Abstract
Aim:
We are using multimodal technique to improve hand hygiene (HH) compliance among all health care staff for the past 1-year. This cross-sectional observational study was conducted in the surgical ICU to assess adherence to HH among nurses and allied healthcare workers, at the end of the training year.
Materials and Methods:
This was a cross-sectional observational study using direct observation technique. A single observer collected all HH data. During this analysis, 1500 HH opportunities were observed. HH compliance was tested for all 5 moments as per WHO guidelines.
Results:
Overall compliance as per WHO Guidelines was 78%. Nurses had an adherence rate of 63%; allied staff adherence was 86.5%. Compliance was 93% after patient contact versus 63% before patient contact. Nurses'compliance before aseptic procedures was lowest at 39%. 92% staff was aware of the facts viz. Diseases prevented by hand washing, ideal duration of HH, reduction of health care associated infections, etc.
Conclusion:
After 1-year of aggressive multimodal intervention in improving HH compliance, we have an overall compliance of 78%. It implies that sustained performance and compliance to HH can be ensured by ongoing training. Direct observation remains a widely used, easily reproducible method for monitoring compliance.
Keywords: 5 moments, compliance, hand hygiene
Introduction
Institution drove hand hygiene (HH) started in our hospital in January 2013. There is no prior data on compliance. Since 1-year, we have arranged regular training courses for all healthcare workers. Training includes practical demonstration and practice of the technique of HH. It is augmented by placement of posters in all strategic places and availability of alcohol based hand rub gels at bedside. The training program is based on WHO recommendation.[1] This study examines the effectiveness of training in our hospital.
Health care associated infections (HAI) affect 1 in 20 hospitalized patients.[2] Patients in the ICUs are more likely to be colonized or infected by multi-drug resistant organisms. Most of these infections are spread via health care workers' hands. HH is the single most effective measure to prevent this spread. Despite its relative simplicity, HH compliance rates vary and may still be very poor.[1]
We used direct observation method for WHO's five moments of HH as it is still considered the gold standard.[1] It provides quantitative and qualitative information about when and why failures in HH occur, and minimizes any change in behavior of the staff members.[4]
Materials and Methods
Our hospital is a tertiary level multispecialty hospital. ICU is divided into four subunits with combined 3000 admissions yearly. ICU's have conveniently located hand washing facilities and availability of alcohol-based hand rub gels with each bed. This single observer study was conducted in the 10 bedded surgical and trauma subunit.
A survey was done, prior to the study, by filling a pretested close ended validated questionnaire. The questionnaire was pertaining to intentions of adherence to HH, perception and knowledge, opportunities, steps, actions and attitude toward HH [Appendix 1].
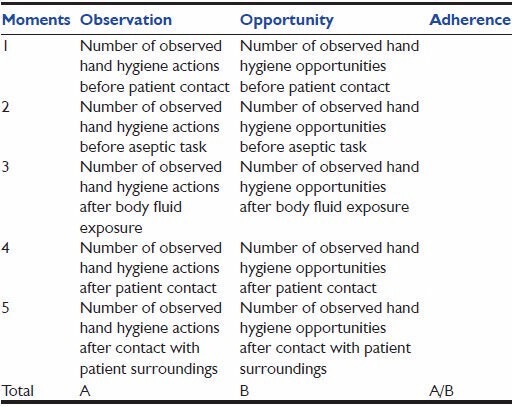
The nursing staff (n = 28) and allied healthcare workers (n = 10) was taken as a sample size. All the staff had undergone an orientation and training program in HH practices as per WHO guidelines. The observer recorded all possible opportunities for HH in the ICU for a period of 10 days. Direct observation involved observing 150 opportunities per day. A single observer visited the ICU over a period of 12 h each time, till 1500 observations were completed. The observations were noted for all five moments of HH before and after patient contact. A separate checklist was used for nursing and allied staff. If an indication for HH was noted, a tick was placed on the checklist next to the relevant guideline, under the column “indication”. If HH occurred, another tick was inserted in the column “occurred.” If it did not occur, no insertion was made. The procedure was followed for 10 days, and averages were taken to calculate the adherence rate, as in Table 1.
Table 1.
Adherence to hand washing was assessed using direct observation and survey. WHO's 5 Moments of hand hygiene opportunities was surveyed
Results
During the 10 days data collection in the ICU, 1500 HH opportunities were observed. Among 38 healthcare workers, 28 were nurses (73.6%), and 10 (26.3%) other healthcare workers (technicians, physiotherapists) [Table 1].
Table 2 gives the HH opportunities as per healthcare workers.
Table 2.
Overview of hand hygiene opportunities
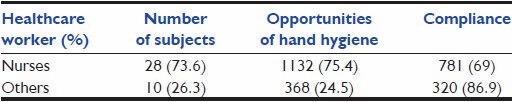
Table 3 gives the observed compliance for nurses as per WHO'S 5 moments.
Table 3.
Observed compliance for nurses
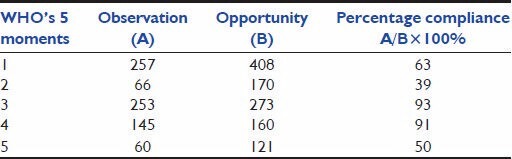
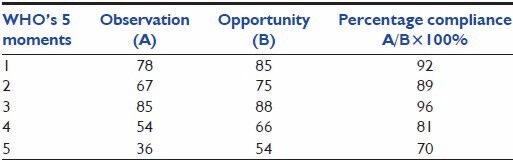
Table 4 gives the observed compliance for allied staff as per WHO'S 5 moments.
Table 4.
Observed compliance for allied staff
A single observer underwent an orientation about the correct method of HH procedure by our infection control nurses. He did a preliminary run on observing adherence with the infection control nurse and results were compared. This reduced inter-observer variation and guaranteed uniformity of data collection. He stayed in the ICU for 12 h every day. Data were collected over 12 h shifts, between 8 am and 8 pm for 6 shifts and 8 pm to the next morning 8 am for 4 shifts. The healthcare staff was not aware of this data collection since the observer was part of the team of junior doctors working in the ICU.
Out of the total opportunities, nurses had the highest number of contacts (75.4%), followed by allied healthcare workers (24.5%). The average compliance was about 78%, which differed significantly among healthcare workers, with higher compliance among the allied staff (86.9%) followed by nurses (69%). Out of the average overall compliance of 78%, maximum compliance was seen for moment 3, that is, the staff were very careful after body fluid contact as it was perceived important for self-protection. The HH instances after patient contact (91%) also suggested similarly. The nurses' compliance was 63% before patient contact and 50% after touching surroundings. The allied staff did better with a fairly equal distribution across all moments. The HH compliance for moment 5 that is, after touching patient surroundings, was poor across all staff. We noted no difference in compliance rates between day and night times. However, compliance fell when the ICU was busy especially during acute resuscitation settings or if multiple admissions occurred simultaneously.
Analysis of the survey showed that 92% of the healthcare staff was aware of HH facts viz. Diseases prevented by HH, type of dirt tackled by hand washing, ideal duration of HH and the extent of reduction of HAI. Reasons for nonadherence emerged as unavailability of hand rub at the clinical area, workload pressure and nurse shortages.
Discussion
The nurses had an overall compliance of 69% that is comparable to most other studies.[4,5,6,7] They fared best for WHO moment 3 and 4 that is, after body fluid exposure risk and patient contact with compliance of 93% and 91% respectively. This reflects an urge to protect oneself. They fared the worst for WHO moment 2 that is, before aseptic procedure (39%). We found that most nurses clubbed moment 1 and 2 together and would not additionally perform HH before suctioning or doing any other clean procedure.
In a study by Marra et al.,[5] comparing the observational method, product use method and electronic surveillance, the overall rate of HH adherence was found to be 62.3% (there were 2,249 opportunities for HH observed, and representing 1,402 cleansing episodes). However, they did not collect data for individual moments.
The allied staff fared better overall with a compliance of 86.9%. All opportunities for allied staff were observed during daytime, and most of the patient contact was elective and planned. This could be one reason why they did better at HH adherence. In a study by Randle et al.,[7] a 24 h observational study, it was found that out of the total of 823 HH opportunities (health care workers, n = 659; patient and visitors, n = 164;) compliance was 47% for doctors, 75% for nurses, 78% for allied health professionals, and 59% for ancillary and other staff.(P < 0.001).
Similarly, in a multi-center study in Poland, 95.6% hospitals had a written protocol for hand washing procedures, but according to the findings of the study, the compliance rates varied from 20% to 80%, although in most institutions it was between 40% and 60%.[6]
We are using multimodal techniques to impart training and improve HH compliance rates since January 2013. We have an induction course for all new recruits, monthly educational sessions, posters at strategic locations, ample supply of alcohol-based hand rubs placed bedside. In a study by Mathai et al.,[8] probably the first published Indian article on multimodal interventions, they have emphasized the importance of multimodal technique in improving HH compliance. They saw a large and significant difference pre and postmultimodal interventions. In another study by Lam et al.,[9] they found that multimodal interventions like educational sessions, posters, performance feedback, and verbal reminders have improved their HH rates.
There is no standard for measuring adherence to HH. Directly observing adherence to HH is the method used in most studies.[3,10,11] WHO guidelines recommend the use of direct observation for monitoring HH compliance. It provides qualitative and quantitative information about why and when failures occur.[1,4] There are recent studies that doubt the efficiency of direct observation methods. Marra et al.[5] in their study stated that the direct observation may not be a gold standard as they found no correlation between observed HH adherence and mean product usage. They preferred electronic counting devices as it recorded opportunities most accurately and could do it over extended periods of time. Both studies, Marra et al.[5] and Randle et al.[7] mention the overall compliance but fail to comment on individual moments. In our study, we found that moment 2 fared the worst in terms of HH adherence. Soon after the study was over, corrective training was done to address this.
In our hospital, we do not have either electronic product dispensers or the technology to visually record HH observations.
Direct observations have limitations; they are time-consuming, manpower intensive, do not allow continuous monitoring. They probably provide information about a very low percentage of all HH opportunities. If staff is aware, direct observation may affect health care workers behavior (Hawthorne effect).[11] We have tried to limit these difficulties by engaging a single trained observer. However, there could be opportunities that were missed. We also made sure that none of the staff involved in the study was aware of the observer as data was collected during his duty rotation. None of the staff was given performance feedback during the study period. The questionnaire was filled before the study period started as part of regular feedback on training.
Conclusion
The average level of compliance with recommended HH techniques among healthcare workers was 78%, which is below the benchmark of 90% for critical care areas. Direct observation is still superior as it can determine compliance with all 5 moments of HH. It can also evaluate HH technique and can check compliance rates according to the healthcare workers.[4] In India, where technology to monitor adherence may not be available, direct observation remains the gold standard.
Easy access and adequate supply of hand rub solutions, presurvey orientation program; preemployment training does not ensure adequate compliance with HH. Continuous training, performance feedback and verbal reminders will be needed to sustain adherence to HH.
Appendix 1: HAND HYGIENE KNOWLEDGE QUESTIONNAIRE
Name ___________________
Staff ID _________________________
Date ____________________________
Dept. ____________________________
1. The most common cause of infections in the hospital is:
Blood pressure cuffs
Computer keyboards
Theatre trolleys
Poor hand hygiene
2. Hand hygiene refers to:
Hand washing using skin cleanser
Hand washing using alcohol hand rub
Decontaminating using 4% chlorhexidine
All the above
3. The advantage of using alcohol hand rubs:
It is self drying
It is more accessible than sinks
It is faster to use than traditional methods
All the above
4. Why is it beneficial to have both alcohol and chlorhexidine in alcohol hand rubs?
Together they prevent your hands from drying
Alcohol is only effective in killing bugs when mixed with chlorhexidine
Alcohol kills bugs rapidly and chlorhexidine provides a longer effect
Together they extend product shelf life
5. The shortest time required to disinfect hands effectively with alcohol hand rubs is:
5 seconds
10 seconds
15 seconds
60 seconds
6. What is the most frequent source of germs responsible for health care-associated infections?
The hospital's water system
The hospital air
Germs already present on or within the patient
The hospital environment (surfaces)
7. Which of the following hand hygiene actions prevents transmission of germs to the patient?
Before touching a patient
Immediately after a risk of body fluid exposure
After exposure to the immediate surroundings of a patient
Immediately before a clean/aseptic procedure
8. Which of the following hand hygiene actions prevents transmission of germs to the health-care worker?
After touching a patient
Immediately after a risk of body fluid exposure
Immediately before a clean/aseptic procedure
After exposure to the immediate surroundings of a patient
9. Which of the following statements on alcohol-based handrub and handwashing with soap and water are true?
Handrubbing is more rapid for hand cleansing than handwashing
Handrubbing causes skin dryness more than handwashing
Handrubbing is more effective against germs than handwashing
Handwashing and handrubbing are recommended to be performed in
10. Which type of hand hygiene method is required in the following situations?
-
Before palpation of the abdomen
◻ Rubbing ◻ Washing ◻ None
-
Before giving an injection
◻ Rubbing ◻ Washing ◻ None
-
After emptying a bedpan
◻ Rubbing ◻ Washing ◻ None
-
After removing examination gloves
◻ Rubbing ◻ Washing ◻ None
-
After making a patient's bed
◻ Rubbing ◻ Washing ◻ None
-
After visible exposure to blood
◻ Rubbing ◻ Washing ◻ None
11. Which of the following should be avoided, as associated with increased likelihood of colonisation of hands with harmful germs?
Wearing jewellery
Damaged skin
Artificial fingernails
Regular use of a hand cream
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.WHO Guidelines on Hand Hygiene in Health Care, 2009. 2014. Sep 11th, Available from: http://www.whqlibdoc.who.int/publications/2009/9789241597906_eng.pdf .
- 2.CDC-Public Health Reports. Estimating Health Care Associated Infections and Deaths in US Hospitals. 2007 Mar-Apr; doi: 10.1177/003335490712200205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mathai E, Allegranzi B, Kilpatrick C, Pittet D. Prevention and control of health care-associated infections through improved hand hygiene. Indian J Med Microbiol. 2010;28:100–6. doi: 10.4103/0255-0857.62483. [DOI] [PubMed] [Google Scholar]
- 4.Stewardson A, Pittet D. Quicker, easier, and cheaper. The promise of automated hand hygiene monitoring? Infect Control Hosp Epidemiol. 2011;32:1029–31. doi: 10.1086/662023. [DOI] [PubMed] [Google Scholar]
- 5.Marra AR, Moura DF, Jr, Paes AT, dos Santos OF, Edmond MB. Measuring rates of hand hygiene adherence in the intensive care setting: A comparative study of direct observation, product usage, and electronic counting devices. Infect Control Hosp Epidemiol. 2010;31:796–801. doi: 10.1086/653999. [DOI] [PubMed] [Google Scholar]
- 6.Heczko PB, Kleszcz P. Handwashing practices in Polish hospitals: Results of a survey conducted by Polish Society of Hospital Infection. J Hosp Infect. 2001;48(Suppl A):S47–9. doi: 10.1016/s0195-6701(01)90013-1. [DOI] [PubMed] [Google Scholar]
- 7.Randle J, Arthur A, Vaughan N. Twenty-four-hour observational study of hospital hand hygiene compliance. J Hosp Infect. 2010;76:252–5. doi: 10.1016/j.jhin.2010.06.027. [DOI] [PubMed] [Google Scholar]
- 8.Mathai AS, George SE, Abraham J. Efficacy of a multimodal intervention strategy in improving hand hygiene compliance in a tertiary level intensive care unit. Indian J Crit Care Med. 2011;15:6–15. doi: 10.4103/0972-5229.78215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lam BC, Lee J, Lau YL. Hand hygiene practices in a neonatal intensive care unit: A multimodal intervention and impact on nosocomial infection. Pediatrics. 2004;114:e565–71. doi: 10.1542/peds.2004-1107. [DOI] [PubMed] [Google Scholar]
- 10.Rupp ME, Fitzgerald T, Puumala S, Anderson JR, Craig R, Iwen PC, et al. Prospective, controlled, cross-over trial of alcohol-based hand gel in critical care units. Infect Control Hosp Epidemiol. 2008;29:8–15. doi: 10.1086/524333. [DOI] [PubMed] [Google Scholar]
- 11.Kohli E, Ptak J, Smith R, Taylor E, Talbot EA, Kirkland KB. Variability in the Hawthorne effect with regard to hand hygiene performance in high- and low-performing inpatient care units. Infect Control Hosp Epidemiol. 2009;30:222–5. doi: 10.1086/595692. [DOI] [PubMed] [Google Scholar]


