Abstract
Background: Identifying factors associated with effective treatment for childhood obesity is important to improving weight loss outcomes. The current study investigated whether child or parent motivation throughout the course of treatment predicted reductions in BMI.
Methods: Fifty 8- to 12-year-old children with overweight and obesity (BMI percentiles 85–98%) and their parents participated in a guided self-help weight loss program, which included 12 brief sessions across 5 months. Parents and interventionists reported on child and parent motivation level at each session. Multilevel slopes-as-outcome models were used to examine growth trajectories for both child and parent BMI across sessions.
Results: Greater interventionist-rated child motivation predicted greater reductions in child BMI; parent motivation did not. However, interventionist-rated parent motivation predicted greater reductions in parent BMI, and its impact on BMI became more pronounced over the course of treatment, such that sustained motivation was more important than initial motivation. Children who were older, Latino, or who had lower initial BMIs had slower reductions in BMI.
Conclusions: This study suggests that motivation may be an important predictor of reduced BMI in child obesity treatment, with sustained motivation being more important than initial motivation. In particular, interventionist-rated, but not parent-rated, motivation is a robust predictor of child and parent BMI outcomes. Future research may evaluate whether motivational interventions can enhance outcome, with particular attention to improving outcomes for Latino children.
Introduction
Pediatric overweight and obesity are prevalent in the United States, affecting approximately one third of children.1 Though effective treatments for childhood obesity have been identified,2 there is significant variability in outcome and a paucity of research about predictors of outcome with mixed findings.3 For example, greater parent and child baseline BMI are sometimes associated with poorer child weight loss outcomes,4 but sometimes not.5 Psychosocial and family sociodemographic factors are also inconsistent predictors of attrition and weight outcomes.6–9 Although early treatment response is consistently associated with better outcomes,6,10 baseline factors associated with positive early treatment response are not well understood.
Motivation may be important in influencing weight outcomes because it consistently predicts weight loss in adults.11 Initial motivation in adults is associated with better eating regulation12 and greater weight loss,13 whereas sustained motivation predicts exercise behavior and weight loss in the long term.14 Motivation to exercise is also associated with weight loss15 and maintenance in adults,16,17 as well as exercise behavior in adolescents.18 However, only two studies have evaluated the role of motivation in weight loss among children. In the first study, analysis of interview and focus group data revealed that children receiving treatment for obesity identified sustained motivation as important in long-term weight loss.19 In the second study, parent confidence (one aspect of motivation) was found to predict treatment completion and child weight loss in a family-based weight control program.10 Though these findings are promising, more research on the role of parent and child motivation in pediatric weight loss is needed, particularly because parent and child motivation appear to be an important factor in the management of other childhood conditions.20,21 Further, motivational interventions appear to be effective across other health-related child behaviors.22
This study examined child and parent motivation as predictors of reduced BMI in children and parents with overweight and obesity who participated in a guided self-help treatment for childhood obesity. High parent motivation was hypothesized to more strongly predict subsequent reduced child BMI than child motivation, given the importance of parent behaviors in supporting positive dietary and physical activity changes in children. Further, parent ratings of motivation were hypothesized to more strongly predict subsequent reduced BMI than interventionist ratings, given that motivation may not always be readily observable. Motivation earlier in treatment was also expected to more strongly predict BMI change because of its hypothesized relation to early treatment engagement, compared to motivation later in treatment.
Methods
Participants
Fifty children with overweight and obesity and their parents enrolled in a guided self-help weight loss program. Eligibility criteria included child age between 8 and 12 years and child BMI (adjusted for age and sex) between the 85th and 98th percentiles. Children with a BMI at or above the 99th percentile were excluded. Families were also excluded if either the child or parent had a psychiatric diagnosis, was receiving psychological or weight-loss treatment, was using medications that affect appetite or weight, or did not speak English. Additional details about the treatment, study design, and main outcomes have been previously reported.23
Guided self-help for pediatric obesity
The guided self-help for pediatric obesity intervention is described in full elsewhere.23 Briefly, this intervention consisted of 12 visits delivered over 20 weeks by nine clinical psychology doctoral trainees. Visits were 20 minutes in length, with the exception of one 60-minute session addressing dietary recommendations. Visits were focused on monitoring child and parent weight, reviewing self-monitoring booklets (food intake and physical activity), and problem-solving barriers to implementing program recommendations. Although children were present for all sessions, this treatment targeted parents as the primary agents of change.24–26
Measures
Body mass index
Child and parent body weight were measured at each session in duplicate on a Tanita Digital Scale (model WB-110A; Tanita, Arlington, IL); the average of the two values was used in analyses. Height was measured in duplicate using a portable Schorr height board (Schorr Inc, Olney, MD); measurements were taken at baseline and every six sessions for child height. BMI (kg/m2) was used as the outcome in this study because of its sensitivity to change across degrees of adiposity and its relative stability in assessing child adiposity change compared to BMI-z and BMI percentile.27 Additionally, BMI change is most highly correlated with dual-energy X-ray absorptiometry measurements of change over time in children.28 Although BMI z-score is optimal for assessing adiposity on a single occasion, it is not necessarily ideal for measuring change in adiposity because within-child variability over time depends on the child's initial level of adiposity.
Motivation
Before the start of each session, parents rated their own motivation (i.e., “How motivated are you to continue the program?”) and their child's motivation (i.e., “How motivated is your child to continue the program?”) from 1 (not at all motivated) to 5 (very motivated). This two-item questionnaire was developed to quickly and feasibly assess motivation before the start of each session; it was pilot tested, but not validated, before use in this study. Interventionists also rated both parent and child motivation using the same metric. Children did not report on motivation because of our previous experience with their high social desirability in this age range.
Statistical Analyses
PASW Statistics 18 (IBM Corp., Armonk, NY) was used to calculate sample descriptives and the mean change in outcomes over time. t-tests and Pearson's correlations were used to examine differences in motivation by treatment drop-out status, as well as baseline demographic characteristics. Given the nested data structure (i.e., time nested within families and families nested within interventionists), SuperMix (Version 1.1; Scientific Software International, Skokie, IL) was used to examine slopes-as-outcome models that modeled growth trajectories for child and parent BMI, accounting for baseline BMI.29 These models appropriately examine multilevel data and can accommodate missing data. The estimate of greatest interest in these models is the slope coefficient, representing an interaction of the predictor (levels 2 or 3) with time (level 1). Time was coded such that the intercept estimate reflects the estimated BMI at the end of treatment, whereas the slope coefficient represents the average change in BMI per session.
As a first step, intraclass correlations (ICCs) were calculated for both outcomes to assess variability attributable to the interventionist and family levels. As a second step, bivariate associations between potential covariates and outcome variables were tested. Potential covariates included main effects and interaction terms (with time) for child and parent age, gender, race (white vs. nonwhite), and ethnicity (Latino vs. non-Latino), controlling for baseline BMI. The main effect of change in parent BMI, entered as a time-varying covariate, was also examined in the child BMI model. Covariates that were associated with the BMI outcomes at p<0.10 were then placed into a multivariate regression model with all predictors of interest (i.e., motivation ratings entered as time-varying covariates) to identify a parsimonious set of predictors. As suggested by Raudenbush and Bryk,30 any nonsignificant variables from this model were removed for statistical efficiency within the multilevel modeling context and a final parsimonious multivariate model was then run for each outcome. For variables that were significantly predictive of slope, values 1 standard deviation (SD) above and below the mean were entered individually into the multivariate model to determine the direction of the effect.
Results
Sample characteristics for participating families are presented in Table 1, including 50 children and 48 parents as two sets of sibling children enrolled in this program. Of the initial 50 child-parent pairs, six (12%) dropped out of treatment (i.e., attended fewer than six sessions). Within reporter (i.e., parent or interventionist), early parent and child motivation (averaged across first five sessions) did not differ between families who dropped out of treatment and those who completed treatment (ps>0.10). Weight outcomes were available for 92% of child and parent participants at session 4 (n=47 and n=46, respectively), 86% at session 8 (both ns=43), and 78% at session 12 (n=39 and n=40, respectively). Over 12 sessions, parents provided an average of 10.58 (SD=2.82) and 10.56 (SD=2.81) ratings of self-motivation and child motivation, respectively. Therapists provided an average of 10.62 (SD=2.94) and 10.65 (SD=2.91) ratings of parent motivation and child motivation, respectively.
Table 1.
Participant Characteristics at Baseline
| Characteristics at entry into treatment | n | Mean (SD) or % | Range |
|---|---|---|---|
| Child characteristics | |||
| Age | 50 | 10.9 (1.3) | 8.0, 12.8 |
| Gender (female) | 31 | 62.0 | |
| Latino/Hispanic ethnicity | 10 | 20.0 | |
| Race | |||
| White | 34 | 68.0 | |
| Asian | 3 | 6.0 | |
| Black | 3 | 6.0 | |
| Mixed race | 10 | 20.0 | |
| White/Asian | 5 | 10.0 | |
| Black/Asian | 2 | 4.0 | |
| White/Black | 2 | 4.0 | |
| White/Native Hawaiian | 1 | 2.0 | |
| BMI | 50 | 24.6 (2.7) | 19.6, 31.5 |
| BMI percentile | 50 | 95.1 (2.9) | 85, 98 |
| Motivation (parent rated) | 49 | 3.9 (0.9) | 2, 5 |
| Motivation (interventionist rated) | 49 | 3.6 (1.1) | 2, 5 |
| Caregiver characteristics | |||
| Age | 48 | 43.8 (5.4) | 30, 54 |
| Gender (female) | 40 | 83.3 | |
| Latino/Hispanic ethnicity | 8 | 16.7 | |
| Race | |||
| White | 38 | 79.2 | |
| Asian | 5 | 10.4 | |
| Black | 2 | 4.2 | |
| Mixed race | 3 | 6.3 | |
| White/Asian | 2 | 4.2 | |
| Black/Asian | 1 | 2.1 | |
| BMI | 48 | 28.0 (6.3) | 19.7, 47.4 |
| Motivation (self-rated) | 47 | 4.5 (0.7) | 3, 5 |
| Motivation (interventionist rated) | 47 | 4.5 (0.7) | 3, 5 |
SD, standard deviation.
Factors Associated with Early Motivation
Early parent-reported self- and child motivation were moderately correlated with one another (r=0.31; p=0.029), confirming that the two are related, but unique, constructs. Early motivation (parent and child) did not differ significantly on child or parent race, ethnicity, age, or by child BMI (ps>0.10). Parent motivation was not significantly related to parent BMI (ps>0.10), but child motivation was moderately and positively correlated with parent BMI (r=0.35; p=0.013), such that parents with higher BMIs perceived their children to be more motivated than children of parents with lower BMIs.
Child Body Mass Index
Only family level (ICC=0.987) was accounted for in this model given the low ICC for interventionist level (ICC=0.002). Child BMI at the start of treatment did not differ by initial level of parent or child motivation level (rs=−0.06, 0.01; ps>0.10). In the unconditional growth model (with time as the only predictor), child BMI decreased significantly over the course of the intervention (B=−0.080; standard error [SE]=0.033; p=0.014). Child gender, race, and change in parent BMI were not predictive of change in child BMI in bivariate associations (ps>0.10). Therefore, the initial multivariate child BMI model included baseline child BMI, child age, child ethnicity, and parent- and interventionist-reported parent and child motivation. All motivation variables, with the exception of interventionist-rated child motivation, were removed from the final model because of nonsignificance (ps>0.10).
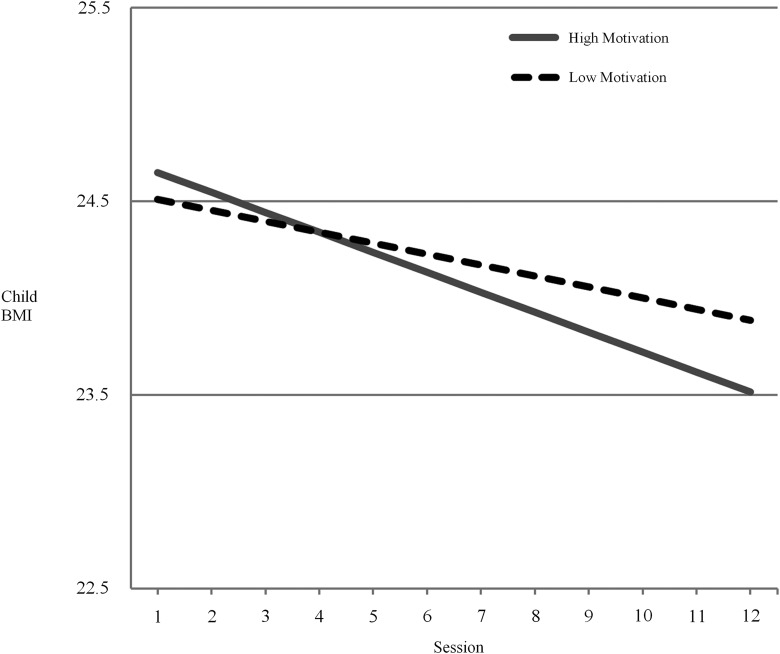
The final multivariate model yielded an estimated decrease of 0.08 BMI points per session for non-Latino children of average age (11 years) with an average BMI at baseline (24.6) and average overall motivation, as rated by their interventionist (B=−0.080; SE=0.013; p<0.001; Table 2). Interventionist-rated child motivation remained significantly predictive of BMI change (B=−0.159; SE=0.032; p<0.001), and the effect of motivation on BMI became more pronounced across time (B=−0.020; SE=0.004; p<0.001). Faster reductions in child BMI were predicted by greater initial BMI (B=−0.020; SE=0.006; p<0.001), younger age (B=0.031; SE=0.011; p=0.006), and non-Latinos ethnicity (B=0.088; SE=0.033; p=0.007). Follow-up analyses showed that rate of decline in child BMI was steeper for children with higher interventionist-rated motivation, compared to those with lower motivation (Fig. 1).
Table 2.
Multivariate Growth Model Predicting Child BMIa
| Parameter | B | SE | p value |
|---|---|---|---|
| Intercept | 23.699 | 0.133 | <0.001 |
| Slope | −0.080 | 0.013 | <0.001 |
| Initial child BMI | 0.782 | 0.057 | <0.001 |
| Initial child BMI* | −0.020 | 0.006 | <0.001 |
| Child motivation (interventionist rated) | −0.159 | 0.032 | <0.001 |
| Child motivation (interventionist rated)* | −0.020 | 0.004 | <0.001 |
| Latino ethnicity | 0.988 | 0.326 | 0.002 |
| Latino ethnicity- | 0.088 | 0.033 | 0.007 |
| Age | 0.298 | 0.114 | 0.009 |
| Age* | 0.031 | 0.011 | 0.006 |
Variables with an asterisk (*) indicate a variable by time interaction (i.e., slope). Non-Latino ethnicity was coded as 0.
SE, standard error.
Figure 1.
Interventionist ratings of child motivation predicting rate of change in child BMI. This graph depicts BMI slopes for children with high and low interventionist-rated motivation (i.e., motivation 1 SD above or below the mean) as a follow-up analysis to the significant motivation by time interaction term.
Parent Body Mass Index
Only family level (ICC=0.998) was accounted for in this model given the negative ICC for interventionist level (ICC=−0.014). Parent BMI at the start of treatment did not differ by initial level of self- or interventionist-rated motivation (rs=−0.08, −0.07; ps>0.10). In the unconditional growth model, parent BMI decreased significantly over the course of the intervention (B=−0.069; SE=0.013; p<0.001). Parent age, race, and ethnicity did not significantly predict change in parent BMI in bivariate associations (ps>0.10). Therefore, the initial multivariate model included baseline parent BMI, self- and interventionist-reported parent motivation, and parent gender.
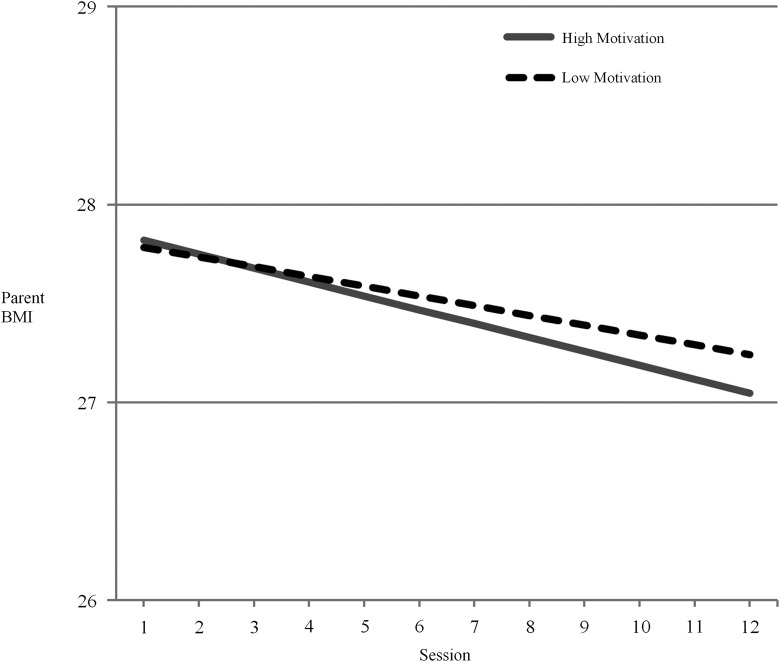
All predictors were retained in the final model, which yielded an estimated decrease of 0.059 BMI points per session for mothers who had an average BMI at baseline (28.0) and average overall motivation, as rated by both themselves and their interventionist (B=−0.059; SE=0.018; p<0.001; Table 3). Faster reductions in parent BMI were predicted by male gender (B=−0.088; SE=0.038; p=0.019), but not initial BMI (B=−0.006; SE=0.003; p=0.107). The impact of self-rated parent motivation on BMI change was only significant at the trend level (B=−0.085; SE=0.045; p=0.056), but did become significantly more pronounced over time (B=−0.014; SE=0.007; p=0.048). Follow-up analyses showed that rate of decline in parent BMI was steeper for parents with higher self-rated motivation, compared to those with lower motivation. Interventionist-rated parent motivation was also significantly associated with change in BMI (B=−0.105; SE=0.034; p=0.002), and this effect became more pronounced across time (B=−0.012; SE=0.005; p=0.023). Follow-up analyses showed that rate of decline in parent BMI was steeper for parents with higher interventionist-rated motivation, compared to those with lower motivation (Fig. 2).
Table 3.
Multivariate Growth Model Predicting Parent BMIa
| Parameter | B | SE | p value |
|---|---|---|---|
| Intercept | 27.150 | 0.151 | <0.001 |
| Slope | −0.059 | 0.018 | <0.001 |
| Parent motivation (interventionist rated) | −0.105 | 0.034 | 0.002 |
| Parent motivation (interventionist rated)* | −0.012 | 0.005 | 0.023 |
| Parent motivation (self-rated) | −0.085 | 0.045 | 0.056 |
| Parent motivation (self-rated)* | −0.014 | 0.007 | 0.048 |
| Gender | −0.903 | 0.256 | <0.001 |
| Gender* | −0.088 | 0.038 | 0.019 |
Variables with an asterisk (*) indicate a variable by time interaction (i.e., slope). Female gender was coded as 0.
SE, standard error.
Figure 2.
Interventionist ratings of parent motivation predicting rate of change in parent BMI. This graph depicts BMI slopes for parents with high and low interventionist-rated motivation (i.e., motivation 1 SD above or below the mean) as a follow-up analysis to the significant motivation by time interaction term.
Discussion
This study found that interventionist-rated motivation to participate in a pediatric obesity treatment program predicted greater reductions in child and parent BMI. Contrary to expectations, motivation later in treatment had a greater impact on BMI reductions than motivation earlier in treatment, suggesting that sustained motivation is more potent than initial motivation. Our finding that parent-reported motivation was not a predictor of reductions in BMI was surprising given that parents were ultimately responsible for implementing program recommendations at home. Nevertheless, self-reported parent motivation had a trend-level impact on parent BMI reduction, and sustained parent motivation significantly predicted reduced parent BMI more than initial motivation. In parallel with the interventionist-rated motivation findings, these results suggest that interventions designed to increase motivation are more likely to be effective when delivered toward the middle or end of treatment. Further, this pattern of results suggests that interventionists may be able to effectively identify—based on motivation—families who may be at risk for poorer weight loss outcomes.
This study also found that greater initial child BMI, younger age, and non-Latino ethnicity predicted greater reductions in child BMI. The age effect may be the result of relatively lower parental control over older children's food consumption and physical activity; alternatively, engaging older children in a guided self-help program with relatively minimal contact may be more difficult than engaging younger children. Our finding that BMI reductions were smaller for children from Latino, compared to non-Latino white, backgrounds suggests that future research on self-help programs should more carefully consider cultural factors and availability of written program materials in Spanish, when appropriate. This is especially true given the disproportionate rates of obesity in older children from Latino, compared to non-Latino white, backgrounds.1 Finally, although greater BMI reductions in children with higher initial BMIs may be accounted for, in part, by regression to the mean, future research is needed to improve outcomes across levels of overweight. Interestingly, this study also found that child BMI reductions did not parallel those of parents, suggesting that children may play a more critical role in their own weight behaviors in guided self-help interventions, despite the fact that parents are responsible for implementing and modeling the majority of behaviors in this behavioral weight loss program (e.g., grocery shopping, meal preparation, and creating opportunities for physical activity).
Motivational interviewing appears to be a feasible, promising adjunct to treatment for pediatric obesity,31,32 and it has been associated with increased physical activity33 and improved weight loss in adults.33–35 Findings from the current study provide additional evidence for the importance of targeting motivation within the context of weight loss interventions and extend this literature by suggesting that motivation may be a more critical target in the later—compared to the earlier—stages of treatment. Therefore, incorporating motivational techniques toward the end of treatment may potentially enhance weight loss outcomes, particularly for families who are perceived by interventionists as less motivated. Given poor long-term weight loss maintenance outcomes,36 “motivation maintenance” subsequent to initial weight loss interventions may be important. Future research might examine the impact of brief, sequential interventions delivered post-treatment to sustain high motivation on long-term weight loss maintenance.
This study has both strengths and limitations. The use of repeated measures of motivation and weight allowed for examination of session-by-session growth trajectories in child and parent BMI through multilevel slopes-as-outcomes analytic models. In addition, its examination of an efficacious treatment in the context of guided self-help may help to increase the dissemination and feasibility of this treatment. Nevertheless, this sample was predominantly non-Hispanic whites who received guided self-help in a university setting, so findings may not generalize to more racially diverse families, usual care settings, or more traditional (i.e., non-self-help) treatments. In addition, these treatment-seeking families were likely more motivated than non-treatment-seeking families. Additionally, motivation was only assessed for families who attended sessions, which impeded a broader examination of how motivation impacts BMI reduction outside the context of an intervention. Further, questions assessing motivation were pilot tested, but not validated, before conducting the current study. Though the use of a one-item measure may be more feasible within a clinical context, future research should seek to develop and utilize measures that capture the multidimensional nature of motivation. A ceiling effect for parent motivation was also observed, which likely reflects that families in the current sample were treatment seeking. Assessment of motivation to participate in interventions that are less self-selecting and are more globally targeted (e.g., schools and primary care offices) would provide a greater understanding of how variability in initial motivation impacts treatment engagement and outcome. Finally, given that school-aged children have more control over their diet and activity habits, it will also be important for future studies to examine child self-reported motivation.
Conclusion
This study suggests that interventionist-rated, but not parent-rated, motivation is a robust predictor of child and parent BMI outcomes for families engaging in a weight loss program. Although clinicians may not be able to rely on parent-reported motivation as a predictor of treatment success, their own assessment of family motivation may have some clinical utility. Examination of mediators will be important to better understand the motivation-outcome relationship. Despite several limitations and the need for replication, this study is one of the first to examine the role of family motivation in a guided self-help weight loss intervention, which may be particularly important in the context of a relatively brief, minimally structured intervention that requires a high level of family independence and initiative. As a potentially modifiable factor that is not yet well understood, motivation—particularly toward the end or follow-up phases of treatment—may prove important. Finally, cultural adaptations may be necessary to improve outcomes for Latino children.
Acknowledgments
This research was supported by the National Institutes of Health (DK080266; to K.N.B.), the National Institute of Diabetes and Digestive and Kidney Diseases (P30 DK050456; to S.J.C.), and the National Institute of Mental Health (T32 MH082761; to E.C.A. and S.J.C.). clinicaltrials.gov identifier: NCT01145833. The authors acknowledge Hanaah Fannin for her assistance with data collection as well as all of the participating families.
Author Disclosure Statement
Scott Crow receives funding from Shire. No competing financial interests exist for any of the other authors.
References
- 1.Ogden CL, Carroll MD, Kit BK, et al. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 2014;311:806–814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Epstein LH, Paluch RA, Roemmich JN, et al. Family-based obesity treatment, then and now: Twenty-five years of pediatric obesity treatment. Health Psychol 2007;26:381–391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Waters E, de Silva-Sanigorski A, Hall BJ, et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev 2011;12:CD001871. [DOI] [PubMed] [Google Scholar]
- 4.Eliakim A, Friedland O, Kowen G, et al. Parental obesity and higher pre-intervention BMI reduce the likelihood of a multidisciplinary childhood obesity program to succeed—A clinical observation. J Pediatr Endocrinol Metab 2004;17:1055–1061 [DOI] [PubMed] [Google Scholar]
- 5.Wrotniak BH, Epstein LH, Paluch RA, et al. Parent weight change as a predictor of child weight change in family-based behavioral obesity treatment. Arch Pediatr Adolesc Med 2004;158:342–347 [DOI] [PubMed] [Google Scholar]
- 6.Jelalian E, Hart CN, Mehlenbeck RS, et al. Predictors of attrition and weight loss in an adolescent weight control program. Obesity 2008;16:1318–1323 [DOI] [PubMed] [Google Scholar]
- 7.Zeller M, Kirk S, Claytor R, et al. Predictors of attrition from a pediatric weight management program. J Pediatr 2004;144:466–470 [DOI] [PubMed] [Google Scholar]
- 8.Levine MD, Ringham RM, Kalarchian MA, et al. Is family‐based behavioral weight control appropriate for severe pediatric obesity? Int J Eat Disord 2001;30:318–328 [DOI] [PubMed] [Google Scholar]
- 9.Skelton JA, Goff DC, Ip E, et al. Attrition in a multidisciplinary pediatric weight management clinic. Child Obes 2011;7:185–193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gunnarsdottir T, Njardvik U, Olafsdottir AS, et al. The role of parental motivation in family-based treatment for childhood obesity. Obesity 2011;19:1654–1662 [DOI] [PubMed] [Google Scholar]
- 11.Teixeira PJ, Going SB, Sardinha LB, et al. A review of psychosocial pre-treatment predictors of weight control. Obes Rev 2005;6:43–65 [DOI] [PubMed] [Google Scholar]
- 12.Mata J, Silva MN, Vieira PN, et al. Motivational “spill-over” during weight control: Increased self-determination and exercise intrinsic motivation predict eating self-regulation. Health Psychol 2009;28:709–716 [DOI] [PubMed] [Google Scholar]
- 13.Teixeira PJ, Palmeira AL, Branco TL, et al. Who will lose weight? A reexamination of predictors of weight loss in women. Int J Behav Nutr Phys Act 2004;1:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Williams GC, Grow VM, Freedman ZR, et al. Motivational predictors of weight loss and weight-loss maintenance. J Pers Soc Psychol 1996;70:115–126 [DOI] [PubMed] [Google Scholar]
- 15.Palmeira AL, Teixeira PJ, Branco TL, et al. Predicting short-term weight loss using four leading health behavior change theories. Int J Behav Nutr Phys Act 2007;4:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Silva MN, Markland D, Carraça EV, et al. Exercise autonomous motivation predicts 3-yr weight loss in women. Med Sci Sports Exerc 2011;43:728–737 [DOI] [PubMed] [Google Scholar]
- 17.Teixeira PJ, Silva MN, Coutinho SR, et al. Mediators of weight loss and weight loss maintenance in middle-aged women. Obesity 2010;18:725–735 [DOI] [PubMed] [Google Scholar]
- 18.Gillison FB, Standage M, Skevington SM. Relationships among adolescents' weight perceptions, exercise goals, exercise motivation, quality of life and leisure-time exercise behaviour: A self-determination theory approach. Health Educ Res 2006;21:836–847 [DOI] [PubMed] [Google Scholar]
- 19.Murtagh J, Dixey R, Rudolf M. A qualitative investigation into the levers and barriers to weight loss in children: Opinions of obese children. Arch Dis Child 2006;91:920–923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Channon SJ, Huws-Thomas MV, Rollnick S, et al. A multicenter randomized controlled trial of motivational interviewing in teenagers with diabetes. Diabetes Care 2007;30:1390–1395 [DOI] [PubMed] [Google Scholar]
- 21.Ellis DA, Berio H, Carcone AI, et al. Adolescent and parent motivation for change affects psychotherapy outcomes among youth with poorly controlled diabetes. Journal Pediatr Psychol 2012;37:75–84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Suarez M, Mullins S. Motivational interviewing and pediatric health behavior interventions. J Dev Behav Pediatr 2008;29:417–428 [DOI] [PubMed] [Google Scholar]
- 23.Boutelle KN, Norman GJ, Rock CL, et al. Guided self-help for the treatment of pediatric obesity. Pediatrics 2013;131:e1435–e1442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Epstein LH, Wing RR, Koeske R, et al. Child and parent weight loss in family-based behavior modification programs. J Consult Clin Psychol 1981;49:674–685 [DOI] [PubMed] [Google Scholar]
- 25.Boutelle KN, Cafri G, Crow SJ. Parent‐only treatment for childhood obesity: A randomized controlled trial. Obesity 2011;19:574–580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Janicke DM, Sallinen BJ, Perri MG, et al. Comparison of parent-only vs family-based interventions for overweight children in underserved rural settings: Outcomes from project STORY. Arch Pediatr Adolesc Med 2008;162:1119–1125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cole TJ, Faith MS, Pietrobelli A, et al. What is the best measure of adiposity change in growing children: BMI, BMI %, BMI z-score or BMI centile? Eur J Clin Nutr 2005;59:419–425 [DOI] [PubMed] [Google Scholar]
- 28.Kakinami L, Henderson M, Chiolero A, et al. Identifying the best body mass index metric to assess adiposity change in children. Arch Dis Child 2014May19 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hedeker D, Gibbons RD, Du Toit SHC, et al. SuperMix: A Program for Mixed-Effects Regression Models. Scientific Software International: Chicago, IL, 2008 [Google Scholar]
- 30.Raudenbush SW, Bryk AS. Hierarchical Linear Models: Applications and Data Analysis Methods, 2nd ed. Sage: Newbury Park, CA, 2002 [Google Scholar]
- 31.Resnicow K, Davis R, Rollnick S. Motivational interviewing for pediatric obesity: Conceptual issues and evidence review. J Am Diet Assoc 2006;106:2024–2033 [DOI] [PubMed] [Google Scholar]
- 32.Schwartz RP, Hamre R, Dietz WH, et al. Office-based motivational interviewing to prevent childhood obesity. Arch Pediatr Adolesc Med 2007;161:495–501 [DOI] [PubMed] [Google Scholar]
- 33.Hardcastle SJ, Taylor AH, Bailey MP, et al. Effectiveness of a motivational interviewing intervention on weight loss, physical activity and cardiovascular disease risk factors: A randomised controlled trial with a 12-month post-intervention follow-up. Int J Behav Nutr Phys Act 2013;10:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.DiMarco ID, Klein DA, Clark VL, et al. The use of motivational interviewing techniques to enhance the efficacy of guided self-help behavioral weight loss treatment. Eat Behav 2009;10:134–136 [DOI] [PubMed] [Google Scholar]
- 35.McDoniel SO, Wolskee P, Shen J. Treating obesity with a novel hand-held device, computer software program, and internet technology in primary care: The SMART motivational trial. Patient Educ Couns 2010;79:185–191 [DOI] [PubMed] [Google Scholar]
- 36.Kraschnewski JL, Boan J, Esposito J, et al. Long-term weight loss maintenance in the United States. Int J Obes 2010;34:1644–1654 [DOI] [PMC free article] [PubMed] [Google Scholar]