Abstract
Background: The home food environment influences children's eating behaviors and potentially affects overall diet quality. The aim of the present study was to evaluate the relationship between the home food environment and Hispanic children's diet quality.
Methods: Hispanic children, 10–14 years of age (n=187), and their parents participated in this cross-sectional study. The Healthy Eating Index (HEI) was used to determine diet quality based on reported dietary intake obtained through a food frequency questionnaire administered to the children. Parents self-reported home food availability, familial eating habits, and their own habitual diet through a home environment survey.
Results: The children's HEI total score was 59.4±8.8. Reported diets did not adhere to the dietary recommendations for total vegetables, greens and beans, whole grains, seafood and plant proteins, fatty acids, refined grains, sodium, solid fats, and added sugars. None of the participants had “good” scores (HEI, >80), 86% had scores that “need improvement” (HEI, 51–80), and 14% had “poor” scores (HEI, <50). Children with lower HEI scores had sugar-sweetened beverages available at home and participated in family meals while watching television more frequently, when compared with children with higher HEI scores.
Conclusions: Home food availability, parental diet, and familial eating habits seem to play an important role in the diet quality of children. Interventions targeting family education on healthful dietary habits at home could have a positive impact on children's diet quality and overall health.
Introduction
The burden of obesity falls disproportionately on minority groups. The prevalence of obesity among non-Hispanic white adolescents was 16.1% by 2010, whereas that for Hispanics was greater than 23%.1 Food environments that promote dietary patterns that are high in energy-dense, nutrient-poor foods usually lead to a positive energy imbalance and thus to excess weight gain.2 Poor diet quality is known to increase the risk for obesity, diabetes, and all-cause mortality.3,4 One means of assessing diet quality is by using the Healthy Eating Index (HEI), which scores compliance with the Dietary Guidelines for Americans.5 When the HEI was used to assess the diet quality of children in the United States, it provided evidence of poor to modest compliance with dietary guidelines, with children's diet quality averaging only 55.9 of 100 points.6,7
The home food environment and familial eating habits play a key role in children's diet given that they impart examples of eating habits and influence access to foods at home.8 For example, extensive research has demonstrated a positive association between fruit and vegetable availability at home and children's intakes of these foods, and the frequency of family meals is proposed to influence the diet of children.9,10 However, as children age, their food habits reflect a lessening of the role of parental influences, in that older children are found to eat less fruits and vegetables and more energy-dense foods and beverages.11
Because there are a paucity of data available regarding the extent to which home food availability and familial eating habits specifically influence diet quality among Hispanic children, the present study focused on this group. The aim was to evaluate the diet quality of urban Hispanic children and investigate the influences of home food availability, parental diet, and familial eating habits on children's overall diet quality. We focused on this Hispanic community because it represents an underserved minority group with increased risk for obesity.
Methods
The present study was part of a multidisciplinary research project between investigators at the University of Wisconsin–Madison and the United Community Center (UCC)–Bruce-Guadalupe Charter School (BGCS) in Milwaukee, Wisconsin. The BGCS has 860 enrolled students, 98% of whom are Hispanic. The study target population was children attending BGCS and their parents. Inclusion criteria for the children included academic attendance at the BGCS in grades 5–8 (n=300) and Hispanic ethnicity. Recruitment included sending descriptive study materials to their homes and providing oral and written information during family events at the school. A contribution was made to the school toward health education, and gift cards ($25) were offered to parents for completion of the home survey. Children were not compensated for participation in the study. The University of Wisconsin–Madison Institutional Review Board approved the study, and written parental consent and participant assent were obtained before inclusion in the study.
Children's weight was measured using a beam balance scale, and height was measured using a stadiometer at the school physical education class without shoes and in light clothing. BMI was calculated as weight in kilograms divided by height in meters squared (kg/m2). CDC growth charts were used to classify childhood overweight and obesity.12
The children's diet was assessed using the Block for Kid's Food Frequency Questionnaire (FFQ) with Hispanic foods.13 The questionnaire surveys foods and beverages consumed during the previous 7 days. Study personnel administered the questionnaire, and the first few questions were read aloud until it was determined that participants understood how to complete the survey. Pictures were provided to enhance accuracy of quantification of portion size. The original questionnaire was validated in numerous studies and in a variety of populations.13,14 This specific FFQ has not been validated exclusively in Hispanic populations. Therefore, we pretested its design and comprehension with a subgroup of children (n=10) who participated in the study to assess whether the children understood the questions. No changes were made to the original FFQ given that the subgroup of children who participated in our pretest had no difficulty understanding the survey.
The children's diet quality was calculated based on dietary intake obtained through the FFQ administered to the children using the HEI–2010 scoring criteria (Table 1).15 The HEI was calculated in the present study using SAS software (version 9.3; SAS Institute Inc., Cary, NC). The original SAS coding was available at the USDA Center for Nutrition Policy and Promotion website.16 The total HEI score ranges from 0 to 100, with a higher score indicating a higher quality of diet. The scoring uses a density approach to set standards, and food components are expressed as percent of total energy or per 1000 kcal, as a proxy for energy intake adjustment. The adequacy and moderation of intake are captured with higher scores for increased intake of total fruit, whole fruit, total vegetables, greens and beans component, whole grains, dairy, total proteins, seafood and plant proteins, and fatty acids together with moderation or reduced intake of refined grains, sodium, and empty calories. Individual intakes for each food component consumed at the level of recommendation or above received the maximum number of points. Reported intakes between the minimum and maximum standards were scored proportionally. A total score was then derived from the sum of individual food component scores.
Table 1.
Healthy Eating Index (2010) Scoring Criteriaa
| Food componentsb | Maximum points | Standard for maximum score | Standard for minimum score of zero |
|---|---|---|---|
| Adequacy | |||
| Total fruitc | 5 | ≥0.8 cup equivalent per 1000 kcal | No fruit |
| Whole fruitd | 5 | ≥0.4 cup equivalent per 1000 kcal | No whole fruit |
| Total vegetablese | 5 | ≥1.1 cup equivalent per 1000 kcal | No vegetables |
| Greens and beanse | 5 | ≥0.2 cup equivalent per 1000 kcal | No dark green vegetables |
| Whole grains | 10 | ≥1.5-oz equivalent per 1000 kcal | No whole grains |
| Dairyf | 10 | ≥1.3-oz equivalent per 1000 kcal | No dairy |
| Total protein foodsg | 5 | ≥2.5-oz equivalent per 1000 kcal | No protein foods |
| Seafood and plant proteinsg,h | 5 | ≥0.8-oz equivalent per 1000 kcal | No seafood or plant proteins |
| Fatty acidsi | 10 | (PUFAs+MUFAs)/SFAs>2.5 | (PUFAs+MUFAs)/SFAs≤1.2 |
| Moderation | |||
| Refined grains | 10 | ≤1.8-oz equivalent per 1000 kcal | ≥4.3-oz equivalent per 1000 kcal |
| Sodium | 10 | ≤1.1 g per 1000 kcal | ≥2.0 g per 1000 kcal |
| Empty caloriesj | 20 | ≤19% of energy | ≥50% of energy |
Table adapted from Guenther and colleagues.15
Intakes between the minimum and the maximum standards are scored proportionally.
Includes fruit juice.
Includes all forms except juice.
Includes any beans and peas not counted as total protein foods.
Includes all milk products, such as fluid milk, yogurt, cheese, and fortified soy beverages.
Beans and peas are included here when the total protein foods are otherwise not met.
Includes seafood, nuts, seeds, soy products, and beans and peas counted as total protein foods.
Ratio of PUFAs and MUFAs to SFAs.
Calories from solid fats, alcohol, and added sugars; threshold for counting alcohol is >13 g per 1000 kcal.
PUFAs, polyunsaturated fatty acids; MUFAs, monounsaturated fatty acids; SFAs, saturated fatty acids.
The home environment was assessed using a survey designed jointly by university and community partners. Given the complexity of measures and to minimize burden on the study participants, questions for all measures were merged into a single survey. Selection of constructs to assess the home environment was guided by the social ecological theory.17 A literature review was also conducted to gather available validated items to assess the home environment in relation to children's diet, and items were taken from the most widely used instruments.18–20 Finally, a pilot test of the survey was conducted with a subgroup of parents (n=10) of students at BGCS who were participating in the study to determine applicability and comprehension. UCC research personnel conducted interviews and open-ended questions were used to help select survey items, and additional items were generated as needed. The questionnaire was available in English and Spanish.
Statistical Analysis
A total of 187 children were enrolled in the cross-sectional study. Parents provided parental consent for the children to participate, but only 93% (n=173) of parents agreed to participate in the study themselves. Children (n=4) who did not complete the dietary intake survey (FFQ) and subjects (n=8) with highly implausible reported energy intakes (<500 or >3500 kcal) were removed only from further dietary intake analysis. The distribution of dietary intake and diet quality across potential confounders, which may alter total energy intake, was examined with respect to age, gender, and family income. Univariate linear regression models were used to evaluate the relationships between children's calculated HEI total score and home food availability, parental reported diet, and familial eating habits. For dichotomous variables, linear models were used to compare the children's HEI total score across the reported availability of foods at home. HEI total scores in categories of parental reported diet and familial eating habit variables were compared: Reference value (never) to each increased frequency category and p values for each comparison are reported. A test of linear trend that used a continuous specification of ordinal variable across the categories was also conducted. Regression models were adjusted for children's age and gender. p values <0.05 were considered statistically significant. All analyses were completed with SAS software (version 9.3; SAS Institute).
Results
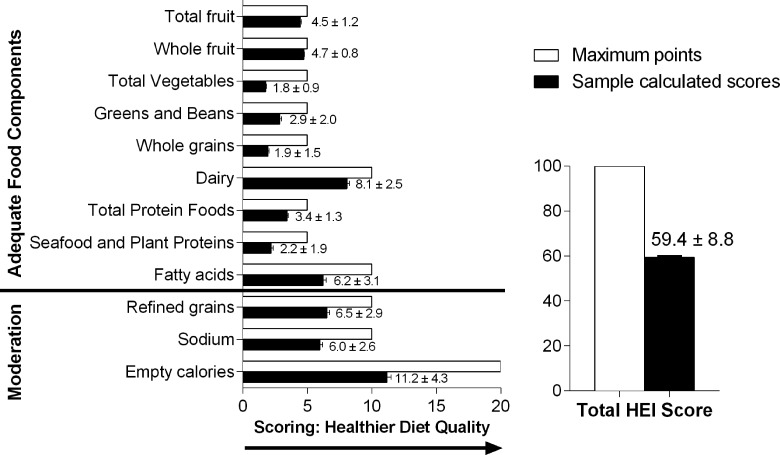
The final sample for the present study consisted of 187 Hispanic children 11.9±1.4 years of age (47% males) and their parents. In this sample, 47% of children were healthy weight, 25% were overweight, and 28% were obese. The HEI total score was 59.4±8.8, and most of the HEI food components received only approximately half of the maximum score (Fig. 1), reflecting dietary patterns failing to meet dietary recommendations. Children in this study obtained good scores for total fruit, whole fruit, dairy, and total protein foods; they, however, did not meet the recommendations for total vegetables, greens and beans, and whole grains food components. Children failed to adhere to recommendations for seafood and plant proteins, fatty acids, refined grains, sodium, and empty calories (i.e., solid fats and added sugars).
Figure 1.
Children's calculated mean (±standard error) HEI food component and total scores. HEI, Healthy Eating Index.
Table 2 illustrates frequency of distribution of home food availability, parental dietary intake, and familial eating habits. Most parents reported having fruits, vegetables, 100% fruit juice, and milk available at home (97%, 91%, 86%, and 83% of parents, respectively). Fifty-six percent of parents reported having soda in the home, and 54% reported having fruit drinks available in the home. Eighty-four percent reported having energy-dense snacks, such as potato chips, cookies, cake, and/or ice cream, available in their homes during the past week. As for parental dietary intake, most parents reported consumption of fruits, vegetables, 100% fruit juice, and milk at least twice per week (88%, 83%, 78%, and 91% of parents, respectively), whereas 42% reported consumption of soda, 38% reported consumption of fruit drinks, and 60% reported intakes of energy-dense snacks at least twice per week. Family meals were reported as frequent behaviors in that most families reported having family meals (89%) at least twice per week, whereas approximately 50% of the families reported eating a meal while watching television (TV) at least twice per week.
Table 2.
Home Food Availability, Parental Dietary Intake, and Familial Eating Habit Characteristicsa
| Measure of interest | n | % |
|---|---|---|
| Home food availability (reported foods and beverages available in the home) | ||
| Fruits | 155 | 97 |
| Vegetables | 144 | 91 |
| 100% fruit juice | 132 | 86 |
| Milk | 128 | 83 |
| Soda | 81 | 56 |
| Fruit drinks | 83 | 54 |
| Snacksb | 133 | 84 |
| Parental reported intake (≥2 times per week) | ||
| Fruits | 136 | 88 |
| Vegetables | 127 | 83 |
| 100% fruit juice | 118 | 78 |
| Milk | 140 | 91 |
| Soda | 65 | 42 |
| Fruit drinks | 60 | 38 |
| Snacksb | 94 | 60 |
| Familial eating habits (≥2 times per week) | ||
| Family meals | 138 | 89 |
| Family meals while watching television | 78 | 50 |
n=173.
Snacks were described as sweets or desserts, such as cookies, candy, cake, and/or ice cream, also including salty snacks, such as tortilla or potato chips.
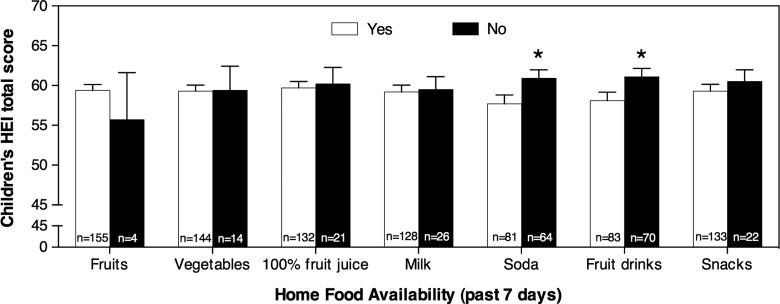
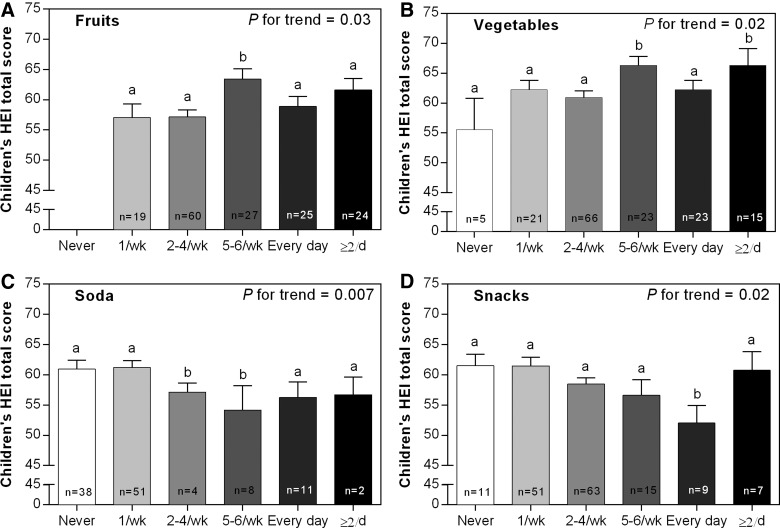
The results for home food availability associations with children's HEI total score are presented in Figure 2. Soda and fruit drink availability at home were both associated with a significant, but modest, reduction in children's HEI scores (HEI: 60.9 vs. 57.7 and HEI: 61.1 vs. 58.1, respectively; p<0.05). Parental diet associations with children's HEI total score included their reported intake of nutrient-rich and nutrient-poor, energy-dense foods and beverages (Fig. 3). Parental reported intake of fruits and vegetables were found to be positively associated with children's HEI total score (p for trend =0.03 and 0.02, respectively). Parental reported intake of milk and 100% fruit juice was not associated with children's HEI total score (Supplementary Table 2; see online supplementary material at www.liebertpub.com/chi); however, reported intakes of soda and energy-dense snacks, which are foods to be eaten in moderation and thus foods for which higher intake is scored lower, were inversely associated with children's HEI total score (p for trend=0.007 and 0.02, respectively). Parents' highest reported intake of 100% fruit juice was found to be positively associated with children's HEI total score, only when compared to the reference value (HEI: 61.6 vs. 53.4; p value=0.04), but no significant linear trend was found (Supplementary Table 2; see online supplementary material at www.liebertpub.com/chi).
Figure 2.
Children's calculated mean (±standard error) Healthy Eating Index (HEI) total score by reported home food availability. Univariate linear regression models were used for differences in children's HEI total score by home food availability (dichotomous variable: yes or no). The distribution (n value) of responses is illustrated for each category. *p<0.05. Refer to Supplementary Table 1 for complete regression analyses results (see online supplementary material at www.liebertpub.com/chi).
Figure 3.
Children's calculated mean (±standard error) Healthy Eating Index (HEI) score in categories of parental reported frequent intake of foods and beverages (panels A–D: fruits, vegetables, soda, and snacks). Univariate linear regression models were used to test for linear trend that used a continuous specification of ordinal variables across parental reported frequent intake (never, once per week, 2–4 times per week, 5–6 times per week, every day, and twice or more per day), and for comparing the reference value (never) with every increased frequency in parental reported intake. None of the parents reported “never” having fruits during the past week; therefore, the reference value for this association was “once per week.” The distribution (n value) of responses is indicated for each category. Bars with different letters are significantly different from the reference value (never). *p<0.05. Refer to Supplementary Table 2 for complete regression analyses results (see online supplementary material at www.liebertpub.com/chi).
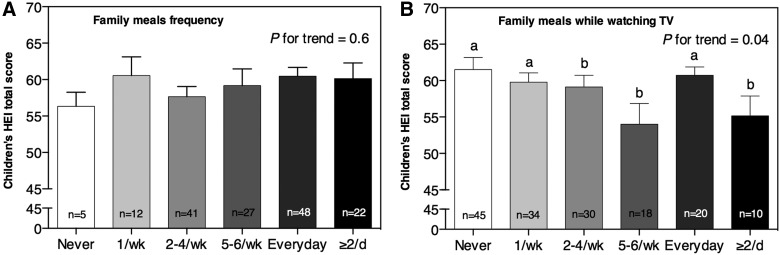
Figure 4 illustrates the results for the relationship between children's HEI total score and frequency of family meals, as well as family meals while watching TV. Family meals while watching TV were inversely associated with children's HEI total score, and children's HEI total scores decreased significantly as reported family meals while watching TV frequency increased (HEI: 61 to 55; p for trend=0.04). Given the high prevalence of overweight and obesity in this cohort of Hispanic children, we evaluated the association between children's weight status and diet quality. But, contrary to what we expected, HEI total scores were not found to be associated with weight status in this community (p value=0.7)
Figure 4.
Children's calculated mean (±standard error) Healthy Eating Index (HEI) total score in categories of family meal frequency. (A) Family meal frequency. (B) Family meals while watching television (TV). Univariate linear regression models were used to test for linear trend that used a continuous specification of ordinal variables across family meals reported frequency (never, once per week, 2–4 times per week, 5–6 times per week, every day, and twice or more per day) and for comparing the reference value (never) with every increased frequency in family meals. The distribution (n value) of responses is indicated for each category. Bars with different letters are significantly different from the reference value (never). *p<0.05. Refer to Supplementary Table 3 for complete regression analyses results (see online supplementary material at www.liebertpub.com/chi).
Discussion
The diet quality of Hispanic children in this study was in need of improvement. This is comparable to recent reports among US youth, where children's reported diet resulted in low HEI scores (55.9 of 100).6 Reported dietary intakes in the current study revealed a lack of adherence to recommendations to dietary guidelines, including total vegetables, greens and beans, whole grains, seafood and plant proteins, fatty acids, refined grains, sodium, added sugars, and solid fats. The home food availability, parental diet, and family eating habits were found to be associated with the diet quality of Hispanic children.
To our knowledge, this is the first study to evaluate the associations between different aspects of the home food environment and Hispanic children's diet quality using the HEI. In the present study, most of the families reported having healthy foods available at home, such as fruits and vegetables, but it was the availability of sugar-sweetened beverages (SSBs) and energy-dense snacks that had an apparent negative impact on the diet quality of the children. Similar to our results, among children (8–13 years of age), investigators identified several predictors of SSB consumption, including SSB availability at home, taste preferences, and parental SSB intake.21 A similar approach for the association between eating behaviors and the home environment on children's diets was conducted among a primarily minority population of adolescent girls, which included 11% Hispanic adolescents.20 It was reported that the availability of SSBs at home was positively associated with girls' intake of these beverages. In addition, having fruits and vegetables available at home and the frequency of family meals were positively associated with girls' consumption of fruits and vegetables. These results suggest that the availability of nutrient-poor, energy-dense beverages as well as healthier food items, such as fruits and vegetables, at home may play a role in children's dietary intake and, consequently, in their overall diet quality.
Another tier of influence at home is the role of parental dietary habits that may affect children's preferences and intake of certain foods. Parental reported intakes of fruits and vegetables were positively associated with children's HEI total score, whereas parental reported intake of SSBs and energy-dense snacks were negatively associated with children's HEI total score. This is similar to reports among non-Hispanic white girls, where intakes of fruits and vegetables were predicted by their parents' reported intake of these foods.22 Similar reports among Hispanic children suggest an apparent influence of parents' dietary habits on children's diets, including similar intakes of dairy,23 SSBs,24 and fast food consumption.25 Further, longitudinal studies have reported that parental consumption of fruits, vegetables, and dairy at baseline predicted adolescent's intake of these foods 5 years later.23 These findings suggest that parents not only play a role in Hispanic children's access to foods and beverages at home, but also in their preferences for such foods and beverages given that children may mimic parental eating behaviors.
In the present study, we did not find a positive association between family meals and children's diet quality as hypothesized. We did find, however, an inverse association between family meals while watching TV and children's diet quality. These results are in agreement with findings by Feldman and colleagues,26 where family meals while watching TV were associated with poorer quality of diets among adolescents. They also found that family meals, even in the presence of TV, were associated with better eating habits than no family meals at all, which we did not confirm. Nonetheless, our study further supports the research by Feldman and colleagues,26 given that we focused on younger children rather than adolescents alone. These results indicate the complex interaction between watching TV and “unhealthy” eating, which has also been reported by others.27,28
Although not finding a relationship between HEI and weight status in the present study may appear surprising, it should be noted that the HEI was developed as a summary score for the diet relative to general dietary guidelines. The HEI dietary guidelines are not specific for obesity, but rather are meant to assess aspects of eating behaviors, and it does not directly capture calorie intake or physical activity. Further, our findings are in agreement with another study among Hispanic children, in which it was concluded that children's diet quality did not adhere to dietary recommendation for Americans and diet quality was not associated with their weight status.29
The weaknesses of the present study include the cross-sectional design, which prevents us from identifying causality, and the use of self-reported measures of children's dietary intake and home environment. Our findings, however, are in agreement with earlier research studies that have assessed home environments and have reported an apparent influence of the home food environment on children's dietary pattern.10,30 However, these results still need to be confirmed in longitudinal studies with validated tools, and the generalizability to age, ethnicity, and geographically diverse samples need to be tested.
Conclusions
The results suggest that home food availability, parental diet, and familial eating habits play an important role in the diet quality of Hispanic children. Interventions targeting family education should not only focus on having healthy foods available at home, but also include a focus on the reduction of nutrient-poor, energy-dense foods and beverages from the home given that they might negatively affect children's diet quality and overall health.
Supplementary Material
Acknowledgments
The community-engaged research project, Healthy Activities Partnership Program for Youth (HAPPY), is a partnership among staff from the Community Research Office and Bruce-Guadalupe Community School at the United Community Center in Milwaukee, Wisconsin, and researchers from the University of Wisconsin–Madison, who are members of the Wisconsin Prevention of Obesity and Diabetes (WiPOD) network. Also contributing to the success of HAPPY is funding from the University of Wisconsin (UW) Collaborative Center for Health Equity, a National Institutes of Health (NIH)/National Institute on Minority Health and Health Disparities–funded Center of Excellence in Minority Health and Health Disparities (grant no.: 5 P60 MD 003428).
Funding for this project was provided by the UW School of Medicine and Public Health from the Wisconsin Partnership Program (233-PRJ49PH), along with support from the UW Institute for Clinical and Translational Research, an NIH-funded Clinical and Translational Science Award (grant no.: 9U54TR000021). The sponsors had no involvement in the design, data collection, or analysis.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Ogden CL, Carroll MD, Flegal KM, et al. . Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA 2012;307:483–490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Campbell KJ, Crawford DA, Ball K. Family food environment and dietary behaviors likely to promote fatness in 5–6 year-old children. Int J Obes (Lond) 2006;30:1272–1280 [DOI] [PubMed] [Google Scholar]
- 3.Guo X, Warden BA, Paeratakul S, et al. . Healthy eating index and obesity. Eur J Clin Nutr 2004;58:1580–1586 [DOI] [PubMed] [Google Scholar]
- 4.McNaughton SA, Bates CJ, Mishra GD. Diet quality is associated with all-cause mortality in adults aged 65 years and older. J Nutr 2012;142:320–325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guenther PM, Reedy J, Krebs-Smith SM. Development of the Healthy Eating Index-2005. J Am Diet Assoc 2008;108:1896–1901 [DOI] [PubMed] [Google Scholar]
- 6.Fungwe T, Guenther PM, Juan WY, et al. . The Quality of Children's Diets in 2003–04 as Measured by the Healthy Eating Index-2005. US Department of Agriculture Center for Nutrition Policy and Promotions: Alexandria, VA, 2009 [Google Scholar]
- 7.Hiza HA, Casavale KO, Guenther PM, et al. . Diet quality of americans differs by age, sex, race/ethnicity, income, and education level. J Acad Nutr Diet 2013;113:297–306 [DOI] [PubMed] [Google Scholar]
- 8.Gillman MW, Rifas-Shiman SL, Frazier AL, et al. . Family dinner and diet quality among older children and adolescents. Arch Fam Med 2000;9:235–240 [DOI] [PubMed] [Google Scholar]
- 9.Neumark-Sztainer D, Wall M, Perry C, et al. . Correlates of fruit and vegetable intake among adolescents—Findings from Project EAT. Prev Med 2003;37:198–208 [DOI] [PubMed] [Google Scholar]
- 10.Larson NI, Neumark-Sztainer D, Hannan PJ, et al. . Family meals during adolescence are associated with higher diet quality and healthful meal patterns during young adulthood. J Acad Nutr Diet 2007;107:1502–1510 [DOI] [PubMed] [Google Scholar]
- 11.Hendrie GA, Coveney J, Cox DN. Defining the complexity of childhood obesity and related behaviours within the family environment using structural equation modelling. Public Health Nutr 2012;15:48–57 [DOI] [PubMed] [Google Scholar]
- 12.Kuczmarski RJ, Ogden CL, Guo SS, et al. . 2000 CDC growth charts for the United States: Methods and development. Vital Health Stat 11 2002;(246):1–190 [PubMed] [Google Scholar]
- 13.Block G, Thompson FE, Hartman AM, et al. . Comparison of two dietary questionnaires validated against multiple dietary records collected during a 1-year period. J Acad Nutr Diet 1992;92:686–693 [PubMed] [Google Scholar]
- 14.Cullen KW, Watson K, Zakeri I. Relative reliability and validity of the Block Kids Questionnaire among youth aged 10 to 17 years. J Acad Nutr Diet 2008;108:862–866 [DOI] [PubMed] [Google Scholar]
- 15.Guenther PM, Casavale KO, Reedy J, et al. . Update of the Healthy Eating Index: HEI-2010. J Acad Nutr Diet 2013;113:569–580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.US Department of Agriculture, Center for Nutrition Policy and Promotion. Healthy Eating Index 2010 support files-2007-2008. Available at www.cnpp.usda.gov/HealthyEatingIndexSupportFiles0708.htm Last accessed July21, 2014
- 17.Bronfenbrenner U. Ecology of the family as a context for human development: Research perspectives. Dev Psychol 1986;22:723–742 [Google Scholar]
- 18.Hanson NI, Neumark-Sztainer D, Eisenberg ME, et al. . Associations between parental report of the home food environment and adolescent intakes of fruits, vegetables and dairy foods. Public Health Nutr 2005;8:77–85 [DOI] [PubMed] [Google Scholar]
- 19.Gattshall ML, Shoup JA, Marshall JA, et al. . Validation of a survey instrument to assess home environments for physical activity and healthy eating in overweight children. Int J Behav Nutr Phys Act 2008;5:1–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bauer KW, Neumark-Sztainer D, Fulkerson JA, et al. . Familial correlates of adolescent girls' physical activity, television use, dietary intake, weight, and body composition. Int J Behav Nutr Phys Act 2011;8:1–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Grimm GC, Harnack L, Story M. Factors associated with soft drink consumption in school-aged children. J Acad Nutr Diet 2004;104:1244–1249 [DOI] [PubMed] [Google Scholar]
- 22.Fisher JO, Mitchell DC, Smiciklas-Wright H, et al. . Parental influences on young girls' fruit and vegetable, micronutrient, and fat intakes. J Acad Nutr Diet 2002;102:58–64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Arcan C, Neumark-Sztainer D, Hannan P, et al. . Parental eating behaviours, home food environment and adolescent intakes of fruits, vegetables and dairy foods: Longitudinal findings from Project EAT. Public Health Nutr 2007;10:1257–1265 [DOI] [PubMed] [Google Scholar]
- 24.Acharya K, Feese M, Franklin F, et al. . Body mass index and dietary intake among Head Start children and caregivers. J Acad Nutr Diet 2011;111:1314–1321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Eisenberg CM, Ayala GX, Crespo NC, et al. . Examining multiple parenting behaviors on young children's dietary fat consumption. J Nutr Edu Behav 2012;44:302–309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Feldman S, Eisenberg ME, Neumark-Sztainer D, et al. . Associations between watching TV during family meals and dietary intake among adolescents. J Nutr Educ Behav 2007;39:257–263 [DOI] [PubMed] [Google Scholar]
- 27.Andaya AA, Arredondo EM, Alcaraz JE, et al. . The association between family meals, TV viewing during meals, and fruit, vegetables, soda, and chips intake among Latino children. J Nutr Educ Behav 2011;43:308–315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sisson SB, Shay CM, Broyles ST, et al. . Television-viewing time and dietary quality among US children and adults. Am J Prev Med 2012;43:196–200 [DOI] [PubMed] [Google Scholar]
- 29.Wilson TA, Adolph AL, Butte NF. Nutrient adequacy and diet quality in non-overweight and overweight Hispanic children of low socioeconomic status: The Viva la Familia Study. J Acad Nutr Diet 2009;109:1012–1021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hendrie GA, Coveney J, Cox DN. Defining the complexity of childhood obesity and related behaviours within the family environment using structural equation modelling. Public Health Nutr 2012;15:48–57 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.