Abstract
Background: Adolescence is a critical period for the development of depressive symptoms and obesity. This study examined the association of depressive symptoms with standardized BMI (BMI z-score), lifestyle behaviors, and self-efficacy measures in a sample of urban adolescents.
Methods: A school-based study was conducted among adolescents (N=1508) enrolled from 11 public schools. Depressive symptoms were assessed with Kandel's depressive symptoms scale for adolescents. Fruit and vegetable intake and intake of energy-dense foods were assessed by a short food frequency questionnaire. Sedentary behavior and physical activity (PA) were obtained by self-report. Height and weight were measured directly and BMI z-scores were calculated. Mixed-effects models were used to examine the association of depressive symptoms with BMI z-score and lifestyle behaviors, accounting for clustering at school level and adjusting for confounders. Self-efficacy measures were evaluated as potential mediators.
Results: The sample was 53% female, 75% Hispanic, and 82% US born, with a mean age of 13.9 years. Higher depressive symptoms were associated with higher BMI z-score (β=0.02; p=0.02), intake of energy-dense foods (β=0.42; p<0.001), and sedentary behavior (β=0.48; p<0.001), but lower PA (β=−0.03; p=0.01). There was an interaction by gender in the association of depressive symptoms and PA. Self-efficacy mediated the association of depressive symptoms and PA.
Conclusions: Obesity prevention and treatment programs should consider addressing the role of negative emotions as part of their preventive strategies.
Introduction
Adolescence is a vulnerable period for the emergence of depression and obesity.1,2 Depressive symptoms are associated with risk behaviors and adverse health outcomes in adolescents. For example, adolescents with high depressive symptoms are more likely to have problems getting along with parents and peers, are more likely to smoke, and are at greater risk of substance use.3,4 Previous studies indicate that obesity may increase the risk of depression.5,6 However, recent studies also suggest that depressive symptoms could put adolescents at risk of obesity.7–9
Several cross-sectional studies provide evidence for a link between depressive symptoms and weight status or BMI in adolescence.3,10,11 Using a nationally representative sample of US adolescents, BeLue and colleagues10 found an association between several mental health indicators and overweight, including depression, anxiety, and stress coping. Findings from a long-term follow-up study of youth ages 6–17 years showed that childhood and adolescent depression predicted BMI in adulthood.12 Results from another longitudinal study showed that depressed mood in adolescents was predictive of BMI 1 year later, controlling for initial BMI.13 There also appear to be gender differences. Several studies found that the association between depressive symptoms and weight status or adiposity was only evident in females.14 However, the pathways explaining the association between depressive symptoms and obesity are not well understood. One proposed mechanism linking depression to the development of obesity includes the adoption of unhealthy lifestyle behaviors. Research studies suggest that some adolescents may use food as a coping mechanism, showing a preference for high-energy, more palatable foods.15–18 Mental distress could then be associated with higher intake of energy-dense foods that are low in nutritional value. Consequently, this type of change in eating behaviors could lead to increased caloric intake and excess weight.
The behavioral mechanisms that relate depressive symptoms to unhealthy lifestyle behaviors and obesity have not been fully examined. One potential mechanism is the adverse effect of depressive symptoms on self-efficacy. Self-efficacy is defined as the perceived capability for achieving behavioral goals.19 Previous studies show an association of self-efficacy with health-promoting behaviors.20–22 For example, higher levels of self-efficacy are related to increased intake of fruit and vegetables,20,21 and self-efficacy is one of the strongest predictors of physical activity (PA) among adolescents.23 In addition, because people with depression often report a sense of worthlessness and a more pessimistic view of themselves, adolescents with high levels of depressive symptoms may experience decreased confidence in being capable of engaging in and sustaining healthy lifestyle behaviors.19
Taking these aspects into consideration, this study examined whether depressive symptoms were associated with excess weight in a sample of inner-city adolescents. We focused on urban minority youth because they are at high risk of obesity and depression.24–26 Youth from socioeconomically disadvantaged backgrounds are also found to have lower self-efficacy than youth from higher socioeconomic backgrounds.27 Understanding these interrelations is important, because it may help build more successful intervention strategies for improving the health of urban youth. In addition, the study examined whether there would be an association of depressive symptoms with lower self-efficacy for healthy eating and being physically active and whether lower self-efficacy was related to lifestyle behaviors. We hypothesized that higher depressive symptoms would be associated with higher BMI z-score and more sedentary behavior, but lower intake of fruit and vegetables. Because there is some evidence that the association between depressive symptoms and health-related behaviors are mediated by self-efficacy,28 we also hypothesized that the association between depressive symptoms and lifestyle behaviors was mediated by lower self-efficacy for exercising and eating healthy. We also examined interaction effects by gender because earlier research indicates that girls have higher levels of depressive symptoms than boys and that the effect of depressive symptoms on outcomes may vary by gender.14,29–31
Methods
Participants
The study enrolled 1809 participants in grades 7–10 from 11 public schools in the Bronx, New York. The study took place during the months of February–June and October–December 2008 and was part of a larger study examining the association of psychosocial factors with obesity in this population. Inclusion criteria included adequate facility in English and not being enrolled in special education classes. Of the total number enrolled, 301 did not complete the depressive symptoms scale and were excluded from these analyses, leaving a total sample size of 1508. Age, self-efficacy measures, lifestyle behaviors, and BMI z-score were similar in adolescents who completed the depressive symptoms scale and in those who had it missing. However, boys and foreign-born adolescents were less likely to complete the depression symptoms scale than girls and US-born adolescents.
Procedure
The study was approved by the institutional review boards of the Albert Einstein College of Medicine and the New York City Department of Education. Letters were mailed to parents informing them of the research study. Parents were told to mail back a self-addressed prepaid postcard or to notify a designated school official if they did not want their child to participate in the study. Before data collection, students signed an assent form if they agreed to participate. The overall participation rate was 68%. Reasons for declining to complete the survey included parental or student refusals (4% and 26%, respectively), letters returned by postal office (6%), student transfers to other schools (5%), and student absenteeism (59%). A self-reported questionnaire was administered to students in classrooms by trained research staff. Students' heights and weights were measured within 1 week of survey administration.
Measures
Depressive symptoms
Kandel's six-item depressive symptoms scale was used to assess depressive symptoms.32,33 The scale asks students how much they have been bothered by feelings of being too tired to do things or being unhappy, sad, or depressed. Responses were on a 3-point scale (“Not at all,” “Somewhat,” or “Much”). Scores were computed by summing responses of each individual item (Cronbach's alpha for the study sample=0.78).
Self-efficacy for healthy food choices
The study used the nine-item scale developed by Neumark-Sztainer, which assesses self-efficacy to make healthy food choices in social, emotional, and normal situations (e.g., “if you wanted to, how sure are you that you could eat healthy food when you are…at a fast food restaurant?”).34 Responses were on a 5-point scale that range from “not at all sure” to “very sure.” For each participant, scores were computed using the sum of responses to individual items (Cronbach's alpha for the study sample=0.87).
Self-efficacy for being physically active
The study used Sallis' six-item self-efficacy scale, which asks students how sure they were that they could do PA in a variety of situations, such as when feeling sad or stressed, or when having a lot of homework.35 Responses were on a 5-point scale that ranged from “I'm sure I can't” to “I'm sure I can.” A score was derived using the sum of responses to individual items in the scale (Cronbach's alpha for the study sample=0.85).
Dietary assessment
Fruit and vegetable intake and intake of energy-dense foods (e.g., cookies and French fries) were assessed with the short version of the Youth/Adolescent Questionnaire (YAQ), a food frequency questionnaire (FFQ) that was validated in the Growing Up Today Study, and has shown an adequate correlation against the full YAQ and against 24-hour recall interviews.36,37 Students were asked to report how often, on average, during the past year they had eaten the food items listed (e.g., apples and carrots). Responses were on an 8-point scale that ranged from “Never/less than 1 a month” to “More than 3 per day.” Scores were computed by adding the individual responses to each food item within these food groups.
Physical activity
Vigorous PA was assessed with one item from the Youth Risk Behavior Survey,38 which asked “During the last 14 days, how many days have you done at least 20 minutes of exercise hard enough to make you breathe heavily and make your heart beat fast?” Responses for this item were on a 5-point scale (“none,” “1–2 days,” “3–5 days,” “6–8 days,” or “9 or more days”), and the sum of the responses were used to calculate a score for this variable.
Sedentary behavior
It was assessed by a scale that asked students how much time they spent doing sedentary activities on the most recent day they were not in school.39 Items include time spent watching television, playing computer or video games, sitting and listening to music, and sitting and talking on the phone or cell phone or text messaging, which are sedentary activities common among adolescents. Whereas the original scale consists of two subscales for sedentary behaviors during school days and nonschool days, the latter was used because nonschool days are less structured and there is more time for adolescents to choose to engage in more active or sedentary pursuits.40 Responses were on a 9-point scale, from “none” to “6 hours or more.” A score was computed by adding responses to each item in the scale (Cronbach's alpha for the study sample=0.68).
Height and weight
These measures were obtained by trained research staff using a standardized protocol. Privacy screens were set up in the classroom to maintain students' privacy during assessments. Students were instructed to wear light clothing and remove their shoes at the time of the assessment, and each measure was obtained once. Height was measured using a portable stadiometer (Seca Portable Stadiometer 214; SECA GmbH & Co. KG, Hamburg, Germany). Weight was measured using a digital portable scale (Seca Robusta 813; SECA GmbH & Co. KG). These measures were used to derive a BMI z-score for each participant, using the CDC growth curves for age and sex.41
Sociodemographic characteristics
Students were asked to report their age, gender, race/ethnicity, and maternal education.
Statistical Analyses
Descriptive analyses included calculation of the percentage distribution and means with their associated standard deviations (SDs) for categorical and continuous variables. Before any analyses, variables were checked for normality. Differences in percentage and means were tested using chi-square tests for differences between categorical variables and with the Student's t-test for continuous variables. Pearson's correlation coefficients were calculated to examine the association between two continuous variables. Mixed-effects models were conducted to test the association of depressive symptoms with BMI z-score and lifestyle behaviors, accounting for clustering at the school level and adjusting for potential confounders (age, gender, race/ethnicity, and maternal education).42
To examine whether self-efficacy was a mediator of the association of depressive symptoms with lifestyle behaviors, a path analysis was conducted with depressive symptoms specified as the independent variable, self-efficacy as the mediator, and health behavior as the outcome. A Sobel-Goodman test was performed to test the statistical significance of the indirect effects.43,44 Interaction by gender was examined by including a multiplicative term in the models (gender*depressive symptoms). Analyses were performed using Stata statistical software (Stata/SE 12.0; StataCorp LP, College Station, TX).
Results
Characteristics of the Study Population
The mean age of study participants was 13.9 years (SD, 1.4; range, 11–18) and 53% were female. The sociodemographic distribution of participants is presented in Table 1. Adolescent girls reported higher depressive symptoms than boys (11.3±3.0 vs. 10.4±2.9; p<0.001). Girls also reported less self-efficacy for healthy eating and being physically active than boys (23.5±8.5 vs. 24.3±8.0; p=0.048 and 16.6±5.7 vs. 19.7±5.8; p<0.001, respectively). Girls showed lower PA than boys (2.4±1.2 vs. 3.2±1.33; p<0.001), but higher intake of energy-dense foods (31.9±12.7 vs. 29.2±11.7; p<0.001) and more time spent in sedentary behaviors (24.6±7.8 vs. 22.8±7.4; p<0.001). Compared to non-Hispanic adolescents, Hispanic teenagers had a higher BMI z-score (0.90±0.98 vs. 0.66±0.94; p<0.001), lower intake of fruits and vegetables (14.2±6.9 vs. 15.3±6.7; p=0.01), and lower PA levels (2.7±1.3 vs. 2.9±1.3; p=0.02). Further, Hispanic youth reported lower self-efficacy for healthy eating (23.5±8.3 vs. 24.7±8.2; p=0.02) and lower self-efficacy for being physically active (17.8±6.1 vs. 18.6±5.6; p=0.04). Depressive symptoms did not vary by race/ethnicity. Adolescents with mothers who did not complete a high school education had higher depressive symptoms and lower self-efficacy for being physically active, compared to adolescents whose mothers had a high school or greater education attainment (11.4±3.2 vs. 10.8±3.0, p=0.008 and 22.6±8.5 vs. 24.0±8.2, p=0.03, respectively). However, lifestyle behaviors and BMI z-score did not vary by maternal educational attainment.
Table 1.
Characteristics of the Study Sample
| Characteristic | N (%) |
|---|---|
| Female | 799 (53) |
| Hispanic | 1123 (75) |
| Non-Hispanic African American | 94 (6) |
| Other race/ethnicity | 291 (19) |
| US born | 1221 (82) |
| Obesity (BMI ≥95th percentile) | 361 (22.5) |
| Maternal education | |
| Less than high school | 196 (23) |
| High school | 192 (23) |
| Some college | 117 (14) |
| College | 231 (28) |
| Graduate education (e.g., master, doctoral) | 86 (11) |
Association of Depressive Symptoms with Body Mass Index z-Score and Lifestyle Behaviors
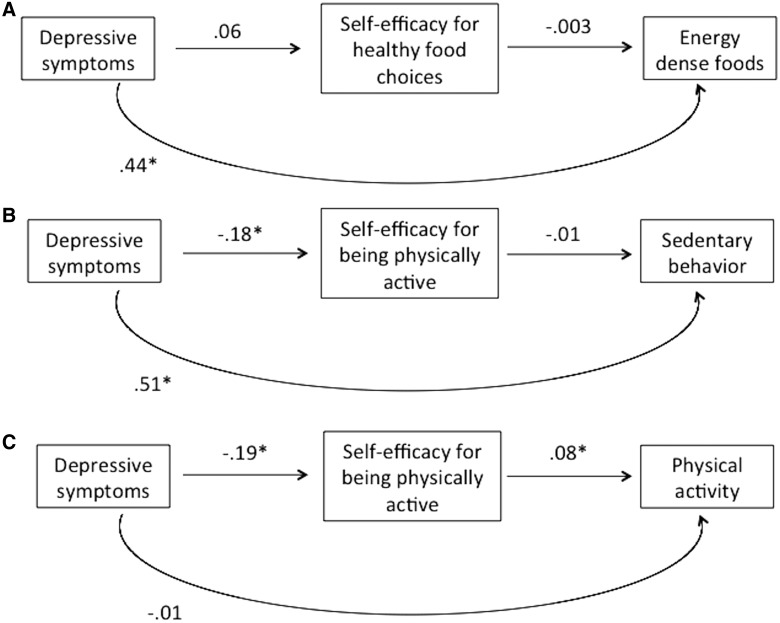
Mixed-effects models showed an association between depressive symptoms, unhealthy lifestyle behaviors, and excess weight (Table 2). Higher depressive symptoms were associated with higher intake of energy-dense foods (β=0.42; p<0.001), more time spent on sedentary behaviors (β=0.48; p<0.001), and higher BMI z-score (β=0.02; p=0.02). Higher depressive symptoms were significantly associated with lower PA (β=−.03; p=.01). However, depressive symptoms were not associated with fruit and vegetable intake or with self-efficacy for healthy eating. When self-efficacy for being physically active was included in the models, the magnitude of the inverse association of depressive symptoms with PA was substantially reduced and became nonsignificant, suggesting that this measure of self-efficacy mediated the association. Results of the path analysis (Fig. 1) showed direct effects of depressive symptoms on PA (β=−0.01; p<0.01) and indirect effects mediated by self-efficacy for being physically active (β for indirect effect=−0.01; p<0.001). The Sobel mediation test indicated that 50% of the total effect of depressive symptoms on PA was mediated by self-efficacy. Self-efficacy for healthy food choices did not mediate the association of depressive symptoms and intake of energy-dense foods. Similarly, self-efficacy for being physically active did not mediate the association of depressive symptoms with sedentary behavior (Fig. 1).
Table 2.
Mixed-Effects Models for the Association of Depressive Symptoms with BMI and Lifestyle Behaviors
| Alla | Girlsb | Boysb | ||||
|---|---|---|---|---|---|---|
| β (SE) | p value | β (SE) | p value | β (SE) | p value | |
| BMI z-score | 0.02 (0.01) | 0.02 | 0.03 (0.01) | 0.005 | 0.01 (0.01) | 0.48 |
| Energy-dense foods | 0.42 (0.12) | <0.001 | 0.54 (0.16) | 0.001 | 0.24 (0.17) | 0.16 |
| Physical activity | −0.03 (0.01) | 0.01 | −0.01 (0.01) | 0.54 | −0.06 (0.02) | 0.003 |
| Sedentary behavior | 0.48 (0.07) | <0.001 | 0.60 (0.09) | <0.001 | 0.33 (0.10) | 0.001 |
Models are adjusted for age, gender, race/ethnicity, and maternal education.
Models are adjusted for age, ethnicity, and maternal education.
SE, standard error.
Figure 1.
Path analyses for the association of depressive symptoms, self-efficacy measures, and lifestyle behaviors. Standardized coefficients are reported in the figure. All models are adjusted for age, gender, race/ethnicity, and maternal education. (A) β for indirect effect=−0.0002, p>0.5; (B) β for indirect effect=0.001, p>0.05; (C) β for indirect effect=−0.01, p<0.001. *p<0.05
Differences by Gender
This study also examined whether the effects of depression on BMI z-score and lifestyle behaviors varied by gender. In order to test for interaction, we first conducted separate mixed-effects models for boys and girls (Table 2) and later added a cross-product term (gender*depression) to the overall models described in the previous paragraph. Boys, but not girls, showed an inverse association of depressive symptoms with physical activity, and this interaction was found to be significant in the full model (p=0.04). The association of depressive symptoms and sedentary behavior appeared to be stronger among adolescent girls than in boys, but the interaction did not reach statistical significance (p=0.07). No interaction with gender was observed for the association of depressive symptoms with BMI z-score.
Discussion
The study findings showed that higher depressive symptoms were associated with higher intake of energy-dense foods, more time spent on sedentary behaviors, and higher BMI z-score, but lower PA levels. Consistent with previous research, adolescent girls had higher depressive symptoms than boys.2 This study also identified gender differences in the association of depressive symptoms and weight-related lifestyle behaviors. Among boys, there was an inverse association of depressive symptoms and PA, which was not observed among girls.
The study findings are consistent with reports from other research studies.3,7,9,29,45,46 Jaser and colleagues45 showed that youth with higher levels of depressive symptoms had higher BMI, and depressive symptoms also showed a strong inverse correlation with self-efficacy. The National Longitudinal Study of Adolescent Health (Add Health) showed that depressed adolescents were twice as likely to become obese than adolescents without depression.13 Adolescents who were already obese at baseline showed a worsening of their obesity if they were depressed. Further, the Trial of Activity for Adolescent Girls study reported bidirectional associations of depressed mood with obesity in a large sample of adolescent girls. However, these associations were observed only among white girls, and not among minority girls.47
Similar to our findings, Project EAT investigators reported an inverse association of depressive symptoms with PA among boys, but not girls.4 However, in Project EAT, girls with higher depressive symptoms engaged in more sedentary behaviors, an association that was not observed in boys. Project EAT did not find an association of depressive symptoms with dietary intake, but there was a significant association with some dietary behaviors; adolescents with higher scores of depressive symptoms reported eating breakfast, lunch, and dinner less frequently than adolescents reporting fewer depressive symptoms. Gender differences in the association of depressive symptoms and PA could be explained by differences in how boys and girls respond to distress, but further research is needed to elucidate the reasons for these gender interactions and help improve the effects of health-promoting interventions.
One of the novel contributions of the study is examining the association of self-efficacy with lifestyle behaviors and depressive symptoms. Whereas the association of self-efficacy with lifestyle behaviors has been inconsistent across studies,20 in this study a strong positive correlation was found between self-efficacy for being physically active and PA levels, and a moderate correlation was found between self-efficacy for healthy eating and intake of fruits and vegetables. Further, self-efficacy mediated the inverse association of depressive symptoms and PA; this finding suggests that depressive symptoms decrease adolescents' perception of self-efficacy for being physically active and, in turn, make them less likely to engage in PA. These results corroborate findings from the few studies that have examined the relationship between depressive symptoms and self-efficacy. A prospective study reported that among girls, increases in depressive symptoms lead to lower PA levels despite high self-efficacy at baseline.48 Though Project EAT did not examine self-efficacy in relation to depressive symptoms,4 the study found that adolescents with higher depressive symptoms reported more barriers to healthy eating. In the present study, self-efficacy for healthy eating did not mediate the association between depressive symptoms and intake of energy-dense foods. This could be explained by the nature of the self-efficacy scale that is specific for healthy foods and does not ask about adolescents' perception of their capacity for minimizing intake of foods that are of low nutritional value.
One of the strengths of this study is the community-based sample of predominantly Hispanic adolescents, a group that is at disproportionately high risk of obesity and depression.10,49,50 The large sample size allowed us to examine interaction effects by gender. An important limitation of the study is the cross-sectional design, which prevents us from making statements about temporality and causality. Further, a bidirectional relationship between efficacy beliefs and depression has been postulated,19,51 with depressive symptoms leading to a sense of low efficacy, and this inefficacy belief, in turn, increasing the sense of hopelessness and depressive symptoms, thus creating a detrimental cycle for the adolescent. The lack of prospective data prevents us from testing this bidirectionality. Similarly, we were unable to determine whether depression increases the risk of obesity or whether obesity increases the risk of depression; the relationship is suggested to be bidirectional.14,47
Other limitations of the study include the use of a short version of an FFQ, self-reported measures of sedentary behaviors, and a very brief measure of self-reported PA; thus, there is the potential for measurement error. However, the measurement error was not systematic, and therefore it is more likely that it biased results toward the null. The scale to assess depressive symptoms was a brief inventory, and not a diagnostic instrument, so caution is needed when interpreting results. In addition, the study was conducted during the school academic year and did not include the summer months. There are likely seasonal variations affecting the amount of PA and the type of foods consumed, given that students may decrease their PA because of cold weather and the availability of certain fruits and vegetables may decrease during the winter.52 Therefore, seasonal variability may have led some students to underreport their usual physical activity. However, for dietary intake, as students were asked to report their intake over the past year, seasonal changes in food availability may be less important. Further, seasonal variability of depressive symptoms may affect only older adolescents (16–18 years of age) and do not appear to be as pronounced as for adults.53
The study results have important clinical implications. Minority urban youth are reported to have higher burden of obesity and depressive symptoms.10,49,50 Both are complex health conditions requiring intense interventions, and the resources to address these needs in disadvantages areas, such as the Bronx, are scarce. Two reports addressing children's mental health needs in the Bronx found that more than half (57%) of referrals for outpatient mental health services never receive any treatment.54,55 The main barriers to address these needs are related to a reduced workforce capacity, limited insurance coverage, and language barriers.54,55 Further, these reports also indicate that the majority of children needing mental health services in the Bronx were of Hispanic or African American background, but the majority of providers were not, suggesting that cultural sensitivity may be another barrier to care.54,55 Improving youth access to mental health services has the potential for improving health above and beyond mental health functioning, reducing the risks of obesity and chronic diseases.
Conclusions
The study findings highlight the need to address mental health in our efforts to reduce obesity and promote the adoption of healthy behaviors in order to decrease the risk of chronic disease later in adulthood. More research is needed to gain a better understanding of the behavioral processes that link mental health to lifestyle behaviors and obesity in youth. Future studies may need to identify the factors that may modify and ameliorate the effects of depressive symptoms on health behaviors to build more-successful prevention programs. For example, resilience factors that may buffer the effects of depressive symptoms (e.g., parental support and positive coping strategies) need to be identified. The role of the urban environment needs to be considered in explaining the link between obesity and mental distress in youth. Many studies have found that exposure to neighborhood disorder and violence as well as limited access to fresh produce and places to exercise are important predictors of obesity.56 These neighborhood characteristics are very common in urban areas and have been also related to mental functioning.57–59 All these aspects may be particularly important during adolescence, given that this is a critical period for the development of obesity and for the emergence of depressive symptoms. Further, minority adolescents report higher depressive symptoms than nonminority adolescents60 and may have limited access to mental health services61; thus, building mental health components into health promotion interventions may have a greater impact on adolescents' physical and mental health.
Acknowledgments
The authors thank the principals and teachers of the schools for their support, as well as participating parents and students for their cooperation. The authors also thank the Montefiore School Health Program and the Bronx School Nutrition and Fitness Committee for facilitating schools' participation. The project was supported by Award No. R21HD052721 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Eunice Kennedy Shriver National Institute of Child Health and Human Development of the National Institutes of Health. Preliminary findings were reported as posters at the International Society of Behavioral Nutrition and Physical Activity, Melbourne, Australia, June 15–18, 2011, and the First Annual Conference of the New York City Epidemiology Forum, New York, NY, February 28, 2014.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Dietz WH. Critical periods in childhood for the development of obesity. Am J Clin Nutr 1994;59:955–959 [DOI] [PubMed] [Google Scholar]
- 2.Rawana JS, Morgan AS, Nguyen H, et al. The relation between eating- and weight-related disturbances and depression in adolescence: A review. Clin Child Fam Psychol Rev 2010;13:213–230 [DOI] [PubMed] [Google Scholar]
- 3.Katon W, Richardson L, Russo J, et al. Depressive symptoms in adolescence: The association with multiple health risk behaviors. Gen Hosp Psychiatry 2010;32:233–239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fulkerson JA, Sherwood NE, Perry CL, et al. Depressive symptoms and adolescent eating and health behaviors: A multifaceted view in a population-based sample. Prev Med 2004;38:865–875 [DOI] [PubMed] [Google Scholar]
- 5.Needham BL, Crosnoe R. Overweight status and depressive symptoms during adolescence. J Adolesc Health 2005;36:48–55 [DOI] [PubMed] [Google Scholar]
- 6.Boutelle KN, Hannan P, Fulkerson JA, et al. Obesity as a prospective predictor of depression in adolescent females. Health Psychol 2010;29:293–298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liem ET, Sauer PJ, Oldehinkel AJ, et al. Association between depressive symptoms in childhood and adolescence and overweight in later life: Review of the recent literature. Arch Pediatr Adolesc Med 2008;162:981–988 [DOI] [PubMed] [Google Scholar]
- 8.Needham BL, Epel ES, Adler NE, et al. Trajectories of change in obesity and symptoms of depression: The CARDIA study. Am J Public Health 2010;100:1040–1046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Luppino FS, de Wit LM, Bouvy PF, et al. Overweight, obesity, and depression: A systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry 2010;67:220–229 [DOI] [PubMed] [Google Scholar]
- 10.BeLue R, Francis LA, Colaco B. Mental health problems and overweight in a nationally representative sample of adolescents: Effects of race and ethnicity. Pediatrics 2009;123:697–702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goldfield GS, Moore C, Henderson K, et al. Body dissatisfaction, dietary restraint, depression, and weight status in adolescents. J Sch Health 2010;80:186–192 [DOI] [PubMed] [Google Scholar]
- 12.Pine DS, Goldstein RB, Wolk S, et al. The association between childhood depression and adulthood body mass index. Pediatrics 2001;107:1049–1056 [DOI] [PubMed] [Google Scholar]
- 13.Goodman E, Whitaker RC. A prospective study of the role of depression in the development and persistence of adolescent obesity. Pediatrics 2002;110:497–504 [DOI] [PubMed] [Google Scholar]
- 14.Marmorstein NR, Iacono WG, Legrand L. Obesity and depression in adolescence and beyond: Reciprocal risks. Int J Obes (Lond) 2014;38:906–911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Michaud CI, Khan JP, Musse N, et al. Relationships between a critical life event and eating behavior in high school students. Stress Med 1990;6:57–64 [Google Scholar]
- 16.Cartwright M, Wardle J, Steggles N, et al. Stress and dietary practices in adolescents. Health Psychol 2003;22:362–369 [DOI] [PubMed] [Google Scholar]
- 17.Jenkins SK, Rew L, Sternglanz RW. Eating behaviors among school-age children associated with perceptions of stress. Issues Compr Pediatr Nurs 2005;28:175–191 [DOI] [PubMed] [Google Scholar]
- 18.Mooreville M, Shomaker LB, Reina SA, et al. Depressive symptoms and observed eating in youth. Appetite 2014;75:141–149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bandura A. Self-Efficacy: The Exercise of Control. Prentice Hall: Englewood Cliffs, NJ, 1997 [Google Scholar]
- 20.McClain AD, Chappuis C, Nguyen-Rodriguez ST, et al. Psychosocial correlates of eating behavior in children and adolescents: A review. Int J Behav Nutr Phys Act 2009;6:54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Larson NI, Neumark-Sztainer D, Story M, et al. Whole-grain intake correlates among adolescents and young adults: Findings from Project EAT. J Am Diet Assoc 2010;110:230–237 [DOI] [PubMed] [Google Scholar]
- 22.Bruening M, Kubik MY, Kenyon D, et al. Perceived barriers mediate the association between self-efficacy and fruit and vegetable consumption among students attending alternative high schools. J Am Diet Assoc 2010;110:1542–1546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Van Der Horst K, Paw MJ, Twisk JW, et al. A brief review on correlates of physical activity and sedentariness in youth. Med Sci Sports Exerc 2007;39:1241–1250 [DOI] [PubMed] [Google Scholar]
- 24.BeLue R, Francis LA, Rollins B, et al. One size does not fit all: Identifying risk profiles for overweight in adolescent population subsets. J Adolesc Health 2009;45:517–524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Witherspoon D, Latta L, Wang Y, et al. Do depression, self-esteem, body-esteem, and eating attitudes vary by BMI among African American adolescents? J Pediatr Psychol 2013;38:1112–1120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rudolph KE, Stuart EA, Glass TA, et al. Neighborhood disadvantage in context: The influence of urbanicity on the association between neighborhood disadvantage and adolescent emotional disorders. Soc Psychiatry Psychiatr Epidemiol 2014;49:467–475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.De Cocker K, Artero EG, De Henauw S, et al. Can differences in physical activity by socio-economic status in European adolescents be explained by differences in psychosocial correlates? A mediation analysis within the HELENA (Healthy Lifestyle in Europe by Nutrition in Adolescence) study. Public Health Nutr 2012;15:2100–2109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mee S. Self-efficacy: A mediator of smoking behavior and depression among college students. Pediatr Nurs 2014;40:9–15, 37. [PubMed] [Google Scholar]
- 29.Dockray S, Susman EJ, Dorn LD. Depression, cortisol reactivity, and obesity in childhood and adolescence. J Adolesc Health 2009;45:344–350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Richardson LP, Davis R, Poulton R, et al. A longitudinal evaluation of adolescent depression and adult obesity. Arch Pediatr Adolesc Med 2003;157:739–745 [DOI] [PubMed] [Google Scholar]
- 31.Kalarchian MA, Marcus MD. Psychiatric comorbidity of childhood obesity. Int Rev Psychiatry 2012;24:241–246 [DOI] [PubMed] [Google Scholar]
- 32.Kandel DB, Davies M. Epidemiology of depressive mood in adolescents: An empirical study. Arch Gen Psychiatry 1982;39:1205–1212 [DOI] [PubMed] [Google Scholar]
- 33.Kandel DB, Raveis BH, Davies M. Suicidal ideation in adolescence: Depression, substance use, and other risk factors. J Youth Adolesc 1991;20:289–309 [DOI] [PubMed] [Google Scholar]
- 34.Neumark-Sztainer D, Wall M, Perry C, et al. Correlates of fruit and vegetable intake among adolescents. Findings from Project EAT. Prev Med 2003;37:198–208 [DOI] [PubMed] [Google Scholar]
- 35.Sallis JF, Pinski RB, Grossman RM, et al. The development of self-efficacy scales for healthrelated diet and exercise behaviors. Health Educ Res 1988;3:283–292 [Google Scholar]
- 36.Rockett HR, Berkey CS, Colditz GA. Comparison of a short food frequency questionnaire with the Youth/Adolescent Questionnaire in the Growing Up Today Study. Int J Pediatr Obes 2007;2:31–39 [DOI] [PubMed] [Google Scholar]
- 37.Rockett HR. Validity and reliability of the Youth/Adolescent Questionnaire. J Am Diet Assoc 2005;105:1867.; author reply, 1867–1868. [DOI] [PubMed] [Google Scholar]
- 38.Brener ND, Kann L, McManus T, et al. Reliability of the 1999 youth risk behavior survey questionnaire. J Adolesc Health 2002;31:336–342 [DOI] [PubMed] [Google Scholar]
- 39.Norman GJ, Schmid BA, Sallis JF, et al. Psychosocial and environmental correlates of adolescent sedentary behaviors. Pediatrics 2005;116:908–916 [DOI] [PubMed] [Google Scholar]
- 40.Zabinski MF, Norman GJ, Sallis JF, et al. Patterns of sedentary behavior among adolescents. Health Psychol 2007;26:113–120 [DOI] [PubMed] [Google Scholar]
- 41.Centers for Disease Control and Prevention, National Center for Health Statistics. 2000 CDC Growth Charts: United States. 2000. Available at www.cdc.gov/growthcharts Last accessed July30, 2014
- 42.Snijders TA, Bosker RJ. Multilevel Analysis. An Introduction to Basic and Advanced Multilevel Modeling. Sage: Thousand Oaks, CA, 1999 [Google Scholar]
- 43.MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Ann Rev Psychol 2007;58:593–614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.MacKinnon DP, Lockwood CM, Hoffman JM, et al. A comparison of methods to test mediation and other intervening variable effects. Psychol Methods 2002;7:83–104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jaser SS, Holl MG, Jefferson V, et al. Correlates of depressive symptoms in urban youth at risk for type 2 diabetes mellitus. J Sch Health 2009;79:286–292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rofey DL, Kolko RP, Iosif AM, et al. A longitudinal study of childhood depression and anxiety in relation to weight gain. Child Psychiatry Hum Dev 2009;40:517–526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Anderson SE, Murray DM, Johnson CC, et al. Obesity and depressed mood associations differ by race/ethnicity in adolescent girls. Int J Pediatr Obes 2011;6:69–78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Neissaar I, Raudsepp L. Changes in physical activity, self-efficacy and depressive symptoms in adolescent girls. Pediatr Exerc Sci 2011;23:331–343 [DOI] [PubMed] [Google Scholar]
- 49.Potochnick SR, Perreira KM. Depression and anxiety among first-generation immigrant Latino youth: Key correlates and implications for future research. J Nerv Ment Dis 2010;198:470–477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ogden CL, Carroll MD, Kit BK, et al. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 2014;311:806–814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Konttinen H, Silventoinen K, Sarlio-Lahteenkorva S, et al. Emotional eating and physical activity self-efficacy as pathways in the association between depressive symptoms and adiposity indicators. Am J Clin Nutr 2010;92:1031–1039 [DOI] [PubMed] [Google Scholar]
- 52.Carson V, Spence JC. Seasonal variation in physical activity among children and adolescents: A review. Pediatr Exerc Sci 2010;22:81–92 [DOI] [PubMed] [Google Scholar]
- 53.Nillni YI, Rohan KJ, Rettew D, et al. Seasonal trends in depressive problems among United States children and adolescents: A representative population survey. Psychiatry Res 2009;170:224–228 [DOI] [PubMed] [Google Scholar]
- 54.Engstrom M, Lee R, Ross R, et al. Children's Mental Health Needs Assessment in the Bronx. New York City Department of Health and Mental Hygiene, Division of Mental Hygiene, Bureau of Planning Evaluation and Quality Improvement: New York, 2003 [Google Scholar]
- 55.The Children's Health Fund. Mental health care in New York State: Prescriptions for policy change. Available at www.childrenshealthfund.org/sites/default/files/Mental-Health-WhitePaper-March-2008-final.pdf Last accessed June20, 2014
- 56.Lovasi GS, Hutson MA, Guerra M, et al. Built environments and obesity in disadvantaged populations. Epidemiol Rev 2009;31:7–20 [DOI] [PubMed] [Google Scholar]
- 57.Galea S, Ahern J, Nandi A, et al. Urban neighborhood poverty and the incidence of depression in a population-based cohort study. Ann Epidemiol 2007;17:171–179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Nutsford D, Pearson AL, Kingham S. An ecological study investigating the association between access to urban green space and mental health. Public Health 2013;127:1005–1011 [DOI] [PubMed] [Google Scholar]
- 59.Galea S, Ahern J, Rudenstine S, et al. Urban built environment and depression: A multilevel analysis. J Epidemiol Community Health 2005;59:822–827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Eaton DK, Kann L, Kinchen S, et al. Youth risk behavior surveillance—United States, 2007. MMWR Surveill Summ 2008;57:1–131 [PubMed] [Google Scholar]
- 61.Thomas JF, Temple JR, Perez N, et al. Ethnic and gender disparities in needed adolescent mental health care. J Health Care Poor Underserved 2011;22:101–110 [DOI] [PMC free article] [PubMed] [Google Scholar]