Abstract
Objective:
To determine the effectiveness of glenohumeral-joint stability braces in limiting active and passive shoulder abduction and external rotation in collegiate football players.
Design and Setting:
A 2-factor, repeated-measures design was used. The independent variables were brace condition (Denison and Duke Wyre harness, Sawa shoulder brace) and force application (active, passive). The dependent variables were shoulder abduction (45° braced limit) and external-rotation angular displacements.
Subjects:
Fifteen National Collegiate Athletic Association Division I male college football players (age = 19.9 ± 1.37 years, height = 183.2 ± 7.85 cm, mass = 89.9 ± 14.79 kg) participated in the study.
Measurements:
We used the PEAK Motus motion analysis system to measure angular displacements.
Results:
Neither brace maintained the arm position at the 45° braced limit during active or passive shoulder abduction (motion ranged from 56.8° to 73.0°). Although we did not use a priori external-rotation limits in this study, motion ranged from 71.6° to 93.9° with the braces. A repeated-measures multivariate analysis of variance indicated no significant interaction effect (P = .41), but main effects were significant for brace condition and force application (P < .001). Reported differences are statistically significant. For abduction, the Denison and Duke Wyre harness resulted in 12.3° (21%) greater angular displacement than the Sawa shoulder brace, and passive abduction resulted in 3.9° (6%) more angular displacement than active abduction. For external rotation, the Denison and Duke Wyre harness resulted in 6.7° (9%) more angular displacement than the Sawa shoulder brace, and passive external rotation resulted in 15.6° (21%) more angular displacement than active external rotation.
Conclusions:
Preset, braced abduction motion limits were not realized during active and passive physiologic loading of the glenohumeral joint. However, protection against the vulnerable position of 90° of abduction and external rotation was attained at a preset braced limit of 45° of abduction (the exception was the Denison and Duke Wyre harness during passive external rotation). The Sawa shoulder brace was most effective for this purpose.
Keywords: bracing, shoulder joint, angular displacement
Anterior glenohumeral-joint dislocations can be problematic for athletes competing in sports requiring overhead movements. Anterior dislocations account for 98% of all shoulder dislocations.1 The most common injury mechanism of acute anterior glenohumeral dislocations is excessive indirect force involving abduction, horizontal abduction, and external rotation,2 as often occurs during arm tackling in football.
Glenohumeral-joint stability braces are purported to protect the shoulder from recurrent dislocation by limiting glenohumeral abduction and external rotation. However, minimal research has been reported on their biomechanical effectiveness for limiting joint motion. DeCarlo et al3 investigated the Denison and Duke Wyre harness (CD Denison Orthopaedic Appliance Corp, Baltimore, MD), Sawa shoulder brace (Brace International, Atlanta, GA), and Shoulder Subluxation Inhibitor (Boston Brace International, Inc, Avon, MA) and reported that after exercise, flexion range of motion significantly increased for all 3 braces, whereas abduction significantly increased for the Sawa shoulder brace only. McLeod et al4 investigated the Sawa shoulder brace, Sully brace (Saunders Group, Chaska, MN), Douglas shoulder sling (Douglas Protective Equipment, Houston, TX), and a homemade elastic restraint (shoulder strap) and found that all 4 loosened after exercise, resulting in increased active shoulder abduction and external rotation. DeSavage et al5 investigated the Sawa shoulder brace, Denison and Duke Wyre harness, and Simply Stable Shoulder Stabilizer (Joint Solutions Inc, Tustin, CA) and reported that none of the braces restricted active shoulder abduction and external rotation to preset limits during physiologic loading.
All three cited studies,3–5 however, have methodologic limitations. Testing in these studies was limited to active range-of-motion assessment and did not include a passive load, which is a component of anterior glenohumeral dislocations. Furthermore, assessment in 2 of the studies3,5 was limited to testing with an isokinetic dynamometer, which lacked specificity to functional movement. Our purpose was to determine the effectiveness of the Denison and Duke Wyre harness and the Sawa shoulder brace for limiting passive and active glenohumeral abduction and external rotation. The outcome of this study is intended to improve clinical practice in the prevention of anterior glenohumeral dislocations and subluxations in the physically active.
MATERIALS AND METHODS
Research Design
We used a 2-factor, repeated-measures design in this study. The independent variables were brace condition (Denison and Duke Wyre harness, Sawa shoulder brace) and force application (active, passive). The dependent variables were shoulder abduction and external-rotation angular displacements.
Participants
Fifteen male Temple University (National Collegiate Athletic Association Division I) football players (age = 19.9 ± 1.37 years, height = 183.2 ± 7.85 cm, mass = 89.9 ± 14.79 kg) participated in this study. The study was conducted after a 5-week spring practice season was completed. Potential participants completed an Injury History Questionnaire and underwent a clinical examination of the right shoulder. Potential participants were excluded from the study if they had a right shoulder injury within 12 months of the study, prior right shoulder surgery, or prior experience with glenohumeral-joint stability braces. Participants were tested on the right arm (dominant) and had a minimum range of motion of 180° of shoulder abduction and 90° of shoulder external rotation (assessed at 90° of shoulder abduction). Dominance was defined as the arm the participant used to throw a football. The right arm was designated as the testing arm because of the availability of right-arm glenohumeral-joint stability braces. The study was approved by the Temple University Institutional Review Board, and participants read and signed informed consent and consent-to-videotape forms before participating.
Instrumentation
Health, Shoulder Injury, and Goniometer Assessments
We used an Injury History Questionnaire to determine the shoulder injury history of the participants. Questions addressed previous injuries to the upper extremity, surgery to the upper extremity, and use of glenohumeral-joint stability braces.
A clinical assessment was conducted by the primary investigator (K.W., a National Athletic Trainers' Association Board of Certification–certified athletic trainer with 4 years of collegiate football-team experience) to determine whether participants had any pre-existing shoulder instability. Assessment consisted of the anterior apprehension, posterior apprehension, and sulcus sign tests. The testing protocols and standards of Starkey and Ryan6 were used for these tests. All data were recorded on the Shoulder Assessment Form.
Goniometer assessment was conducted to ensure that the range-of-motion inclusionary criteria of the study were met. A 1°-increment goniometer was used to measure passive range of motion after the assessment protocols of Norkin and White.7 Measurements were made in degrees in the coronal plane. For abduction, the participant was positioned supine, and the movement arm of the goniometer was aligned with the shaft of the humerus, while the stationary arm was aligned along the lateral torso of the body parallel to the sternum. For external rotation, the participant was positioned supine with the humerus at 90° of abduction and the elbow at 90° of flexion. The movement arm of the goniometer was placed along the shaft of the forearm, and the stationary arm was positioned perpendicular to the body. Three measurements were taken for each motion, and the average was used as the criterion value. Goniometer intratester reliabilities were intraclass correlation coefficients (3,1) of .99 (SEM = .39°) and .95 (SEM = .66°) for shoulder abduction and external rotation, respectively.
Shoulder Braces
The 2 glenohumeral-joint stability braces we tested were the Denison and Duke Wyre harness and the Sawa shoulder brace. Both braces are marketed for the purpose of decreasing the incidence of anterior glenohumeral dislocations by limiting shoulder abduction and external rotation. We chose these 2 braces because of their use within sports medicine and because they can be worn with or without padding or restraint (eg, football shoulder pads).
The Denison and Duke Wyre harness (Figure 1) is constructed of a canvas vest, shoulder cap, and cuff that encircles the upper arm. The arm cuff attaches to the vest of the brace via leather laces, which can be adjusted to limit range of motion. The Sawa shoulder brace (Figure 2) is a blend of cotton, polyester, and elastic. It has a thorax vest, humeral cuff, and anterior and posterior straps. The straps connect to the thorax vest and humeral cuff and are adjustable, allowing for various degrees of range-of-motion restriction.
Figure 1.

Denison and Duke Wyre harness.
Figure 2.

Sawa shoulder brace.
Manufacturers' recommendations were followed to ensure proper fitting of each brace by the primary investigator (K.W.). For the Sawa shoulder brace, chest circumference at the areolar level was used to determine proper brace size: medium (91.2–98.4 cm), large (98.4–105.6 cm), or extra-large (105.6– 115.2 cm).
Peak Motus Motion Analysis System
The PEAK Motus motion analysis system (Peak Performance Technologies, Inc, Englewood, CO) was used to measure shoulder abduction and external-rotation angular displacements. These movements were analyzed with a single-camera set-up that allowed 2-dimensional kinematic data to be collected. The camcorder was positioned at 90° to the field of view. Reflective markers were placed on the participant's upper extremity to aid in the analysis. Trials were recorded on a standard VHS tape using a color camcorder (Panasonic AG-456, Panasonic Matsushita Electric Corporation of America, Secaucus, NJ). Video was collected at 60 images per second. A meter stick was used to calibrate the system before each test session. The video was manually digitized, and data were processed and filtered with the Peak Motus software (version 6.1).
Before data collection, reflective markers (modified Helen Hayes marker set) were placed as follows: shoulder abduction, over the C7 spinous process, a midlevel thoracic vertebral spinous process, olecranon process of the ulna, and humeral shaft of the dominant arm (Figure 3); external rotation, over the ulnar styloid and olecranon processes of the ulna and on the box below the forearm (Figure 4). The markers were used to define the position of 2 segments, and tracking these markers allowed us to determine angular displacement at the glenohumeral joint. The PEAK Motus system has an angular displacement reliability of .99 and measurement error of 0.5%.8
Figure 3.
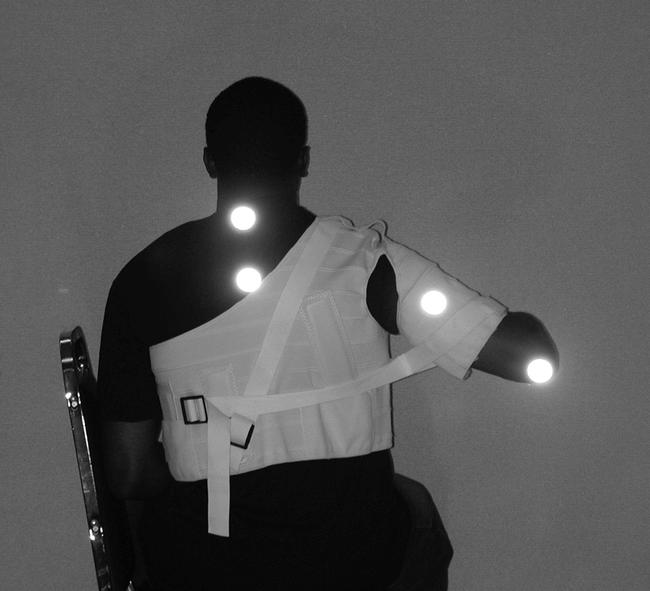
Abduction marker placement.
Figure 4.
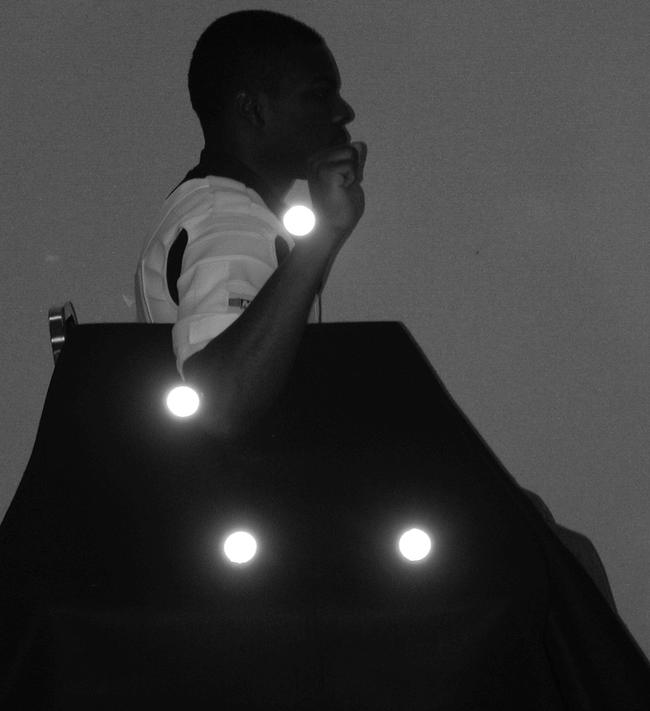
External-rotation marker placement.
MicroFET Hand Held Dynamometer
The MicroFET handheld dynamometer (Hoggan Health Industry, South Draper, UT) was used to ensure the consistent application of force during passive testing. The dynamometer has an internal cantilevered arm with 3 strain gauges arranged so that perpendicular and nonperpendicular forces are measured simultaneously. Force was applied in a single plane and measured in newtons.
Data Collection
A standardized protocol was followed for testing. After the purpose and protocol of the study were explained to potential participants, interested participants read and signed a written informed consent and completed the Injury History Questionnaire. A clinical shoulder evaluation was then conducted by the primary investigator. Participants who met all of the inclusionary criteria completed the testing phase of the study.
Testing began with the shoulder braces being randomly assigned and properly fitted to the participant by the primary investigator. As per manufacturers' recommendations, all participants wore a cotton T-shirt under the brace during testing. Reflective markers were placed over the landmarks as previously described. Participants were then seated sideways in a high-backed chair and stabilized with a Velcro (Velcro Inc, Manchester, NH) strap. Functional movement (abduction or external rotation) was randomly assigned, with active testing completed before passive testing.
To assess glenohumeral abduction, the brace limit was set to 45° of abduction, which was confirmed via passive goniometric measurement. Participants then performed 3 submaximal practice trials by actively abducting the shoulder, followed by a 1-minute rest period. Three trials for record were completed with the participant starting with his arm against his side and actively abducting the glenohumeral joint to its braced limit. Participants rested for 5 seconds between trials. For the passive-abduction trial, the handheld dynamometer was used by the primary investigator to apply 20 lb (88.96 N) of force to the medial epicondyle of the humerus in the direction of abduction. Three recorded trials were performed with 5 seconds rest between trials.
To assess glenohumeral external rotation, the brace was limited to 45° abduction (confirmed via passive goniometric measurement), which was maintained by resting the upper arm on an Orthoplast (Johnson & Johnson Products Inc, New Brunswick, NJ) foam wedge. The elbow was flexed to 90°, and the glenohumeral joint was internally rotated with the forearm resting on a wooden box. This was the start position for all external-rotation trials. The participant actively externally rotated his shoulder to its braced limit, keeping the upper arm resting on the wedge. For the passive-motion trial, a force of 10 lb (44.48 N) was applied by the primary investigator with the handheld dynamometer to the distal radius in the direction of external rotation. The same sequence of practice and test trials used for abduction was used for external rotation.
After all trials were recorded, the Peak Motus software was used to determine the abduction (ie, attained motion minus 45° set position) and external-rotation (ie, total external rotation motion at 45° of abduction) angular displacements of the shoulder. The average for the test trials was used as the respective criterion value for data analysis. Eight frames at the end range of motion were used to determine total angular displacement.
Data Analysis
Data were analyzed using a 2 (brace) × 2 (force application) multivariate analysis of variance with repeated measures on both factors. The dependent variables were shoulder abduction and external-rotation angular displacement. The Statistical Package for Social Sciences (version 11.0; SPSS Inc, Chicago, IL) was used for all statistical analyses. An alpha level of .05 was set as statistically significant.
RESULTS
Active shoulder abduction resulted in an average increase of 23.0° (51%) for the Denison and Duke Wyre harness and 11.8° (26%) for the Sawa shoulder brace from the 45° braced limit (Table 1). Passive shoulder abduction resulted in an average increase of 28.0° (62%) for the Denison and Duke Wyre harness and an average increase of 14.6° (32%) for the Sawa shoulder brace from the 45° braced limit.
Table 1.
Total Abduction Angular Displacement (Degrees) for Brace and Force Application
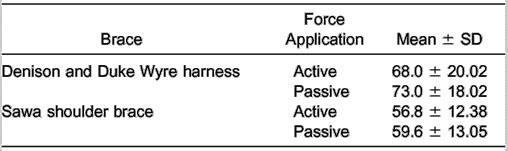
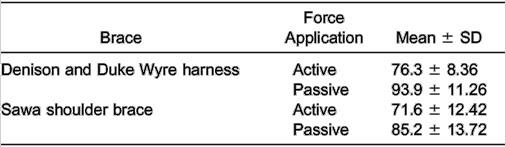
The repeated-measures multivariate analysis of variance indicated no significant interaction (Wilks lambda, F2,13 = .957, P = .41); however, significant main effects did exist for brace condition (Wilks lambda, F2,13 = 13.738, P = .001) and force application (Wilks lambda, F2,13 = 15.663, P = .001). Univariate analyses revealed significant differences for both independent variables for abduction (brace condition, F1,14 = 9.420, P = .008; force application, F1,14 = 4.742, P =.047) and external rotation (brace condition, F1,14 = 9.736, P = .008; force application, F1,14 = 32.928, P <.001) angular displacements. For abduction, the Denison and Duke Wyre harness resulted in 12.3° (21%) more angular displacement than the Sawa shoulder brace, and passive abduction resulted in 3.9° (6%) more angular displacement than active abduction. For external rotation, the Denison and Duke Wyre harness resulted in 6.7° (9%) more angular displacement than the Sawa shoulder brace, and passive external rotation resulted in 15.6° (21%) more angular displacement than active external rotation (Table 2).
Table 2.
Total External-Rotation Angular Displacement (Degrees) for Brace and Force Application
DISCUSSION
Neither glenohumeral-joint stability brace maintained the 45° motion limit during active or passive shoulder abduction. The Denison and Duke Wyre harness and Sawa shoulder brace allowed abduction motion, on average, to 68° and 56.8°, respectively, during active loading and to 73° and 59.6°, respectively, during passive loading. Although we did not use a priori external-rotation limits, motion ranged from 71.6° to 93.9° for the braces. Notwithstanding these results, the Sawa shoulder brace significantly limited motion more effectively than the Denison and Duke Wyre harness for all of the test conditions.
Comparison of specific brace results between the current and the 3 previously cited glenohumeral bracing studies3–5 reveals similar outcomes. Except for DeCarlo et al,3 who reported no significant increase in abduction motion for the Denison and Duke Wyre harness, McLeod et al4 (Denison and Duke Wyre harness not tested) and DeSavage et al5 found that neither the Denison and Duke Wyre harness nor the Sawa shoulder brace restricted shoulder abduction to a preset limit. In agreement with our findings, DeSavage et al5 determined that the Sawa shoulder brace significantly limited abduction more effectively than the Denison and Duke Wyre harness. Although the external-rotation findings of McLeod et al4 and DeSavage et al5 are similar to ours, DeCarlo et al3 reported no significant increase in external-rotation motion for either brace.
In our study, neither brace maintained the preset 45° of abduction position nor allowed active or passive shoulder abduction to reach the vulnerable 90° of abduction position. External rotation was similarly restricted to less than 90°, except with the Denison and Duke Wyre harness under a passive load. The extent to which these findings exist when both conditions are simultaneously assessed, as occurs in vivo on the field of play, is yet to be determined. This is important because as force increases, so does its effect on joint laxity, displacement, and range of motion (to a point). Based on these results, the motion-limiting efficacy of glenohumeral-joint stability braces is enhanced when preset limits are restricted below the protected motion minimum.
Several factors potentially contributed to each brace's inability to control motion to a preset limit. One factor was the restraint system's material in each brace. The Denison and Duke Wyre harness uses laces to restrain movement. The increase in motion may have been attributed to loosening of these laces during repetitive movement. The Sawa shoulder brace uses plastic clips to restrict motion. Slippage between the plastic clip-strap interface most likely contributed to motion allowance. Common to both braces was deformation of their composition materials, which are pliable (eg, cotton, polyester, elastic). Differences in material composition and design between the braces most likely contributed to the greater efficacy of the Sawa shoulder brace in limiting motion than the Denison and Duke Wyre harness. Another contributing factor to the increase in motion was the brace-body interface. All participants wore a cotton T-shirt under the brace as per manufacturers' recommendation. Although this most likely led to greater comfort to the braced participant, slippage between the surface interfaces may have affected the braces' restriction effectiveness.
This was the first study to assess glenohumeral-joint stability braces passively. Passive assessment is important because of its integral contribution to anterior shoulder dislocation and instability. It was not unexpected that passive assessments would yield greater angular displacements than active assessments because the former elicited greater stress-strain on the material composition of the braces and the brace-body interface. With even higher passive forces being produced in the athletic setting than were tested in this study, the true effectiveness of these braces for limiting motion is yet to be determined.
As the shoulder is abducted, fewer soft tissues contribute to stabilization of the anterior glenohumeral joint.9 When the humerus is between 0° and 45° of abduction, anterior displacement of the humerus is resisted by the middle glenohumeral ligament, superior fibers of the inferior glenohumeral ligament, and subscapularis muscle.9 At 90° of abduction, anterior displacement is resisted by the inferior glenohumeral ligament alone.9 This ligament functions similar to a sling by preventing increased translation of the humeral head on the glenoid fossa.10 With abduction, the entire complex moves beneath the humeral head and becomes taut, and when coupled with external rotation, moves anteriorly, statically limiting anterior translation.10,11 The inferior glenohumeral ligament has a high incidence of structural damage during anterior glenohumeral- joint dislocations.2 In athletes, glenohumeral-joint stability braces are used to limit shoulder motion, purportedly reducing recurrent episodes of instability.12 By limiting shoulder motion, the premise of these types of braces is to prevent the shoulder from reaching a vulnerable abducted, externally rotated position. The brace itself is not able to prevent dislocation if the shoulder reaches (either actively or passively) a vulnerable position. Injury occurs (eg, Bankart lesion) when the passive stabilizers of the shoulder (eg, joint capsule and ligaments) are taken to and past their physiologic limits. The efficacy of glenohumeral-joint stability bracing is attributed to range-of-motion protection, allowing the dynamic-restraint system to react to sudden, forceful abduction and external forces before the shoulder reaches a vulnerable position of 90° of abduction.
In conclusion, preset, braced abduction motion limits were not realized during active and passive physiologic loading of the glenohumeral joint. However, protection against the vulnerable position of 90° of abduction and external rotation (except for the Denison and Duke Wyre harness during passive external rotation) was attained at a preset braced limit of 45° of abduction. The Sawa shoulder brace was most effective for this purpose. Validation of bracing in general and prophylactic bracing specifically is based on 3 areas of assessment: biomechanical, to include kinematic, kinetic, and sensorimotor control; clinical efficacy; and functional performance. Although limited biomechanical assessment of these braces has been conducted, no research has been conducted to determine their effectiveness in reducing the incidence, severity, or type of glenohumeral-joint dislocation or their effect on functional performance. Furthermore, no research has assessed the effect of these braces in the lax or unstable glenohumeral joint, the latter being the very condition in which they are often used. Although we did not assess laxity and instability, we recommend these factors be included in future research with the intent of providing evidence-based outcomes to enhance decision making in clinical practice.
ACKNOWLEDGMENTS
We thank CD Denison Orthopaedic Appliance Corp (Baltimore, MD) and Brace International (Atlanta, GA) for providing the braces that were tested in this study.
REFERENCES
- 1.Rowe CR. Prognosis in dislocation of the shoulder. J Bone Joint Surg Am. 1956;38:957–977. [PubMed] [Google Scholar]
- 2.Matsen FA, Thomas SC, Rockwood CAO. The Shoulder. Vol. 1. Philadelphia, PA: WB Saunders Co; 1990. [Google Scholar]
- 3.DeCarlo M, Malone K, Gerig J, Hucker M. Evaluation of shoulder instability braces. J Sport Rehabil. 1996;5:143–150. [Google Scholar]
- 4.McLeod IA, Uhl TL, Arnold BL, Gansneder BM. The effectiveness of shoulder braces in limiting active range of motion. J Athl Train. 1999;34:S84. [Google Scholar]
- 5.DeSavage M, Sitler MR, Swanik K. Effects of glenohumeral joint stability braces on restricting active shoulder range of motion during physiological loading [abstract] J Athl Train. 2000;35:S-90. [Google Scholar]
- 6.Starkey C, Ryan JL. Evaluation of Orthopedic and Athletic Injuries. Philadelphia, PA: FA Davis Co; 1996. pp. 330–347. [Google Scholar]
- 7.Norkin CC, White DJ. Measurement of Joint Motion: A Guide to Goniometry. 2nd ed. Philadelphia, PA: FA Davis Co; 1995. pp. 58–64. [Google Scholar]
- 8.Scholz JP, Millford JP. Accuracy and precision of the PEAK Performance Technologies Motion Measurement System. J Mot Behav. 1993;25:2–7. doi: 10.1080/00222895.1993.9941634. [DOI] [PubMed] [Google Scholar]
- 9.Turkel SJ, Panio MW, Marshall JL, Girgis FG. Stabilizing mechanisms preventing anterior dislocation of the glenohumeral joint. J Bone Joint Surg Am. 1981;63:1208–1217. [PubMed] [Google Scholar]
- 10.O'Brien SJ, Neves MC, Arnoczky SP, et al. The anatomy and histology of the inferior glenohumeral ligament complex of the shoulder. Am J Sports Med. 1990;18:449–456. doi: 10.1177/036354659001800501. [DOI] [PubMed] [Google Scholar]
- 11.Levine WN, Flatow EL. The pathophysiology of shoulder instability. Am J Sports Med. 2000;28:910–917. doi: 10.1177/03635465000280062501. [DOI] [PubMed] [Google Scholar]
- 12.Sawa TM. An alternative conservative management of shoulder dislocations and subluxations. J Athl Train. 1992;27:366–369. [PMC free article] [PubMed] [Google Scholar]


