Abstract
Three critical issues in determining the usefulness of a patient classification in hospital and physician payment, hospital management, and utilization monitoring include: 1) the clinical relevance of the categorization, 2) the extent to which severity of illness distinctions are incorporated, and 3) the identification of comorbidity. Each of these issues has been addressed in the design of patient-management categories, a clinically based patient classification developed by the Health Care Research Department of Blue Cross of Western Pennsylvania under Grant No. 18-P-97063/3-06 from the Health Care Financing Administration. This article describes the clinical specificity of patient-management categories, how their design and definition incorporates severity of illness, and how comorbid patients are differentiated from single disease patients having multiple related diagnoses.
Introduction
Investigators in the area of hospital costs and case-mix measurement agree that for reimbursement purposes patient categories should be reasonably homogeneous with respect to expected resource use. It is equally clear that at some basic level of aggregation patient categories should also be clinically relevant and homogeneous with respect to severity of illness. Without this clinical homogeneity, the categorization loses its usefulness as the basis for establishing predictable patterns of resource use (i.e., planning, budgeting, and management) and for monitoring practice pattern changes (i.e., utilization review and quality assurance).
Although a number of recent developmental efforts have improved methods used in classifying patients— most notably the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) version of diagnosis-related groups (DRG's) (Fetter, Thompson, and Averill, 1981) and disease staging (Gonnella, Hornbrook, and Louis, 1984)— limitations remain in using these and other approaches. In general, certain patient categories are not as clinically relevant as desirable, methods of incorporating severity of illness distinctions between categories are often inadequate, and comorbidity has received only limited attention. The purpose of this article is to describe how research in the measurement of hospital case mix and costs conducted by the Health Care Research Department of Blue Cross of Western Pennsylvania has addressed each of these issues—clinical specificity, severity of illness, and comorbidity. Prior to a discussion of each of these issues, however, it is necessary to describe the case-mix measure that is a result of this research.
Case-mix measurement: Analytic approach
The primary product of this research is a patient classification, referred to as patient-management categories, that has a number of important characteristics, specifically:
Patient types have been defined within disease or disorder groups by physician panels before patient discharge abstract data are used to operationalize the classification;
Levels of severity are incorporated in the design and definitions of patient management categories;
The actual sequence of discharge diagnoses for a patient (i.e., principal versus secondary) does not affect category assignment;
Single disease patients having multiple related diagnoses are differentiated from comorbid cases; and
Assignment of patients to patient-management categories is computerized by using currently available discharge abstract data. The categorization software can be applied to any database compatible with the Uniform Hospital Discharge Data Set (UHDDS) and is thus readily exportable.
In addition to defining clinically distinct case types that should be managed similarly, physician panels also specified types and quantities of services required for the effective management of a typical patient in each patient management category. This management strategy consists of diagnostic and treatment services or components of care (e.g., X-rays, scans, laboratory studies, and specific operative procedures required, if any) as well as expected lengths of stay in special care units and in total. These components of care are not used in the assignment of a patient to a category. Rather, they were specified by physicians only to provide a basis for the derivation of a relative value scale based on actual hospital costs (as opposed to charges or charges adjusted to reflect costs) of services required (as opposed to services rendered).
For each patient-management category, a relative cost weight was derived using actual hospital cost data in a small but diverse sample of hospitals. Standard costs at each of six western Pennsylvania hospitals (teaching and nonteaching, with 175-625 beds) were obtained by using the following detailed cost finding process:
Detailed expenses (general ledger data from all six hospitals) were reclassified using System for Hospital Uniform Reporting (Health Care Financing Administration, 1978) to assure comparability;
Patient-related costs were identified and allocated to appropriate hospital revenue-producing centers; and
Revenue-producing center costs were allocated to particular services produced by that center (e.g., X-rays, scans, laboratory studies) by using departmental relative value scales that were defined as part of this research.
Component costs were then associated with different patient types according to the a priori clinical management strategies specified by the physician panels as opposed to actual patient utilization. It should be noted that patient-management categories can be used independently of this weighting methodology. For example, weights could be based on actual resource use patterns of patients assigned to each category. Average charges adjusted to reflect costs for each category (as used in Medicare's prospective payment system) could also be the basis of relative weights for patient-management categories.
It is important to emphasize that the management strategy and thus the relative cost weight associated with each patient-management category reflect the resources required for the effective care of that patient type, not necessarily the actual resources used by patients assigned to that category. This approach enables comparison of the expected resource use with actual resource use. It also permits the estimation of a relative cost weight for each case type that is independent of both hospital inefficiencies and diversity of actual clinical management within a category.
This case-mix system was designed and operationalized to distinguish patient types for which hospital resources and costs were expected to vary (Young, Swinkola, and Zorn, 1982; and Young et al., 1983). The objective of this research was not to capture severity distinctions among individual patients, nor was it to capture the plethora of clinical factors that influence diagnosis and treatment for a particular patient. Rather, it was to identify and incorporate clinical and severity distinctions among patient types where those distinctions reflect expected differences in patient management and, consequently, hospital resource requirements. Although these clinical and severity distinctions may or may not reflect substantial differences in actual hospital use and/or costs, the clinical specificity of patient-management categories has been preserved for further analyses.
Patient-management categories: Description
Patient-management categories were specifically designed to represent clinically distinct patient types, each requiring a different diagnostic and treatment strategy for effective care. Within clinically defined disease or disorder groups, patient types were initially identified in clinical terms by expert panels of physicians, independent of diagnosis and procedure codes and other patient data. Approximately 50 disease-specific panels were formed to define patient categories and specify typical management strategies. Each panel consisted of four to six physicians (generalists and specialists) who treat patients with the disease in question. Because of the a priori role of clinical judgment in category development, each patient-management category was defined to be clinically specific enough so that physicians could explicitly specify diagnostic and treatment components of care for the typical patient in each category.
Only after this specification process was complete were ICD-9-CM codes mapped to the resultant categories in order to computerize the assignment of patients to categories. The actual operational definition of patient-management categories uses combinations of diagnoses and, when necessary, specific procedures to capture the clinical specificity of the patient types identified by physicians. Age1 and sex are also used to assign patients to categories in a few isolated instances.
Because the International Classification of Diseases was not designed for the identification of unique clinical presentations, more than one ICD-9-CM diagnosis code is frequently required to represent a single disease process and/or stage or manifestation of a single disease that is being managed in a particular hospitalization. These diagnoses frequently, and legitimately, appear in any order on the patient's discharge abstract. For this reason, combinations of diagnoses are used to assign patients to categories, and the sequence of diagnosis codes listed on the patient's discharge abstract (i.e., principal versus secondary) does not affect category assignment.
Although other widely used patient classifications assume that multiple diagnoses represent comorbidity or a more severe patient type, patient-management categories recognize that several interrelated diagnoses may, in fact, represent only one manifestation (which may or may not be a complication) of a single disease process. As shown in the following example, multiple diagnosis codes do not necessarily represent comorbid conditions. In such instances, assignment to a single patient-management category is made.
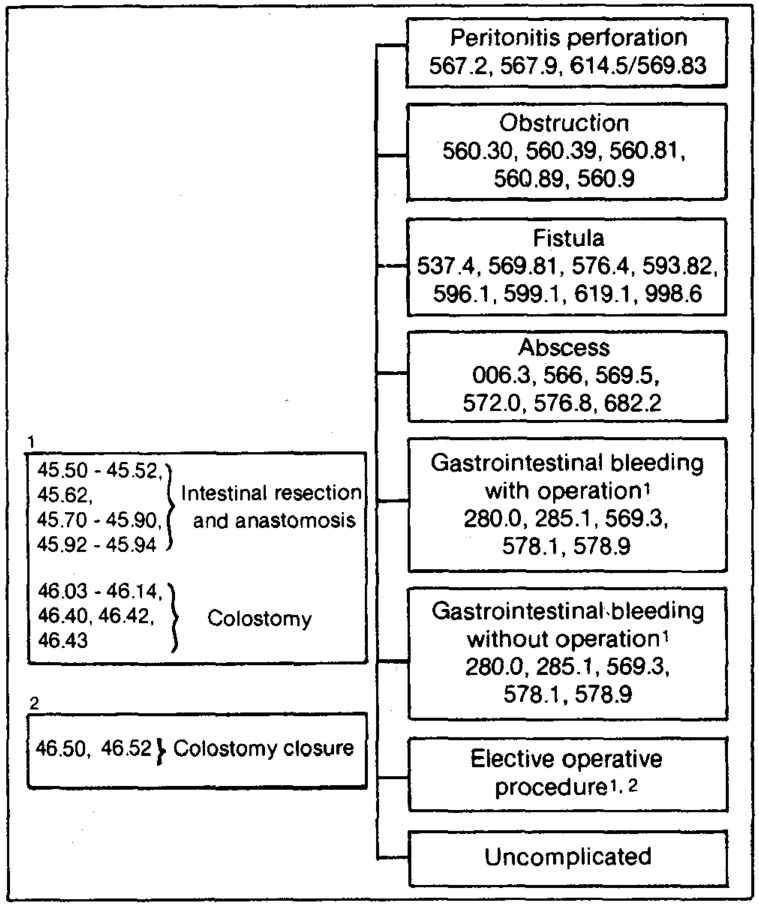
The multiple related diagnosis codes that are used for assignment to patient-management categories within diverticular disease are shown in Figure 1. These diagnosis codes can appear on a patient's discharge abstract in many combinations. For example, if a discharge abstract has anemia due to chronic blood loss (280.0), diverticulosis (562.10), and melena or blood in stool (578.1), in any order, without a specified procedure, that patient will be assigned to the patient-management category labeled diverticular disease: gastrointestinal bleeding without operation.
Figure 1. Multiple related diagnoses and patient management categories for diverticular disease [key codes 562.10, 562.11].
Although melena and anemia are not differential diagnoses in this example, there are ICD-9-CM diagnosis codes for these conditions that are frequently coded on the patient's discharge abstract along with the primary disease state, diverticulosis. The problems of melena and anemia are both caused by the diverticulosis and are not separate disease entities. The problems are typical reasons for admitting patients who are subsequently diagnosed as having diverticulosis. Note that the presence of more than one discharge diagnosis code in this example is not an adequate indicator of comorbidity. Nor do these particular multiple diagnosis codes necessarily reflect a more severe or a more costly patient type.
Note also in Figure 1 that the clinically specific complications, or more severe patient types, that are associated with diverticular disease such as peritonitis/perforation, obstruction, and fistula of the intestine are identified and categorized separately. Again, multiple diagnosis codes are required to reflect these specific conditions. Consequently, it is the specific combination of codes (in any order) that determines assignment to a patient-management category.
Classification software
The process of explicitly identifying and mapping multiple diagnosis codes to patient-management categories was performed as part of the computer software development. That is, the computerization of patient-management categories represents the operationalization of clinical distinctions among patient types identified by physician panels. The combinations of discharge diagnoses used in the computerization reflect the disease manifestations, etiology, signs, and symptoms associated with each distinct patient type identified by physician panels. Thus, the classification software incorporates the interrelationship of diagnosis codes within a disease and permits the valid assignment of patients to patient-management categories.
In general, a two-part computerized selection strategy has been used in assigning patients to one or more disease groups and to one patient-management category within each disease. First, a list of key diagnosis codes has been compiled for each disease or disorder group. Key codes for diverticular disease are shown in Figure 1. In order for a patient to be assigned to this particular disease group, one of these key codes must be present in one of the first five discharge diagnosis positions on the patient's discharge abstract.
In addition to these key codes, a more extensive set of ICD-9-CM codes has been identified and mapped to each patient-management category within a disease area. These codes represent the most accurate description of reason for admission, final diagnoses, and when necessary, the procedure(s) specified by physicians for each patient-management category. After a case has been assigned to a disease area using key codes, a search is made for the specific codes that will allow placement into one of the categories within the disease.
The multiple related diagnoses for diverticular disease shown in Figure 1 reflect this two-part computerized assignment of patients to categories. Using this strategy, it is possible to assign a patient to one category within a disease area, but up to five category assignments can be made if each diagnosis code represents a key code for a different disease or disorder. As will be described below, this latter circumstance facilitates the identification of comorbid cases.
Single disease: Multiple clinical conditions
Within some disease or disorder groups, patients frequently have two or more clinical conditions related to the same disease, each of which could be represented by a separately identified patient-management category. For example, in one hospitalization a patient with diverticular disease (Figure 1) could have both a fistula and peritonitis (e.g., diagnosis codes 537.4, 567.2, and 562.11, listed in any order). Each of these two conditions associated with diverticular disease represents a separate patient-management category because it would require a distinct clinical management strategy if it occurred by itself. When these conditions occur together, however, the question is whether the resources required to manage both conditions are substantially different from the resources required to manage either of the conditions occurring by itself.
In recognition of the fact that multiple clinical conditions can occur within most disease groups, physician panels (as part of the developmental process) reviewed combinations of categories that are possible and likely to occur within each disease group and recommended a hierarchy of categories. Specifically, physicians ranked the categories within each disease group so that the more severe categories and/or the more difficult and urgent to manage are identified first. Although this is conceptually similar to the process of identifying staging categories within diseases (Gonnella, Hornbrook, and Louis, 1984), no attempt was made to quantify the resultant severity distinctions into either an ordinal or a ratio scale that reflects severity only. Instead, the subjective clinical criteria embodied in the physician specified hierarchy were used in conjunction with other information about the nuances of the coding system and coding practice to finalize a hierarchy that is built into the classification software. Since the resultant hierarchy is based on a combination of multiple dimensions, the value of associating a numerical scale with the severity distinctions made among patient categories would be limited within a disease and such a scale would be uninterpretable across diseases.
In general, when interrelated clinical conditions occur together, the treatment for patient types that are higher in the hierarchy is expected to subsume the management specified for the categories lower in the hierarchy. This hierarchical structure forces each patient record to be categorized in only one patient-management category within a particular disease or disorder group. The hierarchy of categories for the acute myocardial infarction (AMI) disease group is shown in Table 1. Using an example from this disease, the patient who has an acute myocardial infarction with both bradyrhythmias and cardiogenic shock will be assigned to the patient-management category labeled AMI: cardiogenic shock as opposed to the category AMI: bradyrhythmia/heart block. According to physicians, the clinical management for cardiogenic shock is not only more extensive than the management for bradyrhythmia, but it would also subsume the management of the bradyrhythmia without requiring additional resources.
Table 1. Acute myocardial infarction patient management categories.
| Classification hierarchy | Cost weight | Fiscal Year 1983 death rate |
|---|---|---|
| Cardiogenic shock | 28.72 | 83.8 |
| Congestive heart failure with operation | 41.44 | NA1 |
| Pulmonary edema | 15.98 | 26.3 |
| Congestive heart failure without operation | 23.84 | 22.4 |
| Bradyrhythmias/heart block | 15.78 | 41.6 |
| Tachyrhythmias | 14.09 | 12.7 |
| Hypertension | 16.37 | 10.0 |
| Uncomplicated | 13.71 | 9.6 |
The frequency of patients in this category was too small to estimate a stable death rate.
Although not available to physicians during category development, the relative cost weights (July 1984) and death rates for each AMI patient-management category are also shown in Table 1. The death rate for each category can be used, especially in this disease area, as a proxy measure of clinical severity of the patient type. The relative cost weights shown reflect the costs of hospital resource requirements (as opposed to the costs of resources used) for patients discharged alive. For certain applications (e.g. hospital payment) these cost weights have been adjusted to reflect differences in actual resource use between patients discharged dead versus alive.
The decision of the physician panel (independent of data) had been that the management of cardiogenic shock would take precedence over the management of most other conditions in this disease group. As shown in Table 1, patients with an AMI and cardiogenic shock are clearly the most severe patient type, but not necessarily the most costly to manage. The most costly patient type is the congestive heart failure patient who receives an open heart operation.
The use of hierarchies within disease areas has facilitated categorization of the patient with two or more related clinical conditions being managed in one hospitalization. Each disease or disorder group has its own hierarchical structure that is built into the classification software. It is important to understand these relationships when using this system for data analysis or more specific applications such as reimbursement and utilization monitoring.
Clinical specificity
If one objective of a case based hospital payment system is to encourage product management, then the definition of the product must be sufficiently precise to enable physicians as well as hospital administrative staff to obtain data that describe the hospital's case mix and to examine patterns of patient care. That is, it is most important that the patients in each category require similar clinical management (so that physicians can interpret data associated with them) and that they require similar hospital resources (to enable product management and institutional planning). Physicians and other clinicians seem to recognize immediately the extent to which a patient category is clinically specific enough to infer similar clinical management. This is because clinical specificity is a concept that relates to the process of medical care, i.e., diagnosing and treating patients, a process which they understand.
In an attempt to illustrate the concept of clinical specificity, the relative clinical specificity of two patient classifications will be compared in the following section. Examples will be used from patient-management categories and diagnosis-related groups. The latter categorization should be especially familiar to most readers since the implementation of the Medicare prospective payment system. The data used in these examples is taken from a database of 2,228 cases in five disease and disorder areas discharged in a 6-month period from six hospitals during fiscal year 1980. The medical records of these cases were individually reviewed by nurses to correct coding errors and to validate patient-management category assignments. Each of these cases was then assigned to a DRG.2
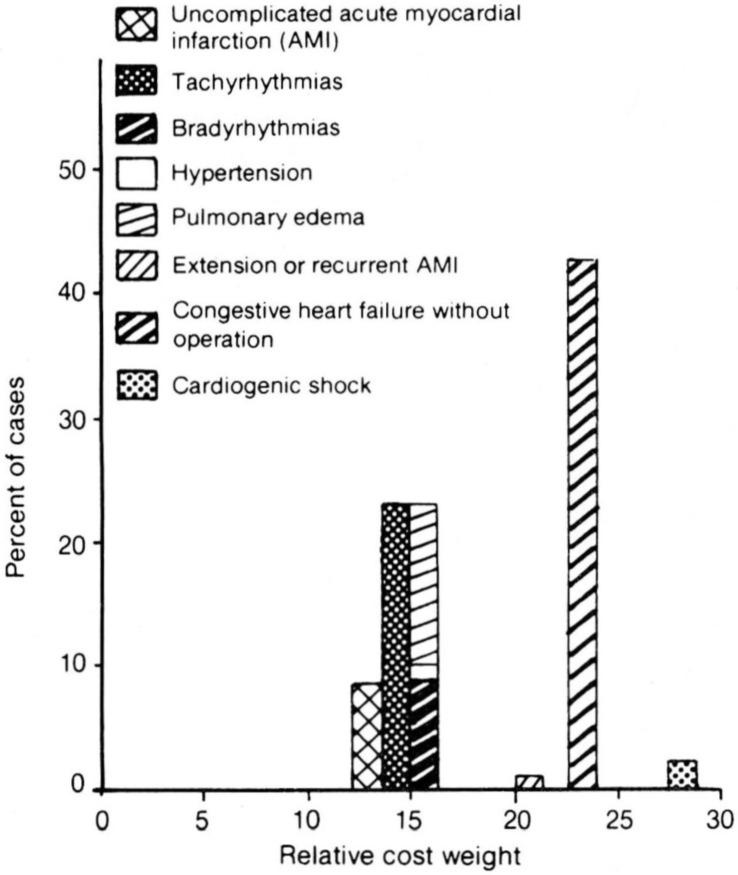
Figure 2 displays eight clinically distinct acute myocardial infarction (AMI) patient-management categories that occur within DRG 121: Circulatory disorders with AMI and cardiovascular complications, patients discharged alive. The 105 patients assigned to this DRG are arranged in terms of the cost based relative weight derived as of July 1984 for each patient-management category. Note that five patient-management categories (i.e., uncomplicated AMI, tachyrhythmias, bradyrhythmias, hypertension, and pulmonary edema) have similar relative cost weights, suggesting that similar resource use would be expected for this subset of patient types. To physicians, however, it is clear that the clinical management and thus the hospital resource requirements for a patient with an AMI and cardiogenic shock or congestive heart failure are substantially different than an AMI patient with tachyrhythmias. This conclusion is also suggested by the variation in the cost weights for these distinct patient types.
Figure 2. Diagnosis related group 1211 in relation to acute myocardial infarction patient management categories.
1DRG 121:Circulatory disorders with acute myocardial infarction and cardio-vascular complications, dischared alive (major diagnosis category. circulatory system). (N = 105)
In a second example, 990 patients were identified by nurses through medical record review as having chronic obstructive pulmonary disease (COPD) without comorbid conditions. These cases were assigned to the seven COPD patient-management categories shown in Table 2. The relative cost weight for each of these clinically distinct patient types is also shown to indicate expected differences in clinical management and thus required hospital resources.
Table 2. Percent distribution of chronic obstructive pulmonary disease (COPD) patients within diagnosis-related groups (DRG's) N = 990.
| COPD patient management category1 | Relative cost weight | DRG 88 chronic obstructive pulmonary disease N = 267 | DRG 96 bronchitis and asthma age ≥ 70 and/or C.C.2 N = 200 | DRG 97 bronchitis and asthma age 18-69 w/o C.C.2 N = 201 | DRG 98 bronchitis and asthma age 0-17 N = 188 | 29 other DRG's 3 N = 134 |
|---|---|---|---|---|---|---|
| Percent distribution | ||||||
| Chronic bronchitis/asthma (N = 622) | 6.82 | 71.2 | 73.0 | 67.2 | 66.5 | 19.4 |
| Acute asthma attack (N = 151) | 1.69 | 0.7 | 14.0 | 31.3 | 30.3 | 0.7 |
| Acute respiratory failure (N = 53) | 22.50 | 9.7 | 1.5 | 0.5 | 0 | 17.2 |
| Cor pulmonale (N = 52) | 10.90 | 12.4 | 5.5 | 0 | 0 | 6.0 |
| Bronchiectasis (N = 4) | 8.83 | 1.1 | 0.5 | 0 | 0 | 0 |
| Pneumonia (N = 99) | 10.55 | 4.1 | 5.5 | 1.0 | 3.2 | 51.5 |
| Spontaneous pneumothorax (N = 9) | 14.45 | 0.7 | 0 | 0 | 0 | 5.2 |
Nurse reviewed medical record assignments.
Comorbidities and complications.
Includes 16 DRG's in the respiratory system major diagnosis category (MDC) and 13 DRG's in eight different MDC's.
When these same COPD patients were categorized into DRG's, 97.7 percent (or 967 patients) were assigned to 20 DRG's within the respiratory system major diagnosis category (MDC). Of these patients, 88.5 percent (or 856 patients) were assigned to 4 of the 20 DRG's. The distribution of patients in these four DRG's and all other DRG's combined in comparison to the COPD patient-management categories is shown in Table 2. Note that the patient-management category for chronic bronchitis/asthma not only occurs in each of the DRG categories, but this one clinical patient type also represents the largest proportion of patients in each of the four high frequency DRG's. Similarly, other patient-management categories, with diverse cost weights reflecting different hospital resource requirements, occur across several DRG's.
The COPD patients that were assigned to 29 other DRG's as shown in Table 2, occurred in 9 different MDC's. The large number of MDC assignments for the same clinical patient type in this example is a result of the importance given to the order of diagnoses in the computerized algorithm that assigns patients to diagnosis-related groups. Elsewhere it has been shown that multiple diagnosis codes are frequently used, and are in fact required, in order to accurately represent a single disease process and/or clinical condition that is being managed in a given hospitalization (HCFA Grant No. 18-P-97063/3-06, progress reports dated April 1981 and June 1982). Since the order of these multiple diagnosis codes is the basis for assigning the patient to an MDC, the same clinical patient type could be assigned to multiple MDC's. This problem of misclassification of the same clinical type occurs more frequently among DRG's within a single MDC than it does across MDC's. Findings from studies conducted by the Institute of Medicine (1980), Barnard and Esmond (1981), and Simborg (1981) all suggest the unreliability of making category assignments on the basis of principal diagnosis.
Since validated information from medical record review was available to assure accurate assignment of patients to categories, it is clear that in this example patients requiring different clinical management occur within single DRG's, and clinically similar patients are assigned to different DRG's. Although the examples shown are limited to only two disease areas, they do illustrate the relative clinical specificity of the two patient categorizations. These distinctions, however, may or may not have a substantial impact on actual hospital cost analyses, which is a separate issue for investigation.
Severity of illness
The implementation of diagnosis-related groups in the Medicare prospective payment system has focused attention on severity of illness as an especially important problem. That is, the lack of clinical specificity of certain DRG's has led to the speculation of potential inequities in payment as a consequence of differences in severity of illness across hospitals. The need to define patient categories that are clinically distinct and thus to incorporate severity of illness distinctions in patient classification is clear. It is not clear, however, within the context of hospital reimbursement, that severity of illness distinctions must necessarily be quantified (i.e., on either an ordinal or ratio scale).
Severity of illness generally refers to the probability of death or loss of function over the natural history of a disease (Hornbrook, 1982). Using this conceptualization, the term severity of illness is disease specific and has no heuristic value when used across diseases. It is precisely because severity of illness refers to a disease-specific clinical condition at a point in time that the quantification of this concept has been so elusive.
Research on severity measurement includes at least three distinct conceptualizations of severity of illness:
Severity of illness among patient types within a disease, for example, disease staging (Gonnella, Hornbrook, and Louis, 1984);
Severity of illness among individual patients within a disease, for example, trauma scores (Baker et al., 1974; American College of Surgeons, 1980); and
Severity of illness among individual patients across diseases, for example, generic severity indexes (Wagner, Knaus, and Draper, 1983; Horn, Chachich, and Clopton, 1983).
The methods used in these attempts to measure severity of illness include a priori physician judgment to define severity levels within a disease and subjective assessment or physiological measurement of an individual patient's condition at a specific point in time (usually admission or discharge).
Physicians who participated in this research have suggested that the more severe patients or patient types are those who have a greater probability of death or disability and/or whose management (diagnosis and treatment) is more difficult or complicated than others. Physicians recognize severity distinctions among clinically distinct patient types within a disease and, in many cases, are able to rank these patient types by degree of severity. For example, a diverticular disease patient with nonmassive gastrointestinal bleeding is generally considered less severe than a diverticular disease patient with obstruction or fistula. Even though the degree of severity in this example is not explicitly quantified, the clinical distinction among patient types, which implicitly includes a severity distinction, can be incorporated in a patient classification.
Physicians are less able to compare the relative severity of patient types across diseases, nor is it necessarily desirable to do so. That is, it is difficult to postulate explicit criteria with which to compare an uncomplicated acute myocardial infarction with diverticular disease complicated by a fistula or obstruction. For this reason, except for special cases such as critically ill patients (Wagner, Knaus, and Draper, 1983), attempts to measure severity distinctions across disease areas have been unsuccessful to date.
The design of patient-management categories incorporates severity of illness distinctions among patient types as a byproduct of the clinical specificity of each patient-management category and in the definition of a hierarchy for each disease area. No attempt is made, however, to quantify directly severity distinctions that have been incorporated in the category definitions and the classification software. The focus of our research has been to measure the relative cost of care using patient-management categories. That is, the relative costliness of each patient-management category is quantified rather than the severity of the illness.
It has been noted that physicians recognize the clinical and severity distinctions incorporated in the definitions of patient-management categories. As previously shown in the acute myocardial infarction example, however, the more severe patient type is not always the patient type whose management requirements are more extensive. Thus, it should not be assumed that severity will necessarily be related consistently to costs, charges, or to any other measure of resources used in patient management.
Comorbidity
The term comorbid implies the presence of more than one disease or pathological condition. It should be emphasized, however, that comorbid patients are not necessarily more severely ill or more costly to manage than patients with a single disease. That is, a patient can be comorbid with two relatively minor conditions, each requiring few hospital resources for effective management. Therefore, what the particular comorbid conditions are and how each is managed will determine the cost of care. Optimally, within the context of hospital case-mix measurement and reimbursement, the definition of comorbidity should reflect only diseases or disorders that are actively managed (or affect the active management of the other disease or condition) during a particular hospitalization. Unfortunately, it is not always possible to operationalize this latter condition due to the practice of coding incidental findings and to other constraints of the diagnosis coding system.
In order to effectively identify comorbid conditions or multiple disease processes that impact on clinical management, it is essential to be able to first isolate single disease processes accurately. More specifically, multiple related diagnoses that represent a single disease should not be considered part of comorbidity; rather, such patients should be identified for single categorization. Only in this way can the true extent of comorbidity and its effect on resource use be assessed.
Patient-management category classification software not only permits the assignment of a patient to an appropriate category within a disease group but it also permits multiple assignment to different disease groups, thus identifying comorbid cases. Multiple category assignments are possible because of the identification of key diagnosis codes for each disease or disorder group. Specifically, where ICD-9-CM codes associated with different disease or disorder groups are present, the classification software identifies these comorbid conditions and makes one patient-management category assignment in each disease.
As discussed previously, computerized assignment of a patient to a disease group is made by scanning that patient's discharge abstract for key diagnosis codes. This is a manageable task because key diagnosis codes do not include the vast majority of diagnosis codes frequently used to qualify or specify a patient's condition more precisely. If a key code for more than one disease group is present, each relevant disease module (subroutine in the classification software) is accessed, and category assignment within that disease group is made. The present classification software permits a patient to be assigned to as many as five patient-management categories.
An example of the results of this strategy for identifying comorbidity is shown here using all discharges from 90 western Pennsylvania hospitals in fiscal year 1983. Of 797,833 patients, 96.1 percent were classified into patient management categories. As shown in Table 3, 65.5 percent were categorized in a single patient management category, 30.6 percent had comorbid conditions, and 3.9 percent were not able to be categorized with the information on the discharge abstract. This percentage of patients with comorbid conditions is not constant across payers, however. As expected, Medicare has a much larger proportion of patients with comorbid conditions than each of the other payers shown on Table 4.
Table 3. Number and percent distribution of patients, by number of patient management category assignments: Fiscal year 1983.
| Number of category assignments | Number of patients | Percent |
|---|---|---|
| Total | 797,833 | 100.0 |
| One | 522,586 | 65.5 |
| Two | 173,135 | 21.7 |
| Three | 58,461 | 7.3 |
| Four | 11,930 | 1.5 |
| Five | 988 | .1 |
| Uncategorized | 30,733 | 3.9 |
Table 4. Comorbidity by payer, western Pennsylvania hospital discharges: Fiscal year 1983.
| Payer | Percent of comorbid patients |
|---|---|
| All payers | 31 |
| Medicare | 52 |
| Blue Cross | 21 |
| Commercial | 19 |
| Medicaid | 19 |
| Other | 19 |
It should be emphasized that the number of category assignments made will not necessarily be the same as the number of diagnosis codes listed on the patient's discharge abstract because several diagnosis codes are frequently used to define a single disease process. For example, although 65.5 percent of the patients in the entire fiscal year 1983 database were categorized in a single patient management category, only 29.9 percent had a single discharge diagnosis code. Of the patients assigned to one patient management category, 57.6 percent had multiple diagnosis codes.
Given the large number of comorbid combinations that can occur in any given database, it is not feasible to create separate categories for all possibilities. For this reason, a method has been designed to adjust the relative cost weight of particular patients who have multiple category assignments. Costs are assigned to each comorbid case based on the physician-specified components of care for each patient management category to which the patient is assigned, and an adjusted cost weight is derived for that patient.
An important issue in this cost-weight adjustment is whether particular combinations of comorbid conditions have an important impact on patient management and in what way hospital resource use is affected. For example, comorbid conditions could be independent of each other in terms of hospital resources used or the comorbid conditions could require an overlapping set of hospital resources. In still other cases, the comorbid conditions could influence the physician's monitoring activity but may not alter hospital resources used. Further research on this issue is currently in progress. Preliminary results suggest that certain hospital components of care such as operative procedures are additive for patients with comorbid conditions. Other components of care for patients with comorbid conditions such as length of stay may be equivalent to the length of stay of one of the comorbid conditions.
Using this method, it is not important to make the judgment (which is frequently arbitrary) regarding which category is the most significant for hospital resource use. Instead, all category assignments are taken into account for specifying resource use and for deriving the adjusted relative cost weight. Using this method also maintains the separation between multiple category assignments and the impact of the specific combination of categories on resource requirements and costs. That is, whether a comorbid case is also a costly case depends on the specific multiple category assignments made and the resources required to manage each condition.
Discussion
It is the hope of policymakers that, when hospitals are paid based on case types, administrators will have a strong incentive to develop management control systems and compatible organization structures that assure efficient and effective production of patient care. Case-mix management information is expected to become available and to be used to monitor patterns of care, communicate with physicians, and in general, to manage the institution. These expectations are likely to be fulfilled only if patient information is organized in ways that are meaningful to physicians. Thus, patient types must not only be homogeneous with respect to resource use but also clinically relevant and homogeneous with respect to severity of illness.
The operational strategies for dealing with severity distinctions and comorbidity that have been described in this article are incorporated in the structure of the patient-management category classification software. These methods permit accurate identification of clinically specific patient types, the incorporation of severity distinctions, and the identification of patients who have comorbid conditions. There are, however, certain limitations to the process.
First, in order to make the task of computerizing this system manageable, only one category assignment is permitted within a disease or disorder group. Thus, the number of category assignments made is dependent on the definition of disease and disorder groups. For example, since upper extremity fractures and head injuries are separate disorder groups, a patient with an injury in each area will receive two category assignments, while a patient with multiple upper extremity fractures will receive only one category assignment. The actual impact of this limitation is expected to be small due to the low frequency of such cases and similarities in management for patient types within a disease or disorder group. This assumption, however, needs to be tested.
Second, limitations in the way ICD-9-CM diagnosis codes are used impose constraints on the specificity and the accuracy of this and other patient classifications that use them. For example, certain diagnoses are legitimately coded to reflect a patient's condition, but may not reflect active clinical management of that condition during a particular hospitalization. A diagnosis of hypertension is an example of this type of problem. Incidental diagnostic findings (such as asymptomatic diverticular disease found on barium enema) that are reported on the patient's discharge abstract create a similar problem for all patient classifications. It is important to know where these problems are likely to occur in order to compensate for their effect and operationalize category definitions in a satisfactory way. A longer range strategy for dealing with this problem is to establish special coding guidelines or formats to isolate actively managed conditions on the discharge abstract. This also could be treated as one function of utilization review activity.
The limitations of the ICD-9-CM coding system and the intricacies of coding diagnoses to represent a disease or illness process present some difficult problems. In spite of these problems, it has been possible to design classification software that assigns patients to the clinically distinct patient-management categories that physicians have specified. By using multiple related diagnoses that represent a stage, unique manifestation, and/or complication of a single disease process, severity of illness distinctions among patient types are included in the classification and single disease patients are differentiated from patients with comorbid conditions.
Acknowledgments
The completion of this research would not have been possible without the commitment of the entire staff of the Health Care Research Department of Blue Cross of Western Pennsylvania over the past 6 years. Important contributions to this specific article were made by the following project staff: James Walrath and Dorothy Joyce, Project Directors; Marlene Patterson, Category Development; and Jenny Schuchert, Classification Software Development. The critical review and suggestions made by Julian Pettengill have also been especially significant.
This research was supported by the Health Care Financing Administration, Department of Health and Human Services, Grant No. 18-P-97063/3-06.
Footnotes
In most panel sessions, physicians indicated that if clinically specific patient types as they defined them could be identified, age would not be a significant factor in determining differences in clinical management for the typical patient. In preliminary analyses of length-of-stay distributions by age for high volume patient-management categories, this expectation has been confirmed.
The Commission on Professional and Hospital Activities assigned DRG's to this patient data using the ICD-9-CM version of the DRG classification software available in May 1982.
References
- American College of Surgeons Committee on Trauma. Field categorization of trauma patients and hospital trauma index. Bulletin of the American College of Surgeons. 1980 Feb. Appendix E. [PubMed] [Google Scholar]
- Baker SP, O’Neill B, Haddon W, Long W. The injury severity score, a method for describing patients with multiple injuries and evaluating emergency care. Journal of Trauma. 1974;14:187. [PubMed] [Google Scholar]
- Barnard C, Esmond T. DRG-based reimbursement, the use of concurrent and retrospective clinical data. Med Care. 1981 Nov.20(11):1071–1082. doi: 10.1097/00005650-198111000-00002. [DOI] [PubMed] [Google Scholar]
- Fetter RB, Thompson JD, Averill RA, et al. The New ICD-9-CM Diagnosis-Related Groups Classification Scheme, Users Manual. Vol. 1. New Haven, Conn.: Health Systems Management Group, School of Organization and Management, Yale University; 1981. [Google Scholar]
- Fetter RB, Shin Y, Freeman JL, Averill RF, Thompson JD. Case mix definition by diagnosis-related groups. Med Care. 1980;18(Supplement):1–53. [PubMed] [Google Scholar]
- Gonnella JS, Hornbrook MC, Louis OZ. Staging of Disease, a case-mix measurement. JAMA. 1984;251:637. [PubMed] [Google Scholar]
- Grimaldi PL, Micheletti JA. Diagnosis-Related Groups: A Practitioner's Guide. Chicago, Ill.: Pluribus Press, Inc.; 1982. [Google Scholar]
- Health Care Financing Administration. System for Hospital Uniform Reporting. 1978 Sept. [Google Scholar]
- Horn SD, Chachich B, Clopton C. Measuring severity of illness: A reliability study. Med Care. 1983;21:705. doi: 10.1097/00005650-198307000-00004. [DOI] [PubMed] [Google Scholar]
- Hornbrook MC. Med Care Review. 2. Vol. 39. Michigan: Health Administration Press; Summer. 1982. Hospital case mix, its definition, measurement, and use. Part II. Review of Alternative Measures; pp. 73–123. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Reliability of National Hospital Discharge Survey Data: Report of a Study. Washington, DC: Institute of Medicine, National Academy of Sciences; 1980. [Google Scholar]
- Simborg DW. Sounding board, DRG Creep, a new hospital-acquired disease. The New England Journal of Medicine. 1981 Jun;304(26):1602–1604. doi: 10.1056/NEJM198106253042611. [DOI] [PubMed] [Google Scholar]
- Wagner DP, Knaus WA, Draper EA. Statistical validation of a severity of illness measure. American Journal of Public Health. 1983;73:878. doi: 10.2105/ajph.73.8.878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young WW, Swinkola RB, Zorn DM. The measurement of hospital case mix. Med Care. 1982 May;20(5):501–512. doi: 10.1097/00005650-198205000-00006. [DOI] [PubMed] [Google Scholar]
- Young WW, et al. Hospital case mix: development and implementation. Health Care Research Department, Blue Cross of Western Pennsylvania; 1983. [Google Scholar]