information within columns) and its density (i.e., the number of labels and items).
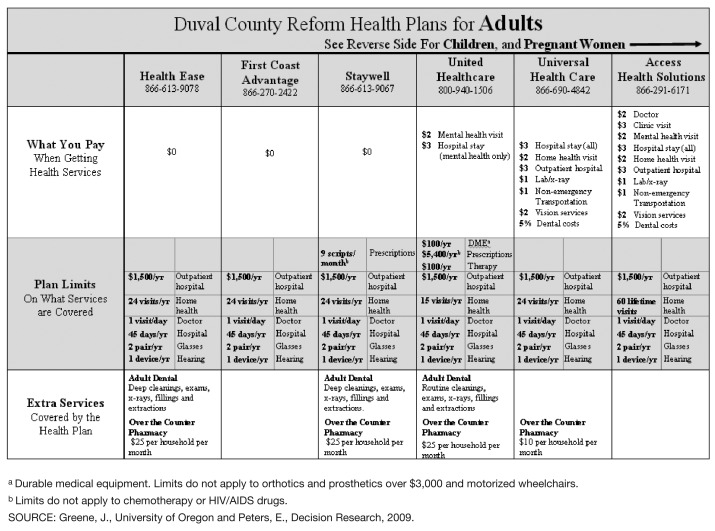
The other one-half of participants received a version of the plan comparison chart that the authors revised to reduce complexity and increase readability, while at the same time maintaining the differences between plans included in the original chart (Figure 2). We made four key changes, which were based on principles for increasing readability for people with low literacy skills (Doak, Doak, and Root, 1996; Hibbard et al., 2002; Mosenthal and Kirsch, 1998). First, rather than listing all 27 benefit areas, only those areas where there were differences among plans were listed. Second, instead of nesting information on cost-sharing and benefit limitations for each plan in separate columns, cost-sharing information was presented in one row and benefit limitations in another. Third, the plans were arranged from most generous to least generous based on costsharing and extra benefits, rather than alphabetically. Fourth, the font size was increased from size 7 to 10, with labels as large as size 13 font. With these changes, the revised chart was still complex because of the number of plans and areas on which they were assessed. It was assessed as being appropriate for readers with at least a high school degree. To further reduce the complexity, we would have had to abandon our goal of creating a chart that preserved all the differentiating information included in the original chart.
Figure 2. Revised Medicaid Reform Plan Comparison Chart for Duval County, Florida.
Respondents were provided with one version of the health plan comparison chart (either the original or the revision) and asked to answer nine comprehension questions. Six of the questions asked respondents to identify specific information from the chart. The following examples illustrate this set of questions: “How much do adults enrolled in Access Health Solutions have to pay for a clinic visit?” and “How many pairs of glasses can adults get in First Coast Advantage each year?” The remaining three questions asked respondents to synthesize the information across the plans to identify the plan with “the most generous benefits”, “the most limits on the services it covers for adults”, and the plan that “requires adult members to pay ($1-$3) for the most medical services”. Respondents were asked to select the one correct answer from a listing of six or seven possible response options. Such items tailored specifically to the information provided are often used to assess comprehension in health and health-related studies (Peters et al., 2007) when comprehension of specific provided information for use in decisions is the goal rather than understanding of general concepts (in which case a more generic scale validated in previous research could be used).
We then developed a comprehension index based on the number of correct answers to the nine comprehension questions. Because some comprehension items required identifying specific information from the chart while others required synthesizing differences across all plans, we also created two subindices to test whether consumer skills or the revised chart would be related more to one subindex than another. We hypothesized that numeracy would be more important for synthesizing information across the chart since more complex processing was required, and that the revised chart, in which plans were ordered by generosity, would have a greater impact on synthesizing information.
The identifying subindex included the six items that required identifying specific information from the chart. These items had a high level of reliability (Cronbach's alpha= 0.74). The synthesizing subindex included three items, though, the reliability was low (Cronbach's alpha= 0.35). This is likely due to the fact that the synthesizing tasks were more complex, required a greater assortment of skills, were answered incorrectly by most participants (resulting in a floor effect that could have attenuated correlations between items), as well as the fact that there were fewer items.
Participants also completed numeracy and literacy assessments. The numeracy assessment used was an 8-item subjective assessment that included questions such as: “How good are you at calculating a 15 percent tip?” and “When reading the newspaper, how helpful do you find tables and graphs that are parts of a story?” This subjective numeracy assessment is highly correlated with objective measures of numeracy, and research subjects have found it less stressful to complete (Fagerlin et al., 2007). To assess reading literacy, we used a part of the Test of Functional Health Literacy (Passage B) as has been done by prior authors (Gazmararian, Parker, and Baker, 1999; Greene et al., 2008). This passage tests literacy by using the Cloze procedure. The Cloze procedure tests whether a person can identify words that are missing from a passage of text. In this task, 20 words were missing from a passage on Medicaid and participants had to select which was the most appropriate of four words to fill the blank.
Experimental Study Analysis
The analysis began with basic descriptive statistics of the overall sample and comparative characteristics of the two randomized groups.
Next, we conducted factorial ANOVA tests, which simultaneously tested our three hypotheses that numeracy skill would be predictive of higher comprehension, that the revised version of the comparison chart would be predictive of higher comprehension; and finally, that the revised comparison chart would assist comprehension among more skilled (numerate or literate). We dichotomized subjective numeracy at the median score for our sample (4.3 on scale from 1 to 6). We conducted comparable analysis for literacy skills, dichotomizing literacy at its median (18 on a scale from 0 to 20).
We then conducted multivariate regression models to test the independent effects of numeracy, literacy, and plan comparison chart version on the comprehension index and its two subindices. Again, numeracy and literacy were dichotomized in these models.
To examine whether the impact of the revised comparison chart differed based on skill level, we tested whether models that included an interaction either between literacy and plan-comparison chart type or between numeracy and plan-comparison chart type improved the predictive power of the models. When the interaction provided a significant improvement in the R-square (at p<0.10), we presented the interaction model rather than the base model.
Findings
Study participants were mostly women (78 percent) and between the ages of 18 and 34 (57 percent), as is shown in Table 1. The sample was overwhelmingly African-American (90 percent), substantially underrepresenting White Medicaid consumers (Bureau of the Census, 2000). Consistent with the low socio-economic status of Medicaid consumers, respondents' education attainment was relatively low. One-quarter (26 percent) had less than a high school degree, which was comparable to a random sample of Medicaid beneficiaries surveyed from Duval and Broward Counties (Coughlin et al., 2008). The health status was also similar to that found in Coughlin and colleagues' study although our sample had fewer people in fair or poor health. This difference is likely due to the fact that our survey was conducted in person in common areas of a housing complex rather than by telephone in participants' home and suggests that our sample may be higher functioning than the Florida Medicaid population as a whole.
Table 1. Characteristics of the Experiment Sample and of the Two Experimental Groups.
| Characteristics | Total Sample | Experimental Group | |
|---|---|---|---|
|
| |||
| Original Comparison Chart | Revised Comparison Chart | ||
|
| |||
| (n=122) | (n=59) | (n=63) | |
| Percent | |||
| Socio-Demographics and Health | |||
| Sex | |||
| Female | 77.9 | 72.9 | 82.5 |
| Male | 22.1 | 27.1 | 17.5 |
| Age | |||
| 18-34 | 57.3 | 63.6 | 51.6 |
| 35-44 | 18.8 | 10.9 | 25.8 |
| 45-64 | 23.9 | 25.5 | 22.6 |
| Race/Ethnicity | |||
| Black | 90.2 | 89.8 | 90.5 |
| White | 4.9 | 6.8 | 3.2 |
| Other | 4.9 | 3.4 | 6.3 |
| Education | |||
| Less than High School Degree | 25.6 | 22.0 | 29.0 |
| High School Diploma or GED | 41.3 | 47.5 | 35.5 |
| Some College/Trade School | 30.6 | 28.8 | 32.3 |
| College Graduate | 2.5 | 1.7 | 3.2 |
| Health Status | |||
| Excellent/Very Good | 52.1 | 53.4 | 50.8 |
| Good | 31.4 | 34.5 | 28.6 |
| Fair/Poor | 16.5 | 12.1 | 20.6 |
| Medicaid Recipient | |||
| Children | 20.4 | 18.9 | 21.7 |
| Self | 17.7 | 20.8 | 15.0 |
| Children and Self | 61.9 | 60.4 | 63.3 |
| Skill Level | |||
| Literacy | |||
| Higher (Score of 19 or 20) | 43.4 | 42.4 | 44.4 |
| Lower (Score 18 or Lower) | 56.6 | 57.6 | 55.6 |
| Subjective Numeracy | |||
| Higher (Score of 4.3 to 6) | 46.2 | 43.9 | 48.4 |
| Lower (Score of 1 up to 4.3) | 53.8 | 56.1 | 51.6 |
NOTE: None of the differences between experimental groups was statistically significant.
SOURCE: Greene, J., University of Oregon and Peters, E., Decision Research, 2009.
We found no statistically significant differences in demographics or in skill level (literacy or numeracy) between those randomized to the two experimental groups. As a result and given the limited sample size, we did not control for demographics in multivariate analysis.
Attitude and Experience with Plan Choice
Focus group participants responded positively to the idea of having health plan options. One participant said, “Having more than one choice is always good,” and another explained, “You get a choice to choose who you want to work for you.” Appreciating having choices among health plans, however, was not the same as comparison shopping for health plans.
Very few participants described comparing the benefits and costs of the different health plans. Participants' appreciation of plan choice, instead, appeared to be grounded in a desire to switch health plans if there was a problem with their existing plan. One woman, who was particularly vocal about the benefits of health plan choice, but who let Medicaid make the health plan choice for her explained, “…if something don't go right or my doctor should change and he don't take HealthEase no more, I can always say, ‘hey, what [are] you taking?’”
Just over one-half of the focus group participants said that they had selected a Medicaid health plan, which is slightly lower than the 68 percent voluntary selection rate for Medicaid reform in its first year in both Broward and Duval Counties (Agency for Health Care Administration, 2008). Most who actively made a choice reported that they either decided to stay enrolled in their existing health plan or that they selected a health plan in order to continue seeing a specific doctor. “It was more important to me that their [the children's] doctor was using the plan, so it was like whatever comes with the plan was [okay],” one participant explained. Several also mentioned picking the plan because doctors were close by: “I chose it [health plan] because it's more accessible….I didn't have to go across town to get there, just down the street.”
Although these are valid reasons for wanting to have health plan choices, they are not consistent with value-driven health care since they are not catalyzing improved health care quality or reduced costs. Only a handful of participants reported comparing the health plans based on their different benefits and cost-sharing requirements. Of them, several described sticking with their existing plan or doctor because the differences in health plans were not too great. “I was already on Health Ease when I got the form. I was going to change but when I was looking through it, comparing what services, co-payments… that mainly helped me decide that I would stay on it,” explained one participant. Another said, “I stayed with Health Ease because the difference was so small and I had been with Health Ease for so long. I just stayed there with Health Ease.” It was very rare that a participant could identify a specific plan characteristic that drew them to the plan. In one case when that happened, a woman said she had selected a plan because it offered $25 a month in over-the-counter pharmacy products, yet two other plans offered the same benefit.
Reasons for Not Making a Plan Selection
Almost one-half of the participants reported that Medicaid assigned them to a health plan, and their reasons fell into one of three areas. Most commonly, participants said that they just didn't get around to making the decision: “Every day you'd say, I'm gonna get to that, and it gets to you first,” and “I guess I just let it go past the time so they picked it for me.”
Others described trusting Medicaid to make the best choice for them and simply appreciating that they had health coverage: “So I said I'll take a chance with what they give me and if I don't like it I'll call them back. But they did all right,” and “I just took whatever they gave me and was grateful.” A third group shared a related sentiment, that as long as Medicaid provided health coverage they were not interested in the specifics: “As long as the card is active and when I go to the doctor they don 't say ‘no, this is not active,’ I'm fine. I don't want to read much more.”
A number of focus group participants commented on being overwhelmed or annoyed by the Medicaid mailing, which may have been a factor in putting off making a plan selection. One woman said, “Don't send the whole book. I hated reading books in school let alone reading [about Medicaid health plans].” Others commented that the materials were not targeted specifically for them; “You only need one piece of paper, but you got 15 of them, [some] basically don't really pertain to you.”
Impact on Comprehension
Consumer comprehension of the information contained in the plan comparison chart was generally poor. On average, respondents correctly answered fewer than one-half of the nine comprehension questions correctly (mean of 4.3) and only 2 percent correctly answered all nine questions. The percent of questions correctly answered was higher for the identifying subindex (56 percent), than for the synthesizing subindex (30 percent).
Numeracy skill was strongly predictive of the comprehension index and its two subindices. Less numerate participants had total comprehension scores that were 30 percent lower than more numerate participants (3.6 compared to 5.1 out of 9 possible, data not shown). The gap in scores was even greater for the synthesizing subindex, consistent with these items requiring more complex processing of numeric information. Although comprehension was low for both groups, the less numerate participants had scores one-half the level of the higher numerate (0.6 compared to 1.2 items answered correctly out of a possible 3).
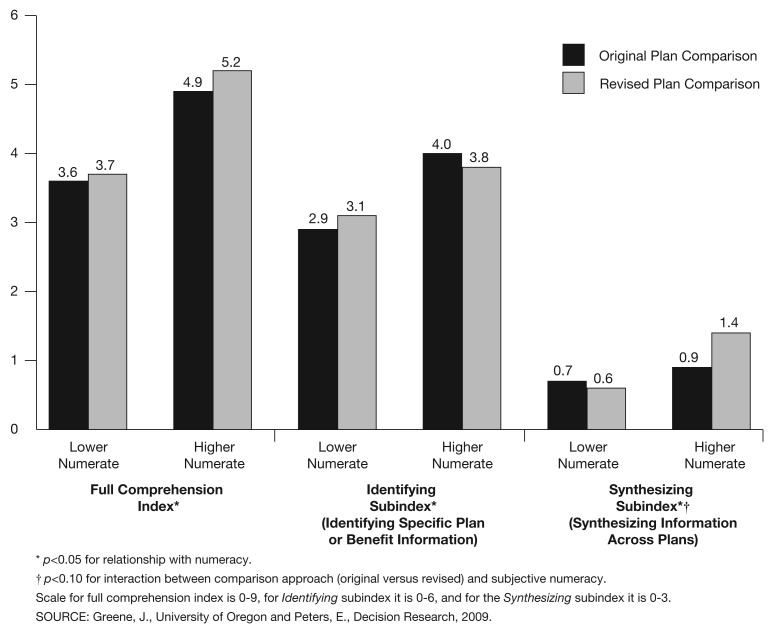
In factorial ANOVA tests, the revised plan comparison chart did not result in higher comprehension levels on the full index or on the identifying subindex (Figure 3). For the synthesizing subindex, however, the revised plan comparison chart almost doubled the comprehension score for the higher numerate participants but not the less numerate. Among the higher numerate, 1.5 questions (out of 3) were correctly answered on average when viewing the revised chart, compared to 0.9 with the actual chart. Not breaking up the items into the two different types of comprehension items would have resulted in our missing this effect. Further analyses were conducted only on the two separate subindices.
Figure 3. Influence of Subjective Numeracy and Plan Comparison Approach (Original Versus Revised) on the Full Comprehension Index, the Identifying Subindex, and the Synthesizing Subindex.
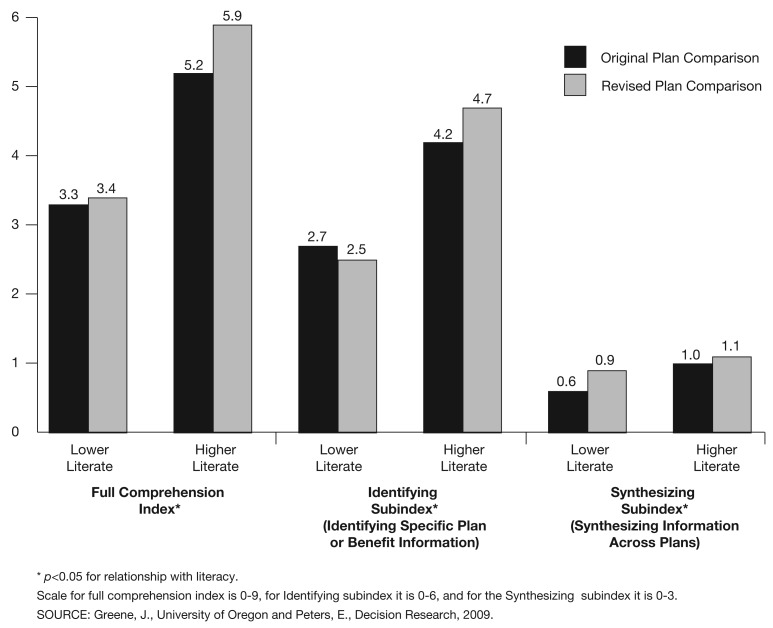
Literacy skill was also strongly related to the identifying subindex, but not to the synthesizing subindex. Lower literate participants had scores on the identifying subindex that were 42 percent lower than the higher literate participants (2.6 versus 4.5 out of 6 possible). Although Figure 4 shows a trend that the revised plan comparison chart resulted in higher identifying subindex scores for higher rather than lower literate participants, this relationship was not statistically significant.
Figure 4. Influence of Literacy and Plan Comparison Approach (Original Versus Revised) on the Full Comprehension Index, the Identifying Subindex, and the Synthesizing Subindex.
In multivariate analyses, we found that both literacy and numeracy skills were independent predictors of the identifying subindex (Table 2, column 2). The revised plan comparison chart had no impact for lower literacy readers. Among those with higher literacy, however, it appeared to result in comprehension levels 0.6 points higher on the subindex than for those viewing the original chart [-0.4(revised chart coefficient)+1.0 (revised chart and higher literacy coefficient)=0.6].
Table 2. Multivariate Regression Models Examining Literacy, Numeracy, Plan Comparison Approach, and Interactions Between Skill Level and Chart Approach.
| Regression Coefficients | ||
|---|---|---|
|
| ||
| Identifying Subindex | Synthesizing Subindex | |
| Literacy | ||
| Lower | — | — |
| Higher | 1.3** | 0.3* |
| Subjective Numeracy | ||
| Lower | — | — |
| Higher | 0.6* | 0.2 |
| Plan Comparison Chart | ||
| Original | — | — |
| Revised | -0.4 | -0.1 |
| Interactions | ||
| Revised Chart * Higher Literacy | 1.0† | — |
| Revised Chart * Higher Numeracy | — | 0.7* |
| Adjusted R2 | 0.28 | 0.14 |
<0.10.
p<0.05.
p<0.01.
p<0.001.
NOTES: Interaction terms were included if they improved the model's R2 over the base model at the p<0.10 level.
SOURCE: Greene, J., University of Oregon and Peters, E., Decision Research, 2009.
We see a similar pattern for the synthesizing subindex. Again, the revised chart does not benefit those with low skills, in this case numeracy skills. Yet, it aids those with higher skills—boosting their scores by 0.6 points on the subindex compared to those viewing the original chart. It is notable that the full regression model for this index has approximately half of the predictive power as that for the identifying subindex. The low R-squared may be due to having less power because we used a subjective numeracy scale (where scores are based on perceptions of one's own number skills) rather than an objective one (where math skill is tested).
Discussion
In 2006, Florida's Medicaid reform required consumers in two counties to enroll in health plans that differed in terms of benefits, cost-sharing requirements, and additional services. The intent was to provide consumers with true choices among health plans so they could find the best fit for their individual needs, which in turn would create competition for higher quality, more generous health plans. This study examined consumer experiences making health plan choices and examined barriers to consumers' comprehension of the health plan comparison charts used in the Medicaid Program.
Our focus group participants reported having done little of the type of comparison shopping for health plans envisioned by policymakers. The health plan characteristics that participants said influenced their decisions were physician location, physician network, and prior enrollment in the plan. Although these are important considerations, only a handful said they had compared the plans' cost sharing requirements, benefits, or extra services when selecting a plan. This suggests that voluntary choice, which is often used as an indicator of informed decisionmaking, may overstate how informed health care decisions in fact are.
Our survey results uncovered several reasons for the lack of proactive choice of plan and further undermined the notion that informed decisionmaking was taking place. Specifically, we found that Medicaid consumers in this study had very low comprehension of the Medicaid agency's health plan comparison chart. On average, consumers were able to correctly answer one-half of the questions related to the chart material. They were more able to answer questions that asked them to identify specific information from the chart (e.g., about one plan or one benefit) than they were to answer questions requiring them to synthesize information across all plans (e.g., to identify the most generous plan). It is, however, this latter skill that consumers need to size up which health plan best meets their needs.
This study also sheds light on a possible route towards helping at least some Florida Medicaid consumers make more fully informed health plan choices. The usual information provided on health plan choices was very complex. The chart the Medicaid agency provided was assessed as being readable for people with at least 15 years of education, when most Medicaid consumers have health literacy skills assessed as basic or below basic. We sought to simplify the plan comparison chart while maintaining all the differences across plans in the original version. We increased the font size, ordered the plans by generosity, eliminated categories where all plans offered the same benefit, and moved information so it was no longer nested in two columns per plan. These steps helped, but they were not enough. We were only able to lower the assessed skill level to 12 years of education. Not surprisingly, we found comprehension levels for the revised chart were somewhat higher for those with higher literacy and numeracy skills, but they were unchanged for those with lower skill levels.
Further simplifying the plan comparison chart would be possible if only the most salient information was included. Given that prior studies have found that providing less information aids comprehension and that this is particularly true in less skilled populations (Peters et al., 2007), it seems likely that a reduction in the number of areas the plans were compared on would similarly help the less skilled more. This speculation awaits further research.
Another way to simplify the comparison chart would be to simplify the Medicaid Program by limiting the number of health plan choices. While constraining choice may be counter to the notion of offering as diverse a set of options to consumers as possible, research in the field of psychology suggests it might improve another goal—informed decisionmaking. Research has found that consumers are attracted to having more choices (as they were in this study), yet they are less likely to make a selection and often make poorer quality choices when they have more options (Botti and Iyengar, 2006; Hanoch and Rice, 2006; Iyengar and Lepper, 2000).
Another reason for the low comprehension observed in this study is related to the low literacy and numeracy skills of many Medicaid consumers. We found that those with lower literacy and numeracy skills were substantially less likely to comprehend comparative health plan information, and that both skills are important for consumer comprehension. On the one hand, this underscores the importance of conducting further research on how to present important information about health care choices so it is understood by lower skilled consumers. On the other hand, if we acknowledge that there will always be some consumers with low skill levels who will not make informed decisions, policymakers should consider how to default these consumers into health plans in a way that promotes their welfare (Thaler and Sunstein, 2003). In other words, Medicaid agencies should create default algorithms that benefit individuals (and the program) by placing those consumers who do not select a plan into the most generous plan that allows them to maintain their primary care provider, rather than defaulting them equally across all the plans or to the cheapest plan. This approach of preserving choice, while acknowledging that some consumers need to be nudged in the direction that promotes their welfare, has been called libertarian paternalism (Thaler and Sunstein, 2003).
Our findings should be interpreted considering the following limitations. While we selected focus groups as a methodology to better understand how some consumers made health plan choices and why other consumers did not make a choice, our findings are based on a small, convenience sample in Duval County. As such, the findings may not be generalizable to Medicaid consumers undergoing Florida's Medicaid reform, particularly where there are more plans to choose from (Broward County) or fewer plans (Baker, Clay, and Nassau Counties). Our sample was, however, comparable with overall Medicaid reform statistics with regard to the percentage who selected their own health plan.
The experimental component of this study has high internal validity because subjects were randomized to the different study conditions. Of course, the use of a convenience samples does raise the question of the generalizability of the findings, in particular the absolute level of comprehension. However, since the cognitive processes that we studied are considered fundamental to the way that human beings process information, the relationships between variables observed in this study are unlikely to vary widely from those with other low income samples.
In sum, we find that Florida Medicaid reform's efforts to engage Medicaid consumers in making health plan decisions has not been working as anticipated. Consumers' low literacy and numeracy skills made selecting among the many health plans too challenging for many of them. This was further complicated by the quantity of information included in the plan comparison chart, which was assessed as being appropriate for college readers. These findings are relevant broadly to value-based health care initiatives, which require consumers to make (and assume that they do indeed make) informed choices. Effectively informing Medicaid consumers of the decisions they will have to make and facilitating effective decisionmaking will be crucial to the success of any value-based initiative.
Acknowledgments
The authors would like to thank the Jacksonville Housing Authority and Community Connections of Jacksonville for their assistance in recruiting participants for this study. The authors also thank the participants for sharing their insights and experiences.
Footnotes
Jessica Greene is with the University of Oregon. Ellen Peters is with Decision Research. The research in this article was supported by funding, in part by The Center for Health Care Strategies (CHCS), in Hamilton, NJ. The grant was made possible through a separate grant to CHCS by the Robert Wood Johnson Foundation. Partial funding also came from the National Science Foundation (SES-0820197). The statements expressed in this article are those of the authors and do not necessarily reflect the views or policies of the University of Oregon, Decision Research, CHCS, the Robert Wood Johnson Foundation, National Science Foundation, or the Centers for Medicare & Medicaid Services (CMS).
The other key VDHC component in Florida's Medicaid reform is a financial incentive program to spark preventive care and participation in healthy behavior programs.
Since the tasks in the focus groups and the surveys were distinct, we do not believe participation in one component would impact responses in the other.
Reprint Requests: Jessica Greene, Ph.D., Assistant Professor, Department of Planning, Public Policy & Management, 1209 University of Oregon, Eugene, OR 97405. E-mail: jessicag@uoregon.edu
References
- Agency for Health Care Administration. Florida Medicaid Reform Quarterly Progress Report, January 1, 2008-March 31, 2008. 2008.
- Agency for Health Care Administration. Florida Medicaid Reform, Year 1 Annual Report. 2008.
- Botti S, Iyengar S. The Dark Side of Choice: When Choice Impairs Social Welfare. Journal of Public Policy and Marketing. 2006;25(1):24–38. [Google Scholar]
- Bureau of the Census. Census 2000 Summary File 3 (Sf 3) 2000 Internet address: http://factfinder.census.gov/servlet/BasicFactsServlet (Accessed 2009.)
- Coughlin TA, Long SK, Triplett T, et al. Florida's Medicaid Reform: Informed Consumer Choice? Health Affairs. 2008 Nov-Dec;27(6):w523–532. doi: 10.1377/hlthaff.27.6.w523. [DOI] [PubMed] [Google Scholar]
- Davies HT, Washington AE, Bindman AB. Health Care Report Cards: Implications for Vulnerable Patient Groups and the Organizations Providing Them Care. Journal of Health Politics, Policy and Law. 2002 Jun;27(3):379–399. doi: 10.1215/03616878-27-3-379. [DOI] [PubMed] [Google Scholar]
- Davis TC, Wolf MS, Bass PF, 3rd, et al. Low Literacy Impairs Comprehension of Prescription Drug Warning Labels. Journal of General Internal Medicine. 2006 Aug;21(8):847–851. doi: 10.1111/j.1525-1497.2006.00529.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doak C, Doak L, Root J. Teaching Patients with Low Literacy Skills. Lippencott; 1996. [Google Scholar]
- Department of Health and Human Services. Value-Driven Health Care Home. 2008 Internet address: http://www.hhs.gov/valuedriven/index.html (Accessed 2009.)
- Fagerlin A, Zikmund-Fisher BJ, Ubel PA, et al. Measuring Numeracy without a Math Test: Development of the Subjective Numeracy Scale. Medical Decision Making. 2007 Sep-Oct;27(5):672–680. doi: 10.1177/0272989X07304449. [DOI] [PubMed] [Google Scholar]
- Farley DO, Elliott MN, Short PF, et al. Effect of CAHPs Performance Information on Health Plan Choices by Iowa Medicaid Beneficiaries. Medical Care Research and Review. 2002a Sep;59(3):319–336. doi: 10.1177/107755870205900305. [DOI] [PubMed] [Google Scholar]
- Farley DO, Short PF, Elliott MN, et al. Effects of CAHPs Health Plan Performance Information on Plan Choices by New Jersey Medicaid Beneficiaries. Health Services Research. 2002b Aug;37(4):985–1007. doi: 10.1034/j.1600-0560.2002.62.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farley DO, Short PF, McCormack L, Hibbard J, et al. Similarities and Differences in Choosing Health Plans. Medical Care. 2002 Apr;40(4):289–302. doi: 10.1097/00005650-200204000-00005. [DOI] [PubMed] [Google Scholar]
- Felt-Lisk S, Barrett A, Nyman R. Public Reporting of Quality Information on Medicaid Health Plans. Health Care Financing Review. 2007 Spring;28(3):5–16. [PMC free article] [PubMed] [Google Scholar]
- Gazmararian JA, Parker RM, Baker DW. Reading Skills and Family Planning Knowledge and Practices in a Low-Income Managed-Care Population. Obstetrics and Gynecology. 1999 Feb;93(2):239–244. doi: 10.1016/s0029-7844(98)00431-1. [DOI] [PubMed] [Google Scholar]
- Gerteis M, Gerteis JS, Newman D, et al. Testing Consumers' Comprehension of Quality Measures Using Alternative Reporting Formats. Health Care Financing Review. 2007 Spring;28(3):31–45. [PMC free article] [PubMed] [Google Scholar]
- Greene J. State Approaches to Consumer Direction in Medicaid. The Center for Health Care Strategies; Jul, 2007. [Google Scholar]
- Greene J, Hibbard J, Tusler M. How Much Do Health Literacy and Patient Activation Contribute to Older Adults' Ability to Manage Their Health? AARP Public Policy Institute; Jun, 2005. [Google Scholar]
- Greene J, Peters E, Mertz CK, et al. Comprehension and Choice of a Consumer-Directed Health Plan: An Experimental Study. American Journal of Managed Care. 2008;14(6):369–376. [PubMed] [Google Scholar]
- Hanoch Y, Rice T. Can Limiting Choice Increase Social Welfare? The Elderly and Health Insurance. Milbank Quarterly. 2006;84(1):37–73. doi: 10.1111/j.1468-0009.2006.00438.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hibbard J, Peters E, Slovic P, et al. Making Health Care Report Cards Easier to Use. The Joint Commission Journal on Quality Improvement. 2001 Nov;27(11):591–604. doi: 10.1016/s1070-3241(01)27051-5. [DOI] [PubMed] [Google Scholar]
- Hibbard JH, Peters E, Dixon A, et al. Consumer Competencies and the Use of Comparative Quality Information: It Isn't Just About Literacy. Medical Care Research and Review. 2007 Aug;64(4):379–394. doi: 10.1177/1077558707301630. [DOI] [PubMed] [Google Scholar]
- Hibbard JH, Slovic P, Peters E, et al. Strategies for Reporting Health Plan Performance Information to Consumers: Evidence from Controlled Studies. Health Services Research. 2002 Apr;37(2):291–313. doi: 10.1111/1475-6773.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iyengar S, Lepper M. When Choice Is Demotivating: Can One Desire Too Much of a Good Thing? Journal of Personality and Social Psychology. 2000;79(6):995–1006. doi: 10.1037//0022-3514.79.6.995. [DOI] [PubMed] [Google Scholar]
- Keysar B, Hendly A. Speakers' Overestimation of Their Effectiveness. Psychological Science. 2002;13(3):207–212. doi: 10.1111/1467-9280.00439. [DOI] [PubMed] [Google Scholar]
- Kutner M, Greenberg E, Jin Y, et al. The Health Literacy of America's Adults: Results from the 2003 National Assessment of Adult Literacy. U.S. Department of Education National Center for Education Statistics; 2006. [Google Scholar]
- Miles M, Am H. Qualitative Data Analysis. Sage Publications; 1994. [Google Scholar]
- Milligan C, Woodcock C, Burton A. Turning Medicaid Beneficiaries into Purchasers of Health Care. AcademyHealth; 2006. [PubMed] [Google Scholar]
- Mosenthal P, Kirsch I. A New Measure of Assessing Document Complexity: The Pmose/Ikirsch Document Readability Formula. Journal of Adolescent & Adult Literacy. 1998;41(8):638–657. [Google Scholar]
- Peters E, Dieckmann N, Dixon A, et al. Less Is More in Presenting Quality Information to Consumers. Medical Care Research and Review. 2007 Apr;64(2):169–190. doi: 10.1177/10775587070640020301. [DOI] [PubMed] [Google Scholar]
- Rice T. The Impact of Cost Containment Efforts on Racial and Ethnic Disparities in Healthcare: A Conceptualization. The National Academies Press; 2003. [Google Scholar]
- Smith D. Centers for Medicare & Medicaid Services Communication to State Medical Directors. Value-Driven Health Care. Apr 25, 2007. Correspondence Control Number SMD #07-005.
- Thaler R, Sunstein C. Libertarian Paternalism. American Economic Review. 2003;93(2):175–179. [Google Scholar]