Dear Editor:
The epidemic of thyroid cancer among children exposed to radiation is a worldwide known health consequence of the Chernobyl accident, which took place on April 26, 1986. In Ukraine, a sharp increase in the incidence of thyroid cancer was observed since 1990, and had been preceded by a so-called period of latency during which no significant raise in baseline incidence was registered (1). Current interpretation of the cases in young patients detected during the period of latency in Chernobyl areas is that they were not due to radiation.
A large-scale nuclear accident occurred at the TEPCO-Fukushima Daiichi Nuclear Power plant in Mach 2011. In response to the disaster, Fukushima Prefecture launched the Fukushima Health Management Survey to investigate long-term low-dose radiation health effects. The Thyroid Ultrasound Examination Program, a component of the Survey, was started in October 2011 aiming at performing ultrasound examination of the neck in some 360,000 Fukushima Prefecture residents aged up to 18 years in March 2011. As of February 2014, the Program covered nearly 80% of the target population and reported 75 cases suspicious for malignancy or malignant (2). Note that these findings were obtained using highly sensitive ultrasound equipment in the course of an unprecedented mass screening, which unavoidably increases incidence rate (3); the screening is being performed for the first time in this geographic area, and in a screening-naïve population. Thirty-four patients have received surgery; pathological diagnoses include one benign tumor, one suspicious for poorly differentiated thyroid carcinoma, and 32 papillary thyroid carcinomas. Such a high prevalence has not been anticipated, and is widely discussed by the specialists and the public, sometimes expressing concerns about possible relationship to radiation exposure.
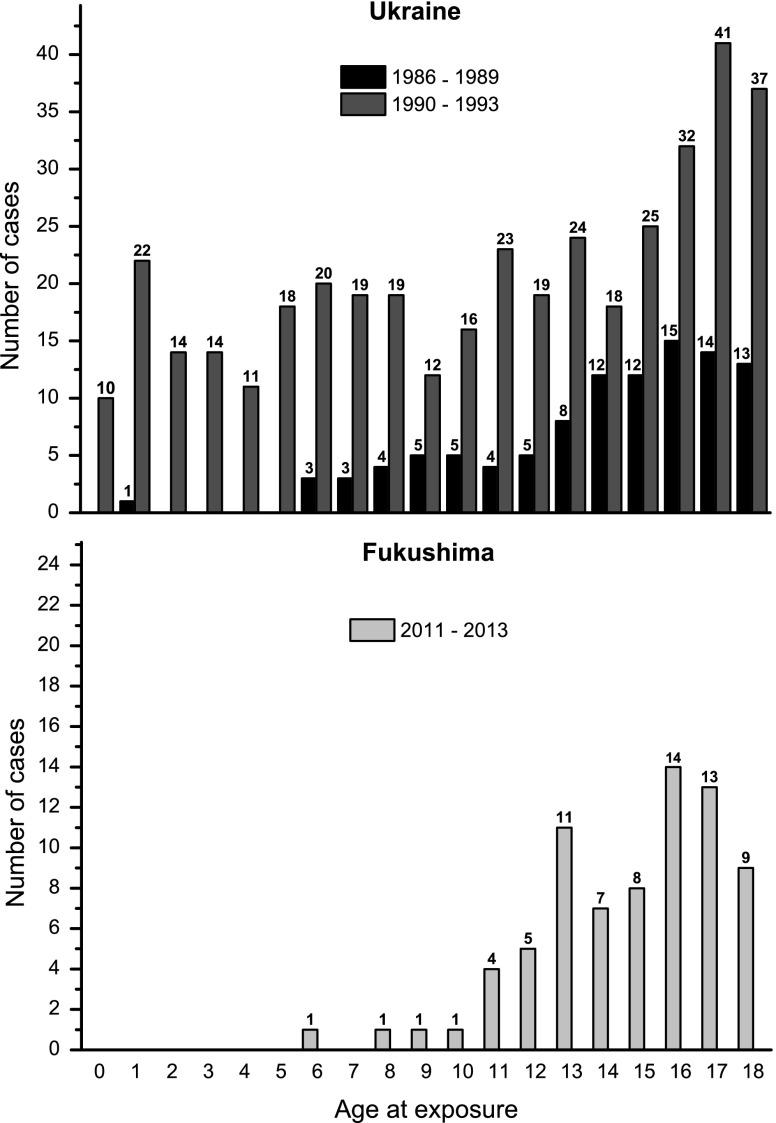
In Figure 1, we plotted the distribution of thyroid cancer patients aged up to 18 years at accident by their age at exposure diagnosed in Ukraine during the period of latency and first years after it (1), and of those diagnosed in Fukushima (2). There is a striking similarity between the profiles of patients diagnosed during the period of latency after Chernobyl in Ukraine and currently in Fukushima. In contrast, patients diagnosed in Ukraine after the period of latency, when radiation-induced tumors started to manifest, display principally a different age pattern. A large number of individuals exposed below five years of age, who are at the highest risk for radiation-induced thyroid cancer, have been seen. No such patients have been diagnosed in Fukushima so far.
FIG. 1.
Distribution of thyroid cancer patients by age at exposure diagnosed during the period of latency (1986–1989) and after it (1990–1993) in Ukraine, and patients with verified or suspicious thyroid cancer in Fukushima diagnosed during 2011–2013. Numbers above the bars correspond to the number of patients of a given age at exposure. Note that comparison of the absolute number of cases between the two regions of radiological accidents would be inappropriate because of differences in population size and screening protocols, in particular a more systematic approach, higher population coverage, and advanced ultrasound equipment in Fukushima.
In our opinion, if thyroid cancers in Fukushima were due to radiation, more cases in exposed preschool-age children would have been expected. In addition, thyroid doses in Fukushima are markedly lower than those in Chernobyl areas (4). Further analysis will be necessary with respect to the thyroid cancer cases that may appear in the coming years, once the period of latency has passed. Particular attention should be paid to thyroid dose reconstruction, age at exposure and diagnosis, tumor morphology (the solid growth pattern was frequently observed in childhood papillary thyroid carcinomas that developed after the short period of latency in Chernobyl), and whether there will be a “harvesting effect,” which is a spike in cases after introduction of screening.
Acknowledgment
This publication was supported by research grant 25257508 from the Japan Society for the Promotion of Science (JSPS).
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Tronko M, Shpak V, Bogdanova T, Saenko V, Yamashita S.2014Epidemiology of thyroid cancer in Ukraine after Chernobyl. In: Tronko M, Bogdanova T, Saenko V, Thomas GA, Likhtarov I, Yamashita S. (eds) Thyroid Cancer in Ukraine after Chernobyl. Dosimetry, Epidemiology, Pathology, Molecular Biology. IN–TEX, Nagasaki, Japan, pp 39–64 [Google Scholar]
- 2.Thyroid Ultrasound Examination, Fukushima Health Management Survey. Available at: www.fmu.ac.jp/radiationhealth/results/media/14-2_ThyroidUE.pdf (accessed April21, 2014)
- 3.Jacob P, Kaiser JC, Ulanovsky A.2014Ultrasonography survey and thyroid cancer in the Fukushima Prefecture. Radiat Environ Biophys 53:391–401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.UNSCEAR 2014 Sources, effects and risks of ionizing radiation. Volume I: Scientific Annex A. Levels and effects of radiation exposure due to the nuclear accident after the 2011 great east-Japan earthquake and tsunami. UNSCEAR 2013 Report. United Nations, New York [Google Scholar]