Abstract
Statistics from several Organization for Economic Cooperation and Development countries on consumption and cost of health care services, physician workload, and physician earnings are presented. Data are analyzed according to type of physician payment used: fee for service, per case, capitation, or salary. Incentives theoretically embodied in each payment method are often offset by other factors—scale of charges, patient out-of-pocket payment, and patient access or physician activity restrictions. Moreover, the impact of payment method on use appears to be weaker than the impact of such factors as population morbidity, national health insurance, professional ethics, and medical technology.
Introduction
This article is a presentation of a set of statistics gathered to describe the behavior of patients and doctors, the consumption and cost of health care services, and physician earnings in a number of Organization for Economic Cooperation and Development (OECD) countries. The countries concerned are Canada, Denmark, France, the Federal Republic of Germany (hereafter called Germany), Italy, Japan, the Netherlands, the United Kingdom, and the United States. (In Canada, health care systems differ somewhat from province to province. Quebec's system is studied in more detail here because some aspects of its system of remuneration for physicians are unique.) The data are studied in relation to the methods used in the different countries to compensate physicians. First, the scope and comparability of the data available across the countries as well as analysis of the possible impact of the remuneration methods on the behavior of patients and their doctors are discussed.
Methodological remarks
The aggregate statistical data used in this article were derived from a variety of different sources. In some cases, various primary data were combined so as to get as comparable estimates as possible. In the “Technical note,” the sources and computations used for each parameter are listed. It must be stressed that the concepts and definitions used in the different countries—and sometimes inside the same country— vary. Therefore, the parameters used to describe the operation of the health care system in general and the activity or income of physicians in particular are not identical even though the term used may be the same.
Depending on the method of data collection— surveys of households, surveys of physicians, use of health insurance records, or use of national accounts—the data cover a different scope of population, practitioners, and expenses. The discrepancies are sometimes real, but sometimes they are only apparent. For example, using data from the National Ambulatory Medical Care Survey of the National Center for Health Statistics (NCHS), one could quote the figure of 2.7 physician contacts per person per year in the United States during 1985. On the other hand, using 1985 NCHS data from the National Health Interview Survey, one could quote the figure of 5.3 physician visits per person per year. The explanation of the apparent difference lies in the fact that the first estimate refers only to office visits. In other countries, the scope of the data reported by national health insurance funds is generally more restricted than that of data reported in patient interviews. In most cases, the explanations of the differences can be found by careful reading of the detailed methodological appendixes of publications. The data selected for this study are as comparable across countries as possible. However, some bias might be introduced in the intercountry comparisons by the fact that data are not available for all countries on a yearly basis.
The influence of a particular method of payment on the functioning of a health system should, strictly speaking, be assessed in terms of the outcome of the incentive or disincentive effects of each of its dimensions, e.g., basis of remuneration, scale of charges, and type of health coverage provided by the health insurance agency or agencies. However, the methods of payment for medical services can influence the behavior of both those seeking health care and physicians (who are providers in their own right and also prescribers of services supplied by other members of the profession). Therefore, problems arise from the interaction of various other factors when one tries to isolate the impact of methods of remuneration on the functioning of the health care system or to determine the incentive effect of a particular aspect of remuneration.
Patient factors that influence the demand for health care include sociodemographic and cultural characteristics, geographic environment, and self-perception of their state of health. It is difficult to separate the effects of these factors from the effects of economic factors in general and the methods of paying for care in particular.
To some extent, physicians behave like other suppliers: The way they are paid will have some effect on their assessment of the patient's state of health and their consequent decisions regarding the therapy required. Such effects are difficult to isolate from the effects of other factors, such as their professional knowledge, code of ethics, and the medical-technical environment (the possibility to refer patients to hospital consultants, detection and screening services, etc.).
Moreover, each of these factors, depending on how it is applied, has an influence not only on its own account but also because it is coupled with others in a given set of conditions. In practice, the observable variants are not simply random combinations/On the contrary, it would seem that, in most countries, the adoption of particular methods of remuneration has been aimed at achieving compatibility between the different aspects of these methods of payment and their acceptability by the profession. Accordingly, the incentive effects of one feature of physician remuneration are often offset by those inherent in another of its features. Consequently, it might be unrealistic to attribute a separate incentive or disincentive effect to each individual characteristic of a particular method of payment.
From the statistical standpoint, a number of warnings should be given with regard to the conclusions to be drawn from international comparisons. In order to assess the impact of a particular factor, one needs to be able to measure the deviation it causes from a normal situation. However, in the health care area, more than elsewhere, no stable reference values exist. The pace of technological progress is such that the norms as regards numbers and concentration of personnel or equipment are constantly being revised, as is the level of needs. In assessing the values for a particular parameter in the different countries, without knowing whether these are unduly high or unduly low, it is tempting to take as the norm the average derived from a sample of countries. However, such values cannot be used as standards. On the one hand, they are obtained by aggregating highly different situations; on the other hand, it is impossible to say whether they represent an optimum.
How are physicians compensated?
In the different countries considered, there are four main basic ways of remunerating physicians: fee-for-service payment, payment per case, capitation payment, and payment of a salary. These remuneration methods are not mutually exclusive. The full description and analysis of how physicians are paid in different countries can be found elsewhere: Chadwick (1987); Contandriopoulos, Lemay, and Tessier (1987); Glaser (1970); Hogarth (1963); and Reinhardt, Sandier, and Schneider (1986). To avoid repetition, only some comments on the incentives built into each method are provided in this article.
Different points derived from the observation of various countries should be stressed:
In practice, each method of remuneration is applied in a number of ways across countries, depending on the conditions under which it operates. For example, payment to the physician of a fee agreed upon at the time of treatment, as is often the case in the United States, bears only a remote resemblance to the fee-for-service system operated in Germany. Under Germany's statutory health insurance scheme, neither the patient nor the doctor knows at the time of treatment the exact amount the doctor will be paid. The patient, moreover, will never know. The doctor will receive payment later through his professional association on the basis of an agreed-upon nomenclature of services and in accordance with a scale of fees worked out on the basis of the forecast overall budget agreed on by the Health Insurance Funds and apportioned among the physicians within a region in relation to their workload.
Most countries have adopted a combination of methods for remunerating different categories of physicians on the basis of their specialty or where they practice, remunerating the same doctor when he or she performs different activities, or paying for treatment given to a particular category of patient. A physician may be paid by one or more different methods, depending on the type of patients treated. In the Netherlands, for example, the statutory health insurance scheme fixes an earnings target for general practitioners and calculates the capitation payment in such a way that it will provide 70 percent of these earnings, on the assumption that the remaining 30 percent will be derived from private practice, for which payment is on a fee-for-service basis. In the United States, a combination of payment methods is the general rule. Each payment method is represented, ranging from no patient out-of-pocket payment in the case of Medicaid, full or partial direct payments in the case of private insurance schemes, and full or partial reimbursement of the patient's expenditure to full payment with no refund for uninsured patients or for expenditure below a certain level for patients under some insurance arrangements. In sortie countries, the system of remuneration for specialists differs from that for general practitioners, and in some different systems of payment are used for hospital and ambulatory care.
Each method of payment has a particular sphere of application. Fee-for-service payment applies primarily to the situation in which the relationship between physicians, as self-employed persons, and their patients is one of free choice; payment of a capitation is used predominantly in the case of physicians who both provide primary care and act as gatekeepers of the health system by having the responsibility of referring their patients to other providers when necessary; physicians employed in establishments supplying them with other inputs, staff, and equipment are paid a salary proportional to the number of hours worked.
If the patient has no health care insurance, few rules govern the payment of physicians, and generally the amount the patient pays is determined by market forces. However, such a situation rarely occurs in OECD countries. At present, some degree of general coverage of health care expenditure exists in all OECD countries in the form of a national health service, statutory insurance agencies, or private insurance arrangements chosen by individuals. In the case of insured health care, the features and operation of each method of remuneration are usually governed by rules negotiated by representatives of the medical profession and the health insurance agencies. Generally speaking, the smaller the proportion of cost borne by the patients themselves is, the greater are the power and influence of third-party payers.
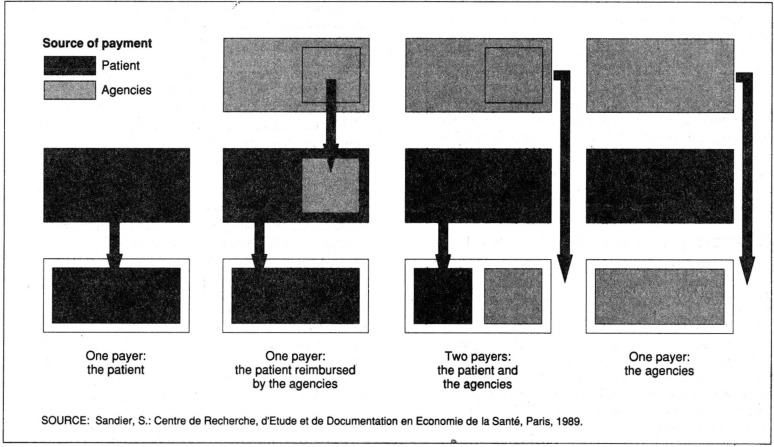
The payment of the physician involves one or more financial transactions. The nature of the payer(s), the proportion that each pays, and the timing of the payment are conditions that, like the basis of the remuneration or the scale of charges, can influence the behavior of the different actors. Describing the methods of physician payment by considering only the last parameter would be an oversimplification and could lead to forgetting the strong incentives and possibilities for control associated with the other factors.
In Figure 1, the four main situations concerned in the case of self-employed physicians are outlined. The physician may receive total payment from the patient (who either is or is not later reimbursed by the agency), total payment from the health insurance agency or agencies, or partial payment from both. Incentives may differ according to who pays and when.
Figure 1. Four main forms of remuneration for self-employed physicians.
When the patients have to make the initial outlay, they are aware of the cost of health care, sometimes to the extent that it may deter them from calling upon a physician's services. In this case, the health care financing agencies lose some power of control. On the other hand, the system of full coverage might be seen as providing an incentive to higher health care consumption, because the demand from the patient for treatment is no longer regulated by prices. However, although the treatment may be free, in most cases, the patient has to be registered on a doctor's list and cannot consult a specialist without the prior consent of the general practitioner. What is more, full and direct physician payment by the health insurance agencies means that they have greater control over the physician's activity and remuneration. The use of a sliding fee scale in Quebec and the fixing of payments in line with an overall budget in Japan are good illustrations of this ability to control expenditure.
Theory versus reality
In comparing the hypotheses implicit in the theory with the reality observable in the sample of countries considered, we look first, at the consumption of physicians' services; second, at physician workload and prescribing behavior; and finally, at the earnings of physicians. The sources of the data used are enumerated in the “Technical note.”
Utilization of health care services
A key question faced by policy analysts concerns the influence on the level of health care consumption of the different methods used to compensate physicians. Based on the data collected, one cannot assert that the relationship is either weak or strong. The data do not support the conventional wisdom that fee-for-service payment is more conducive to overconsumption than the capitation system is.
The number of physician-patient contacts, which can be regarded as an indicator of the consumption of physicians' services, is determined both by the frequency of recourse to health care, which generally is the patient's decision, and by the behavior of the physician, who decides on the treatment and may ask the patient to come back to see him or her or to consult a colleague. A particular payment method can have an opposite effect on the patient's behavior and the physician's behavior, which together determine the level of consumption.
It is difficult to separate the effect of the method of payment as such from that of the amount that the individual consumer bears (either nothing at all or a portion of the cost). The payment method affects the physician's behavior; the amount the individual pays affects that of the consumer. For example, in theory, payment of a fixed capitation to physicians tempts them to restrict the frequency of visits by their registered patients and encourages patients to consult their doctor more frequently because, as is usually the case with a capitation system, the treatment is free. However, the number of visits actually made is the result of the operation of supply and demand within a given system. It is not possible to disentangle the respective effects of the two factors—the patient's contribution, on the one hand, and the unit of measurement of physician output, on the other—on the basis of number of visits.
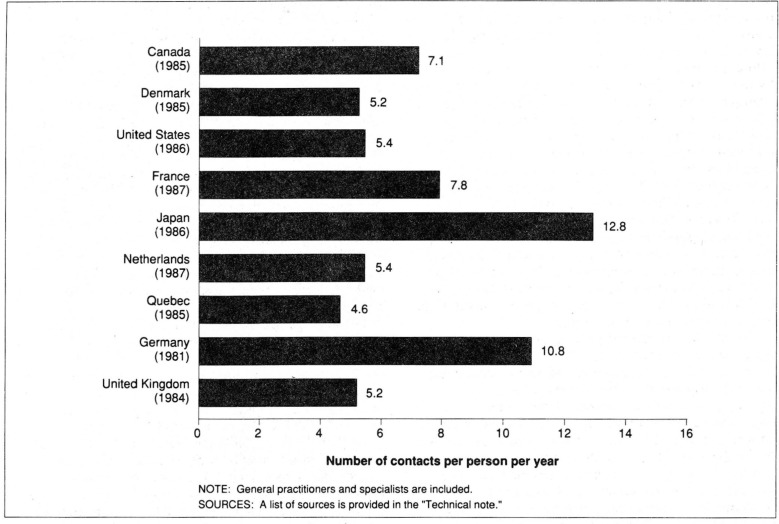
As shown in Figure 2, the use of physicians' services in some countries is twice that in others, measured in terms of the number of contacts per person per year. Just on the basis of these figures, Germany seems to be an example that would support the argument that the fee-for-service system of payment leads to a high level of health care consumption, but questions begin to arise when a more detailed analysis is made taking into account the frequency of recourse to health care, the duration of physicians' services, the breakdown of these between general practitioners and specialists, the financial contribution made by patients, and the rules governing access to specialist care.
Figure 2. Utilization of physician services: Selected countries, selected years 1981-86.
Access to health care, measured in terms of the percentage of the population having recourse to physicians' services, varies little among countries with the exception of Japan, where the proportion of consumers (55 percent) appears to be substantially lower than elsewhere. Access seems to be little influenced by the method of payment of physicians or by the financial contribution required of patients. For example, in the United States, where in many cases patients have to bear at least part of the cost of ambulatory care, 76 percent of the population saw a physician at least once during 1986, whereas in Quebec, where health care is free, the figure was 78 percent in 1985. In a detailed analysis of health care use in the Netherlands, Van Vliet and Van de Ven (1985) revealed that the more frequent recourse to physicians by those with statutory health insurance was related to a higher incidence of illness among these patients than among those with private insurance. On the whole, patients with statutory health insurance were older and in poorer health than patients in the other group were.
The number of general practitioner (GP) services per person is generally expected to be lower in countries where the capitation system predominates, with the incentive that this theoretically gives physicians to limit the number of services per registered patient supposed to overweigh the effect on patient demand of having free health care. However, the analysis of different systems existing alongside one another in Denmark and the Netherlands seems to support the opposite conclusion—that the level of consumption is influenced more by the fact that it is free of charge to the patient than by the method whereby physicians are paid. In these two countries, the number of general practitioner services per insured person using a physician paid a capitation and receiving their treatment free is higher than that for persons covered by the other system, who are generally in better health, consult physicians who are paid on a fee-for-service basis, have to pay the physician themselves, and bear part of the cost. The difference in per capita consumption between publicly and privately insured persons in the Netherlands is 40 percent for physicians as a whole, 28 percent for general practitioners, and 53 percent for specialists. In Denmark, the number of general practitioner services for those insured in Group 1 (with no copayment) is twice that for those insured in Group 2 (less extensive coverage). Faced with an inconsistency of this kind and being unable to control the data for the health status of the population concerned, one has to be cautious with conclusions about impacts.
Data on the consumption of specialist services seem to indicate that access to a specialist is more frequent when referral by a GP is not required. The number of annual contacts with a specialist per person is comparatively higher in Germany (5.0), the United States (3.7), France (3.0), and Canada (2.5) than in the Netherlands (1.8), the United Kingdom (1.2), and Denmark (0.6). However, these figures cannot be used as the basis of an analysis of GPs' referral behavior in relation to the manner in which they are paid because, when access to specialists is free, some consultations are arranged on the initiative of the patients themselves.
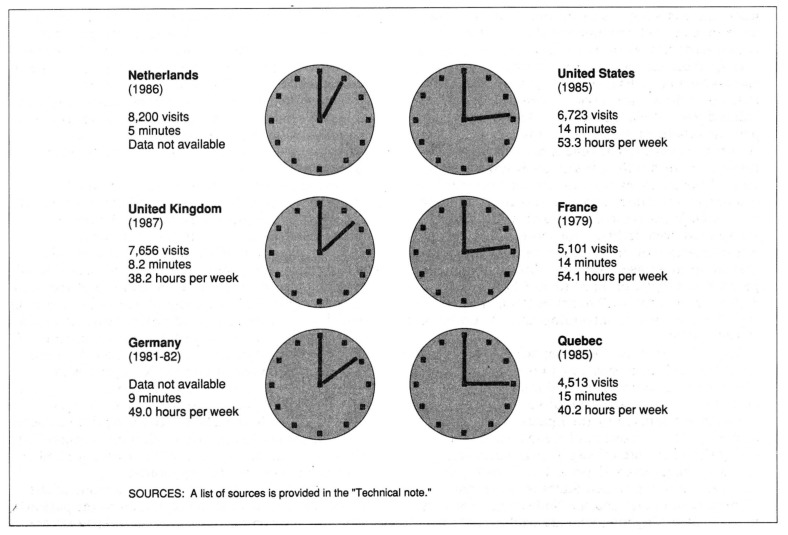
The average length of a GP visit in the countries surveyed varied by a ratio of almost 3 to 1: 5 minutes in the Netherlands in 1985, 9 minutes in Germany during 1981-82, and 14 minutes in the United States in 1985 (Figure 3). It is likely that the content of physician encounters of different lengths also differs, with a more or less detailed interview and a varying number of accompanying tests and examinations. Although the number of countries surveyed is too small to provide conclusive evidence, it would seem that procedures tend to be lengthier when the patient pays the fee directly (United States and France) and when GPs compete with specialists (Germany, United States, and France). Encounters tend to be shorter when the physician is paid a capitation by a health insurance agency without any contribution from the patient.
Figure 3. Number of patient visits per general practitioner per year, average duration of visits, and number of hours worked per week: Selected countries, selected years 1979-87.
The average time spent with a physician, measured by the number of contacts and their duration, is another indicator of the consumption of health care.1 For a general practitioner, it can be reckoned at about 1 hour per person per year in France (67 minutes) and in Germany (57 minutes), whereas in the Netherlands and the United Kingdom, it would seem to be no more than 18 and 33 minutes, respectively. The total amount of time spent with physicians of all types would appear to be about 1 ½ hours in Germany and the United States and roughly 2 hours in France. The ranking of the countries on this basis is thus different from their ranking on the basis of the number of contacts per person and would seem to indicate that the consumption of physicians' time is substantially higher when they are paid on a fee rather than a capitation basis.
Physician workload
The characteristics of the different methods of remuneration play a direct part in determining the income that physicians will derive from their practice for a given amount of work. Conversely, physicians who set themselves an earnings target need to take into account the method of payment for services in determining the output needed to achieve this. Consequently, the method of remuneration is one factor that can influence the way physicians behave when they are providing the health care themselves or referring their patients to other producers of goods and services.
According to the data on physician workload and the number of visits physicians perform in a year, the level of activity differs quite substantially in the countries surveyed. It is not possible to relate these differences to differences in methods of remuneration, because some of the findings are at variance with the theory, the sample is small, and methods of computation may vary.
On the whole, there does not seem to be a strict relationship between the number of visits and the number of hours worked. Visits are shortest in countries where physicians have the most visits. In countries where the average visit lasts less than 10 minutes, i.e., Germany, the Netherlands, and the United Kingdom, the average numbers of visits per general practitioner per year are 10,000, 8,100, and 7,600, respectively. These figures are substantially higher than those recorded for countries where the average visit lasts about 15 minutes: 6,700 visits per GP per year in the United States, 5,100 in France, and 4,500 in Quebec (Figure 3).
Capitation forms the basic remuneration for GPs in the United Kingdom and the Netherlands: Capitation accounts for up to 50 percent of the remuneration of GPs in the United Kingdom and applies to two-thirds of the clientele of GPs in the Netherlands. The fact that GPs in these countries have more visits than their counterparts in the other countries raises doubts as to the theory that the fee-for-service system of payment encourages physicians to increase their output and the system of capitation encourages them to see their patients less frequently. However, this conflict becomes less apparent if one considers their activity in terms of the number of hours worked: GPs in the United Kingdom devote the least amount of time to the provision of care, 38.2 hours a week, compared with more than 50 hours for GPs in France and the United States.
The workload of physicians should not be related to the method of payment without at the same time taking into account the demand factors, the number of physicians, and the financial procedures associated with the methods of remuneration. Moreover, it should be emphasized again that physicians are not alone in determining their level of activity and that, in a system of capitation, the fact that the patient pays nothing generally tends to lead to a higher demand.
The number and distribution of the medical profession are factors that tend to distort the effects of a method of remuneration. The increase in the number of physicians may be associated with the drop in the number of visits per physician that is apparent in each of the countries for which these figures are available, irrespective of the system of remuneration for physicians. For example, the number of visits per GP decreased during the period 1980-86 from 7,448 to 6,723 in the United States, from 5,327 to 5,101 in France, and from 9,847 to 7,656 in the United Kingdom. Both in the United Kingdom, with its capitation system, and in France, with its fee-for-service system, physicians practicing in regions where there is a high concentration of doctors spend more time on each consultation than do their counterparts in regions where there are fewer doctors.
In Quebec, the scale of charges for services over and above a given level of activity was sharply reduced in the fee-for-service system for GPs. The reduced scale of charges seems to have offset the possible inflationary effect of the fee-for-service system of payment. The time spent by Quebec GPs on the delivery of health care services is low (little more than 40 hours) compared with the time spent by their counterparts in other countries who are paid in the same way. What is more, the number of hours worked has been declining for more than 15 years. It was estimated that, in 1972, general practitioners in Quebec spent an average of 49.7 hours treating patients; the figure dropped to 46.8 hours in 1976, 44.6 hours in 1980, 41.9 hours in 1984, and 40.2 hours in 1986 (Contandriopoulos, Fournier, and Boileau, 1988).
The theory that the fee-for-service system is conducive to higher prescribing rates for pharmaceutical products and additional exploratory examinations than capitation or salary is neither proved nor disproved by the figures that have been compiled. The proportion of GP-patient contacts giving rise to the prescribing of pharmaceutical products ranges from 55 percent in Canada and 66.1 percent in the United States to more than 80 percent in France and the Netherlands; for GPs in the United Kingdom, who are paid a capitation, the figure is 74 percent. Part of the explanation for the differences in this case may be the traditions of medical practice and payment of the cost of pharmaceutical products by health insurance agencies. In the United States, for example, patients pay 75 percent of their pharmaceutical costs out of their own pocket (Letsch, Levit, and Waldo, 1988). In France, GPs' higher prescribing rates for pharmaceutical products (more frequent prescriptions and more products per prescription) may, to some extent, counterbalance the lower-than-average admission rate in hospitals in France.
The figures for referrals to other physicians also tie in with the accepted idea that practitioners who are paid a fee prefer to keep their patients and physicians who are paid a capitation are more prone to refer them to other physicians. In France and the United States, where patients can consult specialists directly, the proportion of patients referred by their GP to another physician is relatively low, 2.8 and 5.2 percent, respectively. In contrast, the figures are 8.6 percent in the United Kingdom, where a specialist can be seen only on the recommendation of a GP, and 7.9 percent in the Netherlands, where the same applies to 70 percent of the population. The figures for both Quebec and Germany (8.7 and 9.4 percent, respectively) tend to confirm that the regulations influence behavior. In both Quebec and Germany, access to specialist care is theoretically free, but GPs, who are paid on a fee-for-service basis, refer their patients fairly frequently to other physicians. In Quebec, the scale of charges is calculated in such a way that GPs are not encouraged to perform more services and specialists are not encouraged to recruit patients directly because they are paid a higher rate if the patient is referred to them by a general practitioner. In Germany, under the statutory system of health insurance, a patient who wants to consult a physician other than the one to whom he has surrendered his voucher has to ask for a transfer form.
A question arises as to whether methods of payment also affect other aspects of the provision of health care. Such aspects include the skimming (selection) of patients, emphasis on preventive medicine, provision of a comprehensive and lower geared form of treatment rather than intensive use of sophisticated techniques of examination and specialist expertise, spread of technological innovations, and the split between ambulatory and hospital care. It would be even more risky to answer this sort of question on the basis of the macroeconomic data used for these cross-country comparisons than is the case with questions about overall physician activity. Nonetheless, it appears that the scale of charges (nomenclature, in the case of fee-for-service payment) for the different health care services can substantially affect the orientation of medical practice. A number of examples bear out this hypothesis.
The United Kingdom provides an example of the effectiveness of gearing the capitation to the patient's age so that the elderly, whose health care needs are greater, will not be discriminated against. The fact that persons 65 years of age or over represent the same proportion of a physician's workload in the United Kingdom as in France and the United States (about 20 percent) provides evidence of this.
Another example pertains to tariff changes. The proportion of home visits has declined in all countries. However, the number of home visits has risen in Quebec following a substantial uprating of their tariff, demonstrating that medical practice can be influenced through a change in the scale of tariffs (Contandriopoulos and Fournier, 1983).
Medical practice in every country has been placing increasing emphasis on technical diagnosis and treatment procedures, despite the disparities among the relative scales of charges for different countries. However, in some areas, particularly France and Quebec, what was considered an unduly rapid increase in the use of certain technical procedures has been temporarily checked by making changes in the nomenclature (Contandriopoulos and Fournier, 1983). In fact, the spread or abandonment of particular procedures is primarily a reflection of the development of medical technologies for the treatment, relief, or reassurance of patients. However, at the same time, the behavior of physicians in each specialty can be influenced by the relative scale of charges.
Changes in tariff scales affect the relative position of general practitioners and the different specialists on the earnings ladder. In Ontario, for example, the government leaves it to the medical associations to apportion most of the amount set aside for an increase in tariffs among the different types of medical service.
Physician earnings
Physicians' gross income is determined by their output and the corresponding payments they receive based on the system of remuneration in use. The pretax income that a physician derives from the practice is calculated by subtracting from gross earnings the professional expenses incurred for the performance of work.
In most countries, average physician earnings are, in essence, a reflection of the value that society places on physician services. Apart from the United States, in countries where the cost of health care is financed by the government or by powerful health insurance agencies, a physician's scale of earnings is explicitly or implicitly fixed in advance on the basis of the total amount to be allocated among the physicians and a forecast of the level of activity for the coming year. This is true irrespective of whether physicians are paid on a fee-for-service, capitation, or salary basis. The fee-for-service system of payment is, in theory, more conducive to expenditure overshoots because there may be a sharper-than-expected increase in the number of services performed. However, even in such a case, safeguards like those applied in Germany or Quebec can limit such variations, and they can always be offset the following year.
In order to try to make a cross-country comparison of physician earnings and income in relation to methods of remuneration, a number of different parameters have been used. Physicians' gross and net income have been calculated in U.S. dollars adjusted on the basis of purchasing power parities (PPPs) calculated by the OECD. The purchasing power parities used in this case were based on the gross domestic product (GDP). This means that the crosscountry comparison of the level of physician remuneration is based on a unit that is more meaningful in economic terms than official exchange rates are.
Physician remunerations have been compared with general economic indicators. For example, in each country, the average earnings of a physician have been compared with per capita GDP, and net pretax income has been compared with the average wage. These variables denote the physician's economic status within the community and allow comparisons among countries.
The long-term trend in earnings has been analyzed using series adjusted on the basis of GDP price deflators. These adjustments were made in order to assess the trend in terms of the purchasing power of physician remuneration in each country and also so that a cross-country comparison could be made on the basis of figures that have been adjusted for inflation.
Separate gross and net income series were compiled for GPs and for total physicians. The latter series is an accurate indicator for the medical profession as a whole. However, in each country, it is made up of differing proportions of the various types of specialists, whose scale of earnings differ widely. Surveys carried out in Germany, the United States, and France have shown that pediatricians and psychiatrists were at the bottom end of the income scale for the medical profession, whereas radiologists and surgeons were at the top. The variance in national distributions tends to distort the analysis.
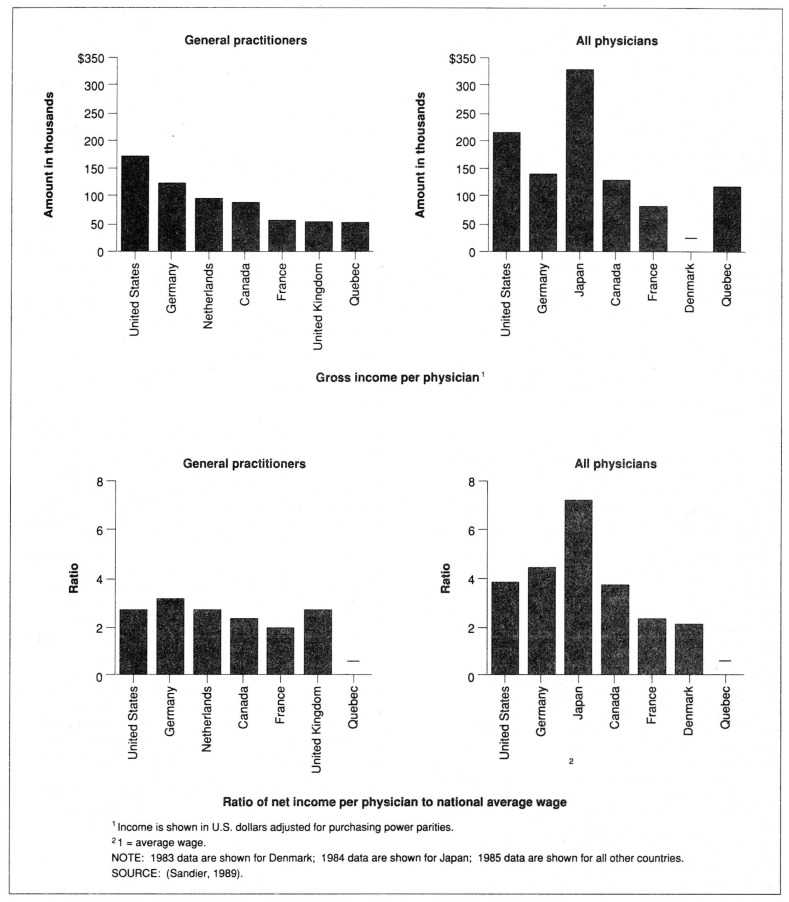
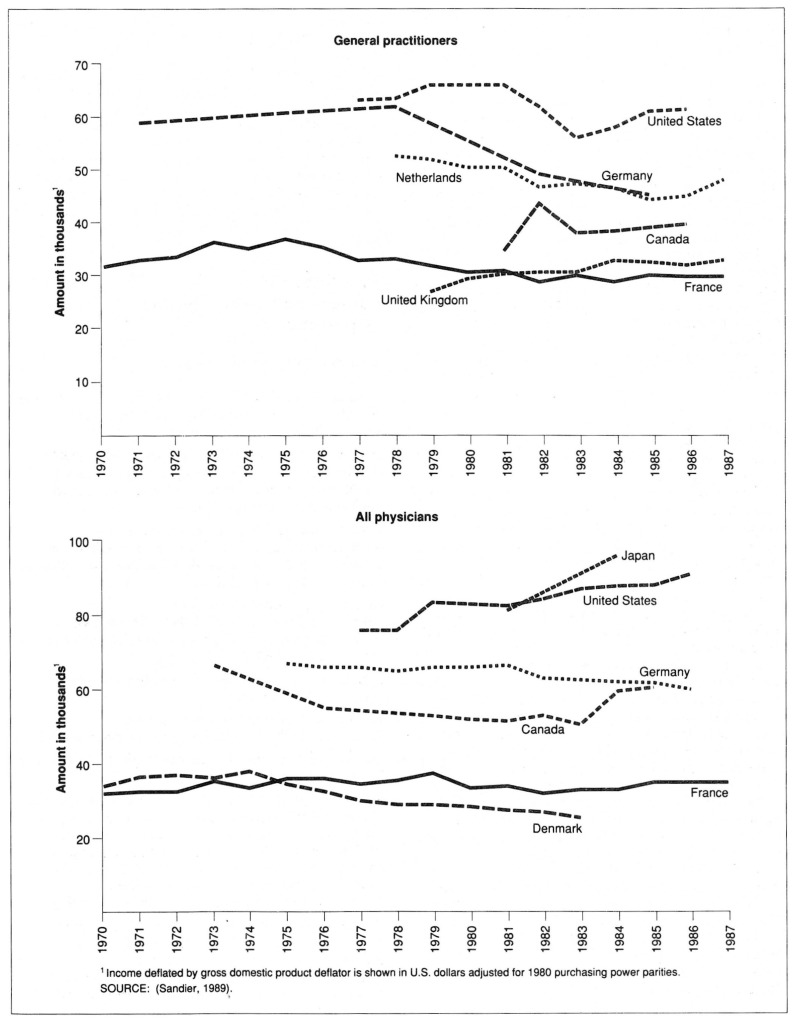
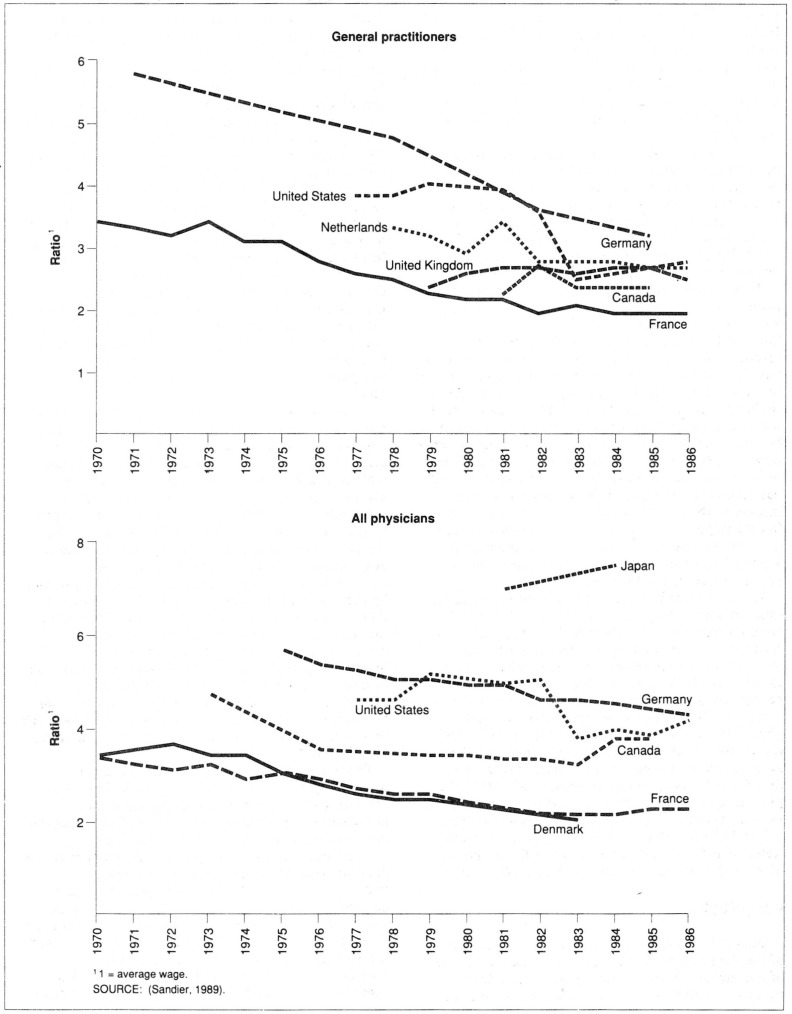
The data that have been collated2 are presented in Figures 4-6. Income is given in PPP-adjusted U.S. dollars. In terms of gross income, Japan has the best paid physicians, followed by the United States and Germany. British, Danish, and French physicians have the lowest earnings. By and large, these differences seem to be related more to countries' economic characteristics than to the methods of remuneration in use. To some extent, this calls to mind the more general link that was shown to exist between a country's economic level and the level of its total expenditure on health care (Organization for Economic Cooperation and Development, 1977, and Schieber, 1987).
Figure 4. Gross income per physician and ratio of net income per physician to national average wage for general practitioners and all physicians: Selected countries, selected years 1983-85.
Figure 6. Income per physician in relative terms for general practitioners and all physicians: Selected countries, selected years 1970-87.
In the case of general practitioners (Figure 4), the most homogeneous category of physicians considered here, average gross income in 1985 was highest in the United States: $174,400, more than twice the figure for Canada and almost three times that for the United Kingdom. However, these disparities become less marked once the figures are adjusted on the basis of national economic indicators. The ratio of net income per physician to the national average wage, an indicator of physicians' relative economic status within their country, falls within a narrower range, 2 to 3.2, the maximum difference between countries being 60 percent between Germany and France. The national average wage, therefore, seems to be a fairly good predictor. For the countries included in the sample, if general practitioners' average income were estimated on the basis of average wage × 2.6, the difference between these estimates and what is believed to be the true figure would be a maximum of 23 percent in the case of Germany and France and less than 10 percent for the other countries. Even if all of this deviation could be ascribed to certain characteristics of the methods of remuneration, the area of their influence on levels of remuneration would appear to be comparatively restricted.
The analysis of average earnings for total physicians does not provide any new insight into the role of method of physician remuneration, but it does yield two further findings. Physicians in Japan, who may practice either as specialists or GPs, appear to be the best paid in absolute and relative terms among the countries considered. Their average gross earnings in 1984 amounted to $325,500, or 1½ times the earnings of U.S. physicians ($202,400), and their average net pretax income was 7.3 times the average wage, compared with figures of 4.4 in Germany and 3.9 in the United States.
In countries for which both total physician and GP incomes are available, the level of income for total physicians is higher than that for GPs. This discrepancy primarily reflects the fact that specialists are, by and large, better paid than GPs. Specialists are generally paid on a fee-for-service basis, and technological innovations often result in scope for increased output for specialists rather than GPs.
By and large, over the past years, physicians' net income has not risen as fast as the national average wage has. This is more marked in the case of GPs than for total physicians (Figure 5). However, in several countries, the sharp downward trend for GPs has, in recent years, been followed by a leveling off of the ratio of net income to average wage, and even a slight upturn in the case of the United States. There was also a narrowing, albeit less marked, of the gap between total physician earnings and the average wage prior to 1983. Since then, however, Germany is the only country among those surveyed where this trend has continued. The ratio of total physicians' net income to the average wage appears to have risen fairly sharply from 1981 to 1984 in Japan. However, it is not possible to be certain that the situation in Japan differs from that in the remaining countries based on figures for 1981 and 1984 only.
Figure 5. Ratio of average net pretax income per physician to national average wage for general practitioners and all physicians: Selected countries, selected years 1970-86.
The difference between the ratios for GPs and for total physicians may result from the fact that GP earnings have risen less sharply than specialist earnings have. It could also reflect changes in the structure of the profession, with specialists, whose earnings are higher, accounting for a growing proportion of the total. Paradoxically, the ratio of income to the average wage could rise for total physicians even if the individual ratios for GPs and specialists remain stable or fall, provided that the average income for specialists is much higher than that for GPs and that the proportion of GPs in the total declines. For example, the index number for the average income for total physicians could rise from 150 to 160 while that for GPs and specialists remains stable at 100 and 200, respectively, if the proportion of general practitioners falls from 50 to 40 percent.
Conclusions
Despite reservations concerning the comparability of the data analyzed, it is possible to draw a number of conclusions from this survey of selected OECD countries. Although these conclusions may have no statistical validity, they are by no means without significance and supplement what can be inferred from the theory.
Methods of payment are applied in so many different ways that it is impossible, from a crosscountry comparison, to make more than a partial assessment of the specific effect on the activity and earnings of physicians of payment of a fee, a salary, or a capitation. The incentives or disincentives theoretically embodied in each method are often offset and sometimes disguised by the influence of the scale of charges, the amount paid by the consumer, and restrictions imposed on access to health care and_ on the activity of physicians.
It seems that the system of funding health care, rather than a particular method of remuneration, is the most potent factor in conditioning the delivery of health care, physician earnings, etc. When the cost of health care is, for the most part, covered by some form of insurance—and this is the case in most OECD countries—the health insurance agencies negotiate the parameters governing remuneration with members of the profession. The amount of influence wielded by these agencies depends on the proportion of health care expenditure that they finance, irrespective of the method by which physicians are paid.
Apart from the United States, where the activity of physicians is still largely governed by market forces, regulations ensure that a physician's total earnings are, in fact, controlled and regulated via a negotiated scale of charges or an overall budget. Physicians' average income, therefore, is the amount that the community either directly or indirectly agrees to pay them, with any deviations from this amount during the year being made good in the following round of negotiations. Generally speaking, under these conditions, physicians as a group have nothing to gain by increasing their output. As individuals, however, they have some scope for improving their position on the scale of earnings for the profession. In some countries, there are provisions, such as a limit on the number of patients on a doctor's list or a sliding scale of charges, designed to limit differences among individual doctors. It seems that there is more room for maneuver with a fee-for-service system of payment than with payment of a capitation and for specialists than for GPs.
The impact of the methods of remuneration themselves appear to be secondary to the impact of other factors on the behavior of patients and physicians—in particular, morbidity in the population, professional ethics, and medical technology.
The number of physician-patient contacts per capita does not seem to be related to the method of remuneration. GPs respond to the quantity of the demand from their patients but seem to have some scope for adjusting the amount of time they devote to them. For example, the duration of medical visits and the average total amount of time spent with a physician are shorter when the physician is paid a capitation by the health insurance agency rather than a fee paid directly by the patient. Similarly, the number of hours worked per week by a physician appears to be shorter under systems of capitation.
The number of medical visits performed by GPs in all of the countries examined has been declining for a number of years. There are several possible reasons for this. Demand may not be sufficiently elastic; average physician workload has decreased with the increase in the number of physicians. The decline in the average number of visits per physician may be a reaction to the budgetary limits that are either implicitly or explicitly fixed in the rules established during negotiations with the health insurance agencies. Therefore, these rules may create an inverse correlation between prices and volume of output, which is the opposite of that generally associated with a classic supply curve.
The national average wage has been shown to be a fairly good predictor of physicians' income. In the case of GPs, it explains more than three-quarters of the variation among countries, thus leaving little room for the method of remuneration as a possible explanatory factor for the level of earnings. A comparable phenomenon in this context is the close and increasing correlation between a country's economic level and its expenditure on health care.
Until the last 4 years, the economic status of GPs, whose income is currently from twice to three times the national average wage (Figure 5) had been deteriorating in most countries (Figure 6). This trend is part of a general pattern of narrowing of income differentials that has been occurring in many countries since the end of the 1960s. Because of this trend, it seems doubtful that physicians have considerable scope to adjust their activity in line with their earnings target. In fact, a number of constraints limit physicians' activity, in particular, those resulting from the increase in their numbers. For physicians as a group, the relative deterioration in economic status is offset by the shift of the profession toward increased specialization.
In recent years, this downward trend has been checked (except in Germany). The ratio of GP income to the average wage has stabilized, and GPs' purchasing power, which had been shrinking, has increased, particularly in the United States. Is this new trend likely to last? The period surveyed here is too short to provide an answer. However, there are three possible explanations of what is happening: a certain loss of enthusiasm for the philosophy of egalitarianism, the perhaps temporary benefits of disinflation, and the comparatively low level to which GP incomes had already descended.
In short, taking into account the difficulties involved in making cross-country comparisons and considering only the countries included in this study, the following conclusion can be made. At present, the influence of the method of remuneration on the behavior of the actors within the health care system seems to be outweighed by other more decisive factors—the coverage of expenditure by health insurance agencies and their powers of intervention, morbidity in the population, medical technology, and the country's economic level.
Acknowledgments
I wish to thank the members of the OECD working party on social policy, both the secretariat and country representatives, for their support, encouragement, and valuable insights. I am particularly grateful to Jean-Pierre Poullier, who not only guided me in obtaining information from the OECD Health Data File but also was kind enough to read the preliminary versions and make valuable comments and suggestions. If, despite this assistance, there are still some errors of interpretation, the responsibility is entirely mine.
Technical note: Sources and computations of parameters
Contacts per capita per year
Canada: Number of physician visits per capita for the period 1984-85, excluding X-rays and analyses: Santé et Bien-Etre Social Canada (1987).
Denmark: Total number of contacts: NOMESKO (1988); OECD data file. Extrapolation of findings of a 1983 inquiry on the number of visits for general practitioners: Chadwick (1987).
France: Author's estimate based on service reimbursement by the Health Insurance Scheme and Centre de Recherche, d'Etude et de Documentation en Economie de la Sante (1989).
Germany: Personal contacts with physicians: Schwartz et al. (1984). Breakdown between general practitioners and specialists derived from Delozier et al. (1989).
Japan: Information received from the Japanese delegation to the OECD.
Netherlands: Health Interview Survey, Aug.-Sept. 1988: Central Bureau voor de Statistiek.
Quebec: Figures compiled by the Regie de l'Assurance Maladie du Quebec.
United Kingdom: Office of Population Censuses and Surveys (1986). According to estimates based on the survey General Medical Practitioners' Workload, 1985-86, the number of GP consultations per person has remained stable since 1981. The figure for specialists is based on hospital consultations (Department of Health and Social Security, 1987).
United States: Data from the 1986 National Health Interview Survey of NCHS. For the GP-specialist breakdown, the ratio of 31 percent to 69 percent was used, based on data from the 1981 National Ambulatory Medical Care Survey of NCHS.
Percentage of users
Canada: Health and Welfare Canada (1981).
France: Charraud and Mormiche (1986); Caisse Nationale d'Assurance Maladie des Travailleurs Salaries (1982).
Germany: Ingolstadt, quoted in Geissler (1981).
Japan: Information received from the Japanese delegation to the OECD.
Netherlands: Health Interview Survey, Aug.-Sept. 1988: Central Bureau voor de Statistiek.
Quebec: Figures compiled by the Regie de l'Assurance Maladie du Quebec.
United Kingdom: Office of Population Censuses and Surveys (1986); Cartwright and Anderson (1981).
United States: Data from the 1986 National Health Interview Survey of NCHS.
Duration of physician visits
France: Letourmy (1979).
Germany: Duration of 11.3 minutes in the case of interns: Schwartz et al. (1984).
Netherlands: Central Bureau voor de Statistiek (Jan. 1986).
United Kingdom: Department of Health and Social Security (1987).
United States: Data from the 1985 National Ambulatory Medical Care Survey of NCHS.
Physicians' workload
Canada and Quebec: Taylor, Stevenson, and Williams (1984); Contandriopoulos, Fournier, and Boileau (1988).
France: Self-employed physicians: Bui Dang Ha Doan (1980).
Germany: Gesundheitswesen (1988).
United Kingdom: All activities relating to care: Department of Health and Social Security (1987).
United States: American Medical Association (1987). Care includes direct care of patients plus interpretation of results of tests.
Outcome of physician contacts
Canada: Prescription of pharmaceuticals, 1977 data: IMS Canada, 1988. Number of services: Taylor, Stevenson, and Williams (1984).
France: Le Fur and Sermet (1985); Institut National de la Sante et de la Recherche Medicale (1976).
Japan: Information received from the Japanese delegation to the OECD.
Netherlands: Estimates based on findings from the Health Interview Survey: Central Bureau voor de Statistiek (various years).
Quebec: Estimated rate of referral to a specialist: Taylor, Stevenson, and Williams (1984).
United Kingdom: Estimates based on findings from the 1984 General Household Interview Survey: Abel-Smith (1981). Number of services: Department of Health and Social Security (1987).
United States and Germany: Ambulatory care comparisons: Delozier et al. (1989). Number of services in the United States: American Medical Association (1987). Number of services in Germany: Schwartz et al. (1984).
Gross earnings of physicians
Canada: Santé et Bien-Etre Social Canada (1984 and 1985).
France: Centre de Recherche, d'Etude et de Documentation en Economie de la Sante (1989).
Germany: Schneider, Sommer, and Kececi (1987); Brenner (1988).
Netherlands: Author's computation using Ministerie van Volksgezondheid en Milieuhygiene (1985); Central Bureau voor de Statistiek (1988).
Quebec: Contandriopoulos and Fournier (1983).
United Kingdom: Review Body on Doctors' and Dentists' Remuneration (1987) for data since 1980. Earlier data were estimated by Centre de Recherche, d'Etude et de Documentation en Economie de la Sante.
United States: American Medical Association (1987). For GPs: average of GPs and family practice.
Net income before taxes
Canada: 62 percent of gross income (1984 ratio for physicians with at least one visit during each trimester).
France: 60 percent of gross income.
Germany: Brenner (1988); Geissler (1981).
Japan: Information received from the Japanese delegation to the OECD.
Netherlands: 60 percent of gross income.
United Kingdom: Review Body on Doctors' and Dentists'Remuneration (1987).
United States: American Medical Association (1987).
Population, gross domestic product, and deflator
Organization for Economic Cooperation and Development (1988a and 1988b); Poullier, Gillion, and Schieber (1985).
Footnotes
The estimates used here were derived by multiplying the number of services by their average duration. Because the figures are not always for the same years, the estimates can provide only an approximate idea of the situation.
The earnings and income figures for GPs and physicians as a whole have been either derived from national published data or calculated by the author. All variables are available for Canada, the United States, France, and Germany. Some countries have been included only for certain of the variables: general practitioner earnings and income in the case of the United Kingdom, general practitioner earnings in the case of the Netherlands and Quebec, net income for physicians as a whole in the case of Denmark and Japan.
The main ideas for this article were put together during 1988, which the author spent at the Organization for Economic Cooperation and Development on sabbatical from the Centre de Recherche, d'Etude et de Documentation en Economie de la Santé (Sandier, 1989). More detailed work is expected to be published in due course.
References
- Abel-Smith B. Alternative Methods of Physician Compensation and Their Effects on Physician Activity, an International Comparison: Country Report for the United Kingdom. Paris: Centre de Recherche pour l'Etude et l'Observation des Conditions de Vie; 1981. [Google Scholar]
- American Medical Association. Socioeconomic Characteristics of Medical Practice, 1987. Chicago: 1987. [Google Scholar]
- Brenner G. Realinkommen weiter Rückläufig. Arzt und Wirtschaft. 1988;6:11–16. [Google Scholar]
- Bui Dang Ha Doan L'activite professionnelle des medecins en 1977. Cahiers de Sociologie et de Démographie Médicates. 1980;1(special issue):1–58. [Google Scholar]
- Qui Consomme Quoi? Paris: CNAMTS; 1982. Caisse Nationale d'Assurance Maladie des Travailleurs Salaries. [Google Scholar]
- Cartwright A, Anderson R. General Practice Revisited: A Second Study of Patients and Their Doctors. London: Tavistock; 1981. [Google Scholar]
- Central Bureau voor de Statistiek. Maandbericht Gezondheidstatistiek. Various issues. S'Gravenhage; Various years. [Google Scholar]
- Centre de Recherche, d'Etude et de Documentation en Economie de la Santé. ECO-SANTE, un Logiciel pour Analyser l'Evolution du Système de Santé en France. Paris Medsi: McGraw-Hill; 1989. Software. [Google Scholar]
- Chadwick LK. Unpublished report. London: 1987. Incentives Influencing General Practitioners in Selected European Health Systems: A 1985 Comparative Study. [Google Scholar]
- Charraud A, Mormiche P.Disparites de consommations medicales, Enqueue Santé 1980-1981 Collections de I'INSEE (Institut National de la Statistique et des Etudes Economiques) Series M(118)111351986 [Google Scholar]
- Contandriopoulos AP, Fournier MA. Les Services Médicaux au Québec. Montréal, Canada: Groupe de Recherche Interdisciplinaire en Santé, University of Montréal; 1983. [Google Scholar]
- Contandriopoulos AP, Fournier MA, Boileau H. Les Effectifs Médicaux au Québec: Situation de 1972 à 1986 et Projections pour 1990. Québec, Canada: Corporation Professionnelle des Médecins du Québec; 1988. [Google Scholar]
- Contandriopoulos AP, Lemay A, Tessier G. Les Publications du Québec. No. 29. Québec, Canada: 1987. Les coûts et le financement du systeme socio-sanitaire. [Google Scholar]
- Delozier J, et al. Vital and Health Statistics. No. 5. National Center for Health Statistics, Public Health Service; Washington: U.S. Government Printing Office; Jun, 1989. Ambulatory care comparisons: France, Federal Republic of Germany, and the United States of America. (Series 5). [PubMed] [Google Scholar]
- General Medical Practitioners' Workload. London: 1987. Department of Health and Social Security. [Google Scholar]
- Geissler U. Alternative Methods of Physician Compensation and Their Effect on Physician Activity: Country Report for the Federal Republic of Germany. Paris: Centre de Recherche pour l'Etude et l'Observation des Conditions de Vie; 1981. [Google Scholar]
- Gesundheitswesen. Medizinische und Ökonomische Orientierung. Baden-Baden: Federal Republic of Germany; 1988. [Google Scholar]
- Glaser WA. Paying the Doctor. Baltimore, Md.: The Johns Hopkins Press; 1970. [Google Scholar]
- Health and Welfare Canada. The Health of Canadians. Ottawa, Canada: 1981. [Google Scholar]
- Hogarth J. Payment of the General Practitioner. Oxford, England: Pergamon Press; 1963. [Google Scholar]
- IMS Canada. Personal communication. 1988
- Institut National de la Santé et de la Recherche Medicale. Les Malades en Médecine Libérale: Qui Sont-Ils? De Quoi Souffrent-Ils? Paris: 1976. [Google Scholar]
- Kassenärztliche Bundesvereinigung. Grunddaten zur Kassenärztlischen Versogung in der Bundesrepublick Deutschland. Bonn: Federal Republic of Germany; Undated. [Google Scholar]
- Le Fur P, Sermet C. Clientèle, Morbidité, Prescriptions en Médecine Libérale. Paris: Centre de Recherche, d'Etude et de Documentation en Economie de la Santé; 1985. [Google Scholar]
- Letourmy A. Etude du Comportement du Médecin Généraliste de Ville. Paris: Centre de Recherches et d'Etudes sur le Bien-Etre; 1979. [Google Scholar]
- Letsch SW, Levit KR, Waldo DR. Office of Research and Demonstrations, Health Care Financing Administration. Health Care Financing Review. No. 2. Vol. 10. Washington: U.S. Government Printing Office; Winter. 1988. National health expenditures, 1987. HCFA Pub. No. 03276. [PMC free article] [PubMed] [Google Scholar]
- Ministerie van Volksgezondheid en Milieuhygiene. Financieel Overzicht van de Gezondheidzorg. The Netherlands: Various years. [Google Scholar]
- NOMESKO. Health Statistics in the Nordic Countries. Copenhagen, Denmark: 1988. [Google Scholar]
- Office of Population Censuses and Surveys. General Household Survey, 1984. London: Her Majesty's Stationery Office; 1986. [Google Scholar]
- Organization for Economic Cooperation and Development. Les Dépenses Publiques de Santé. Paris: 1977. [Google Scholar]
- Organization for Economic Cooperation and Development. Banque de Données sur le Secteur de la Santé. Paris: 1988a. Data tape. [Google Scholar]
- Organization for Economic Cooperation and Development. Comptes Nationaux Principaux Agrégats, 1960-1988. Paris: 1988b. [Google Scholar]
- Poullier JP, Gillion C, Schieber G. La Santé en Chiffres, 1960-1983, Dépenses, Coûts, Résultats. Paris: Organization for Economic Cooperation and Development; 1985. [Google Scholar]
- Regie de l'Assurance Maladie du Québec. Statistiques Annuelles. Québec, Canada: Various years. [Google Scholar]
- Reinhardt U, Sandier S, Schneider M. Die Wirkungen von Vergütungs-Systemen auf die Einkommen des Ärzte, die Preise und auf die Struktur Ärztlicher Leistungen im Internationalen Vergleich. Augsburg, Federal Republic of Germany, Paris: BASYS and Centre de Recherche, d'Etude et de Documentation en Economie de la Santé; 1986. [Google Scholar]
- Review Body on Doctors' and Dentists' Remuneration. Seventeenth Report. London: Her Majesty's Stationery Office; 1987. [Google Scholar]
- Sandier S. The Payment of Physicians in Selected OECD Countries. Paris: Organization for Economic Cooperation and Development; Mar. 1989. [Google Scholar]
- Santé et Bien-Etre Social Canada. Etude sur le Revenu des Médecins par Spécialité. Ottawa, Canada: 1984. [Google Scholar]
- Santé et Bien-Etre Social Canada. Les Gains des Médecins au Canada, et Mise à Jour. Ottawa, Canada: 1985. [Google Scholar]
- Santé et Bien-Etre Social Canada. Utilisation des Services de Médecins, 1980-81 à 1984-85. Ottawa, Canada: 1987. [Google Scholar]
- Schieber G. Santé: Financement et Prestations, Analyse Comparée des Pays de l'OCDE. Paris: Organization for Economic Cooperation and Development; 1987. [Google Scholar]
- Schneider M, Sommer J, Kececi A. Gesundheitssysteme in Internationalen Vergleich Gesundheitsforschung 160. Augsburg, Federal Republic of Germany: BASYS; 1987. [Google Scholar]
- Schwartz FW, Kerek-Bodden HE, Schach E, et al. The Ambulatory Medical Care Survey in FRG, 1981-1982, the EVAS-Study; Paper presented at the International Epidemiological Association Meeting; Vancouver, Canada. 1982; 1984. Edited in. [Google Scholar]
- Taylor MG, Stevenson HM, Williams AP. Medical Perspectives on Canadian Medicare. Institute of Behavioural Research, York University; 1984. [Google Scholar]
- Van Vliet R, van de Ven W. Differences in Medical Consumption Between Publicly and Privately Insured in the Netherlands; Paper presented at the International Meeting on Health Econometrics; Rotterdam, The Netherlands. 1985. [Google Scholar]