Abstract
Objective
Fertility sparing surgery (FSS) is a strategy often considered in young patients with early epithelial ovarian cancer. We investigated the role and the outcomes of FSS in eEOC patients who underwent comprehensive surgery.
Methods
From January 2003 to January 2011, 24 patients underwent fertility sparing surgery. Eighteen were one-to-one matched and balanced for stage, histologic type and grading with a group of patients who underwent radical comprehensive staging (n=18). Demographics, surgical procedures, morbidities, pathologic findings, recurrence-rate, pregnancy-rate and correlations with disease-free survival were assessed.
Results
A total of 36 patients had a complete surgical staging including lymphadenectomy and were therefore analyzed. Seven patients experienced a recurrence: four (22%) in the fertility sparing surgery group and three (16%) in the control group (p=not significant). Sites of recurrence were: residual ovary (two), abdominal wall and peritoneal carcinomatosis in the fertility sparing surgery group; pelvic (two) and abdominal wall in the control group. Recurrences in the fertility sparing surgery group appeared earlier (mean, 10.3 months) than in radical comprehensive staging group (mean, 53.3 months) p<0.001. Disease-free survival were comparable between the two groups (p=0.422). No deaths were reported. All the patients in fertility sparing surgery group recovered a regular period. Thirteen out of 18 (72.2%) attempted to have a pregnancy. Five (38%) achieved a spontaneous pregnancy with a full term delivery.
Conclusion
Fertility sparing surgery in early epithelial ovarian cancer submitted to a comprehensive surgical staging could be considered safe with oncological results comparable to radical surgery group.
Keywords: Disease-free survival, Fertility, Lymph node excision, Neoplasm recurrence, Ovarian neoplasms, Pregnancy
INTRODUCTION
In early epithelial ovarian cancer (eEOC), 5 year survival ranges from 70% to 100% for stage I and 50% to 95% for stage II. These wide ranges are due to the heterogeneity of the literature data which are based on small series, with different procedures of staging and different postsurgical treatments [1,2,3,4].
The International Federation of Gynecology and Obstetrics (FIGO) surgical stage is the most relevant prognostic factor for disease-free survival (DFS) and overall survival of apparent eEOC patients. A thorough surgical staging is crucial to address appropriate treatment and guarantee optimal survival. Less extensive surgical procedures may fail to detect extraovarian spread of the disease. Several papers reported on the risk of unrecognized occult disease, with a 30% likelihood of upstaging on restaging surgery [5].
Considered the very good prognosis following an adequate surgical staging in eEOC, the fertility sparing surgery (FSS) for women of childbearing age has become an argument of debate in the last decades. Twenty-five percent of EOCs are diagnosed in early-stages. About 14% of those early-stage patients are under the age of 40 at the time of diagnosis. These women are potentially interested in preserving their fertility [6,7,8].
Literature data, even if based on retrospective series, confirm the likelihood to consider conservative surgery for eEOC in young patients [9,10,11]. However, there is still a lack of consensus concerning the selection criteria to deem patients suitable for FSS. Some authors use restrictive criteria, for example FIGO stage IA, grade1, to admit patients to FSS [12], while others consider all stage I EOC patients eligible for conservative treatment [10,11,13].
In a previous retrospective study, we found that FSS in high risk eEOC is feasible and safe in patients undergoing comprehensive surgical staging [14]. In the present study, we aim to investigate oncological and obstetrical outcome of patients submitted to FSS compared to a one to one matched court of patients submitted in the same period to radical comprehensive staging (RCS).
MATERIALS AND METHODS
After obtaining Institutional Review Board approval, data from a prospectively held database on eEOC, were retrospectively analyzed focusing on patients submitted to FSS from January 2003 to January 2011. Inclusion criteria for FSS were the following: woman strongly interested in preserving their fertility aged ≤40 years; adequate counseling (women were informed of the possible risks and benefits of FSS); signed informed consent; accurate comprehensive staging (no gross evidence of disease); and apparently negative spared ovary (macroscopically or at biopsy). Exclusion criteria were: any extrapelvic metastatic disease and tumors of low malignant potential.
Patients were submitted to a laparoscopic or open conservative surgical approach, consisting of unilateral salpingo-oophorectomy and complete peritoneal staging (washing; random multiple peritoneal biopsies; omentectomy) and systematic bilateral pelvic and para-aortic lymphadenectomy with preservation of uterus and one ovary. Surgical technique has been previously described elsewhere and briefly detailed [15].
The para-aortic systematic lymphadenectomy was performed after opening the retroperitoneum as far as the Treitz ligament and along the paracolic gutters, and included the removal of the lympho-fatty tissue located between: the psoas muscle laterally and the inferior vena cava medially as far as the right renal vein (paracaval lymph nodes); the aorta and the cava, from the aortocaval bifurcation as far as the left renal vein (interaortocaval lymph nodes); the aorta and left psoas muscle from aortocaval bifurcation as far as the left renal vein (para-aortic lymph nodes).
The pelvic systematic lymphadenectomy included the removal of the lympho-fatty tissue located: above the external iliac vessels between the iliac bifurcation, the inferior epigastric vessels, and psoas muscle laterally (external iliac lymph nodes); below the external iliac vessel and above the obturator nerve, between the iliac bifurcation, the psoas muscle laterally, the obturator muscle caudally, and the virtual plane passing through the umbilical artery and bladder medially (obturator lymph nodes); above and laterally to the common iliac vessels between the aortocaval bifurcation and the iliac bifurcation (common iliac lymph nodes).
Intraoperative pathological diagnosis was performed after macroscopic examination, and consisted of two to four sections especially from solid areas according to the type and size of the mass. Frozen procedures were performed through cryostat. The sections were 7 to 8 µm in thickness, were stained with hematoxyline-eosin and examined by a dedicated gynecopathologist. Paraffin blocks were then prepared for the final diagnosis from all specimens and examined with standard technique.
Demographic, clinical, surgical, and pathologic characteristics of the patients were assessed. Pathology information included tumor histology, grade, and stage at diagnosis, number of regional lymph nodes examined, as well as documented extension away from the primary site.
Patients deemed to be at increased risk of recurrence (poorly differentiated tumors, stage IB-C, stage >I) were given adjuvant platinum-based treatment. Regular follow-up four times a year in the first year, three times during years 2 and 3 and every 6 months thereafter was scheduled. Recurrences were diagnosed during regular follow-up visit and confirmed on computed tomographic and/or magnetic resonance imaging scans. Whenever possible, histologic or cytologic confirmation was obtained. Menstrual recovery and pregnancy intent or achievement were assessed too. Complications and morbidity were recorded and classified according to CTCAE 4.03 [16].
Patients undergoing FSS were one-to-one matched and balanced for stage, histologic type, and grading with a group of patients undergoing RCS in the same period. Matching was done stepwise, with the exclusion of unmatchable patients, to reduce any possible bias: firstly stage, than histology and finally grading. We did not consider age as a matching factor as there is no consensus in the literature regarding its actual prognostic value [9,11]. Unmatched patients were excluded.
1. Statistical analysis
Pearson chi-square analysis, Fisher exact test, and Mann-Whitney test when needed were calculated, Kaplan-Meier curves were plotted. The difference between survival curves was evaluated with log rank test. A p<0.05 was considered to be significant. SPSS ver. 15.0 (SPSS Inc., Chicago, IL, USA) was used for the analysis.
RESULTS
A total of 24 women underwent FSS for eEOC. Eighteen out of these were one-to-one matched and balanced for stage, histologic type, and grading with a group of patients who underwent RCS.
Characteristics of eligible patients are marked in Table 1. The mean age was 31 and 51 years for FSS and for RCS, respectively. Endometrioid type was the most frequent. In 10 cases the tumor was poorly differentiated. Ten out of 18 patients in the FSS group were FIGO stage ≥IA grade 3. Data on surgical staging procedures and pathological assessment are shown in Table 1. A median of 22 pelvic and 20 para-aortic nodes were removed. No node metastases were found. Globally, the mean hospital stay was 6 days. We detected a synchronous tumor in the endometrium in a patient in the RCS group.
Table 1.
Clinical, surgical, and pathological characteristics of the patients according to the study treatment group
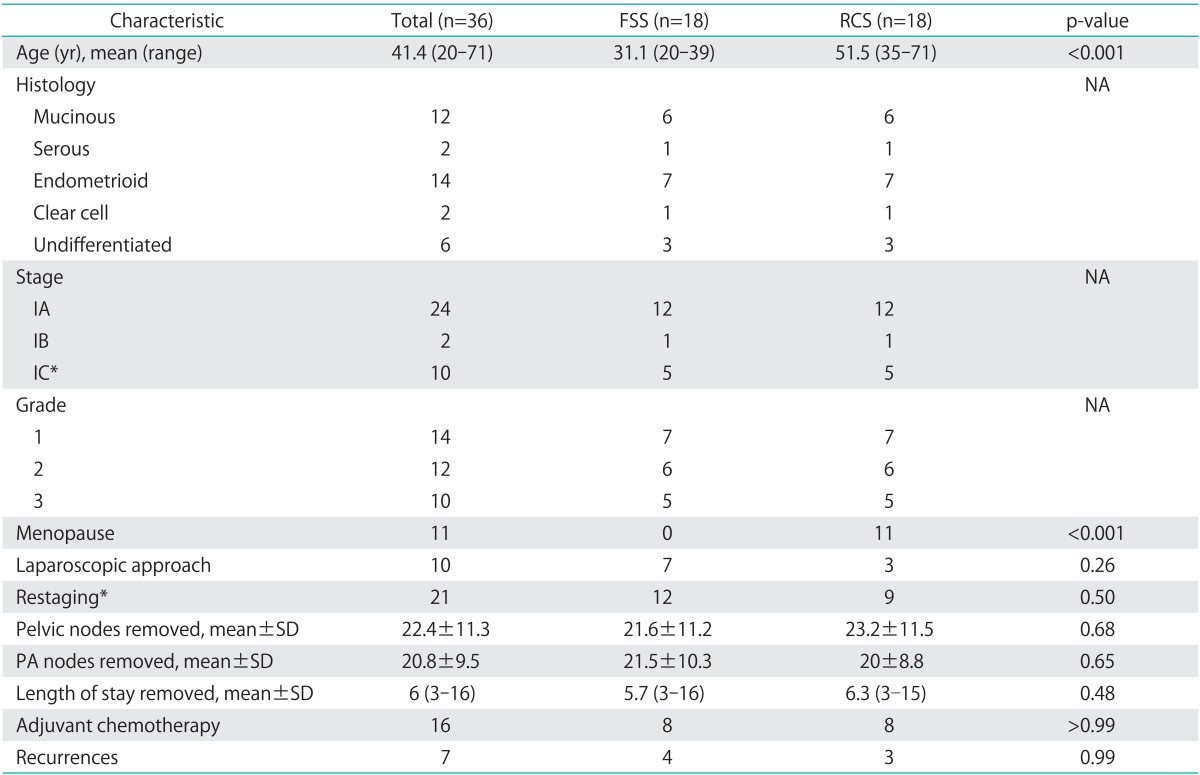
FSS, fertility sparing surgery; NA, not applicable (matching characteristics); PA, para-aortic; RCS, radical comprehensive staging.
*Seven surface invasion, one positive washing, two capsule rupture.
There was one intraoperative vascular injury. In the early postoperative time, two patients suffered of complications: one patient suffered from hemoperitoneum (grade 3) controlled with laparotomy for hemostasis and another required a drainage tube placement for lymphorrea (grade 3). Late postoperative complications were 2: one lymph-cyst formation requiring drainage and one postoperative abdominal hernia. Eight patients per group underwent adjuvant carboplatin AUC 6 +/- paclitaxel 175 mg/mq for 4 to 6 cycles.
Seven patients experienced a recurrence (Table 2): four (22%) in the FSS group and three (16%) in the control group (p=not significant). The recurrence sites were: the residual ovary (two cases), the abdominal wall and peritoneal carcinomatosis, in the FSS group; pelvic (two cases) and abdominal wall in the control group. Recurrences in the FSS group appeared earlier (mean 10.3 months) than in RCS group (mean 53.3 months) (p<0.001).
Table 2.
Characteristics of patients with recurrence
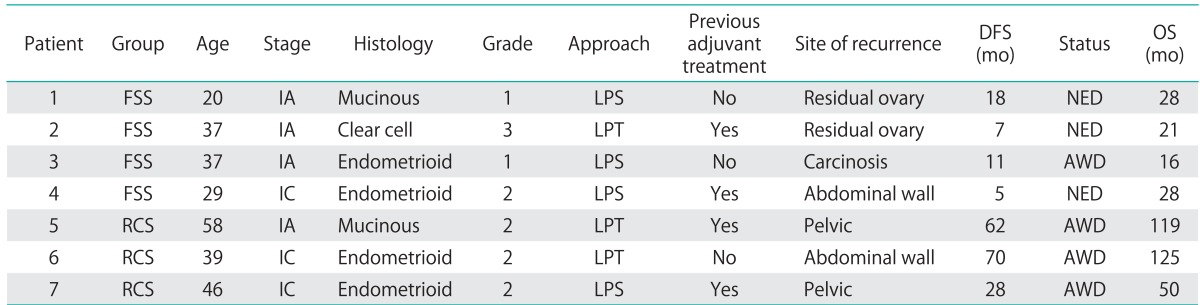
AWD, alive with disease; DFS, disesase free survival; FSS, fertility sparing surgery; LPS, laparoscopy; LPT, laparotomy; NED, no evidence of disease; OS, overall survival; RCS, radical comprehensive staging.
Among FSS patients, recurrences were distributed as follow: two in women with FIGO stage ≥IA grade 3 and 2 in patients with FIGO stage IA grade 1 to 2. The DFS curves did not show any significant difference between the two groups (p=0.422). No deaths were reported. The DFS was not statistically significant (Fig. 1).
Fig. 1.
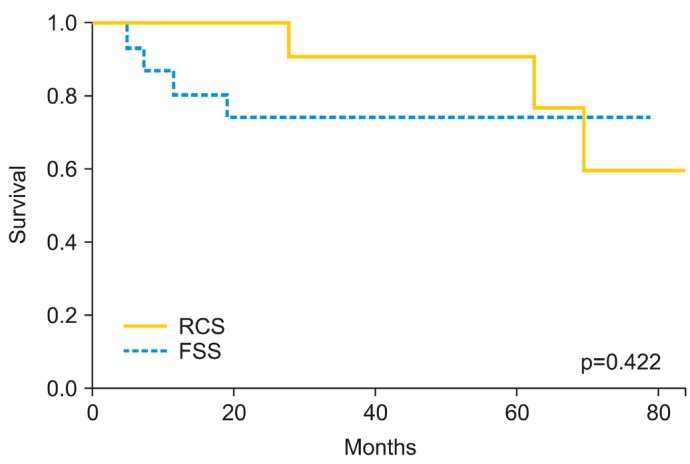
Disesase free survival (DFS) in two groups of patients with early epithelial ovarian cancer undergoing conservative (fertility sparing surgery, FSS) versus radical (radical comprehensive staging, RCS) treatment (Log-rank test, p=0.422; FSS: mean DFS 62.4 months, 95% confidence interval [CI], 48.7 to 76.2; RCS: mean DFS 89.1 months, 95% CI, 71.8 to 106.4).
All the patients in the FSS group returned to regular menses. Thirteen out of 18 (72.2%) attempted to have a pregnancy. Five (38%) achieved a spontaneous pregnancy with full term delivery.
DISCUSSION
FSS is a matter of debate in gynecologic oncology. In spite of the lack of high level of evidence, literature data agree to propose FFS in young patients with FIGO stage IA grade 1 or grade 2 eEOC. More controversial is whether or not to address patients with high risk eEOC (≥IA grade 3) to FSS.
The aim of the present study was to investigate the role of FSS in eEOC in patients who underwent comprehensive surgical staging. The results of the present study showed that FSS is feasible, safe and with a good obstetrical outcome in patients with eEOC after accurate comprehensive staging.
The present study showed that the patients who underwent FSS present a recurrence rate similar to those who underwent RCS. The DFSs are comparable between the two groups. Relapses occurred significantly earlier (10.3 months) in the FSS group compared to the RCS group (53.3 months). In our series, 50% (two out of four) of the relapses occurred in the residual ovary. This kind of relapse has a good possibility of rescue with surgery and chemotherapy, as reported in previous series [11].
Data on obstetrical outcome showed encouraging results with a pregnancy rate (38%) similar to that reported in literature (Table 3) [7,10,11,12,14,17,18,19,20]. All the patients present regular menses regardless of adjuvant chemotherapy. In our series, 13 out of 18 (72.2%) patients attempted to conceive. Since patients undergoing FSS, do not always attempt to conceive, the selection criteria have to be very restrictive and the patients should be thoroughly counseled and highly motivated.
Table 3.
Obstetrical outcome, literature review*
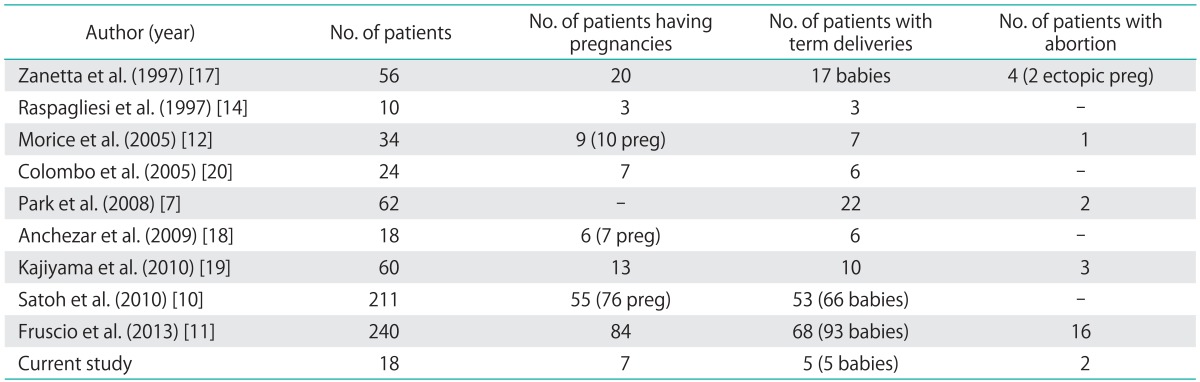
*More recent case series may include previously published data from the same group.
Comprehensive staging is mandatory because an upstaging warrants adjuvant treatments; while a thorough surgical staging could avoid any further medical treatment, according to the ICON-ACTION trial [3].
Literature data are based on heterogeneous series. We subdivided literature data in low-risk patients defined as FIGO stage grade 1 to 2 (Table 4) [7,10,11,12,13,17,18,19,21,20,21,22,23] and high risk patients defined as FIGO stage ≥IA grade 3 (Table 5) [7,10,11,12,13,14,17,18,19,21,22,23]. In the low risk group of 435 cases, the recurrence rate and death rate was 8% (35) and 3.7% (16), respectively. In the high risk group of 364 cases instead, the recurrence rate and death rate was 17.3% (63) and 8% (29), respectively. The recurrence and death rates were markedly different between the two groups.
Table 4.
Low risk group the International Federation of Gynecology and Obstetrics IA G1-2, literature review*
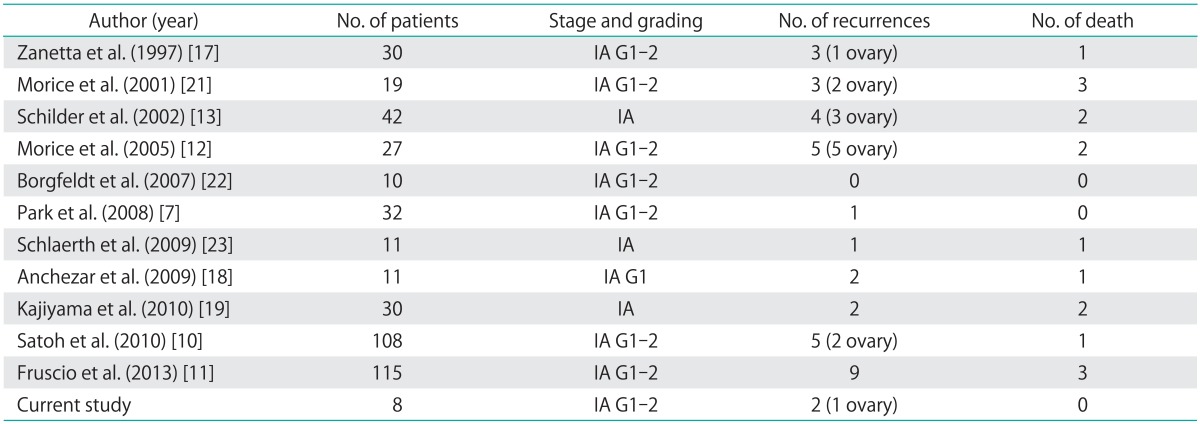
*More recent case series may include previously published data from the same group.
Table 5.
High risk group the International Federation of Gynecology and Obstetrics ≥IA G3, literature review*
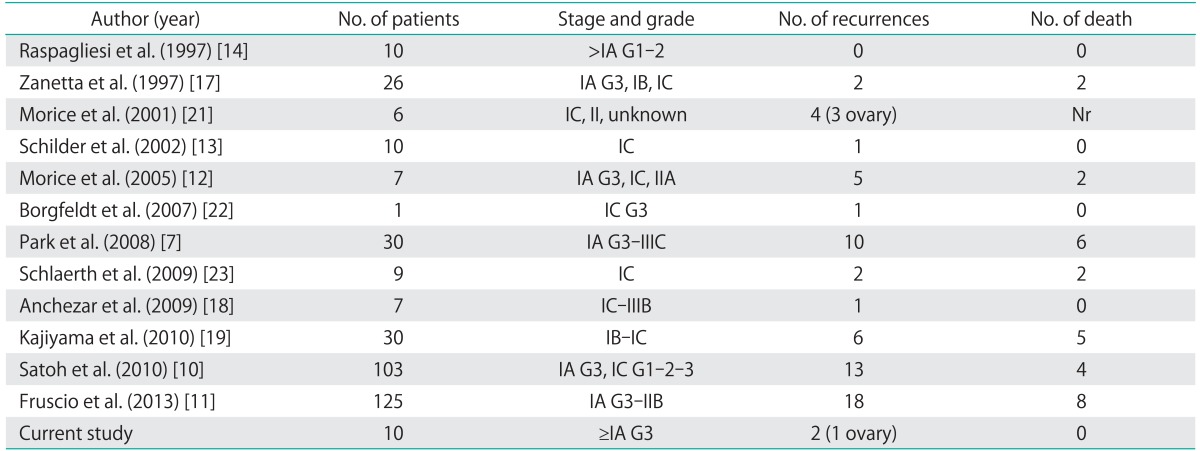
*More recent case series may include previously published data from the same group.
A study has been published by the Japanese Gynecologic Oncology Group [10] on a total of 211 patients (stage IA, n=126; stage IC, n=85) from 30 institutions undergoing FSS. The authors concluded that FSS is a safe treatment for stage IA patients with favorable histology (defined as grade 1 to 2 nonclear cell adenocarcinoma). They also suggested, that stage IA patients with clear cell histology and stage IC patients with favorable histology can be candidates for FSS followed by adjuvant chemotherapy.
Another study based on SEER data [9] evaluated 1,186 women aged ≤50 years with stage IA or IC EOC, of which 754 (64%) underwent radical treatment with bilateral salpingo-oophorectomy, and 432 (36%) underwent FSS. The comparison of data revealed that FSS was safe in young women who had stage IA and IC EOC.
An Italian retrospective study evaluated 240 patients with malignant eEOC treated with FSS. At a median follow-up of 9 years, 27 patients had relapsed (11%) and 11 (5%) had died of progressive disease. Multivariate analysis found only grade 3 negatively affected the prognosis of patients. Grade 3 was also significantly associated with extraovarian relapse. Of the 105 patients (45%) who tried to become pregnant, 84 (80%) were successful. The authors concluded that conservative treatment can be proposed to all young patients when the tumor is limited to the ovaries, as ovarian recurrences can always be managed successfully. Patients with grade 3 tumors are more likely to have distant recurrences and should be closely monitored [11].
Several open questions have to be considered in the management of young patients with EOC undergoing FSS. The main controversial issues are: synchronous endometrial involvement, disease on the remaining ovary and systematic retroperitoneal lymphadenectomy.
Regarding the first issue, the concern about conservative surgery is the possible risk of extension to the endometrium or the presence of concurrent endometrial cancer. Literature data reported an endometrial involvement ranging from 5% to 14% [7,24,25]. In the present series only one patient had concomitant endometrial cancer of endometriod type FIGO stage IA, grade 1. In 1998 we reported a large series of endometrioid EOC with a rate of synchronous endometrial tumor of 11% (12 out of 106) [24]. In conclusion, the candidates to FSS should always be evaluated either with hysteroscopy or endometrial curettage, especially if the ovarian cancer is an endometrioid type tumor.
Regarding the risk of concomitant disease on the residual ovary, old literature data reported a high rate of bilateral disease ranging from 7% to 12%; however, even the presence of macroscopic disease was considered [17,26]. In more recent data, looking only at microscopic disease, the percentage of bilateral involvement dropped to a range of 0%-2% to 5% [7,21,27]. The biopsy of the normal-appearing contralateral ovary is not indicated by many practitioners since it can miss microscopic foci and it has been associated with adhesion formation and subsequent infertility. Based on the data of the present study, an accurate macroscopic inspection of the ovary is sufficient.
Finally, the role of lymphadenectomy is one of the most controversial issues in the treatment of eEOC. Lymph node evaluation is recommended in the surgical treatment of eEOC according to the FIGO criteria; however, the radicality of the lymphadectomy remains unclear. Whereas this procedure certainly has a diagnostic and prognostic impact, the therapeutic role is still unclear. A randomized study showed the high accuracy of systematic lymphadenectomy versus sampling in discovering positive nodes (9% vs. 22%, p=0.007) [28]. In our whole series of eEOC we found a significant association between menopause and lymph-node metastases suggesting childbearing age as a lower risk factor for nodal involvement [15]. An indirect evidence of the therapeutic role of accurate comprehensive staging including lymphadenectomy is the ACTION study. In this study the value of accurate staging in ovarian cancer is confirmed. In optimally staged patients, adjuvant chemotherapy does not improve survival when compared to observational control; a matter of interest for oncofertility considering the detrimental effect that chemotherapy could have on fertility.
In literature, there are many retrospective data and three large studies designed to investigate the role of FSS confirmed the safety of FSS in a selected group of young patients with eEOC. According to literature data, conservative surgery should be considered in the treatment of young women with stage IA, grade 1 and 2. FSS in clear cell cancer and high risk patients with FIGO stage ≥IA G3 is still under debate. In any case, an accurate surgical staging, including pelvic and para-aortic lymphadenectomy, is mandatory in this subset of patients.
The present study based on a series of matched cases and controls confirms the oncological safety of this kind of approach. The shortcoming of this study is the small number of patients enrolled, whilst its main value is the comparison of matched cases and controls operated in the same period by the same surgical group. Another methodological drawback is the unequal distribution of the menopausal status between the study groups. In fact, in the RCS group 11 patients were in menopause while in the FSS group no one was (p<0.05). The menopausal status has been reported to be a risk factor for node metastases in a previous study [15]; however, in the present study, patients were matched by stage. A third possible limitation of the study is the imbalance between the study groups regarding the number of patients submitted to laparoscopy (LPS) and open surgery. Although there is no level I evidence supporting the safety of the laparoscopic approach in eEOC, available literature data are encouraging regarding the oncological outcome of LPS treated patients. In our study in particular, more patients in the FSS group were submitted to a LPS approach with respect to RCS, and if there is a hypothetical negative impact of LPS approach, the FSS group would not have been favored. A fourth limitation is the imbalance of the two populations with respect to age. We did not consider age as a matching factor as there is no consensus in literature regarding its actual prognostic value [9,11]. Finally a third of the tumors in this series were primary mucinous tumors of the ovary (the appendix was evaluated and resulted negative). This percentage is in line with literature data [9,10,11]; however, patients were matched to overcome possible biases.
The data of this study suggest that FSS in eEOC underwent a comprehensive surgical staging could be considered safe with oncological results comparable to radical surgery group. Moreover a good obstetrical outcome could be achieved. The opportunity to extend the indication to conservative surgery to women with more advanced disease is highly controversial and needs further investigations. Clearer data are warranted by prospective controlled studies.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Heintz AP, Odicino F, Maisonneuve P, Beller U, Benedet JL, Creasman WT, et al. Carcinoma of the ovary. Int J Gynaecol Obstet. 2003;83(Suppl 1):135–166. doi: 10.1016/s0020-7292(03)90118-4. [DOI] [PubMed] [Google Scholar]
- 2.Trimbos JB, Vergote I, Bolis G, Vermorken JB, Mangioni C, Madronal C, et al. Impact of adjuvant chemotherapy and surgical staging in early-stage ovarian carcinoma: European Organisation for Research and Treatment of Cancer-Adjuvant ChemoTherapy in Ovarian Neoplasm trial. J Natl Cancer Inst. 2003;95:113–125. [PubMed] [Google Scholar]
- 3.Trimbos B, Timmers P, Pecorelli S, Coens C, Ven K, van der Burg M, et al. Surgical staging and treatment of early ovarian cancer: long-term analysis from a randomized trial. J Natl Cancer Inst. 2010;102:982–987. doi: 10.1093/jnci/djq149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.American Cancer Society. Cancer facts & figures 2013 [Internet] Atlanta, GA: American Cancer Society; c2013. [cited 2014 Sep 16]. Available from: http://www.cancer.org/acs/groups/content/@epidemiologysurveilance/documents/document/acspc-036845.pdf. [Google Scholar]
- 5.Young RC, Decker DG, Wharton JT, Piver MS, Sindelar WF, Edwards BK, et al. Staging laparotomy in early ovarian cancer. JAMA. 1983;250:3072–3076. [PubMed] [Google Scholar]
- 6.Duska LR, Chang YC, Flynn CE, Chen AH, Goodman A, Fuller AF, et al. Epithelial ovarian carcinoma in the reproductive age group. Cancer. 1999;85:2623–2629. doi: 10.1002/(sici)1097-0142(19990615)85:12<2623::aid-cncr19>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 7.Park JY, Kim DY, Suh DS, Kim JH, Kim YM, Kim YT, et al. Outcomes of fertility-sparing surgery for invasive epithelial ovarian cancer: oncologic safety and reproductive outcomes. Gynecol Oncol. 2008;110:345–353. doi: 10.1016/j.ygyno.2008.04.040. [DOI] [PubMed] [Google Scholar]
- 8.McHale MT, DiSaia PJ. Fertility-sparing treatment of patients with ovarian cancer. Compr Ther. 1999;25:144–150. doi: 10.1007/BF02889610. [DOI] [PubMed] [Google Scholar]
- 9.Wright JD, Shah M, Mathew L, Burke WM, Culhane J, Goldman N, et al. Fertility preservation in young women with epithelial ovarian cancer. Cancer. 2009;115:4118–4126. doi: 10.1002/cncr.24461. [DOI] [PubMed] [Google Scholar]
- 10.Satoh T, Hatae M, Watanabe Y, Yaegashi N, Ishiko O, Kodama S, et al. Outcomes of fertility-sparing surgery for stage I epithelial ovarian cancer: a proposal for patient selection. J Clin Oncol. 2010;28:1727–1732. doi: 10.1200/JCO.2009.24.8617. [DOI] [PubMed] [Google Scholar]
- 11.Fruscio R, Corso S, Ceppi L, Garavaglia D, Garbi A, Floriani I, et al. Conservative management of early-stage epithelial ovarian cancer: results of a large retrospective series. Ann Oncol. 2013;24:138–144. doi: 10.1093/annonc/mds241. [DOI] [PubMed] [Google Scholar]
- 12.Morice P, Leblanc E, Rey A, Baron M, Querleu D, Blanchot J, et al. Conservative treatment in epithelial ovarian cancer: results of a multicentre study of the GCCLCC (Groupe des Chirurgiens de Centre de Lutte Contre le Cancer) and SFOG (Societe Francaise d'Oncologie Gynecologique) Hum Reprod. 2005;20:1379–1385. doi: 10.1093/humrep/deh777. [DOI] [PubMed] [Google Scholar]
- 13.Schilder JM, Thompson AM, DePriest PD, Ueland FR, Cibull ML, Kryscio RJ, et al. Outcome of reproductive age women with stage IA or IC invasive epithelial ovarian cancer treated with fertility-sparing therapy. Gynecol Oncol. 2002;87:1–7. doi: 10.1006/gyno.2002.6805. [DOI] [PubMed] [Google Scholar]
- 14.Raspagliesi F, Fontanelli R, Paladini D, di Re EM. Conservative surgery in high-risk epithelial ovarian carcinoma. J Am Coll Surg. 1997;185:457–460. doi: 10.1016/s1072-7515(97)00066-5. [DOI] [PubMed] [Google Scholar]
- 15.Ditto A, Martinelli F, Reato C, Kusamura S, Solima E, Fontanelli R, et al. Systematic para-aortic and pelvic lymphadenectomy in early stage epithelial ovarian cancer: a prospective study. Ann Surg Oncol. 2012;19:3849–3855. doi: 10.1245/s10434-012-2439-7. [DOI] [PubMed] [Google Scholar]
- 16.U.S. Department of Health and Human Services, National Cancer Institute at the National Institutes of Health. Common Terminology Criteria for Adverse Events (CTCAE) version 4.0 [Internet] Bethesda, MD: National Cancer Institute; 2014. [cited 2014 Aug 20]. Available from: http://evs.nci.nih.gov/ftp1/CTCAE/CTCAE_4.03_2010-06-14_QuickReference_5x7.pdf. [Google Scholar]
- 17.Zanetta G, Chiari S, Rota S, Bratina G, Maneo A, Torri V, et al. Conservative surgery for stage I ovarian carcinoma in women of child-bearing age. Br J Obstet Gynaecol. 1997;104:1030–1035. doi: 10.1111/j.1471-0528.1997.tb12062.x. [DOI] [PubMed] [Google Scholar]
- 18.Anchezar JP, Sardi J, Soderini A. Long-term follow-up results of fertility sparing surgery in patients with epithelial ovarian cancer. J Surg Oncol. 2009;100:55–58. doi: 10.1002/jso.21297. [DOI] [PubMed] [Google Scholar]
- 19.Kajiyama H, Shibata K, Suzuki S, Ino K, Nawa A, Kawai M, et al. Fertility-sparing surgery in young women with invasive epithelial ovarian cancer. Eur J Surg Oncol. 2010;36:404–408. doi: 10.1016/j.ejso.2010.01.005. [DOI] [PubMed] [Google Scholar]
- 20.Colombo N, Parma G, Lapresa MT, Maggi F, Piantanida P, Maggioni A. Role of conservative surgery in ovarian cancer: the European experience. Int J Gynecol Cancer. 2005;15(Suppl 3):206–211. doi: 10.1111/j.1525-1438.2005.00428.x. [DOI] [PubMed] [Google Scholar]
- 21.Morice P, Wicart-Poque F, Rey A, El-Hassan J, Pautier P, Lhomme C, et al. Results of conservative treatment in epithelial ovarian carcinoma. Cancer. 2001;92:2412–2418. doi: 10.1002/1097-0142(20011101)92:9<2412::aid-cncr1590>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- 22.Borgfeldt C, Iosif C, Masback A. Fertility-sparing surgery and outcome in fertile women with ovarian borderline tumors and epithelial invasive ovarian cancer. Eur J Obstet Gynecol Reprod Biol. 2007;134:110–114. doi: 10.1016/j.ejogrb.2006.05.037. [DOI] [PubMed] [Google Scholar]
- 23.Schlaerth AC, Chi DS, Poynor EA, Barakat RR, Brown CL. Long-term survival after fertility-sparing surgery for epithelial ovarian cancer. Int J Gynecol Cancer. 2009;19:1199–1204. doi: 10.1111/IGC.0b013e31819d82c3. [DOI] [PubMed] [Google Scholar]
- 24.Grosso G, Raspagliesi F, Baiocchi G, Di Re E, Colavita M, Cobellis L. Endometrioid carcinoma of the ovary: a retrospective analysis of 106 cases. Tumori. 1998;84:552–557. doi: 10.1177/030089169808400508. [DOI] [PubMed] [Google Scholar]
- 25.Kottmeier HL. Surgical treatment-conservative surgery. In: Gentil F, Junqueira AC, editors. Ovarian cancer, UICC monographs series. Vol. 11. New York: Springer Verlag; 1968. pp. 157–164. [Google Scholar]
- 26.Munnell EW. Is conservative therapy ever justified in stage I (IA) cancer of the ovary? Am J Obstet Gynecol. 1969;103:641–653. doi: 10.1016/0002-9378(69)90561-4. [DOI] [PubMed] [Google Scholar]
- 27.Benjamin I, Morgan MA, Rubin SC. Occult bilateral involvement in stage I epithelial ovarian cancer. Gynecol Oncol. 1999;72:288–291. doi: 10.1006/gyno.1998.5260. [DOI] [PubMed] [Google Scholar]
- 28.Maggioni A, Benedetti Panici P, Dell'Anna T, Landoni F, Lissoni A, Pellegrino A, et al. Randomised study of systematic lymphadenectomy in patients with epithelial ovarian cancer macroscopically confined to the pelvis. Br J Cancer. 2006;95:699–704. doi: 10.1038/sj.bjc.6603323. [DOI] [PMC free article] [PubMed] [Google Scholar]


