Abstract
Background: Individuals with posttraumatic stress disorder (PTSD) often exhibit high-risk substance use behaviors. Complementary and alternative therapies are increasingly used for mental health disorders, although evidence is sparse.
Objectives: Investigate the effect of a yoga intervention on alcohol and drug abuse behaviors in women with PTSD. Secondary outcomes include changes in PTSD symptom perception and management and initiation of evidence-based therapies.
Materials and Methods: The current investigation analyzed data from a pilot randomized controlled trial comparing a 12-session yoga intervention with an assessment control for women age 18 to 65 years with PTSD. The Alcohol Use Disorder Identification Test (AUDIT) and Drug Use Disorder Identification Test (DUDIT) were administered at baseline, after the intervention, and a 1-month follow-up. Linear mixed models were used to test the significance of the change in AUDIT and DUDIT scores over time. Treatment-seeking questions were compared by using Fisher exact tests.
Results: The mean AUDIT and DUDIT scores decreased in the yoga group; in the control group, mean AUDIT score increased while mean DUDIT score remained stable. In the linear mixed models, the change in AUDIT and DUDIT scores over time did not differ significantly by group. Most yoga group participants reported a reduction in symptoms and improved symptom management. All participants expressed interest in psychotherapy for PTSD, although only two participants, both in the yoga group, initiated therapy.
Conclusions: Results from this pilot study suggest that a specialized yoga therapy may play a role in attenuating the symptoms of PTSD, reducing risk of alcohol and drug use, and promoting interest in evidence-based psychotherapy. Further research is needed to confirm and evaluate the strength of these effects.
Introduction
Posttraumatic stress disorder (PTSD) affects many individuals in the general population1 and those who have served in the armed forces.2–4 Rates for this debilitating mental health disorder differ across sexes, with women in the United States having higher odds of developing PTSD.5 It is estimated that nearly 10% of women in the general population6 and 9% to 27% of female veterans have received a diagnosis of lifetime PTSD.7,8
Diagnostic and Statistical Manual of Mental Disorders-IV (DSM-IV) diagnostic criteria for PTSD include exposure to a traumatic event, persistent re-experiencing of the trauma, efforts to avoid triggers related to the trauma, and hyperarousal or physiologic reactivity.9 Individuals with PTSD face many barriers to care, some of which are related to the underlying disorder. For example, avoidance, a defining symptom of PTSD, may prevent patients from seeking help.10 Patients with PTSD often have more comorbid medical illnesses and poorer physical health,11–14 which dominate the primary care encounter and limit opportunities for screening and treatment.15 Fear of stigma associated with mental health disorders and poor access to mental healthcare may also keep patients from engaging in evidence-based therapies,2,10,15 including psychotherapy and pharmacotherapy. Prolonged exposure therapy, a well-studied cognitive behavioral approach in which patients explore their trauma with the therapist, may acutely increase PTSD symptoms and be difficult to tolerate.16 Likewise, side effects from medications commonly used in PTSD may limit adherence.17
Substance use is often conceptualized as maladaptive “self-medication” for PTSD symptoms, and some evidence supports this mechanism.18 Substance use disorders (SUDs) are commonly observed in individuals with PTSD: Previous studies reported a 20% prevalence of comorbid SUDs among individuals with PTSD in the general population,19,20 and veterans with PTSD were 3 to 4.5 times more likely to carry a concurrent diagnosis of SUD compared with those with no mental health diagnosis.21 In a study of female veterans in the Northwest United States, participants with more severe PTSD, as measured by the validated PTSD Checklist, had increased odds of risk behaviors, including alcohol and illicit drug use (odds ratio, 1.68–2.04).14 Comorbid SUDs and PTSD are often more difficult to treat than either disorder alone, and prolonged exposure therapy may exacerbate substance use.22–24 While clinical studies of cotreatment of PTSD and SUDs show promise, availability of these specialized programs is limited. Even within the resource-rich setting of a research study, adherence and retention are suboptimal.25–28
Both the Institute of Medicine and the Department of Veterans Affairs (VA) have recognized that many patients and healthcare providers are turning to complementary and alternative medicine (CAM) for the treatment of PTSD.16,29 Complementary and alternative medicine refers to health approaches developed outside of conventional medicine that are used with or in lieu of conventional medicine. Integrative medicine blends evidence-based CAM with evidence-based medicine within a healthcare system.30 Patients commonly use CAM as adjunctive care with conventional medicine rather than exclusively,31 and some data suggest CAM use is more likely when access to conventional care is restricted31 or there is dissatisfaction with conventional care,32,33 although findings have been mixed.34,35
Mental health concerns are common reasons for use of CAM services.32–34 In a recent U.S. national survey, nearly 40% of participants with PTSD in past year reported CAM use.17 Similar rates have been observed among military personnel and veterans.34–36 Many CAM techniques overlap with those used in traditional PTSD treatment approaches, such as breathing and relaxation techniques or stress management, and are postulated to decrease the biologic stress response and improve emotion regulation.16,37,38 The National Center for Complementary and Alternative Medicine classifies CAM therapies into natural products, mind-body medicine, manipulative and body-based practices, and whole medical systems.39 Yoga, classified as a mind-body medicine, is currently not a licensed CAM system, although it is a popular CAM therapy,32 and is beginning to be integrated into conventional care within healthcare systems.30
While there is substantial interest in yoga, evidence for its efficacy in the treatment of PTSD and substance use is limited. Reviews have shown small positive effects of various yoga therapies on PTSD symptoms16 and decreases in addictive behaviors.40 A small number of studies have examined the use of yoga as a complementary therapy in addiction. In a single-arm pilot study of a Kundalini yoga intervention for eight men who had recently undergone alcohol detoxification, symptom management and quality of recovery improved.41 In a randomized controlled trial of 60 male inpatients with alcohol dependence, those randomly assigned to Sudarshana Kriya yoga had greater reduction of cortisol, adrenocorticotropic hormone, and biological hormones associated with stress as compared with usual care controls.42 Another randomized controlled trial of 59 male and female participants with opiate addiction receiving methadone maintenance therapy assigned participants to yoga versus group therapy in addition to standard individual therapy; addiction severity did not differ after the 5-month intervention.43
Few studies have examined yoga as a treatment modality in addiction among female participants. Bock and colleagues added yoga as adjunctive therapy to cognitive-behavioral therapy and compared the intervention to a general health and wellness class in a randomized controlled trial of smoking cessation in 55 women. Women in the yoga group had a higher 24-hour and 7-day abstinence rate compared with controls at the end of the 8-week intervention.44
Research examining yoga therapies for comorbid PTSD and SUD is even more limited. In a randomized controlled trial of a multicomponent yoga breath program versus waitlist control for 50 male Vietnam veterans, Carter and colleagues found a significant reduction in PTSD symptoms in the yoga group, as measured by the Clinically Administered PTSD Scale as well as a nonsignificant decrease in Alcohol Use Disorder Identification Test (AUDIT) scores in participants with high-risk alcohol use.45 More research is needed to guide clinicians on appropriate recommendation of yoga and other CAM therapies for mental health disorders, and little is known about the effect of CAM therapies on engagement and retention in evidence-based therapies.37
The current investigation is based on secondary analysis of data from a pilot yoga intervention for PTSD symptoms. The parent study found that both the yoga and control groups experienced improvements in re-experiencing symptoms; the yoga group demonstrated improvements in hyperarousal symptoms as well.46 The current study examined the effect of the intervention on alcohol and drug use in women with PTSD. As secondary outcomes, the changes in PTSD symptom perception, PTSD symptom management, and initiation of evidence-based therapies were evaluated. The study hypothesized that participants in the yoga intervention would report decreased risk of substance abuse, decreased perception of PTSD symptoms, improved symptom management, and increased use of conventional mental health treatment.
Materials and Methods
The parent study was a randomized controlled pilot comparing women in a 12-session yoga intervention with an assessment-only control group.46 The institutional review board at VA Boston Healthcare System approved the research protocol. All participants provided written informed consent.
Participants
Participants were recruited through flyers placed in VA clinics, including PTSD treatment and primary care settings, and common areas throughout the hospital. Potential participants were also contacted through the National Center for PTSD database at the VA, which contains information on patients who have consented to be contacted for ongoing research studies. Additionally, community participants were recruited through online advertisements (i.e., Craigslist).
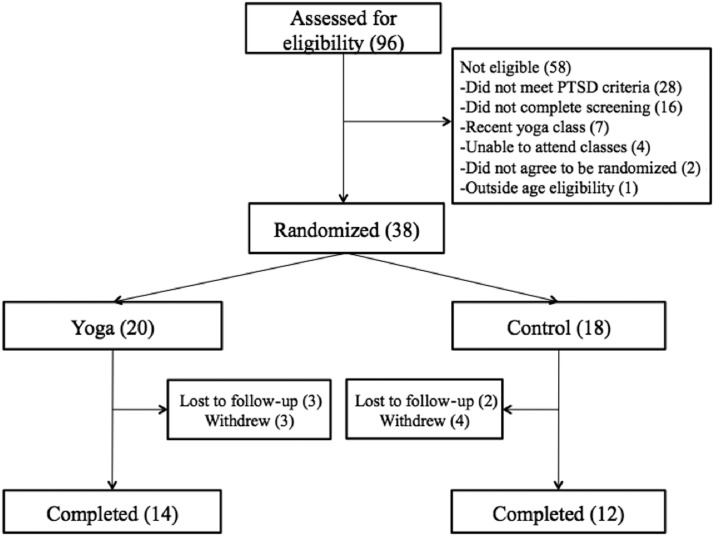
Participants were female, age 18 to 65 years, with at least subthreshold PTSD according to the PTSD Symptom Scale-Interview (PSS-I),47 as indicated by at least one symptom in each PTSD criterion category of re-experiencing, avoidance, and hyperarousal or meeting criteria for two symptom categories.6,48 Each participant was required to obtain a signed letter from her primary care provider stating it was safe for the patient to participate in mild to moderate yoga. Participants with active suicidal or homicidal ideation or who were not receiving stable doses of psychiatric medications were excluded. Women with substance dependence within the past 3 months, as identified by the Structured Clinical Interview for the DSM, were excluded.49 Women were also excluded if they indicated attending a yoga class within the past 6 months or an inability to commit to attending the sessions for the duration of the study. Ninety-six participants were assessed for eligibility; the most common reason for exclusion was not meeting the criteria for PTSD or subthreshold PTSD (Fig. 1). Ultimately, 38 participants were randomly assigned, and 26 completed the study, with completers attending 75% or more of the classes. Nine participants were veterans, and 29 were civilians.
FIG. 1.
Study recruitment and participant flow. PTSD, posttraumatic stress disorder.
Procedures
Participants were screened for eligibility by study staff first by telephone and then with an in-person diagnostic interview. Eligible participants completed baseline assessments before randomization to the yoga group or assessment-only control group.
As described previously, the yoga intervention consisted of 12 Kripalu-based Hatha yoga sessions of 75 minutes each, which included pose modifications for different fitness levels and incorporated guidelines of trauma-sensitive yoga.46 Trauma-sensitive yoga uses inviting, nonthreatening language while avoiding physical contact.50 Additionally, the yoga intervention incorporated elements of mindfulness and dialectical behavioral therapy, a specialized form of cognitive-behavioral therapy.46 For example, class themes included mindfulness, emotion regulation, interpersonal effectiveness, and distress tolerance. The control group completed assessments at the same time intervals as the intervention group. After the study, the control group was offered yoga classes.
Assessments were performed at baseline, immediately after the intervention, and at the 1-month follow-up. Reimbursements were equivalent in each group, including $30 each for the baseline and 1-month follow-up assessments and $20 per weekly assessment and class, for up to $300 per participant. All participants received a free yoga mat and water bottle.
Measures
Demographic information, including age, weight, height, ethnicity, educational attainment, and civilian or veteran status, was collected, along with information on patient's baseline yoga experience and yoga practice outside of the study.
The alcohol use disorder identification test (AUDIT) is a 10-item questionnaire that was developed to screen for a range of alcohol risk behaviors, including hazardous drinking, harmful use, and alcohol dependence.51 Scores above 6 for women indicate risk of hazardous drinking that warrants intervention. The AUDIT has high internal consistency and test-retest reliability. In the current study, the Cronbach α for this measure at baseline was 0.76.
The Drug Use Disorders Identification Test (DUDIT) is an 11-item questionnaire that screens for substance use and dependence.52 A score of 6 or greater for men and 2 or greater for women suggests a drug-related problem. This instrument has demonstrated good internal consistency. In the current study, the Cronbach α for this measure at baseline was 0.74.
Study investigators developed a novel Treatment-Seeking Questionnaire to assess (1) whether the participant had ever met with a professional regarding mental health before the study, (2) whether she had sought mental health care during the study, (3) whether she had interest in PTSD therapy, and (4) PTSD symptom perception and management since the beginning of the study. Responses to these latter two questions were analyzed at the 1-month follow-up.
Statistical analyses
Baseline demographic information were summarized; intervention and control groups were compared by using t-tests for continuous variables and Fisher exact tests for categorical variables. Mean AUDIT and DUDIT scores were calculated for each group at baseline, after the intervention, and at follow-up. Given the presence of missing data points for a small sample, a linear mixed model was used to test the significance of the change in AUDIT and DUDIT scores over time. Time, intervention group, and the interaction of time and group (i.e., the growth rate) were modeled as fixed effects, while intercept and slope of time were modeled as random effects for the study participants. Treatment-seeking questions were compared with Fisher exact tests. All analyses were conducted using SAS software, version 9.3 (SAS Institute, Inc., Cary, NC).
Results
Baseline characteristics for the study participants are presented in Table 1 and have been previously reported.46 Demographic characteristics did not significantly differ between the two groups. In addition, there was no difference in baseline characteristics or outcome measures for yoga completers versus noncompleters,46 or for veteran participants versus civilians (results available upon request). Both groups had a substantial history of past psychotherapy for PTSD (41.4%) and past yoga experience (47.4%). At baseline, the mean AUDIT score for the sample was 2.61 (Table 2). Immediately after the intervention and at follow-up, the mean AUDIT score decreased in the yoga group and increased in the control group. Likewise, the mean DUDIT score was similar between groups at baseline (mean, 1.00), decreasing in the yoga group and remaining stable in the control group (Table 3). In the linear mixed models, the null model likelihood ratio tests for AUDIT and DUDIT scores were significant (p<0.001), indicating that including random effects in the model contributed significantly to the variance in the outcome compared to the model with fixed effects alone. However, the change in AUDIT (B=0.0057, t=0.54, p=0.59) and DUDIT (B=0.0004, t=0.06, p=0.95) scores over time did not differ significantly by group.
Table 1.
Baseline Characteristics
| Characteristic | Total (n=38) | Yoga (n=20) | Control (n=18) |
|---|---|---|---|
| Mean age (y) | 44.4±12.4 | 45.5±12.1 | 43.2±12.9 |
| Mean body–mass index (kg/m2) | 29.39±7.4 | 29.1±7.4 | 29.7±7.6 |
| Education, n (%) | |||
| High school/GED | 2 (5.3) | 2 (10.0) | 0 (0.0) |
| Some college | 15 (39.5) | 4 (20.0) | 11 (61.1) |
| College complete | 10 (25.3) | 6 (30.0) | 4 (22.2) |
| Advanced degree | 11 (29.0) | 8 (40.0) | 3 (16.7) |
| Ethnicity, n (%) | |||
| White | 20 (52.6) | 12 (60.0) | 8 (44.4) |
| Black | 14 (36.8) | 6 (30.0) | 8 (44.4) |
| Asian | 2 (5.3) | 0 (0.0) | 2 (11.1) |
| Other | 2 (5.3) | 2 (10.0) | 0 (0.0) |
| Veteran status, n (%) | |||
| Veteran | 9 (23.7) | 6 (30.0) | 3 (16.7) |
| Civilian | 29 (76.3) | 14 (70.0) | 15 (83.3) |
| Past PTSD therapy, n (%) | 12 (41.4) | 7 (46.7) | 5 (35.7) |
| Yoga experience, n (%) | 18 (47.4) | 9 (45.0) | 9 (50.0) |
Mean values are expressed with standard deviation.
GED, general educational development; PTSD, posttraumatic stress disorder.
Table 2.
Alcohol Use Disorders Identification Test Scores at Baseline, After Intervention, and at 1-Month Follow-Up
| Total | Yoga | Control | ||||
|---|---|---|---|---|---|---|
| Time point | Participants (n) | Mean score | Participants (n) | Mean score | Participants (n) | Mean score |
| Baseline | 38 | 2.61±3.64 | 20 | 1.95±2.35 | 18 | 3.33±4.64 |
| Postintervention | 25 | 2.56±3.97 | 14 | 1.29±1.20 | 11 | 4.18±5.55 |
| Follow-up | 25 | 3.64±7.51 | 13 | 1.00±1.35 | 12 | 6.50±10.19 |
Mean values are expressed with standard deviation. Alcohol Use Disorders Identification Test scored on scale of 0–40. A score of 6 or greater in a woman indicates risk of hazardous drinking.
Table 3.
Drug Use Disorders Identification Test Scores at Baseline, After Intervention, and at 1-Month Follow-Up
| Total | Yoga | Control | ||||
|---|---|---|---|---|---|---|
| Time point | Participants (n) | Mean score | Participants (n) | Participants (n) | Mean score | Participants (n) |
| Baseline | 38 | 1.00±1.96 | 20 | 0.85±2.13 | 18 | 1.17±1.79 |
| Postintervention | 25 | 0.52±1.36 | 14 | 0.07±0.27 | 11 | 1.09±1.92 |
| Follow-up | 25 | 0.76±2.83 | 13 | 0.08±0.28 | 12 | 1.50±4.03 |
Mean values are expressed with standard deviation. Drug Use Disorders Identification Test scored on scale of 0–44. A score of 2 or greater in a woman suggests a drug-related problem.
Next, AUDIT and DUDIT scores were dichotomized into high and low risk, in which AUDIT scores greater than or equal to 6 and DUDIT scores greater than or equal to 2 were categorized as high risk. At baseline, 8% of all participants had high-risk drinking and 21% had high-risk drug use behaviors. At postintervention and follow-up, there were no high-risk alcohol or drug users in the yoga group compared with 3 participants with high-risk drinking in the control group at postintervention and follow-up. Likewise, there were 3 participants with high-risk drug behaviors in the control group after the intervention and 2 at follow-up. The difference in high-risk users between intervention and control groups was not statistically significant (all p>0.05).
When participants were surveyed about how they perceived their PTSD symptoms at 1-month follow-up, most participants in the yoga group (69%) reported that they noticed their symptoms less, while over 80% of control participants reported noticing their symptoms more or noted no difference in symptom perception (Table 4). Nearly all of the yoga participants (92%) reported coping better with their PTSD symptoms, while only a minority of control patients (9%) reported improved symptom management; this difference was statistically significant (Fisher exact test, 0.000016; p<0.001).
Table 4.
Posttraumatic Stress Disorder Symptom Perception and Management at 1-Month Follow-Up
| Question | Total (n=24) | Yoga (n=13) | Control (n=11) |
|---|---|---|---|
| What has your experience of your PTSD symptoms been since you started yoga? n (%) | |||
| I notice them more | 5 (20.8) | 2 (15.4) | 3 (27.3) |
| I notice them less | 11 (45.8) | 9 (69.2) | 2 (18.2) |
| No difference | 8 (33.3) | 2 (15.4) | 6 (54.6) |
| How do you handle your PTSD symptoms? n (%)* | |||
| I can handle them better | 13 (54.2) | 12 (92.3) | 1 (9.1) |
| I feel more overwhelmed by them | 3 (12.5) | 1 (7.7) | 2 (18.2) |
| No difference | 8 (33.3) | 0 (0.0) | 8 (72.7) |
p<0.01.
PTSD, post-traumatic stress disorder.
Fifty-eight percent of all study participants reported practicing yoga outside of the study immediately after the intervention, increasing to 67% at 1-month follow-up. Most participants in both groups reported interest in psychotherapy for PTSD after the intervention (72%) and at follow-up (56%), with no difference between groups. Only 2 of these participants, both in the yoga group, sought mental health care for PTSD during the study period.
Discussion
In this study, women with PTSD symptoms were randomly assigned to a yoga intervention and their substance use risk was measured over time. Current findings illustrated a trend toward decreased alcohol and drug use risk among yoga participants relative to the assessment-only control group. Although these changes were not statistically significant, this may have been due to low power, given the small sample size.
Despite the widespread popular interest and growing academic interest in mind-body CAM therapies such as yoga,53 these therapies remain understudied, with uncertainty around effectiveness and direct cost to the patient. The few previous studies of yoga for SUDs or comorbid PTSD and SUDs have been relatively small,41 and many focused primarily on men.41,42 In addition, these studies were conducted in India,41,42 where there may be a higher level of cultural acceptance of yoga as a treatment. The current study adds to this body of literature in populations where yoga is not indigenous and by focusing on women, which is particularly important as women are more likely to participate in yoga.54
Similar to a previous, larger study by Carter and colleagues looking specifically at male veterans with PTSD and SUD, which showed reductions in PTSD and AUDIT scores after a yoga breath intervention,45 our study demonstrated a trend toward reduced AUDIT scores. In comparison to our study, participants in Carter and colleagues' investigation had higher-risk alcohol use at baseline. Given the common comorbidity of PTSD and SUD and significant dropout and nonresponse rates for empirically supported therapies,55 the engagement and retention in this complementary treatment for these chronic, relapsing conditions are notable. In the current study, which incorporated yoga postures as well as breathing into the intervention, most participants reported practicing yoga outside of the study, even increasing at the 1-month follow-up.
Participants in the yoga group reported significantly improved symptom management compared with controls, suggesting a potential mechanism by which yoga practice may reduce symptoms of PTSD. It is possible that improved symptom management may reduce participants' use of harmful coping mechanisms, such as alcohol and substance use. While few patients sought conventional care, many participants showed interest in psychotherapy for PTSD. It is unclear why a CAM intervention such as yoga may increase interest in evidence-based therapies, although it could be postulated that mindfulness may increase acceptance and reduce stigma. Similarly, a group activity for participants with trauma may feel less stigmatizing for those seeking treatment. Further research, both quantitative and qualitative, would help improve understanding of the relationship between conventional and complementary therapy.
These results should be viewed in the context of several limitations. This small pilot study had inadequate power to find statistically significant differences between groups. However, there is a need for more randomized controlled trials of CAM therapies,16 which our study design addresses. Participants were recruited on the basis of PTSD criteria and excluded if they had a diagnosis of current substance dependence. As a result, participants had a low risk of substance use at baseline, with limited room for improvement even with a positive effect of the intervention. The generalizability of these results to participants with higher-risk substance use or diagnosed SUD is limited. Additionally, health care utilization, such as adherence to concurrent psychotherapy and medications, was not assessed; thus, the study could not examine the effect of the yoga intervention on these variables. Once again, this was not the primary aim of the parent study but is an important direction for future research.
Conclusions
The results of this study suggest that a specialized yoga therapy may play a role in attenuating the symptoms of PTSD, possibly reducing the risk of substance abuse and promoting engagement with evidence-based therapies. However, replication, particularly with larger sample sizes, is needed to confirm these findings. Future research should examine the effect of CAM on utilization of conventional mental health services, in order to better guide clinicians on appropriate treatment options for a debilitating mental health disorder.
Acknowledgments
The authors thank Howard Cabral, PhD, for his statistical consultation.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Kessler RC CW. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry 2005;62:617–627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med 2004;351:13–22 [DOI] [PubMed] [Google Scholar]
- 3.Seal KH, Metzler TJ, Gima KS, et al. . Trends and risk factors for mental health diagnoses among Iraq and Afghanistan veterans using Department of Veterans Affairs health care, 2002–2008. Am J Public Helath 2009;99:1651–1658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Seal KH Bertenthal B, Miner CR, Marmar C. Bringing the war back home: mental health disorders among 103 788 us veterans returning from Iraq and Afghanistan seen at Department of Veterans Affairs facilities. Arch Intern Med 2007;167:476–42 [DOI] [PubMed] [Google Scholar]
- 5.Pietrzak RH, Goldstein RB, Southwick SM, Grant BF. Prevalence and Axis I comorbidity of full and partial posttraumatic stress disorder in the United States: results from wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. J Anxiety Disord 2011;25:456–465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mitchell K, Mazzeo S, Schlesinger M, Brewerton T, Smith B. Comorbidity of partial and subthreshold PTSD among men and women with eating disorders in the National Comorbidity Survey-Replication study. Int J Eat Disord 2012;45:307–315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Freedy J, Magruder K, Mainous A, Frueh B, Geesey M, Carnemolla M. gender differences in traumatic event exposure and mental health among veteran primary care patients. Mil Med 2010;175:750–758 [DOI] [PubMed] [Google Scholar]
- 8.Kulka R, Schlenger W, Fairbank J, et al. . Trauma and the Vietnam War Generation: Report of Findings from the National Vietnam Veterans Readjustment Study. Philadelphia, PA: Brunner/Mazel, 1990 [Google Scholar]
- 9.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV-TR. Washington, DC: American Psychiatric Association, 2000 [Google Scholar]
- 10.Ouimette P, Vogt D, Wade M, et al. . Perceived barriers to care among veterans health administration patients with posttraumatic stress disorder. Psychol Serv 2011;8:212–223 [Google Scholar]
- 11.Frayne SM, Seaver MR, Loveland S, et al. . Burden of medical illness in women with depression and posttraumatic stress disorder. Arch Intern Med 2004;164:1306–1312 [DOI] [PubMed] [Google Scholar]
- 12.Frayne SM, Chiu VY, Igbal S, et al. . Medical care needs of returning veterans with PTSD: their other burden. J Gen Intern Med 2011;26:33–39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nazarian D, Kimerling R, Frayne SM. Posttraumatic stress disorder, substance use disorders, and medical comorbidity among returning U.S. veterans. J Trauma Stress 2012;25:220–225 [DOI] [PubMed] [Google Scholar]
- 14.Dobie DJ, Kivlahan DR, Maynard C, et al. . Posttraumatic stress disorder in female veterans: association with self-reported health problems and functional impairment. Arch Intern Med 2004;164:394–400 [DOI] [PubMed] [Google Scholar]
- 15.Wisco BE, Marx BP, Keane TM. Screening, diagnosis, and treatment of post-traumatic stress disorder. Mil Med 2012;177:7–13 [DOI] [PubMed] [Google Scholar]
- 16.Strauss JL, Durham VA. Efficacy of complementary and alternative medicine therapies for posttraumatic stress disorder. Department of Veterans Affairs Health Services Research & Development Service; 2011. Available at: http://www.hsrd.research.va.gov/publications/esp/cam-ptsd.pdf Accessed July1, 2014 [PubMed] [Google Scholar]
- 17.Libby DJ, Pilver CE, Desai R. Complementary and alternative medicine use among individuals with posttraumatic stress disorder. Psychol Trauma Theory Res Pract Policy 2013;5:277–285 [Google Scholar]
- 18.Hien DA, Jiang H, Campbell ANC, et al. . Do treatment improvements in PTSD severity affect substance use outcomes? a secondary analysis from a randomized clinical trial in NIDA's Clinical Trials Network. Am J Psychiatry 2009;167:95–101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry 1995;52:1048–1060 [DOI] [PubMed] [Google Scholar]
- 20.Stein MB, McQuaid JR, Pedrelli P, Lenox R, McCahill ME. Posttraumatic stress disorder in the primary care medical setting. Gen Hosp Psychiatry 2000;22:261–269 [DOI] [PubMed] [Google Scholar]
- 21.Seal KH, Cohen G, Waldrop A, Cohen BE, Maguen S, Ren L. Substance use disorders in Iraq and Afghanistan veterans in VA healthcare, 2001–2010: Implications for screening, diagnosis and treatment. Drug Alcohol Depend 2011;116:93–101 [DOI] [PubMed] [Google Scholar]
- 22.Mills KL, Teesson M, Ross J, Darke S. The impact of post-traumatic stress disorder on treatment outcomes for heroin dependence. Addiction 2007;102:447–454 [DOI] [PubMed] [Google Scholar]
- 23.Riggs DS, Rukstalis M, Volpicelli JR, Kalmanson D, Foa EB. Demographic and social adjustment characteristics of patients with comorbid posttraumatic stress disorder and alcohol dependence: potential pitfalls to PTSD treatment. Addict Behav 2003;28:1717–1730 [DOI] [PubMed] [Google Scholar]
- 24.Mills K. TReatment of comorbid substance dependence and posttraumatic stress disorder. JAMA 2013;310:482–483 [DOI] [PubMed] [Google Scholar]
- 25.McGovern MP, Stecker T. Co-occurring Substance use and posttraumatic stress disorders: reasons for hope. J Dual Diagn 2011;7:187–193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sannibale C, Teesson M, Creamer M, et al. . Randomized controlled trial of cognitive behaviour therapy for comorbid post-traumatic stress disorder and alcohol use disorders. Addiction 2013;108:1397–1410 [DOI] [PubMed] [Google Scholar]
- 27.Mills KL, Teesson M, Back SE, et al. . Integrated exposure-based therapy for co-occurring posttraumatic stress disorder and substance dependence: a randomized controlled trial. JAMA 2012;308:690–699 [DOI] [PubMed] [Google Scholar]
- 28.Foa EB, Yusko DA, McLean CP, et al. . Concurrent naltrexone and prolonged exposure therapy for patients with comorbid alcohol dependence and PTSD: a randomized clinical trial. JAMA 2013;310:488–495 [DOI] [PubMed] [Google Scholar]
- 29.Institute of Medicine. Treatment for Posttraumatic Stress Disorder in Military and Veteran Populations: Initial Assessment. Washington, DC: The National Academy Press; 2012 [PubMed] [Google Scholar]
- 30.Goldblatt E; Academic Consortium for Complementary and Alternative Health Care, American Massage Therapy Association, Association of Accredited Naturopathic Medical Colleges, Association of Chiropractic Colleges, Council of Colleges of Acupuncture and Oriental Medicine, et al. Clinicians' and educators' desk reference on the licensed complementary and alternative healthcare professions. Seattle, WA: Academic Consortium for Complementary and Alternative Health Care, 2009 [Google Scholar]
- 31.Astin JA. Why patients use alternative medicine. JAMA 1998;279:1548–1553 [DOI] [PubMed] [Google Scholar]
- 32.Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Rep 2008; 1–23 [PubMed] [Google Scholar]
- 33.Kessler RC, Soukup J, Davis RB, et al. . The use of complementary and alternative therapies to treat anxiety and depression in the United States. Am J Psychiatry 2001;158:289–294 [DOI] [PubMed] [Google Scholar]
- 34.Smith TC, Ryan MA, Smith B, et al. . Complementary and alternative medicine use among US Navy and Marine Corps personnel. BMC Complement Altern Med 2007;7:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.White MR, Jacobson IG, Smith B, et al. . Health care utilization among complementary and alternative medicine users in a large military cohort. BMC Complement Altern Med 2011;11:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jacobson IG, White MR, Smith TC, et al. . Self-reported health symptoms and conditions among complementary and alternative medicine users in a large military cohort. Ann Epidemiol 2009;19:613–622 [DOI] [PubMed] [Google Scholar]
- 37.Libby DJ, Pilver CE, Desai R. Complementary and alternative medicine in VA specialized PTSD treatment programs. Psychiatr Serv 2012;63:1134–1136 [DOI] [PubMed] [Google Scholar]
- 38.Streeter CC, Gerbarg PL, Saper RB, Ciraulo DA, Brown RP. Effects of yoga on the autonomic nervous system, gamma-aminobutyric-acid, and allostasis in epilepsy, depression, and post-traumatic stress disorder. Med Hypotheses 2012;78:571–579 [DOI] [PubMed] [Google Scholar]
- 39.National Center for Complementary and Alternative Medicine. [cited 2012November19]; Available at: http://nccam.nih.gov/
- 40.Behere RV, Muralidharan K, Benegal V. Complementary and alternative medicine in the treatment of substance use disorders—a review of the evidence. Drug Alcohol Rev 2009;28:292–300 [DOI] [PubMed] [Google Scholar]
- 41.Khalsa SBS, Khalsa GS, Khalsa HK, Khalsa MK. Evaluation of a residential Kundalini yoga lifestyle pilot program for addiction in India. J Ethn Subst Abuse 2008;7:67–79 [DOI] [PubMed] [Google Scholar]
- 42.Vedamurthachar A, Janakiramaiah N, Hegde JM, et al. . Antidepressant efficacy and hormonal effects of Sudarshana Kriya Yoga (SKY) in alcohol dependent individuals. J Affect Disord 2006;94:249–253 [DOI] [PubMed] [Google Scholar]
- 43.Shaffer HJ, LaSalvia TA, Stein JP. Comparing Hatha yoga with dynamic group psychotherapy for enhancing methadone maintenance treatment: a randomized clinical trial. Altern Ther Health Med 1997;3:57–66 [PubMed] [Google Scholar]
- 44.Bock BC, Fava JL, Gaskins R, et al. . Yoga as a complementary treatment for smoking cessation in women. J Womens Health 2012;21:240–248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Carter JJ, Gerbarg PL, Brown RP, et al. . Multi-component yoga breath program for Vietnam veteran post traumatic stress disorder: randomized controlled trial. J Trauma Stress Disord Treat July31, 2013. doi: 10.4172/2324-8947.1000108 [DOI] [Google Scholar]
- 46.Mitchell K, Dick A, DiMartino D, et al. . A pilot study of a randomized controlled trial of yoga for PTSD symptoms in women. J Trauma Stress 2014;27:121–128 [DOI] [PubMed] [Google Scholar]
- 47.Foa EB, Riggs DS, Dancu CV, Rothbaum BO. Reliability and validity of a brief instrument for assessing post-traumatic stress disorder. J Trauma Stress 1993;6:459–473 [Google Scholar]
- 48.Schnurr PP, Friedman MJ, Rosenberg SD. Premilitary MMPI scores as predictors of combat-related PTSD symptoms. Am J Psychiatry 1993;150:479–483 [DOI] [PubMed] [Google Scholar]
- 49.First M, Spitzer R, Gibbon M, Williams J. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition With Psychotic Screen (SCID-I/P W/PSY SCREEN). New York: Biometrics Research, New York State Psychiatric Institute, 2002 [Google Scholar]
- 50.Emerson D, Sharma R, Chaudhry S, Turner J. Trauma-sensitive yoga: principles, practice, and research. Int J Yoga Ther 2009;19:123–128 [Google Scholar]
- 51.Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. AUDIT. The Alcohol Use Disorders Identification Test. Guidelines for Use in Primary Care, 2nd ed. Available at: http://whqlibdoc.who.int/hq/2001/WHO_MSD_MSB_01.6a.pdf Accessed March1, 2014
- 52.Berman A, Bergman H, Palmstierna T, Schlyter F. The Drug Use Disorders Identification Test (DUDIT) Manual. Stockholm, Sweden: Karolinska Institutet, 2003 [Google Scholar]
- 53.Khalsa SBS. Yoga as a therapeutic intervention: a bibliometric analysis of published research studies. Indian J Physiol Pharmacol 2004;48:269–285 [PubMed] [Google Scholar]
- 54.Birdee GS, Legedza AT, Saper RB, et al. . Characteristics of yoga users: results of a national survey. J Gen Intern Med 2008;23:1653–1658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Schottenbauer MA, Glass CR, Arnkoff DB, Tendick V, Gray SH. Nonresponse and dropout rates in outcome studies on PTSD: review and methodological considerations. Psychiatry 2008;71:134–168 [DOI] [PubMed] [Google Scholar]