Abstract
Medicare private fee-for-service (PFFS) plans are paid like other Medicare Advantage (MA) plans but are exempt from many MA requirements. Recently, Congress set average payments well above the costs of traditional fee-for-service (FFS) Medicare, inducing dramatic increases in PFFS plan enrollment. This has significant implications for Medicare's budget, provoking calls for policy change. We predict the effect of proposals to cut PFFS payments on PFFS plan participation and enrollment. We find that small reductions in payment rates would reduce PFFS participation and enrollment; if Congress reduces payments to traditional FFS levels it would cause the vast majority (85 percent) of PFFS plans to exit the market.
Introduction
MA is the Medicare Program that pays private plans capitated rates to insure beneficiaries. The most familiar MA plan type is the HMO, but the program also includes preferred provider organizations (PPOs) and PFFS plans. PFFS plans assume risk like other MA plans but do not employ all the cost control mechanisms required of other MA plan types (Medicare Payment Advisory Commission, 2007b). In particular, they are not required to manage care or establish networks of providers. In addition PFFS plans must pay physicians at least the same rate as traditional Medicare (Blum, Brown, and Frieder, 2007; Miller, 2008). Because PFFS plans do not build networks, they have been willing to enroll beneficiaries in rural areas that other MA plan types avoid due to the high costs of network contracting in those areas.
The Medicare Prescription Drug, Improvement, and Modernization Act of 2003 (MMA), best known for establishing a Medicare outpatient drug benefit, also made significant changes to the MA program. In the MMA, Congress created conditions favorable for rapid growth of MA plans in general and PFFS plans in particular. Between 2005 and 2006, PFFS enrollment increased 932 percent, while overall MA enrollment grew 37 percent (Gold, 2007a, 2008). The Congressional Budget Office (CBO) estimates that Medicare spending on PFFS plans will increase as a proportion of total MA spending from 21 to 30 percent between 2008 and 2017 (Orszag, 2007).
Increases mandated by the MMA and prior legislation have pushed payments to MA plans, including PFFS plans, well above average per beneficiary costs for traditional FFS Medicare. Payments are especially high relative to FFS expenditures in counties that were subject to the rural floor rate, a minimum payment rate for rural areas established by the Balanced Budget Act of 1997 (BBA) to encourage HMO participation in those areas. The average MA payment was 134 percent of average FFS expenditures in rural floor counties in 2006 (Medicare Payment Advisory Commission, 2007b). Because a greater share of their enrollment is in rural counties, PFFS plans receive greater payment relative to FFS expenditure than other plan types. The Medicare Payment Advisory Commission (MedPAC) reported that payments to MA plans and PFFS plans were 112 percent and 119 percent of FFS expenditures, respectively, in 2006 (Medicare Payment Advisory Commission, 2007b). CBO estimates were similar (Gronniger and Sunshine, 2007). In 2008, payments to PFFS plans declined slightly but were still 17 percent above FFS costs (Medicare Payment Advisory Commission, 2008).
The current state of PFFS differs considerably from the way the plan type was conceived. When the PFFS plan type was introduced in 1997 the expectation was that most Medicare beneficiaries would enroll in managed care plans. Beneficiaries who did not want a limited choice of providers could select PFFS and pay a higher premium for it. Instead, PFFS has become a vehicle for providing extra benefits to enrollees and at great cost to the Medicare Program. Part of this cost is borne by all Medicare beneficiaries through higher Part B premiums (Medicare Payment Advisory Commission, 2007c).
The implications of PFFS growth and spending have caught the attention of Congress and have raised questions about the value of PFFS relative to its cost (Neuman, 2007). Each additional dollar in extra PFFS benefits has been estimated to cost Medicare $3 (Harrison and Zarabozo, 2008). Recent legislation and proposals have targeted MA payments and regulations favorable to PFFS as ways to reduce spending. On July 15, 2008, Congress overrode a veto of the Medicare Improvements for Patients and Providers Act of 2008 (MIPPA) (Iglehart, 2008). Beginning in 2010, MIPPA will remove duplicative payments that MA plans receive for indirect medical education expenses. In 2011 MIPPA will rescind the PFFS provider network exemption in areas with at least two local network plans (HMOs or PPOs) (Congressional Budget Office, 2008; Biles, Adrion, and Guterman, 2008). CBO estimated that these provisions will decrease MA enrollment in 2013 by 2.3 million beneficiaries relative to the pre-MIPPA estimate of 14.3 million; Federal spending will fall by $47.5 billion over 2009-2018 (Orszag, 2008).
Since 2005, MedPAC has recommended parity between per beneficiary MA payment and FFS expenditure (Medicare Payment Advisory Commission, 2005). In a pre-MIPPA analysis, CBO estimated parity would save $149 billion over 2009-2017. CBO has also estimated that Medicare would save $43 billion over 2009-2017 by reducing PFFS payments to FFS costs but leaving payments to other plans at current levels (Gronniger and Sunshine, 2007).
This article complements CBO's analysis by estimating the effects of MedPAC and CBO proposals on PFFS availability and enrollment. We find that a payment rate cap of 100 percent of FFS costs would reduce PFFS plan participation by 85 percent, potentially affecting about 1.9 million enrollees.
Study Data and Methods
Our principal goal is to predict the effects of payment changes on the decisions of PFFS-offering firms to participate (enter) in Medicare. Our approach is to estimate a model of PFFS entry by firm, county, and year. Using this model, we simulate the effect of reduced payment rates. To do so, we created a year-county-firm level file from publicly available data on MA plan participation, enrollment, payment rates, organization names, benefits (2008 only), and FFS costs.1 To these we merged data on Medigap premiums and variables from the Area Resource File (ARF).2 These variables are used to control for PPFS plan cost and have been employed in prior work for similar purposes (Cawley, Chernew, and McLaughlin, 2005).
Our sample frame included all U.S. counties, all firms that ever offered a PFFS product (excluding employer-only plans), and years 2001-2008 (2001 was the first full year of PFFS availability) (Gold, 2007b). Except as indicated below, the analytic file contained one record for each combination of year, county, and PFFS-offering firm. We set an entry variable to one for records indicating a year and county in which a firm entered and zero otherwise.
We used a strict notion of entry: while a firm may contract with CMS to offer a plan in a county, we consider it to have entered only if it enrolled a meaningful number of beneficiaries. Our criteria for entry are enrollment of at least 11 individuals and at least 0.1 percent of beneficiaries in the county. The former is a functional definition: CMS reports enrollment below 11 as missing. The latter is consistent with techniques applied in prior work (Cawley, Chernew, and McLaughlin, 2005; Town and Liu, 2003; Frakt and Pizer, 2009; Pizer and Frakt, 2002).
While some firms offer PFFS products in most counties, others are active only in certain States (e.g., States where they are licensed). Such sub-national participants should not be considered as potential entrants in every county. Therefore, for each firm, we removed all year-county pairs in States in which the firm never entered any county.
In counties with few beneficiaries, average FFS cost is highly influenced by outlier values. Thus, we dropped counties with fewer than 250 beneficiaries (1.5 percent of records). The final file contained 272,580 year-county-firm observations, representing 8 years (2001-2008), 3,075 U.S. counties, and 33 firms. In descriptive results, aggregates are weighted by beneficiaries or PFFS enrollees as indicated. The Technical Note describes the multivariate model used to simulate PFFS firm response to payment changes.
Study Results
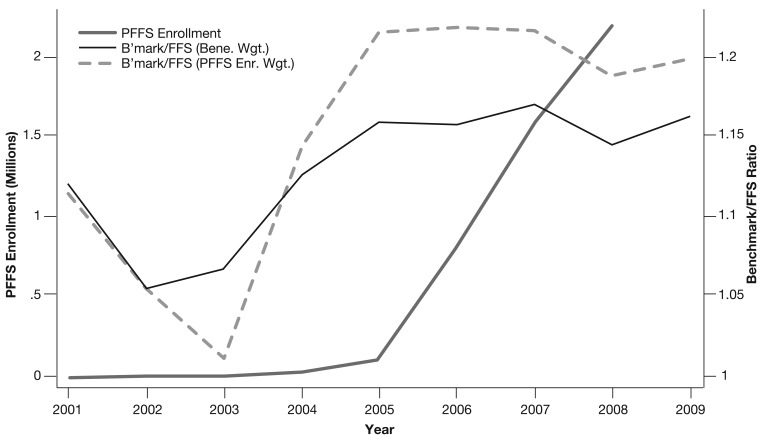
Figure 1 presents PFFS enrollment and average payment rate caps (also called benchmarks) as a proportion of FFS cost for 2001-2008 and 2009 estimates of the latter.3 The calculation of benchmarks follows MedPAC's methodology and complements their analyses of 2006 and 2008 (Biles, Adrion, and Guterman, 2008).
Figure 1. Private Fee-For-Service Enrollment and Benchmark/Fee-For-Service Cost Ratio, 2001-20091.
1 “Benchmark” is the maximum allowable payment rate. Since 2006, the actual rate paid to plans is a function of bids but is no higher than the benchmark. PFFS enrollment is not yet available for 2009; estimates of benchmark/FFS for 2009 are based on 2009 benchmark rates and 2008 enrollment figures.
SOURCE: Frakt, A. B., Pizer, S. D., VA Boston Healthcare System and BU School of Public Health, Feldman, R., University of Minnesota School of Public Health, 2009.
In Figure 1, the benchmark to FFS cost ratio is weighted by county-level counts of all Medicare beneficiaries and by PFFS enrollees. The former is what Medicare offers an MA plan on average to enroll a beneficiary. The latter reflects PFFS enrollment patterns. Both measures are above 1.0 in every year, and since 2004, PFFS enrollment-weighted values are higher than beneficiary-weighted values revealing that PFFS enrollment is disproportionately drawn from highly paid counties relative to FFS.
Table 1 reports the 2008 entry, enrollment, and non-drug benefits patterns for the top 10 PFFS-offering firms (enrollment ranked) and, in aggregate, all other firms. Because our analysis excludes employer-only plans, the ranking differs from that reported elsewhere.4 By our definition of entry (meaningful enrollment), no firm offers plans in all counties, three firms (Humana, Coventry, and Universal American) offer plans in over half the counties, and most are decidedly sub-national players (Table 1).
Table 1. Entry and Enrollment for the Top 10 Private Fee-For-Service-Offering Firms, 2008.
| Entry | Enrollment | Benefits | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Number of Counties Entered | Percent of Counties Entered w/o Rx Benefit | National Enrollment1 | Percent of Enrollment in Rural Counties2 | Monthly Average Net Premium3 | Average Doctor Visit Co-Pay4 | |
| Humana | 2,595 | 0 | 684,087 | 35.60 | $20.45 | $22.39 |
| BC/BS of MI | 262 | 0 | 243,745 | 25.20 | $114.08 | $13.06 |
| Coventry | 1,732 | 98 | 230,498 | 36.10 | $31.47 | $24.43 |
| WellPoint | 1,154 | 2 | 189,500 | 38.90 | $15.84 | $13.39 |
| Aetna | 1,000 | 0 | 188,480 | 18.20 | $89.75 | $8.35 |
| Universal American | 1,664 | 100 | 176,250 | 38.60 | $28.15 | $26.14 |
| Aon | 715 | 100 | 97,930 | 36.60 | $20.28 | $10.00 |
| WellCare | 840 | 0 | 94,833 | 20.20 | $1.87 | $14.54 |
| UnitedHealth | 913 | 92 | 90,739 | 28.30 | $1.71 | $29.57 |
| Universal Health Care | 314 | 0 | 31,021 | 14.20 | -$5.50 | $10.25 |
| All Other Firms | 1,194 | 73 | 134,516 | 17.30 | $53.48 | $12.71 |
| National Total/Average | 12,383 | 47 | 2,161,599 | 31.10 | $38.52 | $18.47 |
Enrollment excludes those in employer-only plans.
Rural counties are defined using the ARF rural/urban continuum codes as non-metropolitan counties with a U.S. Census-defined urban population under 20,000.
Premium is net any Part B premium rebate.
Doctor visit co-pay is for primary care doctor visits, not specialist visits.
SOURCE: Frakt, A. B., Pizer, S. D., VA Boston Healthcare System and BU School of Public Health, Feldman, R., University of Minnesota School of Public Health, 2009.
National PFFS enrollment in 2008 of 2.2 million was concentrated among Humana with 0.7 million enrollees (Table 1), and Blue Cross/Blue Shield of Michigan, Coventry, and Wellpoint, which collectively captured one-third of the market. PFFS enrollment in rural counties was a larger share of total enrollment than is common for MA plans in general: 31 percent for PFFS (Table 1) and 11 percent for MA plans (Gold, 2008).
In contrast to other MA plan types, which must offer at least one product with a drug benefit, PFFS-offering firms are not required to offer a drug benefit (Table 1). Overall, 47 percent of county-plan pairs do not include a drug benefit. But this masks considerable variation by firm. Some firms never or rarely offer a drug benefit (Coventry, Universal American, Aon, and UnitedHealth), while others frequently or always do so. Firms that do not offer a drug benefit may have made a strategic decision to provide drug options only through stand-alone prescription drug plans (PDPs).
The right-most columns of Table 1 report 2008 monthly average net premium (accounting for any Part B premium rebate), and average doctor visit co-payment. The national average premium, $38.52, is lower than the $45 reported elsewhere for 2006 (Gold, 2007a).5 The considerable variation in firm-level net premium is likely due to variations in Part B rebates, differences in benefit design (principally whether or not plans are bundled with a drug benefit), and variation in the geographic area over which different firms operate, which corresponds to variation in average per-beneficiary payment rate. Average doctor co-payments are consistent with those reported elsewhere (Gold, 2007a).
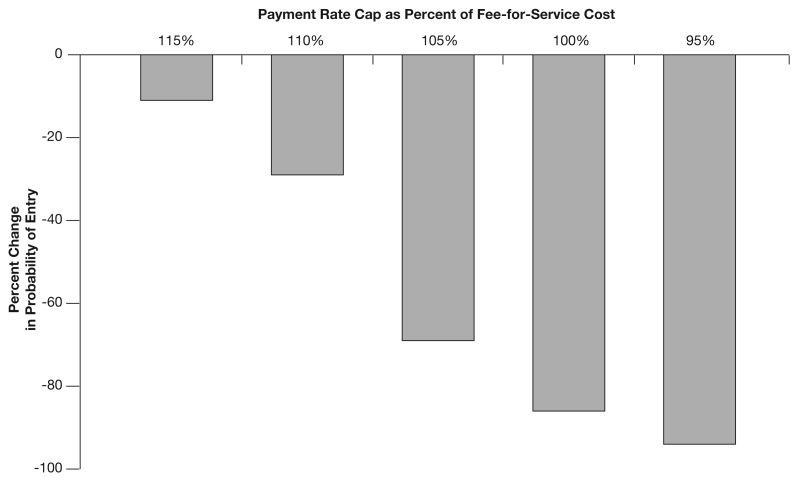
Figure 2 presents our simulations of the effects of changes in payment rates. The simulations were conducted using 2008 data based on the entry model described in the Technical Note. In each successive simulation, we capped the county payment rate at a lower level, starting at 115 percent and ending at 95 percent of county FFS cost, the rate prior to the passage of the 1997 BBA. Since the actual enrollee-weighted average 2008 benchmark/FFS value is 119 percent (Figure 1), all simulations reduce PFFS entry relative to current law. In particular, MedPAC's proposal to pay 100 percent of FFS cost would reduce entry by 85 percent. Assuming a proportional reduction in enrollment, about 1.9 million current PFFS enrollees would have to select another MA plan or switch to traditional FFS Medicare.
Figure 2. Estimated Effect of Payment Rate Caps on Private Fee-For-Service Entry, 20081.
1 Percent changes relative to 2008 benchmark payment rate levels.
SOURCE: Frakt, A. B., Pizer, S. D., VA Boston Healthcare System and BU School of Public Health, Feldman, R., University of Minnesota School of Public Health, 2009.
Discussion
Recent congressionally mandated payment rate increases have stimulated PFFS enrollment and provoked calls for policy change. In recent annual reports to Congress, MedPAC has cautioned that higher payments to MA plans, including PFFS plans, increase Medicare costs and beneficiary Part B premiums. MedPAC has recommended parity between MA payment rates and FFS cost, and CBO has evaluated the budgetary implications of cutting payments to PFFS plans. With the passage of MIPPA, Congress signaled an intention to reverse some of the effects of earlier rate-setting statutes while continuing to consider further measures.
This article makes two empirical contributions to this debate. First, we provide the first time series (2001-2009) of benchmark payment rates as a proportion of FFS cost for PFFS plans. In the existing literature, this number is only available for 2006 and 2008. Second, we evaluate the impact of payment rate cuts on PFFS entry and enrollment, complementing the CBO's budgetary analysis. We predict that a 100 percent FFS cap would reduce PFFS entry by 85 percent, potentially affecting 1.9 million beneficiaries. Those beneficiaries would have to enroll in another MA plan (if available) or receive coverage from FFS Medicare. CBO estimates that achieving payment parity between FFS and PFFS would save Medicare $43 billion over 2009-2017 (Gronniger and Sunshine, 2007).
PFFS plans do have other options in the face of payment cuts. They could reduce benefits. This, as opposed to exit, is more likely for small reductions in the benchmark relative to FFS cost. However, at the margin there will be exits with any size cut in payment. Reducing payments to or near FFS cost essentially returns to rates offered at a time when PFFS was a permitted plan type but actual PFFS entry was tiny. This descriptive evidence strongly suggests that plan exit and not benefits changes will be the dominant response to large changes in payment.
While our analysis is limited to PFFS, it is unlikely Congress would cut payments to PFFS plans while leaving payments to other MA plans intact. Therefore, parity between payment rates and FFS cost would have larger implications for Medicare, MA plans, and beneficiaries than we have described.
Of course, the provision of MIPPA scheduled for 2011 that will remove the PFFS provider network exemption in areas with at least two local network plans will have a large impact on PFFS without affecting other MA plans. Using our study data and CBO methodology, we estimate that had the network exemption repeal occurred in 2008, it would have caused about half of PFFS plans to exit the market, affecting 1.4 million enrollees (Bradley, 2008). Our results suggest that a cut in payments to 100 percent of FFS cost implemented before MIPPA's adjustment of the PFFS network exemption (i.e., in 2010) would render MIPPA's affect moot. On the other hand, if payments are cut after MIPPA is in effect they would induce a further reduction in the number of PFFS plans and enrollees beyond what would be caused by MIPPA alone.
Current fiscal constraints will likely mean less money for private Medicare plans (Krugman, 2008). As the fastest growing and most costly plan type, PFFS plans already are viewed as a potential source for savings. As we have illustrated, payment cuts have the potential to effectively shut down the PFFS market, making PFFS a particularly vivid illustration of the consequences of managing markets through congressional rate-setting. After creating explosive growth in PFFS enrollment, members of Congress will have to weigh the likely disruption and lost benefits for beneficiaries against predicted savings as they consider reversing course.
Technical Note
We estimated a logit model of PFFS entry with clustering on firm to adjust standard errors for firm-specific heteroscedasticity. Because lagged payment-to-FFS cost ratios are included in the model, 2001 data are omitted, reducing the sample to 238,358 year-county-firm observations. Lags are included in the model because plans did not respond to payment incentives instantaneously (Figure 1). Simulations assume that payment caps are set permanently so lags and current values are equal. Variables are defined in Table 2; mean values, model coefficients and marginal effects are provided in Table 3.
Table 2. Definition of Variables.
| Variable | Definition |
|---|---|
| Benchmark/FFS | Year-county specific benchmark payment rates as a proportion of per-beneficiary FFS costs. |
| Average Non-Rx Medigap Premium | Year-state specific average of non-drug Medigap premiums from a large insurer. |
| County Risk Score | Year 2000 county-level CMS diagnosis-based risk score. |
| Urban Adjacent Indicator | County-level indicator of urban status. |
| Rural Indicator | County-level indicator of rural status. |
| Proportion Elderly in Poverty | Year 2000 proportion of elderly population with income below Federal Poverty Level. |
| Per Capital Inc. (in 000) | Year 2000 county per capital income in thousands. |
| Proportion w/Col. Deg. | Year 2000 proportion of individuals in county with college degree. |
| Proportion w/H.S. Diploma | Year 2000 proportion of individuals in county with high school diploma. |
| Proportion Elderly 75+ | Year 2000 proportion of elderly in county that are at least 75 years old. |
| General Practitioner Density | Year 2000 county-level number of general practitioners per square mile. |
| Hospital Density | Year 2000 county-level number of hospitals per square mile. |
| Proportion White Collar | Year 2000 proportion of workers in county in white collar jobs. |
| Proportion Manufacturing | Year 2000 proportion of workers in county in manufacturing jobs. |
| Proportion Construction | Year 2000 proportion of workers in county in construction jobs. |
SOURCE: Frakt, A. B., Pizer, S. D., VA Boston Healthcare System and BU School of Public Health, Feldman, R., University of Minnesota School of Public Health, 2009.
Table 3. Logit Entry Model (Dependent Variable Is an Indicator of Firm-County Entry).
| Variable | Sample Mean | Coefficient (Standard Error) |
Marginal Effect |
|---|---|---|---|
| Benchmark/FFS | 1.14 | 22.11 (6.25)*** |
1.78 |
| 1-Yr Lag Benchmark/FFS | 1.14 | 23.78 (7.34)*** |
1.91 |
| 2-Yr Lag Benchmark/FFS | 1.14 | 24.15 (7.41)*** |
1.94 |
| (Benchmark/FFS) | 1.32 | -8.25 (2.45)*** |
-0.66 |
| 1-Yr Lag (Benchmark/FFS) | 1.33 | -8.92 (2.97)** |
-0.72 |
| 2-Yr Lag (Benchmark/FFS) | 1.32 | -10.12 (2.91)*** |
-0.81 |
| Average Non-Rx Medigap Premium | 117.79 | 0.01 (0.00)*** |
0 |
| County Risk Score | 0.99 | -0.3 -1.11 |
-0.02 |
| Urban Adjacent Indicator | 0.36 | -0.11 (.05)* |
-0.01 |
| Rural Indicator | 0.27 | -0.44 (.17)** |
-0.03 |
| Proportion Elderly in Poverty | 0.12 | -1.08 -1.34 |
-0.09 |
| Per Capital Inc. (in 000) | 22.44 | -0.01 -0.01 |
0 |
| Proportion w/Col. Deg. | 0.16 | 0.26 -0.39 |
0.02 |
| Proportion w/H.S. Diploma | 0.77 | -0.16 -0.76 |
-0.01 |
| Proportion Elderly 75+ | 0.47 | -1.42 -1.12 |
-0.11 |
| General Practitioner Density | 0.06 | -0.29 (.07)*** |
-0.02 |
| Hospital Density | 0.01 | -1.39 (.42)*** |
-0.11 |
| Proportion White Collar | 0.51 | 1.08 (.5)* |
0.09 |
| Proportion Manufacturing | 0.17 | 1.09 (.43)* |
0.09 |
| Proportion Construction | 0.08 | -0.49 -0.9 |
-0.04 |
| Constant | -46.62 (11.84)*** |
p<0.05.
p<0.01.
p<0.001.
N = 238,358 year-county-firm observations.
SOURCE: Frakt, A. B., Pizer, S. D., VA Boston Healthcare System and BU School of Public Health, Feldman, R., University of Minnesota School of Public Health, 2009.
Footnotes
Austin B. Frakt and Steven D. Pizer are with the VA Boston Healthcare System and BU School of Public Health. Roger Feldman is with the University of Minnesota School of Public Health. The research in this article was supported by Grant Number 63744 from the Robert Wood Johnson Foundation's Changes in Health Care Financing and Organization Initiative. The statements expressed in this article are those of the authors and do not necessarily reflect the views or policies of the VA Boston Healthcare System and BU School of Public Health, University of Minnesota School of Public Health, the Robert Wood Johnson Foundation, or the Centers for Medicare & Medicaid Services (CMS).
MA and FFS files are available from CMS at the following Internet sites: MA plan participation www.cms.hhs.gov/Health-PlanRepFileData/03_Geo.asp and www.cms.hhs.gov/MCRAdvPartDEnrolData/MACSASC/list.asp; MA enrollment www.cms.hhs.gov/MCRAdvPartDEnrolData/MMAESCC/list.asp; MA payment rates www.cms.hhs.gov/MedicareAdvtgSpecRateStats/RSD/list.asp; MA organization names www.cms.hhs.gov/MCRAdvPartDEnrolData/PDMCPDO/list.asp; MA drug benefits www.cms.hhs.gov/PrescriptionDrugCovGenIn/; MA non-drug benefits www.medicare.gov/download/downloaddb.asp; and FFS costs www.cms.hhs.gov/MedicareAdvtgSpecRateStats/05_FFS_Data.asp.
Medigap premium data were provided by a large insurer. ARF data are available from Quality Resource Systems, Inc. (www.arfsys.com/).
Before 2006, plans were paid an administratively set payment rate. Since 2006, plans are paid a value no higher than a benchmark. Plans that bid below the benchmark are paid the benchmark less 25 percent of the benchmark-bid difference. For simplicity, we use the term benchmark to refer to the actual payment rate (prior to 2006) and maximum payment rate (2006 and later) (Medicare Payment Advisory Commission, 2007a).
In particular, UnitedHealth is ranked second or third when employer-only plans are included (Gold, 2007b; Blum, Brown, and Frieder, 2007).
It is not clear if the 2006 estimates in Gold (2007a) are net of Part B rebates. Gold (2007a) also reports that the average 2006 PFFS premium was $5 below the average HMO premium.
Reprint Requests: Austin B. Frakt, Ph.D., VA Boston Healthcare System and BU School of Public Health, 150 S. Huntington Avenue (152H), Boston, MA 02130. E-mail: frakt@bu.edu
References
- Biles B, Adrion E, Guterman S. The Continuing Cost of Privatization: Extra Payments to Medicare Advantage Plans in 2008. Vol. 42. The Commonwealth Fund; Sep, 2008. Issue Brief No. 1169. [PubMed] [Google Scholar]
- Bradley T. Congressional Budget Office. Personal communication. Sep 11, 2008.
- Blum J, Brown R, Frieder M. An Examination of Medicare Private Fee-for-Service Plans. The Henry J. Kaiser Family Foundation; Mar, 2007. Medicare Issue Brief. [Google Scholar]
- Cawley J, Chernew M, McLaughlin C. HMO Participation in Medicare+Choice. Journal of Economics & Management Strategy. 2005 Fall;14(3):543–574. [Google Scholar]
- Congressional Budget Office. HR 6331: Medicare Improvements for Patients and Providers Act of 2008, Cost Estimate. Jul 23, 2008.
- Frakt A, Pizer S. Beneficiary Price Sensitivity in the Medicare Prescription Drug Plan Market. Health Economics. doi: 10.1002/hec.1451. Internet address: http://www3.interscience.wiley.com/journal/121673428/abstract (Accessed 2009.) [DOI] [PubMed]
- Gold M. Medicare Advantage in 2006-2007: What Congress Intended? Health Affairs. 2007a Jul-Aug;26(4):w445–w455. doi: 10.1377/hlthaff.26.4.w445. [DOI] [PubMed] [Google Scholar]
- Gold M. Medicare Advantage in 2008. The Henry J. Kaiser Family Foundation; Jun, 2008. Medicare Issue Brief. [Google Scholar]
- Gold M. Private Plans in Medicare: A 2007 Update. The Henry J. Kaiser Family Foundation; Mar, 2007b. Medicare Issue Brief. [Google Scholar]
- Gronniger J, Sunshine R. Medicare Advantage: Private Health Plans in Medicare. Congressional Budget Office; Jun 28, 2007. Economic and Budget Issue Brief. [Google Scholar]
- Harrison S, Zarabozo C. The Medicare Advantage Program. Medicare Payment Advisory Commission Public Meeting; December 5, 2008; Internet address: http://www.medpac.gov/tran-scripts/MA1208presentation%20final%20NO%20NOTES.pdf (Accessed 2009.) [Google Scholar]
- Iglehart J. Medicare Showdown. The New England Journal of Medicine. 2008 Aug 7;359(6):556–558. doi: 10.1056/NEJMp0805760. [DOI] [PubMed] [Google Scholar]
- Krugman P. Kennedy's Big Day. NY Times. 2008 Jul 11; [Google Scholar]
- Medicare Payment Advisory Commission. Medicare Advantage Program Payment System. Oct, 2007a.
- Medicare Payment Advisory Commission. Report to the Congress: Issues in a Modernized Medicare Program. Jun, 2005.
- Medicare Payment Advisory Commission. Report to the Congress: Medicare Payment Policy. Mar, 2007b. Chapter 4.
- Medicare Payment Advisory Commission. Report to the Congress: Promoting Greater Efficiency in Medicare. Jun, 2007c.
- Medicare Payment Advisory Commission. Report to the Congress: Medicare Payment Policy. Mar, 2008. Chapter 3.
- Miller M. Private Fee-for-Service Plans in Medicare Advantage. U.S. Senate; Jan 30, 2008. Medicare Payment Advisory Commission. Statement before the Committee on Finance. [Google Scholar]
- Neuman P. Private Fee-For-Service Plans in Medicare: Rapid Growth and Future Implications. U.S. House of Representatives; May 22, 2007. Testimony before the Subcommittee on Health, Committee on Ways and Means. [Google Scholar]
- Orszag P. Congressional Budget Office letter to Judd Gregg, Ranking Member, Committee on the Budget. U.S. Senate; Jul 8, 2008. [Google Scholar]
- Orszag P. The Medicare Advantage Program. U.S. House of Representatives; Jun 28, 2007. Congressional Budget Office.Testimony before the Committee on the Budget. [Google Scholar]
- Pizer S, Frakt A. Payment Policy and Competition in the Medicare+Choice Program. Health Care Financing Review. 2002 Fall;24(1):83–94. [PMC free article] [PubMed] [Google Scholar]
- Town R, Liu S. The Welfare Impact of Medicare HMOs. Rand Journal of Economics. 2003;34(4):719–736. [PubMed] [Google Scholar]