Abstract
We present the case of an 82-year-old woman undergoing high-risk chronic total occlusion percutaneous coronary intervention (CTO-PCI) of the right coronary artery. Hours after the procedure, a subepicardial haematoma was diagnosed as a result of coronary perforation during the procedure. This rare and potentially lethal complication evolved exceptionally benignly after conservative management; our patient fully recovered. Increasingly complex procedures in high-risk patient categories warrant awareness of procedural complications, especially those that are subtle and appear relatively late, and are therefore most hazardous. Recognition of this rare complication and choosing the optimal strategy is of the utmost importance when dealing with patients who undergo PCI. We here describe the rare case of a potential lethal complication in high-risk CTO-PCI, which evolved relatively benignly.
Background
Chronic total occlusions (CTOs) are encountered in approximately 20% of patients referred for coronary angiography.1 When performing percutaneous coronary intervention (PCI), incomplete revascularisation is associated with an adverse impact on long-term mortality.2 Therefore, recanalisation of a CTO is worthwhile; with improving success rates and long-term stentpatency, CTO-PCI has become a default strategy in percutaneous revascularisation.
Despite increasing procedural success rates due to technological advances and improved operator skills, the CTO-PCI procedure has a greater incidence of procedural complications—including coronary perforation—compared to PCI of non-CTO lesions. This occurrence of perforation is strongly associated with an increase in mortality.3
Case presentation
An 82-year-old woman with progressive angina was referred to our hospital for CTO-PCI of the proximal right coronary artery (RCA). She had a history of multiple PCI's in the left coronary artery (LCA) and was on dual antiplatelet therapy on admission.
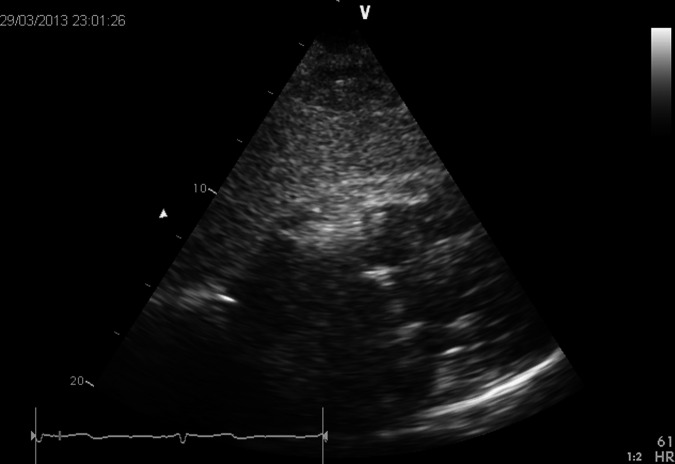
After introducing a 7 Fr sheath in the left femoral artery, an antegrade approach of the occluded RCA was performed, with collateral injections for retrograde visualisation using a 6 Fr sheath in the right radial artery. The CTO was engaged with support of a microcatheter, resulting in a subintimal position of the wires distally of the occlusion. With the use of the parallel wire technique, intraluminal position was obtained. Subsequently, predilation, implantation of two drug-eluting stents was performed from mid to proximal RCA (Orsiro 3.0×30 mm and 3.5×30 mm Biotronik), and postdilation was performed with Thrombolysis in Myocardial Infarction (TIMI) 3 flow as the final result (figure 1).
Figure 1.
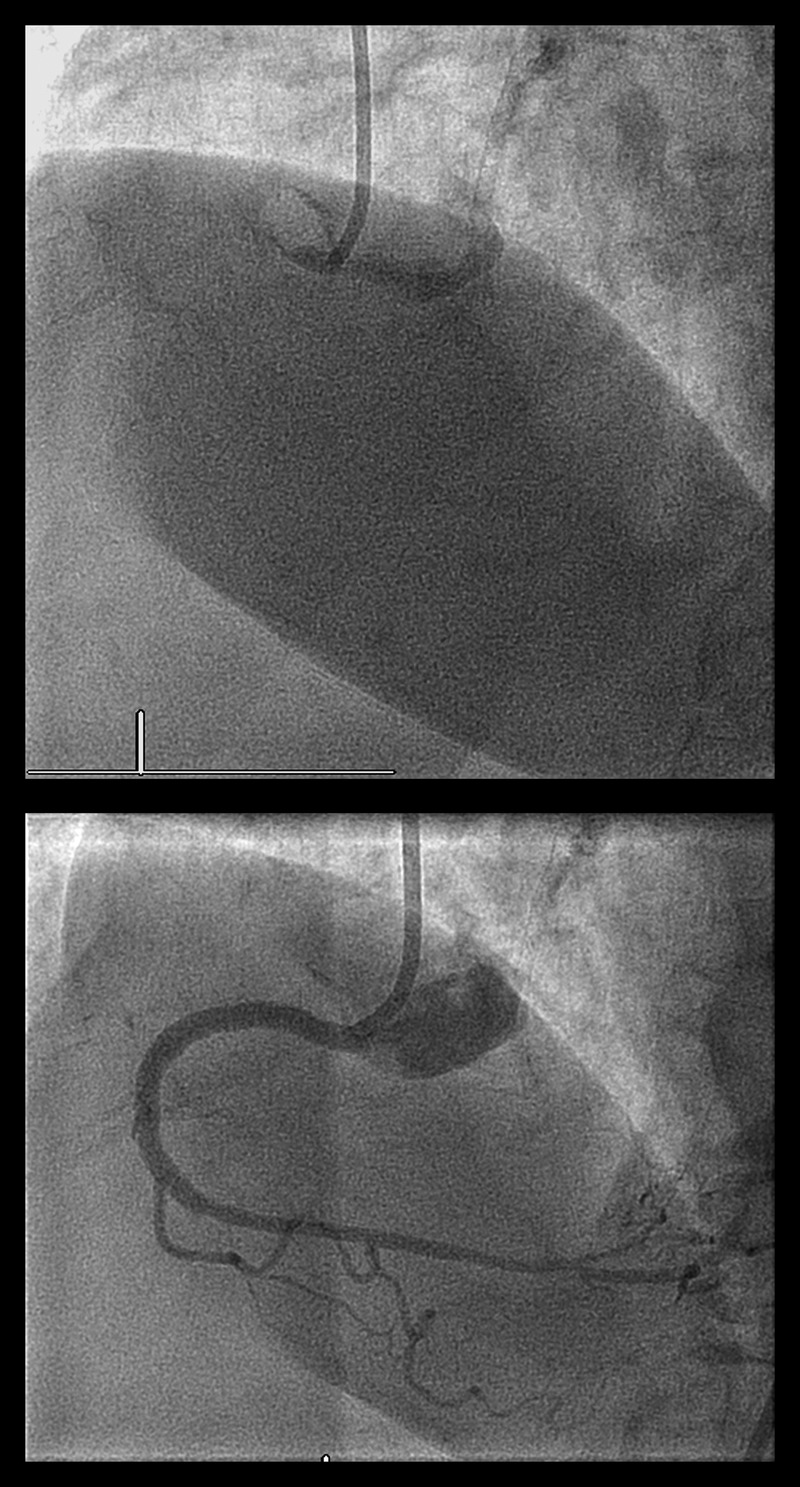
Chronic total occlusion (CTO) of the proximal right coronary artery and the final result after CTO-percutaneous coronary intervention.
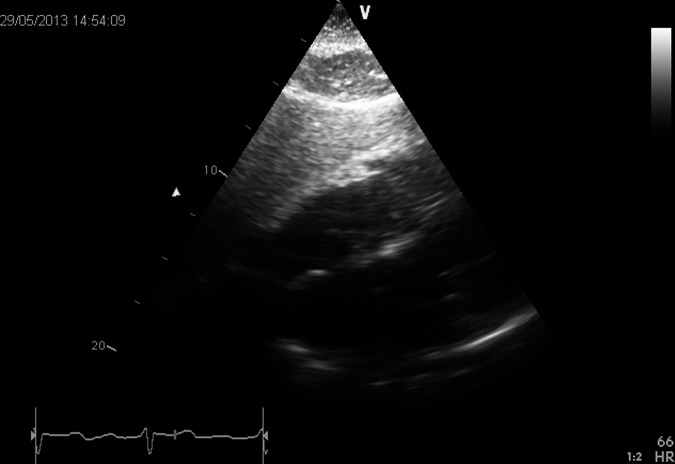
During the procedure, the patient complained of mild chest pain. The ECG showed no abnormalities, blood pressure was in the upper limits of normal and stable. During observation after the procedure, the patient became hypotensive. Further physical examination revealed no abnormalities. An ultrasound was performed, which revealed an echo-dense mass adjacent to the right atrioventricular sulcus, compressing the right ventricular wall with moderate inflow obstruction (figure 2). The patient responded well to administration of saline intravenously and her blood pressure normalised. The chest pain diminished and she became asymptomatic within hours.
Figure 2.
Subepicardial haematoma adjacent to the right atrioventricular sulcus.
Outcome and follow-up
Echocardiographic follow-up the next day showed a reduction of the size of the haematoma, as well as improvement of right ventricular expansion and normalisation of inflow. After a few days, she was dismissed in excellent condition after an uneventful recovery.
Another ultrasound was performed after 2 months, which showed full resolvement of the haematoma and normal left and right ventricular function (figure 3).
Figure 3.
Reduction of haematoma after 2 months, normalisation of right ventricular inflow.
In retrospect, a small amount of contrast extravasation was visible after predilation, distally from the CTO and implanted stents. This extravasation was not visible any more in the final angiogram.
Discussion
The treatment of severe coronary artery disease is constantly evolving, and recanalisation of CTO lesions has often been called ‘the final frontier’ in interventional cardiology. Coronary perforation is a rare complication of PCI (incidence reported <1%),4 but potentially life-threatening with mortality ranging from 7% to 19%.3–4 A number of independent risk factors have been identified which predispose for coronary perforation. Besides treatment of CTO lesions, these factors include female gender, increasing age, calcified lesions and use of cutting balloons and rotational atherectomy.3 The Ellis angiographical classification of coronary perforation is used to grade the severity of perforations and has been shown to be a strong predictor of outcome (table 1).5 Class III perforations often require surgery or pericardiocentesis and are strongly associated with high mortality rates.
Table 1.
Ellis’ perforation classification
| Type I | Extraluminal crater without extravasation |
| Type II | Pericardial or myocardial blush without contrast jet extravasation |
| Type III | Extravasation through frank (≥1 mm) perforation |
| Type III/cavity spilling | Perforation into an anatomic cavity chamber, coronary sinus, etc |
Coronary perforation usually results in pericardial effusion with tamponnade and rarely evolves into a intramyocardial or subepicardial haematoma. As the clinical and echocardiographic features of this more subtle complication can be unrecognised, the outcome of such an event varies from cardiac death to—more exceptional—asymptomatic recovery.
Our patient underwent a high-risk PCI procedure with multiple risk factors for coronary perforation and developed a class III/cavity spilling perforation, resulting in a localised haematoma, which is rarely observed. Her clinical condition with excellent response to fluid therapy justified the conservative management. The diagnosis of a pericardial haematoma as a result of coronary perforation was promptly made, but in the absence of signs of pericardial effusion during the PCI procedure, the diagnosis was made hours after the final angiogram. The small amount of contrast extravasation was merely recognised retrospectively. Nevertheless, the perforation appeared to be restricted, or ‘contained’, and the patient remained haemodynamically stable and recovered well.
In this era of a growing need for complete percutaneous revascularisation in an increasingly complex patient population, there may be an increasing risk of complications. Rapid recognition of coronary perforation, as this remains one of the most frequent procedural complications, is essential. Angiographical classification is a strong predictor of mortality. Cardiac tamponnade is often easily recognised when class III perforation occurs, but one must be aware that extremely small coronary perforations can cause late subepicardial haematomas with a potential lethal outcome, if unrecognised.
Patient's perspective.
Our patient recovered fully without any further intervention, and therefore did not regard this episode as a potentially lethal one. She was relieved, naturally, when it was explained to her that major surgery is sometimes required, but not in her case.
Learning points.
Rapid recognition of coronary perforation is essential, as it remains one of the most frequent and lethal procedural complications.
Cardiac tamponnade is often easily recognised when class III perforation occurs, but one must be aware that extremely small coronary perforations can cause late subepicardial haematomas with a potential lethal outcome, if unrecognised.
Cavity spilling coronary perforations often require surgical interventions, small haematomas, however, can sometimes be contained and managed conservative.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Fefer P, Knudtson M, Cheema A, et al. . Current perspectives on coronary total occlusions: the Canadian Multicentre Chronic Total Occlusions Registry. J Am Coll Cardiol 2012;59:991–7 [DOI] [PubMed] [Google Scholar]
- 2.Hannan EL, Racz M, Holmes DR, et al. . Impact of completeness of percutaneous coronary intervention revascularization on long-term outcomes in the stent era. Circulation 2006;113:2406–12 [DOI] [PubMed] [Google Scholar]
- 3.Hendry C, Fraser D, Eichhofer J, et al. . Coronary perforation in the drug-eluting stent era: incidence, risk factors, management and outcome: the UK experience. EuroIntervention 2012;15:79–86 [DOI] [PubMed] [Google Scholar]
- 4.Shimony A, Zahger D, Van Straten M, et al. . Incidence, risk factors, management and outcomes of coronary artery perforation during percutaneous coronary intervention. Am J Cardiol 2009;104:1674–77 [DOI] [PubMed] [Google Scholar]
- 5.Ellis SG, Ajluni S, Arnold AZ, et al. . Increased coronary perforation in the new device era. Incidence, classification, management and outcome. Circulation 1994;90:2725–30 [DOI] [PubMed] [Google Scholar]