Abstract
Pulmonary haemorrhage is an uncommon symptom in paediatrics with the etiology varying among the series by age, location, and the diagnostic tests employed. Once airway protection and volume resuscitation are ensured, localization of the anatomic site of bleeding, isolation of the involved airway, control of haemorrhage and treatment of the underlying cause of becomes essential. In localized persistent bleeding, airway control may be achieved by lung isolation with double lumen endotracheal tube and synchronous independent lung ventilation
Keywords: Pulmonary haemorrhage, Independent lung ventilation, Double lumen endotracheal tube
Introduction
Pulmonary hemorrhage is a common symptom with many potential causes. Massive pulmonary hemorrhage accounts for 5% of the total, requiring intensive care admission[1] with 30-50% mortality rates. We represent a pediatric case of the massive pulmonary bleed illustrating the use of independent lung ventilation (ILV) rare in pediatrics, albeit an established practice in adult medicine.
Case Report
An 8-year-old male child presented to us with a history of multiple bouts of massive hemoptysis and increasing dyspnea of 3-day duration. He had undergone bidirectional Glenn shunt at the age of 8 months for tricuspid atresia. He had an uneventful course till the present presentation. He was intubated and was mechanically ventilated in view of severe respiratory distress. His hemodynamics was supported with inotropes, and broad spectrum antibiotics were started. Initial workup showed normal blood counts with normal platelet count. Chest X-ray showed multiple heterogeneous opacities in right lung suggestive of hemorrhage [Figure 1]. In view of massive bleed from airway that was not controlled with positive pressure ventilation, he was taken up for an emergency angiography and collateral of 2.5 mm arising from left subclavian artery was occluded by coil embolization; following which there was temporary cessation of bleeding. However the next day, there was recurrence massive bleed from endobronchial tube. This time he underwent bronchoscopy that showed friable mucosa of right main bronchus and also computed tomography (CT) thorax [Figure 2] which showed multiple tiny collaterals arising from the aorta that could not be embolized. Decision of bronchial artery embolization was deferred because of deteriorating general condition with recurrent bleeds.
Figure 1.
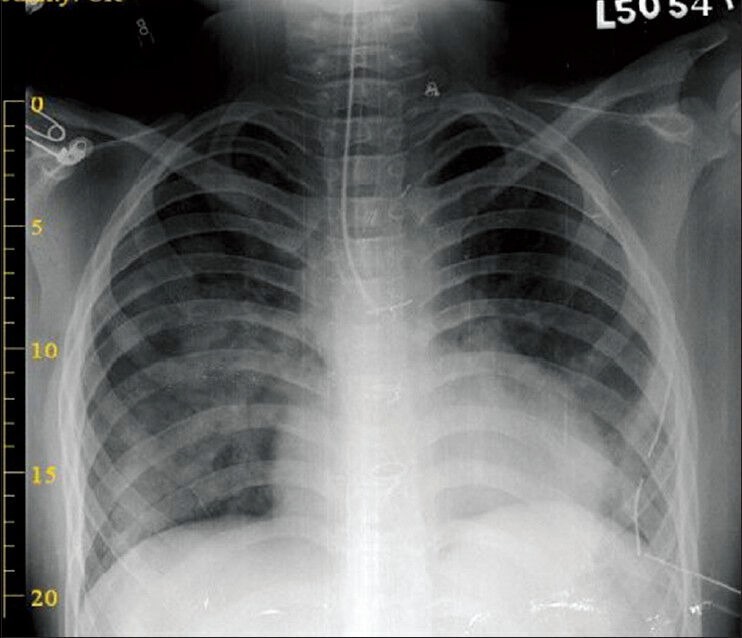
Chest X-ray showing double-lumen tube in situ with improved right lung aeration
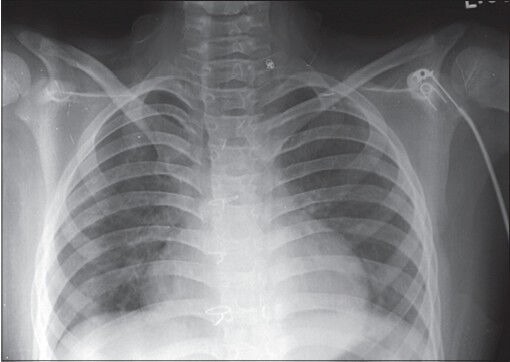
Figure 2.

Computed tomography chest showing pulmonary hemorrhage in right upper lobe
In view of recurrent bleeding and inability to maintain optimum saturations, left side double-lumen endotracheal tube was inserted under bronchoscopic guidance. ILV was initiated by two separate ventilators. Right lung (bleeding) was put on the pressure controlled ventilation and left lung relatively normal, was managed with volume controlled ventilation. Both ventilators were time cycled with same settings and effort was made for maximum synchronization. With complete isolation of bleeding right lung from the left side and effective toileting of the right bronchus, bleeding gradually came down. The child was put back to a single conventional ventilator after 4 days and was extubated subsequently 2 days later, after confirming complete cessation of bleeding by bronchoscopy. The child was observed inward for few days and in the absence of any recurrence of bleeding, he was discharged in healthy condition [Figure 3]. There was no history suggestive of the pulmonary bleed during follow up visits.
Figure 3.
Chest X-ray showing relatively normal lung fields at the time of discharge
Discussion
Massive hemoptysis is defined as bleed of more than 8 mL/kg every 24 h or 200 mL every 24 h from respiratory tract.[2] Esterly and Oppenheimer[3] have characterized massive pulmonary hemorrhage in newborn as the involvement of at least two pulmonary lobes by confluent foci of extravasated erythrocytes. From a clinical point of view, hemoptysis that jeopardizes respiratory function and/or causing hemodynamic instability should be treated as a medical emergency. Our patient satisfied both quantitative and clinical criteria mentioned in definition.
A careful history and clinical examination should be performed in order to rule out nonpulmonary causes of bleeding. A major cause of the pulmonary bleed has been given in Table 1. Chest radiography can identify the site of bleeding in 33-82% of cases of massive hemoptysis,[4] and may reveal the underlying cause (35%). CT scan is much more efficient than bronchoscopy for determining the cause of bleeding (60-77% vs. 2.5-8%).[5] Moreover, by showing possible extra pulmonary causes of hemoptysis, CT scan can obviate the need for bronchial arteriography. Fiber optic bronchoscopy identifies the site of bleeding in 73-93% of episodes of massive bleeding.
Management
General measures
General care measures include maintaining the airway, oxygen supplementation, systemic hemostasis therapy and putting the patient in Trendelenburg position as tolerated to assist clots to propagate superiorly and exit the airway.[5] Following airway control, mechanical ventilation with positive end-expiratory pressure (PEEP) helps to reverse the hypoxemia and provide a measure of tamponade to the site of hemorrhage.
Control of bleeding
Multiple approaches have been described such as Tamponade, (Either the bronchial balloon of a Double-Lumen Tube), cold saline lavage use of Adrenaline or other vasoconstrictors, Topical coagulants (Thrombin and fibrinogen concentrates), laser, diathermy or cryocautery.[1]
Bronchoscopy might be useful as a complementary tool for optimal inspection of the upper lobes and peripheral airways allowing better suction of blood clots and secretions through its large working channel, and improved visualization of the airways.[6]
Lung isolation/independent lung ventilation
In localized persistent bleeding, airway control may be achieved by insertion of a double-lumen endotracheal tube to isolate and ventilate the lungs separately. Left sided tubes are preferable, as occlusion of the right main bronchus is difficult to avoid in an emergency situation.
Synchronous independent lung ventilation
In synchronous ILV, the respiratory rate of both lungs is kept identical. However, the respiratory cycle can either be in phase or 180° out of phase. Selective PEEP can also be added to either lung. The tidal volumes and inspiratory flow rates are set independently. Synchronous ILV can be instituted using either a two ventilator or a single ventilator system. One-ventilator system employs a Y-piece with separate PEEP valves. The airflow and tidal volume to each lung are then determined by the individual lung compliance and airway resistance. They offer the added advantage of permitting bronchial toilet and limited bronchoscopic therapy. We synchronized by keeping similar rates and similar time settings. Although most intensive care units use ILV in fewer than one in 1000 patients requiring mechanical ventilation, it can be a lifesaving measure in specific conditions, making maintenance of suitable equipment and knowledge of its use required[7,8].
Surgery
When all measures fail to control hemoptysis, surgical management should be considered. Segmentectomy or lobectomy is preferred to pneumonectomy as the latter carries a much higher mortality rate.
Conclusion
Intensive care with conservative treatment can stop bleeding in about majority of patients. In cases of continuous bleeding, ILV should be considered even in pediatric population. Placing a double-lumen tube with ILV is an effective modality in the management of unilateral lung bleeds which in itself is a temporizing measure allowing time to identify and to treat the underlying cause definitively. The usage of ILV need to be initiated early during the disease course. There is a need for more pediatric studies and experience on long term outcome and development of evidence based treatment regimes.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Angela T, Gerry L. Management of massive hemoptysis [internet] 2011. [updated 2011 May 30;cited 2014 July 12]. Available from http://http://www.frca.co.uk/Documents/225%20Massive%20Haemoptysis.pdf .
- 2.Gaude GS. Hemoptysis in children. Indian Pediatr. 2010;47:245–54. doi: 10.1007/s13312-010-0044-z. [DOI] [PubMed] [Google Scholar]
- 3.Esterly JR, Oppenheimer EH. Massive pulmonary hemorrhage in the newborn. I. Pathologic considerations. J Pediatr. 1966;69:3–11. doi: 10.1016/s0022-3476(66)80354-2. [DOI] [PubMed] [Google Scholar]
- 4.Hirshberg B, Biran I, Glazer M, Kramer MR. Hemoptysis: Etiology, evaluation, and outcome in a tertiary referral hospital. Chest. 1997;112:440–4. doi: 10.1378/chest.112.2.440. [DOI] [PubMed] [Google Scholar]
- 5.Wong TW. Children with life threatening pulmonary hemorrhage. J Paediatr Respirol Crit Care. 2012;8:1. [Google Scholar]
- 6.Lordan JL, Gascoigne A, Corris PA. The pulmonary physician in critical care illustrative case 7: Assessment and management of massive haemoptysis. Thorax. 2003;58:814–9. doi: 10.1136/thorax.58.9.814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tobin MJ. Principles and Practice of Mechanical Ventilation. 3rd ed. NewYork: McGraw Hill; 2013. pp. 629–654. Chapter 25, Independent lung ventilation. [Google Scholar]
- 8.Charan NB, Carvalho CG, Hawk P, Crowley JJ, Carvalho P. Independent lung ventilation with a single ventilator using a variable resistance valve. Chest. 1995;107:256–60. doi: 10.1378/chest.107.1.256. [DOI] [PubMed] [Google Scholar]


