Abstract
Objective:
The aim of this study was to use an instrument, the menopause-specific quality-of-life satisfaction in the state of Qatar for the premenopausal, menopause and postmenopausal period.
Design:
A cross-sectional descriptive study was used to generate menopause symptoms experienced by Arabian Gulf women. Measurement-specific quality-of-life satisfaction questionnaires and face-to-face interviews were performed.
Setting:
Primary Health Care (PHC) Centers in Qatar.
Materials and Methods:
A multistage sampling design was used and a representative sample of 1,500 women aged 40-60 years were included during July 2012 and November 2013, and 1,158 women agreed to participate (77.2%) and responded to the study.
Results:
The mean age and standard deviation of the subjects was 50.9 ± 6.1. The median age of natural menopause in the present study was 49 years [mean and standard deviation 49.9 ± 2.7]. The rate of consanguineous marriages in the sample was found to be 30.3%. There were statistically significance differences between menopausal stages with regard to ethnicity, education level, occupation, type of housing condition, and consanguinity. There were statistically significance differences between menopausal stages concerning BMI groups, Systolic BP, Diastolic BP, physical activity, parity, and sheesha smoking habits. Meanwhile, the present study revealed that the most common disease was found to be diabetes mellitus (11.4%), followed by hypertension (6.6%), asthma (5.6%) and CHD (2.5%), and the majority of subjects (69.5%) had no specific disease. The most frequent symptom was aches in the back and neck (49.2%), night sweat (37.2%), low backache (35.7%), feeling nervous (35.4%) followed by aches in the muscles/joints (34.6%), hot flashes (33.3%), decreased social activities (28.3%), decreased leisure activities (47.6%), difficulty sleeping (28.9%), mood swings (25.4%), and decreased concentration (28.3%), sexual activity (24.1%) and total energy level (26.7%). The lowest reported symptoms were facial hair at 16.1% followed by dissatisfied with my personal life at 18.1%. Cronbach's alpha scores, measuring the internal consistency of questions in each domain for physical, vasomotor, psychosocial and sexual were 0.883, 0.853, 0.697 and 0.805, respectively. The Spearman's rank correlation coefficient between domains indicated that there is highly significant concordance between the four domains (P < 0.001).
Conclusion:
A large number of factors were associated with experiencing menopausal symptoms and which had negative effects on the quality of life among Arabian women. The current study showed that climacteric symptom in menopausal Arab women is less than Western women, which may be influenced by socio-economic, genetics, environment and parity.
Keywords: Disease, menopause, premenopause, postmenopausal, physical activity, quality of life, Qatar, socio-demographic
INTRODUCTION
Menopause is the cessation of a woman's reproductive ability, the opposite of menarche. Menopause is usually a natural change; it typically occurs in women in midlife, during their late 40s or early 50s, signaling the end of the fertile phase of a woman's life.[1] Menopause is commonly defined by the state of the uterus and the absence of menstrual flow or “periods,” but it can instead be more accurately defined as the permanent cessation of the primary functions of the ovaries.[2] The transition from a potentially reproductive to a non-reproductive state is normally not sudden or abrupt, occurs over a number of years, and is a consequence of biological aging.[3,4,5,6,7] Worldwide, hot flashes are among the most commonly reported symptoms among women transitioning through menopause, and in certain populations, hot flashes affect up to 75% of women undergoing this transition.[6,7] Both the perimenopausal and postmenopausal stages of the transition are characterized by hot flashes, with perimenopause lasting 5-10 years.[3,7,8] in some populations. With an anticipated 1.2 billion perimenopausal or postmenopausal women by 2030,[9] there will be a large population of women affected by hot flashes. Ameliorating the effect of hot flashes on daily life is important because hot flashes are associated with a decrease in quality of life (QOL) and are the most common reason for seeking medical intervention during the menopausal transition.
Many women are likely to live more than 30 years after menopause, spending about one-third of their lives in a state of estrogen deficiency.[2] Age at natural menopause is an important research issue because of the suspected links between it and the risk for certain diseases. Without intervention, more than 75% of these females will suffer the distressing sequelae of menopause,[2,6,7] which include headache, irritability, fatigue, depression ,[3] nervousness, poor concentration,[2] sexual dysfunction,[9,10] physical, psychological and psychiatric disorders[5] and the more worrying effects of menopause-related osteoporosis and ischemic heart disease [IHD].[11] It could also be a strong biomarker of the general aging pattern of individual.[12]
Headache, trouble sleeping, mood swings, vasomotor symptoms such as hot flash, and night sweats, somatic symptoms such as vaginal dryness, or atrophy and dyspareunia, as well as psychological symptoms such as anxieties, difficulty in concentrating, overreacting to minor upsets, quickly being irritated, forgetfulness are symptoms of menopause and affect all dimensions of life quality.[13,14,15] The duration, severity, and impact of these symptoms vary from person to person, and population to population.[2,14,15,16,17]
The date of menopause (in a woman with an intact uterus) is the date when the final menstrual flow finishes. Premenopause is a term used for the years leading up to the last period, when the levels of reproductive hormones are already becoming more erratic and lower, and the effects of hormone withdrawal may be present.[5]
The term “perimenopause,” which literally means “around the menopause,” refers to the menopause transition years, a span of time both before and after the date of the final episode of flow. According to the North American Menopause Society, this transition can last for four to eight years[3] and the Centre for Menstrual Cycle and Ovulation Research describes it as a six- to 10-year phase ending 12 months after the last menstrual period.[4,5,6]
The term postmenopausal describes women who have not experienced any menstrual flow for a minimum of 12 months, assuming that they do still have a uterus, and are not pregnant or lactating.[1,3] In women without a uterus, menopause or postmenopause can be identified by a blood test showing a very high FSH level. Any period-like flow during postmenopause, even spotting, must be reported to a doctor.
Most recently several reports described the perimenopausal symptom experience of women from developing countries, with particular emphasis upon estrogen-related menopause symptoms (day sweat, hot flashes, night sweat and vaginal dryness),[2] and a measurement-specific QOL satisfaction during menopause in Canada.[17] The aim of this study was to collect such information in Qatar using the menopause-specific QOL satisfaction instrument (MENQOL), developed by Bener et al.[2] and Hilditch et al.[17] for the midlife period.
MATERIALS AND METHODS
Study design
This is a cross-sectional Primary Health Care (PHC) Centers-based study conducted in the state of Qatar. The survey was conducted among Qatari national and Arab women aged 40-60 years old, who had not had a hysterectomy, and who had not used hormone therapy during the preceding 6 months. Similar to other reported studies.[2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17] women were excluded with contraindications to estrogen use and, women who had a current unstable medical or social problem.
The study was approved by the IRB of Research Ethics Committee of Hamad Medical Corporation (HMC RC#8222/08), and by the IRB of Weill Cornell Medical College (WCMC-Q).
Questionnaire and interview
The questionnaire and criteria for the menopause-specific QOL (MENQOL) defined and proposed by Hilditch et al.[17] and Bener et al.[2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19] were used. Respondents were asked to indicate if they had experienced symptoms or problem within the past month and, if so, to rate how bothersome it was on a seven-point Likert scale.[2] The questionnaire had 29 questions divided logically into four domains: Physical, emotional (vasomotor), psycho-social and sexual areas, and additional socio-demographic sections, and allowed inclusion of additional symptoms or problems. For each question, an importance score was calculated as the product of the frequency that the problem was experienced, by the mean extent that the symptom was bothersome of women who experienced it. Furthermore, the questionnaire was immediately followed by a comprehensive clinical interview by a General Practitioner.
The data were collected through a validated questionnaire with the help of qualified nurses who were Arab nationals and could speak and write English and Arabic languages well and were aware of the Arabic culture and thus were able to engage and gain the trust of the study participants. Data collection took place from July 2012 to November 2013. The sample size was determined on a priori presumption that the prevalence rate of postpartum depression in Qatar would be more or less similar to rates found in other countries in the eastern Mediterranean, where the reported prevalence of postpartum depression to be 20%, with the 95% confidence interval for 2.5% error of estimation, a sample size of 1,500 subjects would be required for this study. Of the 22 primary health care centers available, we have selected 12 health centers, of these, 10 were located in urban and 2 in semi-urban areas of Qatar. Finally, subjects were selected systematically 1-in-2 using a sampling procedure. Each participant was provided with a brief information about the study and was assured of strict confidentiality. Of the 1,500 women living in urban and rural areas, 1,158 women agreed to participate (77.2%) and responded to the study; 342 (22.8%) subjects did not participate due to lack of time and incomplete questionnaire were excluded. The survey instrument was initially tested for validation on 100 patients through face-to-face interview who visited the health centers. Test-retest reliability measures, using intra-class correlation coefficients were 0.83, 0.82, 0.74 and 0.64 for the physical, psychosocial, sexual domains and the QOL question.
Data were analyzed using SPSS version 21. Student-t test was used to ascertain the significance of differences between mean values of two continuous variables and confirmed by non-parametric Mann-Whitney test. Chi-square test and the Fisher exact test (two-tailed) were performed to test for differences in the proportion of categorical variables between two or more groups. Kruskal Wallis one-way analysis of variance (ANOVA) was employed for comparison of several group means. The Spearman's correlation coefficient was used to evaluate the strength of concordance between variables. All statistical tests were two-sided and P < 0.05 was considered statistically significant.
RESULTS
The mean age and standard deviation of the women was 50.9 ± 6.1. The median age of natural menopause in the present study was 49 years [mean and standard deviation 49.9 ± 2.7]. The rate of consanguineous marriages in the sample was found to be 33.3%.
Table 1 shows the socio-demographic characteristics of studied subject by premenopausal, perimenopausal and postmenopausal status. There were statistically significance differences between menopausal stages with regards to ethnicity, education level, occupation, type of housing condition, and consanguinity.
Table 1.
The socio-demographic characteristics of studied subjects by premenopausal, menopause and postmenopausal status
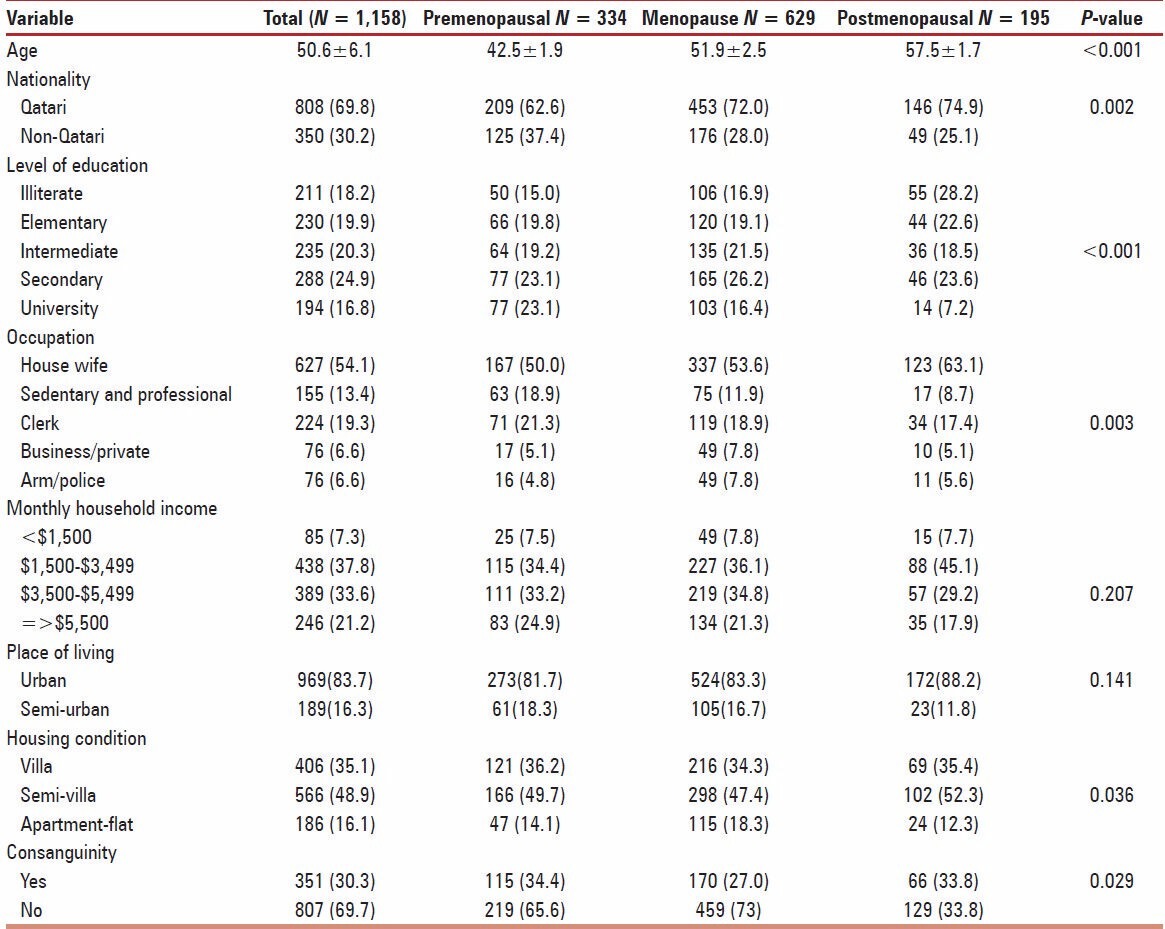
Table 2 presents the lifestyle characters of studied subject by premenopausal perimenopausal and postmenopausal status. This table shows there were statistically significant differences between menopausal stages concerning BMI groups, Systolic BP, Diastolic BP, physical activity, parity and sheesha smoking habits. The most common disease was found to be diabetes mellitus (11.4%), followed by hypertension (6.6%), asthma (5.6%) and CHD (2.5%), and the majority of subjects (69.5%) had no specific disease.
Table 2.
The lifestyle characters of studied subject by premenopausal, menopause and postmenopausal
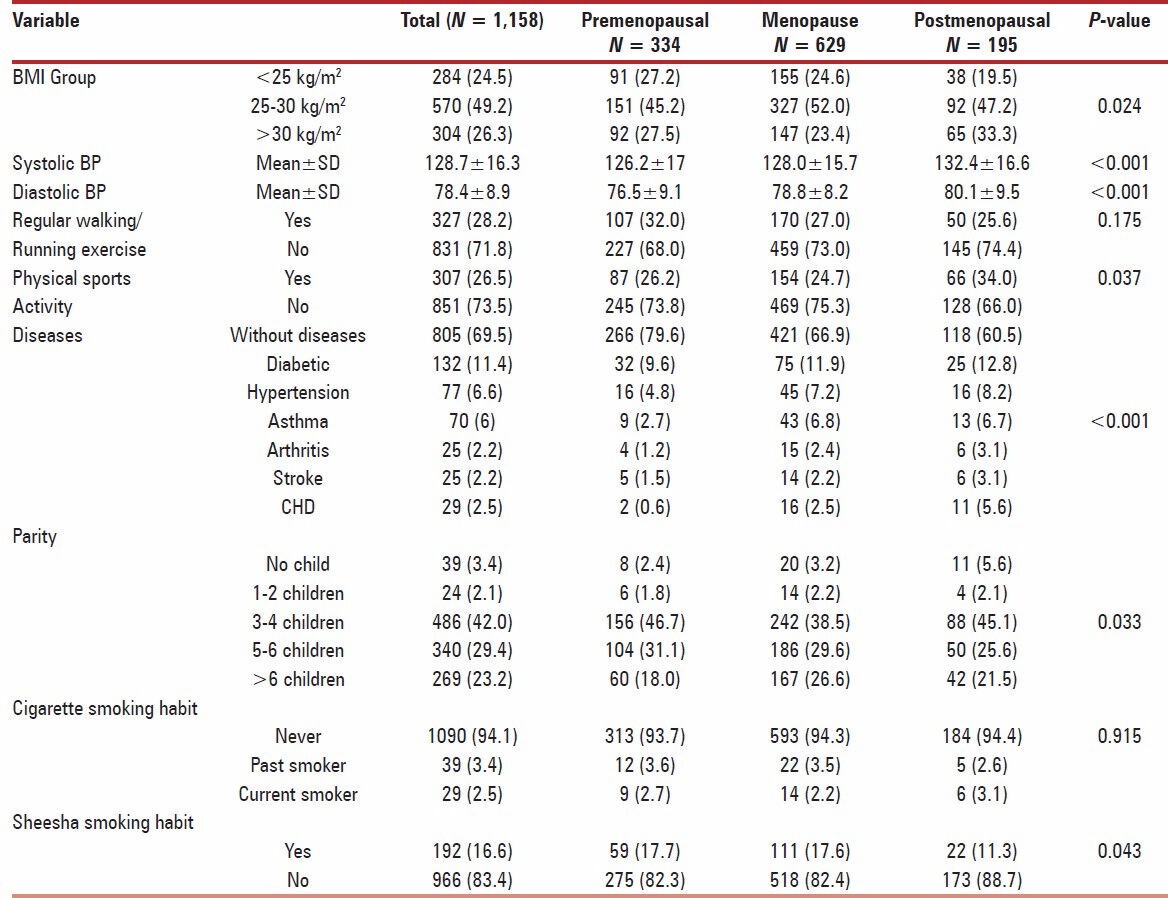
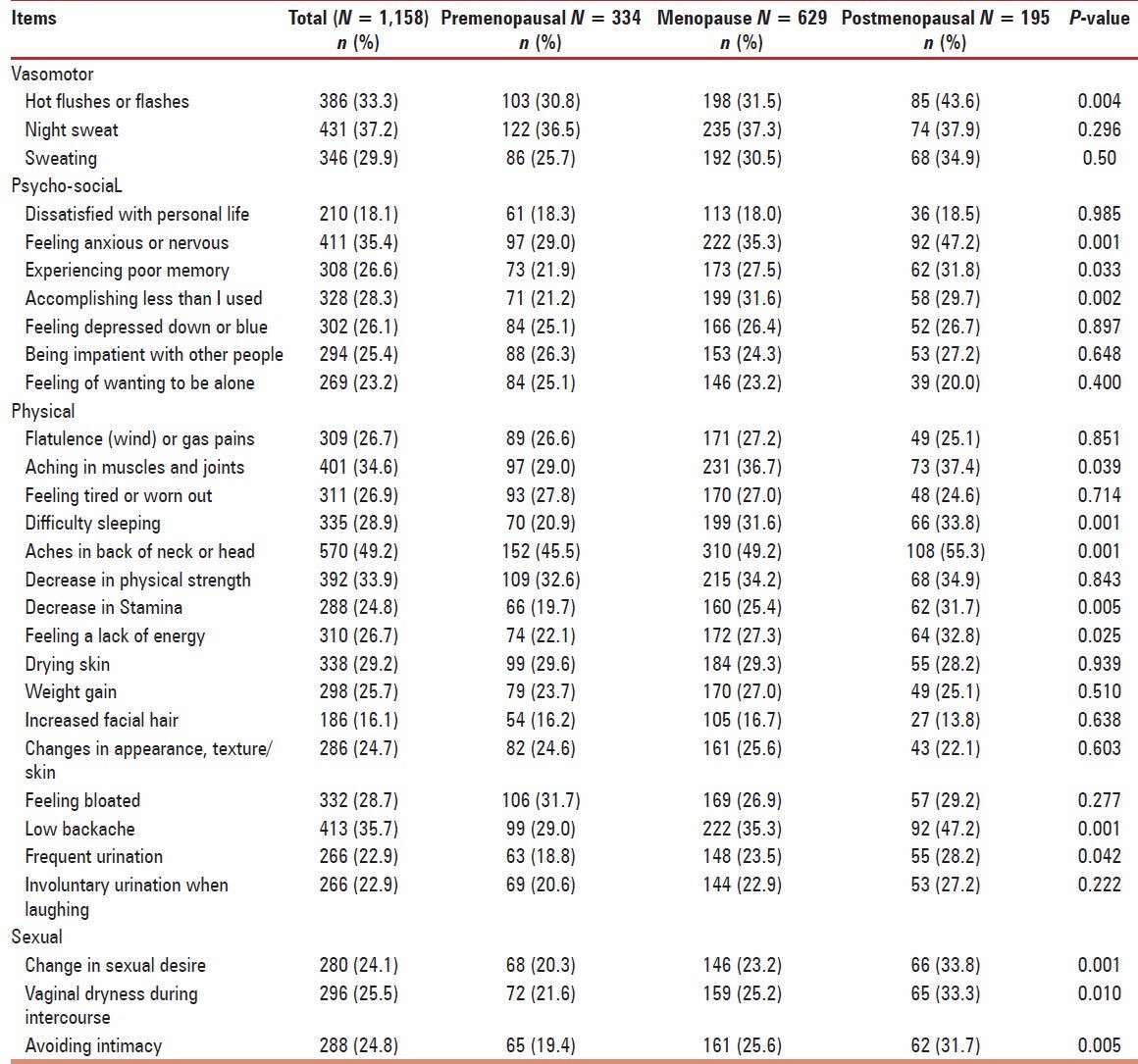
Table 3 gives the frequency of menopause-specific QOL questionnaire responses. The most frequent symptom was “aches in the back and neck” at 49.2%, night sweat (37.2%), low backache (35.7%), feeling nervous (35.4%) followed by “aches in the muscles/joints” at 34.6%, hot flashes (33.3%), decreased social activities (28.3%) and leisure activities (47.6%), difficulty sleeping (28.9%), mood swings (25.4%), and decreased concentration (28.3%), sexual activity (24.1%) and total energy level (26.7%). The lowest reported symptoms were “facial hair” at 16.1% followed by “dissatisfied with my personal life” at 18.1%.
Table 3.
The Menopause-Specific Quality of Life Questionnaire (MENQOL) by pre-menopausal, menopause and postmenopausal (N = 1,158)
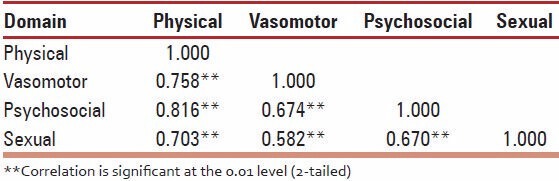
Cronbach's alpha scores, measuring the internal consistency of questions in each domain are shown in Table 4 for physical, vasomotor, psychosocial and sexual domains, were 0.883, 0.853, 0.697 and 0.805, respectively. Spearman's rank correlation coefficient between domains is presented in Table 5. This table indicates that there is highly significant concordance between the four domains (P < 0.001).
Table 4.
Internal consistency (N = 1,158)
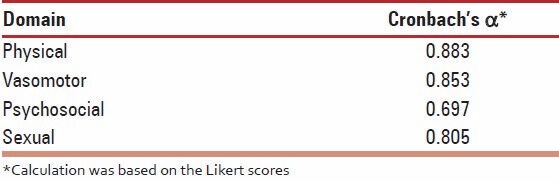
Table 5.
Spearman's correlation matrix: Calculation based on presence/absence of symptoms
DISCUSSIONS
QOL has been defined by the World Health Organization[18] as an “individual's perception of their position in life in the context of the cultural and value systems in which they live and in relation to their goals, expectations, standards and concerns.”[2,14,15,16,17] Various validated tools have been used to determine the influence of the climacteric over QOL; among them is the MENQOL proposed by Hilditch et al.[17]
During perimenopause, estrogen levels average about 20-30% higher than during premenopause, often with wide fluctuations in levels.[4] These fluctuations cause many of the physical changes during perimenopause as well as menopause.[2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18] Some of these changes are hot flashes, night sweats, difficulty sleeping, vaginal dryness or atrophy, incontinence, osteoporosis, and heart disease. During this period, fertility diminishes, but is not considered to reach zero until the official date of menopause. The official date is determined retroactively, once 12 months have passed after the last appearance of menstrual blood. During the perimenopause years, many women undergo noticeable and clinically observable physical changes resulting from hormonal fluctuations. The best known of these is the “hot flash” or “hot flush.”
Menopause is a biological process characterized by cessation of the menstrual cycle in women with a decline in age approximately between 40 and 60 years with the average age observed in the 52 years.[2] Symptoms experienced during menopause and socio-demographic characteristics affect the QOL in postmenopausal women. Hot flashes impact the daily activities of most postmenopausal women, especially those with more frequent/severe symptoms. Treatments that safely and effectively treat these symptoms could improve QOL among postmenopausal women.[20] Menopause is a unique experience. It is not a type of disease, but rather a stage in biological and physiological development. Menopause produces very complex changes during this stage of life, which include psychological and social changes.[2] However, in our study, the median age of menopause was 49 years, which is significantly lower than reports from Europe, North America and America.[3,4,5,6,7,8,9,10,11,12,13,14,15,16,17] Therefore, natural menopause in Qatar women starts at least 2 years earlier than their Western counterparts. It is worthy to note that the estimation of age at menopause may be influenced by the study design (e.g., the age range of the participants). In China,[21] early postmenopausal women presented worst QOL in vasomotor, psychosocial and physical domains. The gradually declining sexual QOL was related to the advancement of menopause. Age had a negative impact on QOL in vasomotor and sexual domains.
The reported symptomatology of menopause was different in these Qatari women than in other reports.[3,4,5,6,7,8,9,10,17,20,21,22,23,24,25,26] Compared to most reports, the symptoms were fewer and of lesser severity. In Turkey, similar to this study.[22] stepwise multiple regression analyses showed that these variables were predictors: Health problems, recent life stresses, being a primary school graduate, absence of relaxation methods, number of pregnancy, financial problems, tea consumption, inadequate and unbalanced nutrition, coffee consumption, age, being a secondary school graduate and dissatisfaction in marriage. In a report from Thailand,[23] menopausal symptoms were much higher than reported here; vasomotor symptoms were at 72.3%, and psychological symptoms were at 98.3%. Symptoms in a Czech population were also high, 58% reporting vasomotor symptoms[24] vs. 40% in this population. Although most of the studies report higher rates than ours, however, this is not always true. Filipino American women[25] were reported to have a similar pattern as the women in this study; 37.6% “hot flashes” vs. our 33.1%, and 24.2% “night sweats” vs. our 28.5%. A UAE study conducted by Bener et al.[2] reported that overall 69% of the women reported physical symptoms, 58.7% reported psychosocial symptoms, 40% reported vasomotor symptoms and 37.9% reported sexual symptoms. This is confirmative with the present study.
With the increase in the life expectancy, a woman spends almost a third of her life in menopause.[26] The transition from the reproductive to the non-reproductive stage is the result of a reduction in the female hormonal production by the ovaries. This transition is normally not sudden or abrupt; it tends to occur over a period of years, and it is a natural consequence of aging. However, for some women, the accompanying signs and effects that occur during the menopause transition years can significantly disrupt their daily activities and their sense of well-being. Numerous physical and psychological symptoms have been attributed to the hormonal changes of menopause. The overall health and well-being of middle-aged women have become a major public health concern around the world. More than 80% of the women experience physical or psychological symptoms in the years when they approach menopause, with various distress and disturbances in their lives, leading to a decrease in QOL.[27]
In Brazil,[4] a study conducted to identify the prevalence of physical, psychological and menopause-related symptoms and their association with minor psychiatric disorders in premenopausal, perimenopausal and postmenopausal women found that fatigue was the most frequent complaint in all groups (61%, 81% and 88% in premenopausal, perimenopausal and postmenopausal women, respectively). Low education level, memory loss, irritability and menopausal transition represent risk factors for positive findings in a screening for minor psychiatric disorders. This is consistent with the current study outcome.
The results of a cross-sectional study conducted through cluster-sampling among 480 postmenopausal women in Iran[28] using MENQOL showed that the menopausal women have worse QOL scores in vasomotor dimension and higher QOL scores in physical dimension. This is confirmative with the current study. A more recent study in Jordan[29] on the severity of menopausal symptoms showed that 15.7%, 66.9% and 17.4% were experiencing severe, moderate and mild menopausal symptoms, respectively. Vasomotor signs were reported to have the highest scores for severity as manifested by hot flushes and night sweating. In addition, women in the perimenopausal period complained more frequently of menopausal symptoms compared to premenopausal and postmenopausal women, except for vasomotor and sexuality symptoms for which postmenopausal women reported higher scores. There was a significant relationship between the severity and occurrence of menopausal symptoms and age, family income, level of education, number of children, perceived health status and menopausal status. This is consistent with the current study in Qatar.
Furthermore, the current study for Cronbach's alpha scores, which is measuring the internal consistency of questions in each domain have shown perfect agreement regarding physical, vasomotor, psychosocial and sexual domains at 0.883, 0.853, 0.697 and 0.805, respectively among Qatari women, which is consistent with the neighboring United Arab Emirates[2] and other developing countries.[2,19,21,22,26,27,28,29,30,31]
Nisar and Sohoo[30] showed that postmenopausal women had significantly higher scores in the physical domain than the menopause transition group, while the scores of the psychological domain were significantly higher in the menopause transition group than in the postmenopausal group and reported vasomotor symptoms in 71% women, psychological symptoms in 96%, and physical and sexual symptoms in 99% and 66%, respectively. These were comparable to our results. A study done by Rahman et al.,[31] showed that the urogenital symptoms were significantly higher in the postmenopausal group as compared to those in the menopause transition group. The psychological symptoms were significantly higher among the perimenopausal women as compared to those among the postmenopausal women.[31] In our study, the vasomotor symptoms and the sexual symptoms were more prominent in the menopause transition group than in the early and late post menopausal groups. But a study from Thailand showed many symptoms to be significantly related to the menopause transition status (such as hot flushes, an upset stomach, insomnia and urinary symptoms) and only night sweats and joint aches and pains were significantly associated with the postmenopausal status.[32] A similar study performed in Kerala[33] showed that the mean age of attaining menopause was 48.26 years and prevalence of symptoms among ladies were emotional problems (crying spells, depression, irritability) 90.7%, headache 72.9%, lethargy 65.4%, dysuria 58.9%, forgetfulness 57%, musculoskeletal problems (joint pain, muscle pain) 53.3%, sexual problems (decreased libido, dyspareunia) 31.8%, genital problems (itching, vaginal dryness) 9.3%, and changes in voice 8.4%. Only 22.4% of women knew the correct cause of menopause. This is confirmative with the current study that all the ladies were suffering from one or more number of menopausal symptoms.
The earlier study reported that the age and symptomatology of natural menopause among Qatari women is consistent with the neighboring United Arab Emirates[2] and other developing countries.[2,19,21,22,26,27,28,29,30,31] However, the present study showed that climacteric symptoms in a postmenopausal woman in Qatar is less compared to her Western counterpart[3,4,5,6,7,8,9,10,17,20] and may be influenced by genetic factors, parity and previous use of oral contraceptives.
Limitations and strengths
There are several limitations of this study. First, there is the potential that women who reported not having hot flashes in the current study may go on to have hot flashes and, thereby, be misclassified in this analysis. Second, the study sample was based on PHC Clinic visits. Third, the majority of the study sample was Arab women and of relatively high socioeconomic and education status; hence, the results are not generalizable to the population of all midlife women. Furthermore, since this is a cross-sectional study, we evaluated the association between factors and QOL. We were unable to evaluate the impact of these factors on change in QOL over time. Despite these limitations, this study had a number of strengths. This study is based on a large representative's sample. The information obtained for the MENQOL was self-reported and may have been affected by personality and social circumstances, yet self-report is an appropriate method to obtain information on perceptions, such as bothersome symptoms. In addition, the MENQOL questionnaire has been validated for use in postmenopausal women and has been used successfully by other studies too.
CONCLUSION
A large number of factors were associated with experiencing menopausal symptoms and these symptoms had negative effects on the QOL among Arabian women. The current study showed that climacteric symptoms in a menopausal woman in Arab is less than Western women, which may be influenced by socio-economic, genetics, environment and parity. Stress management, clinical psychological counseling, and health-promoting practices should be incorporated into menopausal care programs to improve health and QOL of middle-aged women. Health care providers should play a more visible and instrumental role in continuously assessing menopausal women's needs.
ACKNOWLEDGEMENT
This research was supported by the Qatar National Research Fund, National Priorities Research Program 08-467-3-098. The authors would like to thank the Hamad Medical Corporation for their support and ethical approval (HMC RC#8222/08).
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Harlow SD, Gass M, Hall JE, Lobo R, Maki P, Rebar RW, et al. STRAW + 10 Collaborative Group."Executive summary of the Stages of Reproductive Aging Workshop +10: Addressing the unfinished agenda of staging reproductive aging. " J Clin Endocrinol Metab. 2012;97:1159–68. doi: 10.1210/jc.2011-3362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bener A, Rizk DE, Shaheen H, Micallef R, Osman N, Dunn EV. Measurement- specific quality of life satisfaction during menopause in an Arabian Gulf Country. Climacteric. 2000;3:43–9. doi: 10.3109/13697130009167598. [DOI] [PubMed] [Google Scholar]
- 3.North American Menopause, Society. Estrogen and progestogen use in postmenopausal women: 2010 position statement of The North American Menopause Society. Menopause. 2010;17:242–55. doi: 10.1097/gme.0b013e3181d0f6b9. [DOI] [PubMed] [Google Scholar]
- 4.Oppermann K, Fuchs SC, Donato G, Bastos CA, Spritzer PM. Physical, psychological, and menopause-related symptoms and minor psychiatric disorders in a community-based sample of Brazilian premenopausal, perimenopausal, and postmenopausal women. Menopause. 2012;19:355–60. doi: 10.1097/gme.0b013e31822ba026. [DOI] [PubMed] [Google Scholar]
- 5.Nakano K, Pinnow E, Flaws JA, Sorkin JD, Gallicchio L. Reproductive history and hot flashes in perimenopausal women. J Womens Health (Larchmt) 2012;21:433–9. doi: 10.1089/jwh.2011.2999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Avis NE, Crawford SL, McKinlay SM. Psychosocial, behavioral, and health factors related to menopause symptomatology. Womens Health. 1997;3:103–20. [PubMed] [Google Scholar]
- 7.Avis NE, Assmann SF, Kravitz HM, Ganz PA, Ory M. Quality of life in diverse groups of midlife women: Assessing the influence of menopause, health status and psychosocial and demographic factors. Qual Life Res. 2004;13:933–46. doi: 10.1023/B:QURE.0000025582.91310.9f. [DOI] [PubMed] [Google Scholar]
- 8.Nelson HD, Haney E, Humphrey L, Miller J, Nedrow A, Nicolaidis C, Vesco K, Walker M, Bougatsos C, Nygren P. Evidence Report/Technology Assessment No. 120. (Prepared by the Oregon Evidence-based Practice Center, under Contract No. 290-02-0024.) AHRQ Publication No. 05-E016-2. Rockville, MD: Agency for Healthcare Research and Quality; 2005. Mar, Management of Menopause-Related Symptoms. [PMC free article] [PubMed] [Google Scholar]
- 9.Sabia S, Fournier A, Mesrine S, Boutron-Ruault MC, Clavel-Chapelon F. Risk factors for onset of menopausal symptoms: Results from a large cohort study. Maturitas. 2008;60:108–21. doi: 10.1016/j.maturitas.2008.04.004. [DOI] [PubMed] [Google Scholar]
- 10.Iddenden D. Sexuality during the menopause in the menopausal women. Med Clin N Am. 1987;71:87–93. doi: 10.1016/s0025-7125(16)30884-7. [DOI] [PubMed] [Google Scholar]
- 11.Schmidt J, Landin-Wilhelmsen K, Brännström M, Dahlgren E. Cardiovascular disease and risk factors in PCOS women of postmenopausal age: A 21-year controlled follow-up study. J Clin Endocrinol Metab. 2011;96:3794–803. doi: 10.1210/jc.2011-1677. [DOI] [PubMed] [Google Scholar]
- 12.Munir JA, Wu H, Bauer K, Bindeman J, Byrd C, Feuerstein IM, et al. The perimenopausal atherosclerosis transition: Relationships between calcified and noncalcified coronary, aortic, and carotid atherosclerosis and risk factors and hormone levels. Menopause. 2012;19:10–5. doi: 10.1097/gme.0b013e318221bc8d. [DOI] [PubMed] [Google Scholar]
- 13.Chedraui P, San Miguel G, Avila C. Quality of life impairment during the female menopausal transition is related to personal and partner factors. Gynecol Endocrinol. 2009;25:130–5. doi: 10.1080/09513590802617770. [DOI] [PubMed] [Google Scholar]
- 14.Bosworth HB, Bastian LA, Kuchibhatla MN, Steffens DC, McBride CM, Skinner CS, et al. Depressive symptoms, menopausal status and climacteric symptoms in women at midlife. Psychosom Med. 2001;63:603–8. doi: 10.1097/00006842-200107000-00013. [DOI] [PubMed] [Google Scholar]
- 15.Vandenakker CB, Glass DD. Menopause and aging with disability. Phys Med Rehabil Clin N Am. 2001;12:133–51. [PubMed] [Google Scholar]
- 16.Zollner YF, Acquadro C, Schaefer M. Literature review of instruments to assess health-related quality of life during and after menopause. Qual Life Res. 2005;14:309–27. doi: 10.1007/s11136-004-0688-z. [DOI] [PubMed] [Google Scholar]
- 17.Hilditch JR, Lewis J, Peter A, Maris BV, Ross A, Franssen E, et al. A menopause-specific quality of life questionnaire: Development and psychometric properties. Maturitas. 1996;24:161–75. doi: 10.1016/s0378-5122(96)82006-8. [DOI] [PubMed] [Google Scholar]
- 18.Orley J, Kuyken W. Preface. In: Orley J, Kuyken W, editors. Quality of life assessment: international perspectives. Berlin: Springer-Verlag; 1994. [Google Scholar]
- 19.Bener A, Rizk DE, Ezimokhai M, Hassan M, Micallef R, Sawaya M. Consangunity and the age of menopause in the United Arab Emirates. Int J Gynaecol Obstet. 1998;60:155–60. doi: 10.1016/s0020-7292(97)00250-6. [DOI] [PubMed] [Google Scholar]
- 20.Williams RE, Levine KB, Kalilani L, Lewis J, Clark RV. Menopause-specific questionnaire assessment in US population-based study shows negative impact on health-related quality of life. Maturitas. 2009;62:153–9. doi: 10.1016/j.maturitas.2008.12.006. [DOI] [PubMed] [Google Scholar]
- 21.Chen Y, Lin SQ, Wei Y, Gao HL, Wang SH, Wu ZL. Impact of menopause on quality of life in community-based women in China. Menopause. 2008;15:144–9. doi: 10.1097/gme.0b013e318115150e. [DOI] [PubMed] [Google Scholar]
- 22.Karaçam Z, Seker SE. Factors associated with menopausal symptoms and their relationship with the quality of life among Turkish women. Maturitas. 2007;58:75–82. doi: 10.1016/j.maturitas.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 23.Chaikittisilpa S, Limpaphayom K, Chompootweep S, Taechakraichana N. Symptoms and problems of menopausal women in Klong Toey slum. J Med Assoc Thai. 1997;80:257–61. [PubMed] [Google Scholar]
- 24.Nedstrand E, Perrl J, Hammar M. Climacteric symptoms in a postmenopausal Czech population. Maturitas. 1996;23:85–9. doi: 10.1016/0378-5122(95)00965-5. [DOI] [PubMed] [Google Scholar]
- 25.Berg JA, Taylor DL. Symptoms experience of Filipino American midlife women. Menopause. 1999;6:105–14. [PubMed] [Google Scholar]
- 26.Poomalar GK, Arounassalame B. The quality of life during and after menopause among rural women. J Clin Diagn Res. 2013;7:135–9. doi: 10.7860/JCDR/2012/4910.2688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Whelan TJ, Goss PE, Ingle JN, Pater JL, Tu DS, Pritchard K, et al. Assessment of quality of life in MA.17: A randomized, placebo controlled trial of letrozole after 5 years of tamoxifen in postmenopausal women. J Clin Oncol. 2005;23:6931–40. doi: 10.1200/JCO.2005.11.181. [DOI] [PubMed] [Google Scholar]
- 28.Fallahzadeh H. Quality of life after the menopause in Iran: A population study. Qual Life Res. 2010;19:813–9. doi: 10.1007/s11136-010-9644-2. [DOI] [PubMed] [Google Scholar]
- 29.Gharaibeh M, Al-Obeisat S, Hattab J. Severity of menopausal symptoms of Jordanian women. Climacteric. 2010;13:385–94. doi: 10.3109/13697130903050009. [DOI] [PubMed] [Google Scholar]
- 30.Nisar N, Sohoo NA. Frequency of menopausal symptoms and their impact on the quality of life of women: A hospital based survey. J Pak Med Assoc. 2009;59:752–6. [PubMed] [Google Scholar]
- 31.Rahman SA, Zainudin SR, Mun VL. Assessment of menopausal symptoms using modified Menopause Rating Scale (MRS) among middle age women in Kuching, Sarawak, Malaysia. Asia Pac Fam Med. 2010;9:5. doi: 10.1186/1447-056X-9-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Punyahotra S, Dennerstein L, lehert P. Menopausal experiences of Thai women. Maturitas. 1997;26:1–7. doi: 10.1016/s0378-5122(96)01058-4. [DOI] [PubMed] [Google Scholar]
- 33.Borker SA, Venugopalan PP, Bhat SN. Study of menopausal symptoms, and perceptions about menopause among women at a rural community in Kerala. J Midlife Health. 2013;4:182–7. doi: 10.4103/0976-7800.118997. [DOI] [PMC free article] [PubMed] [Google Scholar]


