Abstract
Objective
To review systematic reviews and meta-analyses of integrated care programmes in chronically ill patients, with a focus on methodological quality, elements of integration assessed and effects reported.
Design
Meta-review of systematic reviews and meta-analyses identified in Medline (1946–March 2012), Embase (1980–March 2012), CINHAL (1981–March 2012) and the Cochrane Library of Systematic Reviews (issue 1, 2012).
Main Outcome Measures
Methodological quality assessed by the 11-item Assessment of Multiple Systematic Reviews (AMSTAR) checklist; elements of integration assessed using a published list of 10 key principles of integration; effects on patient-centred outcomes, process quality, use of healthcare and costs.
Results
Twenty-seven systematic reviews were identified; conditions included chronic heart failure (CHF; 12 reviews), diabetes mellitus (DM; seven reviews), chronic obstructive pulmonary disease (COPD; seven reviews) and asthma (five reviews). The median number of AMSTAR checklist items met was five: few reviewers searched for unpublished literature or described the primary studies and interventions in detail. Most reviews covered comprehensive services across the care continuum or standardization of care through inter-professional teams, but organizational culture, governance structure or financial management were rarely assessed. A majority of reviews found beneficial effects of integration, including reduced hospital admissions and re-admissions (in CHF and DM), improved adherence to treatment guidelines (DM, COPD and asthma) or quality of life (DM). Few reviews showed reductions in costs.
Conclusions
Systematic reviews of integrated care programmes were of mixed quality, assessed only some components of integration of care, and showed consistent benefits for some outcomes but not others.
Keywords: integrated healthcare, health services research, quality improvement, chronic conditions, systematic review
Introduction
Integration within and between outpatient and inpatient sectors and collaboration between physicians and other healthcare professionals are central to high-quality patient care [1]. Due to the massive increase in highly specialized diagnostic and therapeutic approaches in recent decades, effective multidisciplinary collaboration has become both increasingly important and increasingly difficult [2]. Lack of integration can make care processes incoherent, redundant or error prone. Integration of care is particularly salient in patients with chronic and multi-morbid disease, who require consistent management over long periods of time [3].
Despite increasing interest, a widely accepted definition of ‘integrated care’ is lacking at present. A comprehensive review of the literature identified close to 180 definitions of terms and concepts that are relevant to one or several aspects of integration of care [4]. This situation has been described as ‘the imprecise hodgepodge of integrated care’ [5]. Integrated care covers a variety of different concepts and programmes intended to foster coordination within and between healthcare organizations, with the goal to improve the experience of patients, the outcomes of care and enhance overall efficiency of health systems [6].
It is important to distinguish between integrated care and integration: integrated care is an organizing principle for care delivery; integration describes the methods, processes and models to achieve such delivery of care [6]. Important dimensions of integration include (i) the ‘orientation of integration’ (horizontal integration, where similar professionals or care organizations at the same level of care join together and vertical integration, where professionals or care organizations align over several levels with upstream and downstream care providers), (ii) the ‘type of integration’ (e.g. institutional or service integration) and (iii) the ‘focus of integration’ (e.g. patients with specific chronic diseases). Ten principles of successfully integrated healthcare systems, which define key areas for restructuring, organizational flexibility and adaptation to local context, have been proposed by Suter et al. [7]. Table 1 summarizes and illustrates these key principles.
Table 1.
Ten key principles for successful health systems integration
| Principle | Implementation example |
|---|---|
| 1. Comprehensive services across the continuum of care | Integrated health systems are responsible from primary through to tertiary care and closely cooperate with social care organizations |
| 2. Patient focus | Service planning and information management are driven by needs assessments and processes designed to improve patient satisfaction and outcomes |
| 3. Geographic coverage and rostering | The system takes responsibility for a clearly defined population in a geographic area, but people can seek services from other providers if they wish |
| 4. Standardized care delivery through inter-professional teams | Best practice guidelines, clinical care pathways and decision-making tools standardize and enhance quality of care; the use of electronic information systems facilitates effective communication |
| 5. Performance monitoring | Monitoring systems measure care processes and outcomes at different levels and are linked to reward systems to promote the delivery of cost-effective high-quality care |
| 6. Information systems | Computerized information systems allow effective tracking of utilization and outcome data across the continuum of care and serve consumers, payers and providers |
| 7. Organizational culture and leadership | Committed leadership brings different cultures together, promotes the vision and mission of integration, and helps staff to take ownership of the process |
| 8. Physician integration | Physicians are effectively integrated at all levels of the system and play leadership roles in the design, implementation and operation of the health system |
| 9. Governance structure | Governance structures promote integration through representation of stakeholder groups involved in the delivery of healthcare along its continuum, including physicians and the community |
| 10. Financial management | Financing mechanisms allow pooling of funds across services, for example, through global capitation, which pays for all insured health and some social services required by the enrolled population. |
Adapted from Suter et al. [7].
Several systematic reviews have investigated the effectiveness of integrated care programmes for chronic disease patients. A 2005 review of 13 such systematic reviews concluded that integrated care programmes have positive effects on the quality of care, but that diverse and inaccurate definitions of integrated care made interpretation difficult [8]. We updated the previous review with a focus on the methodological quality of relevant systematic reviews and meta-analyses, and the elements of integration assessed in the different reviews, based on 10 key principles of integrated healthcare (Table 1).
Methods
Our study followed recommendations for systematic reviews of healthcare interventions [9], which are also called meta-reviews. It was based on clearly defined inclusion criteria, a comprehensive search of the literature, assessment of the methodological quality of eligible reviews and a synthesis and critical appraisal of the evidence.
Inclusion criteria
We included published systematic reviews and meta-analyses on the effects of integrated care programmes in adult patients with chronic non-communicable diseases, except addiction and mental disorders. We defined systematic reviews as reviews that had been prepared using a systematic approach, in an attempt to minimize biases and random errors, which was documented in the Materials and methods section. We defined meta-analyses as reviews that statistically combined the results of different primary studies to obtain an overall estimate of effects [10]. We pragmatically defined integration of healthcare as the provision of multidisciplinary interventions at different stages of the care process in two or more different institutional areas [3]. We also included reviews that reported on transition of services and end-of-life care.
Outcomes
Outcomes of interest were patient-centred outcomes, process quality, use of healthcare resources and costs. Patient-centred outcomes were defined as outcomes from medical care that people care about, such as survival, function, symptoms and health-related quality of life, as proposed by the Patient-Centered Outcomes Research Institute (PCORI, see www.pcori.org).
Study identification and search strategy
We performed a comprehensive search in OVID Medline (1946–March 2012), Embase (1980–March 2012), CINHAL (1981–March 2012) and The Cochrane Database of Systematic Reviews, which includes all reviews done by the Cochrane Effective Practice and Organisation of Care Group (EPOC). The searches included a combination of MeSH terms, text words, free text terms and synonyms for integrated care programmes and chronic conditions (see Supplementary Table S1). The searches were not restricted by age, language, publication date or country. We identified additional articles by hand-searching the reference lists of the included reviews.
Selection and quality assessment of reviews
Two authors independently screened titles and abstracts and assessed the full texts of potentially eligible abstracts for inclusion. Differences were resolved in discussion or consensus with a third author. We used the 11-item Assessment of Multiple Systematic Reviews (AMSTAR) instrument to assess the methodological quality of systematic reviews, which is recommended for this purpose [9, 11]. Two authors carried out independent assessments and resolved differences in discussion with a third author.
Assessment of integrated care programmes and outcomes
We extracted the components of integrated care assessed by the different reviews using the list of 10 key principles of organizational integration in healthcare (Table 1) [7]. For example, patient focus is demonstrated by needs assessments that translate into service planning and information management and internal processes to improve patient satisfaction and outcomes. Patient focus also encourages patient engagement and participation with opportunities for input on various levels [7]. We assessed reviews and examined whether or not one or more of these aspects had been assessed.
We grouped outcomes as follows: clinical (e.g. morbidity, symptoms, disease control and mortality), functional (e.g. functional status, exercise capacity and level of disability), patient-reported (e.g. patient satisfaction, quality of life, health literacy and patient preferences), process (e.g. adherence to treatment guidelines, treatment compliance, physician behaviour and contact with services), use of healthcare resources (e.g. hospital admissions and re-admissions, visits to general practitioners or emergency departments) and costs (direct and indirect costs to patients, payers or society).
Data extraction and synthesis
We designed standardized data collection forms, piloted and revised them and extracted information on the bibliographic details of the review, study designs and operational definition of integrated care considered in the systematic reviews, the study populations and outcomes. We classified primary studies as randomized controlled trials (RCTs), non-randomized studies with concurrent control groups, before–after studies, ecological studies or as other observational studies. Two authors extracted the data and one author cross-checked all extracted data. Differences were resolved in discussion. All data were extracted from the systematic reviews; we did not extract any data from individual study reports. Data were analysed using descriptive statistics (median, range and percentage). The number of reviews indicating a beneficial effect over all reviews assessing the outcome was tabulated by outcome and disease area. No meta-analysis was performed.
Results
Identification of eligible reviews
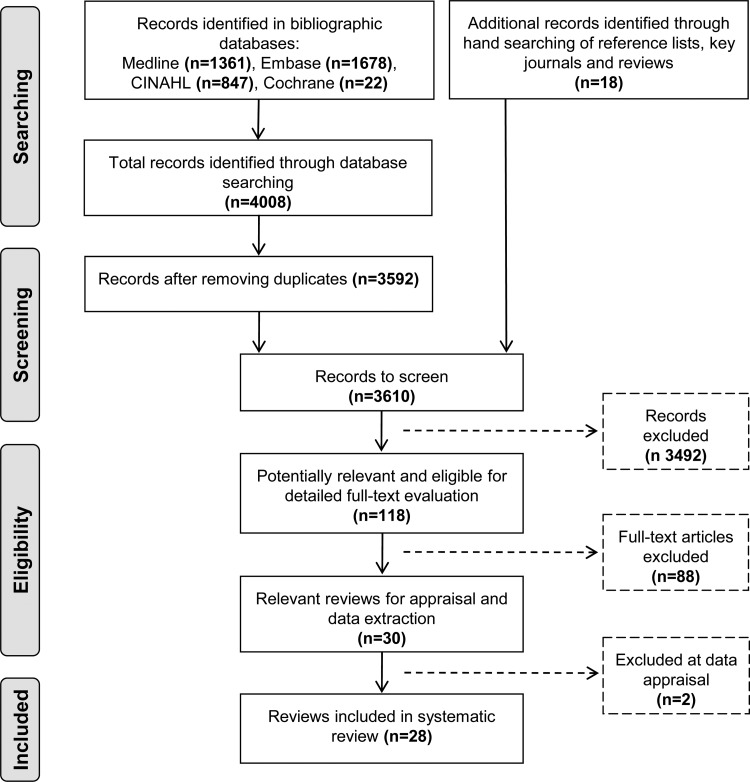
Our searches of electronic databases and reference lists identified a total of 3610 unique citations; of whom, 3492 were excluded based on titles and abstracts. The full text of 118 articles were examined in detail. After excluding 90 articles (see Supplementary Appendix for bibliographic details), 27 reviews, reported in 28 publications, met inclusion criteria. Of those, 26 were published in English [12–37] and one in German [38]. Figure 1 shows the flow of study selection.
Figure 1.
Study selection process.
Characteristics of reviews
The 27 reviews were published from 1997 to 2012; the median year of publication was 2005 (Table 2). Nineteen reviews reported the total number of study participants; this number ranged from 669 to 35 484 patients. Chronic heart failure (CHF; n = 12) was the most common medical condition examined, followed by diabetes mellitus (DM; n = 7), chronic obstructive pulmonary disease (COPD; n = 7), asthma (n = 5), hypertension (n = 3), cancer (n = 2) and rheumatoid arthritis (n = 2). Seventeen reviews (63%) included both RCTs of integrated care interventions and studies where comparisons were not randomized; seven reviews (26%) exclusively focused on RCTs and three reviews did not report the type of studies they included. Eighteen reviews (68.0%) included a meta-analysis to statistically combine results of primary studies. A detailed description of the 27 reviews, with disease area, terms used to describe integrated care, specific aims and conclusions, is given in Supplementary Table S2.
Table 2.
Characteristics of 27 systematic reviews of integrated care
| Characteristic | |
|---|---|
| Year of publication | 2005 (1997–2012) |
| Total no. of studies included (range per review) | 824 (4–112) |
| RCTsa | 480 (1–93) |
| Studies with concurrent control groupsa | 90 (1–27) |
| Before–after studiesa | 41 (2–8) |
| Ecological studiesa | 1 (0–1) |
| Other observational studiesa | 25 (1–6) |
| Review included meta-analysis | 18 (67%) |
| Methodological quality | |
| Median no. of AMSTAR items met (range) | 5 (0–10) |
| Disease areas | |
| CHF | 12 (44%) |
| DM | 7 (26%) |
| COPD | 7 (26%) |
| Asthma | 5 (19%) |
| Hypertension | 3 (11%) |
| Cancer | 2 (7%) |
| Rheumatoid arthritis | 2 (7%) |
| Otherb | 5 (19%) |
| Principles of integration assessed | |
| Comprehensive services across the care continuum | 26 (96%) |
| Standardized care through inter-professional teams | 25 (93%) |
| Patient focus | 22 (81%) |
| Performance management | 17 (63%) |
| Physician integration | 15 (56%) |
| Information systems | 13 (48%) |
| Organizational culture and leadership | 5 (19%) |
| Geographic coverage and rostering | 1 (4%) |
| Governance structure | 1 (4%) |
| Financial management | 0 (0%) |
| Outcomes assessed | |
| Use of healthcare resources | 20 (74%) |
| Patient-centred | 16 (59%) |
| Functional | 16 (59%) |
| Costs | 15 (56%) |
| Process | 11 (41%) |
| Clinical | 10 (37%) |
AMSTAR, Assessment of Multiple Systematic Reviews instrument.
aTwenty-four reviews assessed the design of primary studies.
bStroke, orthopaedics, osteoarthritis, respiratory disease, angina, back pain and chronic pain, angina, hyperlipidaemia and coronary artery disease.
‘Disease management’ was the most frequently used term for integrated care. Other terms included ‘case management’, ‘shared care’, ‘managed care’, ‘comprehensive care’, ‘multidisciplinary care’, ‘organised and coordinated care’, ‘team care’, ‘managed care cooperation’ and ‘chronic care models’ (Supplementary Table S2). Among the 10 key principles, comprehensive services across the care continuum, patient focus and standardized care delivery through inter-professional teams were assessed in most reviews, and performance management, information systems and physician integration in about half of reviews (Table 2). Fifteen reviews (56%) evaluated five or more of the principles. Only one review focused on organizational culture and leadership and governance structure [24]. A description of the integrated care programmes and outcomes evaluated in the reviews is available in Supplementary Table S3. Unfortunately, the description of the programmes and interventions was often superficial and incomplete, hampering a detailed assessment of the different components and interventions. Supplementary Table S4 lists the key principles of integrated care assessed based on the information provided in the reviews.
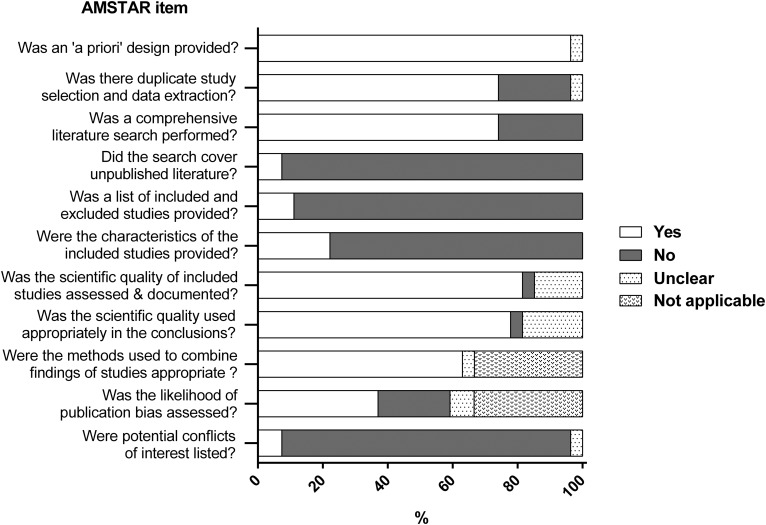
The methodological and reporting quality of reviews varied widely. The median number of AMSTAR criteria met was 5. Reporting was very poor for one review [31]; none of the criteria was clearly met. A Cochrane review met 10 of the 11 criteria [34]. Six reviews scored on eight to nine criteria [12, 17, 18, 29, 30, 32, 39]. The assessments of the methodological quality by AMSTAR item are shown in Fig. 2 and Table 3. Twenty-six reviews (96%) defined a priori research questions and inclusion criteria, 20 (74%) employed duplicate study selection and data extraction, 20 (74%) did a comprehensive literature search, 2 (7%) searched for grey or non-English literature, 3 (11%) provided a list of included and excluded studies, 6 (22%) described the characteristics of the included studies, 22 (82%) assessed and documented their quality and 21 (78%) used the data on the quality of primary studies appropriately when formulating conclusions. Seventeen of 18 meta-analyses (94%) used appropriate statistical methods and 10 (56%) assessed publication bias. Finally, two reviews (7%) considered potential conflicts of interest.
Figure 2.
Proportion of systematic reviews that addressed each of the methodological quality items of the AMSTAR tool; based on 27 included systematic reviews.
Table 3.
Quality of systematic reviews and meta-analyses based on the 11-item AMSTAR tool
| Review | Was an a priori design provided? | Was there duplicate study selection and data extraction? | Was a comprehensive literature search performed? | Did the search cover unpublished literature? | Was a list of included and excluded studies provided? | Were the characteristics of the included studies provided? | Was the scientific quality of included studies assessed and documented? | Was the scientific quality used appropriately in formulating conclusions? | Were the methods used to combine findings of studies appropriate? | Was the likelihood of publication bias assessed? | Were potential conflicts of interest listed? |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Adams et al. [12] | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Yes | Yes | No |
| Badamgarav et al. [13] | Yes | Yes | Yes | No | No | No | Unclear | Unclear | Yes | Yes | No |
| Boult et al. [14] | Yes | Yes | No | No | No | No | Yes | Yes | Not applicable | Not applicable | No |
| Elissen et al. [15] | Yes | Yes | Yes | No | No | No | Yes | Yes | Yes | No | No |
| Gensichen et al. [38] | Yes | Yes | No | No | No | No | Yes | Yes | Yes | No | No |
| Gohler et al. [16] | Yes | No | No | No | No | No | Yes | Yes | Yes | Yes | No |
| Gonseth et al. [17] | Yes | Yes | Yes | No | Yes | No | Yes | Yes | Yes | Yes | No |
| Higginson et al. [18] | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Yes | No |
| Knight et al. [19] | Yes | Yes | Yes | No | No | No | Yes | Yes | Yes | Yes | No |
| Lemmens et al. [20] | Yes | Yes | No | No | No | Yes | Yes | Yes | Yes | No | No |
| Lemmens et al. [21] | Yes | Yes | No | No | No | No | Yes | Yes | Yes | No | No |
| McAlister et al. [22] | Yes | Yes | Yes | No | No | No | Unclear | Unclear | Yes | No | No |
| Mitchell et al. [23] | Yes | No | Yes | No | No | No | Yes | Yes | Not applicable | Not applicable | No |
| Mitchell et al. [24] | Yes | Yes | Yes | No | No | No | Yes | Unclear | Not applicable | Not applicable | No |
| Niesink et al. [25] | Yes | Yes | Yes | No | No | No | Yes | Yes | Not applicable | Not applicable | No |
| Norris et al. [26] | Yes | Yes | Yes | No | No | No | Yes | Yes | Not applicable | Not applicable | No |
| Ofman et al. [27] | Yes | Yes | Yes | No | No | No | Yes | Yes | Not applicable | Not applicable | No |
| Ouwens et al. [28] | Yes | Yes | Yes | No | No | No | Yes | Yes | Not applicable | Not applicable | No |
| Peytremann-Bridevaux et al. [29] | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Yes | Yes | No |
| Phillips et al. [30] | Yes | No | Yes | No | No | Yes | Yes | Yes | Yes | Yes | Yes |
| Rich [31] | Unclear | Unclear | No | No | No | No | Unclear | Unclear | Unclear | Unclear | Unclear |
| Smith et al. [32, 39] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | No |
| Sutherland et al. [33] | Yes | No | Yes | No | No | No | No | No | Not applicable | Not applicable | No |
| Taylor et al. [34] | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Tsai et al. [35] | Yes | No | Yes | No | No | No | Yes | Yes | Yes | Yes | No |
| Vliet Vlieland and Hazes [36] | Yes | No | No | No | No | No | Yes | Yes | Not applicable | Not applicable | No |
| Weingarten et al. [37] | Yes | Yes | Yes | No | No | No | Unclear | Unclear | Yes | Unclear | No |
Characteristics of primary studies included in reviews
A total of 824 primary studies (range: 4–112 per review) had been included in the 27 reviews. The design of studies was reported in 24 reviews: of 637 studies, 480 (75%) were described as RCTs, and 157 (25%) were studies where comparisons had not been randomized (Table 1). All but four reviews reported the setting where the primary studies were conducted. Settings varied widely from inpatient to outpatient care, and included home care, nursing home, rehabilitation centre, community hospital and secondary and tertiary care settings. A detailed description of the primary studies by review is given in Supplementary Table S5, including the number and setting of studies, the study designs and the age and gender distribution of study populations.
Outcomes
The use of healthcare resources was the most frequently examined outcome, followed by patient-reported and functional outcomes, and costs to patients, payers or society. Process-related and clinical outcomes were assessed in less than half of reviews (Table 2). The effects of integrated care found in the 27 reviews are summarized in Table 4 for CHF, diabetes mellitus, COPD and asthma. For outcome assessed in at least two reviews, the table shows the number of reviews that assessed the outcome, and number of reviews that showed a statistically significant (P < 0.05) beneficial effect or trend in the direction of benefit. For CHF, the majority of relevant reviews reported that integrated care programmes reduced mortality and hospital admissions and readmissions, as well as visits to the emergency department. For diabetes mellitus, the majority of reviews showed that glycaemic control, adherence to treatment guidelines and quality of life were improved, and hospital admissions reduced. Similarly, for COPD, reviews showed an improvement in the adherence to treatment guidelines, a reduction in hospital readmissions and length of hospital stays, and a reduction in visits to the emergency department. For asthma, all relevant reviews indicated an improvement in the adherence to treatment guidelines and two of the three reviews showed a reduction in hospital admissions. Of note, few reviews found that costs were reduced and no review found any evidence of harm of integrated care programmes (Table 4).
Table 4.
Results of 27 systematic reviews of integrated care for different conditions and outcomes
| No. of reviews with improved outcome/no. of reviews assessing outcomea |
||||
|---|---|---|---|---|
| Outcome | CHF (12 reviews) | Diabetes (7 reviews) | COPD (7 reviews) | Asthma (5 reviews) |
| Clinical | ||||
| Improved glycaemic control | 4/7 | |||
| Improved blood pressure control | 1/4 | |||
| Reduced mortality | 5/8 | 0/3 | ||
| Functional | ||||
| Improved exercise capacity/functionb | 2/2 | 2/3 | 2/4 | 1/3 |
| Patient centred | ||||
| Improved quality of life | 4/8 | 4/5 | 0/5 | 1/2 |
| Higher patient satisfaction | 0/2 | 4/4 | 2/2 | 1/2 |
| Process of care | ||||
| Improved adherence to treatment guidelinesc | 2/5 | 4/6 | 3/3 | 5/5 |
| More regular retinal and foot examinations | 3/7 | |||
| Use of healthcare resources | ||||
| Reduced hospital admissions | 4/6 | 2/3 | 2/5 | 2/3 |
| Reduced readmissions | 5/9 | 2/3 | ||
| Reduced re-admissions or mortality | 2/2 | |||
| Increased time between discharge and readmission | 1/3 | |||
| Reduced length of hospital stay | 4/8 | 1/1 | 4/4 | |
| Reduced number of ED visits | 2/3 | 1/3 | 2/3 | 1/2 |
| Increased use of appropriate medication | 0/2 | |||
| Costs | ||||
| Reduced costs of services | 1/8 | 1/4 | 0/3 | 1/2 |
Only outcomes assessed by at least two reviews are shown.
LDL, low density lipoprotein; ED, emergency department; CHF, chronic heart failure; COPD, chronic obstructive pulmonary disease.
aNumber of reviews showing positive trends or significant (P < 0.05) improvements associated with integrated care models over the number of reviews that examined this outcome.
bExercise capacity, physical activity, functional status, lung function, forced expiratory volume in 1 s (FEV1).
cAdherence to treatments or diets, provider adherence to guidelines including the screening for risk factors or conditions, improved patient self-care and knowledge as a result of improved adherence of providers to guidelines.
Discussion
Summary of main findings
In this meta-review of reviews, we identified 27 systematic reviews of studies comparing integrated care interventions with usual care. Reviewers found beneficial effects of integration of care on several outcomes, including reduced mortality, reduced hospital admissions and re-admissions, improved adherence to treatment guidelines and quality of life. Of note, there was little evidence for a reduction in direct or indirect costs. The methodological and reporting quality of these reviews was mixed: only a minority of reviews searched for unpublished literature and described the included studies in detail, and not all meta-analyses addressed publication bias. However, most reviewers had performed a comprehensive search of electronic databases, had clearly defined inclusion criteria, selected eligible studies in duplicate and assessed the methodological quality of individual studies. The reviews generally assessed only few of the principles of integrated healthcare systems proposed in 2009 (Table 1) [7]. The use of information systems to track utilization and assess outcomes was examined in less than half of reviews, only five reviews considered organizational cultures and leadership and no review assessed financing mechanisms. This is perhaps not surprising considering that many of the reviews were done before the 10 principles were published [7]. Furthermore, the limited number of components assessed probably reflects poor reporting of integrated care interventions in the individual studies.
Strengths and weaknesses of this meta-review
Systematic reviews are ‘studies of studies’. They may focus on any type of study, including, for example, randomized drug trials, accuracy studies of diagnostic tests or randomized or non-randomized comparative studies of integrated care programmes [10]. Systematic reviews and meta-analyses have become increasingly important since the 1990s, with thousands of such reviews published every year. For example, a search in March 2014 of PubMed with free text words ‘meta-analysis’ and ‘systematic reviews’ in the title returned 11 320 items for 2013 alone. This means that decision makers are now confronted with many different reviews, including, as demonstrated here, in the field of integrated care. Meta-reviews of systematic reviews are, therefore, a logical next step [9]. Indeed, the Cochrane Collaboration introduced reviews of Cochrane reviews in 2009 [40]. Methodological standards for such meta-reviews have been proposed, which closely follow the principles and procedures established for systematic reviews of primary studies [9]. They share the well-documented advantages of systematic reviews over the traditional, narrative approach to reviewing [10].
The present meta-review was based on clearly defined inclusion criteria, a comprehensive search of the literature and included an assessment of the methodological quality of eligible reviews and a qualitative synthesis and critical appraisal of the evidence. A particular strength of our review is that we examined to what extent reviews assessed interventions with respect to the 10 key principles of health systems integration proposed by Suter et al. [7]. We felt that these principles were suitable for this purpose because they comprehensively cover the concepts of integrated care and are applicable to a broad range of integrated care programmes. We restricted our study to systematic reviews and meta-analyses, and excluded narrative reviews. However, the incomplete assessment of the nature of interventions did not allow us to identify the components of care integration that are most strongly associated with beneficial outcomes. We stress that the 10 principles proposed by Suter et al. [7] for successful health systems integration are plausible, but at present they lack a strong empirical evidence base.
Findings in context with other reviews
The present review was inspired by the 2005 overview by Ouwens et al. [8] which used closely similar inclusion criteria and focused on definitions and components of integrated care programmes. Our focus was on the methodological quality of systematic reviews and the a priori list of 10 key components of integrated healthcare [7]. Furthermore, we identified 27 systematic reviews compared with the 13 reviews included in Ouwens et al.'s study [8].
Several recent meta-reviews have used the AMSTAR instrument [11] when assessing the quality of systematic reviews. For example, Parker et al. [41] obtained a median number of positive answers of 6 (range 0–11) among 27 systematic reviews of interventions in maternal anaemia, Brouwers et al. [42] a median number of 7 (range 3–11) for 17 systematic reviews of knowledge translation interventions in cancer control and Hemming et al. [43] a median number of 6 (range 0–9) for reviews of studies comparing staples with sutures in surgery. Although the AMSTAR checklist was not intended by the authors as a quality score [11], it is increasingly used in this way. For example, Parker et al. defined high quality as ≥9, intermediate quality as 5–8 and low quality as ≤4 positive answers. This is problematic for several reasons. Scores are not strictly comparable across reviews because they depend on whether or not the systematic review included a meta-analysis: 2 of the 11 AMSTAR items are only applicable to meta-analyses. Reviewers may have taken the well-considered and appropriate decision not to do a meta-analysis, for example, because of pronounced heterogeneity in study populations, interventions and results. It is a limitation of AMSTAR that the way reviewers dealt with heterogeneity and the appropriateness of doing a meta-analysis is not covered by the instrument. Furthermore, a score gives the same weight to all items; however, their importance may well vary between systematic reviews. For example, conflicts of interest may be more important for drugs than other interventions, and some items in AMSTAR measure the quality of reporting, rather than methodological quality. This issue has been discussed in depth in the context of scoring the quality of RCTs [44, 45].
Conclusions
Our meta-review adds to a growing body of evidence showing that integrated care programmes can improve patient-centred outcomes, process quality and reduce the use of some healthcare resources in chronic diseases such as CHF, diabetes mellitus or COPD. However, it is unclear which components or interventions should be prioritized in integrated care programmes to maximize their benefit. The present and an earlier meta-review [8] fail to shed light on this important question. Future studies of integrated care should provide a detailed description of the components and interventions of integrated care examined, so that study results can be interpreted and interventions replicated. Guidelines for the reporting of complex interventions in healthcare have recently been proposed [46] and may contribute to improving the reporting of comparative studies of integrated care in the future. Systematic reviews and meta-reviews can then be used to identify the components associated with beneficial outcomes within and across different chronic diseases.
Ethical approval is not required for this study.
What is already known on this topic
There is great interest in integration of care, but dimensions of integration, patient populations and medical conditions vary widely across studies.
Many systematic reviews of studies of integrated care programmes in chronic diseases have been done.
What this study adds
This meta-review of 27 systematic reviews of integrated care programmes showed that the methodological quality was mixed: few reviews searched for unpublished literature or described the primary studies and interventions in detail.
The reviews generally assessed only some of the key components of integrated healthcare systems; organizational culture or governance structure were rarely considered.
Benefits of integrated care consistently shown in reviews included reduced use of healthcare resources and improved adherence to treatment guidelines. Few reviews showed reductions in costs.
Supplementary material
Funding
This work was supported by the Swiss Federal Office of Public Health (SFOPH). By contractual agreement, the SFOPH had no involvement in the preparation of the present manuscript. Funding to pay the Open Access publication charges for this article was provided by the Swiss Forum Managed Care.
Supplementary Material
Acknowledgements
We are grateful to Doris Kopp and Beatrice Minder for their help with searching the literature. This study is dedicated to the memory of André Busato who initiated this project.
References
- 1.Leape L, Berwick D, Clancy C, et al. Transforming healthcare: a safety imperative. Qual Saf Health Care. 2009;18:424–8. doi: 10.1136/qshc.2009.036954. [DOI] [PubMed] [Google Scholar]
- 2.Glouberman S, Mintzberg H. Managing the care of health and the cure of disease—Part I: differentiation. Health Care Manage Rev. 2001;26:56–69. doi: 10.1097/00004010-200101000-00006. discussion 87–9. [DOI] [PubMed] [Google Scholar]
- 3.Strandberg-Larsen M, Krasnik A. Measurement of integrated healthcare delivery: a systematic review of methods and future research directions. Int J Integr Care. 2009;9:e01. doi: 10.5334/ijic.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Suter E, Oelke ND, Adair CE, et al. Health Systems Integration. Definitions, Processes & Impact: A Research Synthesis. Ottawa: Canadian Institutes of Health Research; 2007. [Google Scholar]
- 5.Kodner DL. All together now: a conceptual exploration of integrated care. Healthc Q. 2009;13(Spec No):6–15. doi: 10.12927/hcq.2009.21091. [DOI] [PubMed] [Google Scholar]
- 6.Shaw S, Rosen R, Rumbold B. What Is Integrated Care? A Research Report. London: Nuffield Trust; 2011. [Google Scholar]
- 7.Suter E, Oelke ND, Adair CE, et al. Ten key principles for successful health systems integration. Healthc Q. 2009;13(Spec No):16–23. doi: 10.12927/hcq.2009.21092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ouwens M, Wollersheim H, Hermens R, et al. Integrated care programmes for chronically ill patients: a review of systematic reviews. Int J Qual Health Care. 2005;17:141–6. doi: 10.1093/intqhc/mzi016. [DOI] [PubMed] [Google Scholar]
- 9.Smith V, Devane D, Begley CM, et al. Methodology in conducting a systematic review of systematic reviews of healthcare interventions. BMC Med Res Methodol. 2011;11:15. doi: 10.1186/1471-2288-11-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Egger M, Smith GD, Altman DG. Systematic Reviews in Healthcare: Meta-analysis in Context. London: BMJ Books; 2001. [Google Scholar]
- 11.Shea BJ, Hamel C, Wells GA, et al. AMSTAR is a reliable and valid measurement tool to assess the methodological quality of systematic reviews. J Clin Epidemiol. 2009;62:1013–20. doi: 10.1016/j.jclinepi.2008.10.009. [DOI] [PubMed] [Google Scholar]
- 12.Adams SG, Smith PK, Allan PF, et al. Systematic review of the chronic care model in chronic obstructive pulmonary disease prevention and management. Arch Intern Med. 2007;167:551–61. doi: 10.1001/archinte.167.6.551. [DOI] [PubMed] [Google Scholar]
- 13.Badamgarav E, Croft JD, Jr, Hohlbauch A, et al. Effects of disease management programs on functional status of patients with rheumatoid arthritis. Arthritis Care Res. 2003;49:377–87. doi: 10.1002/art.11120. [DOI] [PubMed] [Google Scholar]
- 14.Boult C, Green AF, Boult LB, et al. Successful models of comprehensive care for older adults with chronic conditions: evidence for the institute of medicine's ‘Retooling for an aging America’ report. J Am Geriatr Soc. 2009;57:2328–37. doi: 10.1111/j.1532-5415.2009.02571.x. [DOI] [PubMed] [Google Scholar]
- 15.Elissen AM, Steuten LM, Lemmens LC, et al. Meta-analysis of the effectiveness of chronic care management for diabetes: investigating heterogeneity in outcomes. J Eval Clin Pract. 2012;19:753–62. doi: 10.1111/j.1365-2753.2012.01817.x. [DOI] [PubMed] [Google Scholar]
- 16.Gohler A, Januzzi JL, Worrell SS, et al. A systematic meta-analysis of the efficacy and heterogeneity of disease management programs in congestive heart failure. J Card Fail. 2006;12:554–67. doi: 10.1016/j.cardfail.2006.03.003. [DOI] [PubMed] [Google Scholar]
- 17.Gonseth J, Guallar-Castillon P, Banegas JR, et al. The effectiveness of disease management programmes in reducing hospital re-admission in older patients with heart failure: a systematic review and meta-analysis of published reports. Eur Heart J. 2004;25:1570–95. doi: 10.1016/j.ehj.2004.04.022. [DOI] [PubMed] [Google Scholar]
- 18.Higginson IJ, Finlay I, Goodwin DM, et al. Do hospital-based palliative teams improve care for patients or families at the end of life? J Pain Symptom Manage. 2002;23:96–106. doi: 10.1016/s0885-3924(01)00406-7. [DOI] [PubMed] [Google Scholar]
- 19.Knight K, Badamgarav E, Henning JM, et al. A systematic review of diabetes disease management programs. Am J Manag Care. 2005;11:242–50. [PubMed] [Google Scholar]
- 20.Lemmens KM, Nieboer AP, Huijsman R. A systematic review of integrated use of disease-management interventions in asthma and COPD (Structured abstract) Respir Med. 2009;103:670–91. doi: 10.1016/j.rmed.2008.11.017. [DOI] [PubMed] [Google Scholar]
- 21.Lemmens KMM, Lemmens LC, Boom JHC, et al. Chronic care management for patients with COPD: a critical review of available evidence. J Eval Clin Pract. 2011;19:734–52. doi: 10.1111/j.1365-2753.2011.01805.x. [DOI] [PubMed] [Google Scholar]
- 22.McAlister FA, Lawson FM, Teo KK, et al. A systematic review of randomized trials of disease management programs in heart failure. Am J Med. 2001;110:378–84. doi: 10.1016/s0002-9343(00)00743-9. [DOI] [PubMed] [Google Scholar]
- 23.Mitchell G, Del Mar C, Francis D. Does primary medical practitioner involvement with a specialist team improve patient outcomes? A systematic review. Br J Gen Pract. 2002;52:934–9. [PMC free article] [PubMed] [Google Scholar]
- 24.Mitchell GK, Brown RM, Erikssen L, et al. Multidisciplinary care planning in the primary care management of completed stroke: a systematic review. BMC Fam Pract. 2008;9:44. doi: 10.1186/1471-2296-9-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Niesink A, Trappenburg JCA, de Weert-van Oene GH, et al. Systematic review of the effects of chronic disease management on quality-of-life in people with chronic obstructive pulmonary disease. Respir Med. 2007;101:2233–9. doi: 10.1016/j.rmed.2007.07.017. [DOI] [PubMed] [Google Scholar]
- 26.Norris SL, Nichols PJ, Caspersen CJ, et al. The effectiveness of disease and case management for people with diabetes: A systematic review. Am J Prev Med. 2002;22:15–38. doi: 10.1016/s0749-3797(02)00423-3. [DOI] [PubMed] [Google Scholar]
- 27.Ofman JJ, Badamgarav E, Henning JM, et al. Does disease management improve clinical and economic outcomes in patients with chronic diseases? A systematic review. Am J Med. 2004;117:182–92. doi: 10.1016/j.amjmed.2004.03.018. [DOI] [PubMed] [Google Scholar]
- 28.Ouwens M, Hulscher M, Hermens R, et al. Implementation of integrated care for patients with cancer: a systematic review of interventions and effects. Int J Qual Health Care. 2009;21:137–44. doi: 10.1093/intqhc/mzn061. [DOI] [PubMed] [Google Scholar]
- 29.Peytremann-Bridevaux I, Staeger P, Bridevaux PO, et al. Effectiveness of chronic obstructive pulmonary disease-management programs: systematic review and meta-analysis (Structured abstract) Am J Med. 2008;121:433–43.e4. doi: 10.1016/j.amjmed.2008.02.009. [DOI] [PubMed] [Google Scholar]
- 30.Phillips CO, Wright SM, Kern DE, et al. Comprehensive discharge planning with postdischarge support for older patients with congestive heart failure: a meta-analysis. JAMA. 2004;291:1358–67. doi: 10.1001/jama.291.11.1358. [DOI] [PubMed] [Google Scholar]
- 31.Rich MW. Heart failure disease management: a critical review. J Card Fail. 1999;5:64–75. doi: 10.1016/s1071-9164(99)90026-x. [DOI] [PubMed] [Google Scholar]
- 32.Smith SM, Allwright S, O'Dowd T. Effectiveness of shared care across the interface between primary and specialty care in chronic disease management. Cochrane Database Syst Rev. 2007:CD004910. doi: 10.1002/14651858.CD004910.pub2. [DOI] [PubMed] [Google Scholar]
- 33.Sutherland D, Hayter M. Structured review: evaluating the effectiveness of nurse case managers in improving health outcomes in three major chronic diseases. J Clin Nurs. 2009;18:2978–92. doi: 10.1111/j.1365-2702.2009.02900.x. [DOI] [PubMed] [Google Scholar]
- 34.Taylor SJC, Bestall Janine C, Cotter S, et al. Clinical service organisation for heart failure. Cochrane Database Syst Rev. 2005:CD002752. doi: 10.1002/14651858.CD002752.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tsai AC, Morton SC, Mangione CM, et al. A meta-analysis of interventions to improve care for chronic illnesses. Am J Manag Care. 2005;11:478–88. [PMC free article] [PubMed] [Google Scholar]
- 36.Vliet Vlieland TP, Hazes JM. Efficacy of multidisciplinary team care programs in rheumatoid arthritis. Semin Arthritis Rheum. 1997;27:110–22. doi: 10.1016/s0049-0172(97)80011-x. [DOI] [PubMed] [Google Scholar]
- 37.Weingarten SR, Henning JM, Badamgarav E, et al. Interventions used in disease management programmes for patients with chronic illness-which ones work? Meta-analysis of published reports. BMJ. 2002;325:925. doi: 10.1136/bmj.325.7370.925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gensichen J, Beyer M, Kuver C, et al. Primary case based case management for patients with congestive heart failure—a critical review. Z Arztl Fortbild Qualitatssich. 2004;98:143–54. [PubMed] [Google Scholar]
- 39.Smith SM, Allwright S, O'Dowd T. Does sharing care across the primary-specialty interface improve outcomes in chronic disease? A systematic review (Brief record) Am J Manag Care. 2008;14:213–24. [PubMed] [Google Scholar]
- 40.Becker L, Oxman AD. Overview of reviews. In: Higgins JP, Green S, editors. Cochrane Handbook for Systematic Reviews. Oxford: The Cochrane Collaboration; 2009. Version 5.0.02 (Updated September 2009) [Google Scholar]
- 41.Parker JA, Barroso F, Stanworth SJ, et al. Gaps in the evidence for prevention and treatment of maternal anaemia: a review of systematic reviews. BMC Pregnancy Childbirth. 2012;12:56. doi: 10.1186/1471-2393-12-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Brouwers MC, Garcia K, Makarski J, et al. Evidence Expert P, Team KTfCCiCPR. The landscape of knowledge translation interventions in cancer control: what do we know and where to next? A review of systematic reviews. Implement Sci. 2011;6:130. doi: 10.1186/1748-5908-6-130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hemming K, Pinkney T, Futaba K, et al. A systematic review of systematic reviews and panoramic meta-analysis: staples versus sutures for surgical procedures. PLoS One. 2013;8:e75132. doi: 10.1371/journal.pone.0075132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Juni P, Witschi A, Bloch R, et al. The hazards of scoring the quality of clinical trials for meta-analysis. JAMA. 1999;282:1054–60. doi: 10.1001/jama.282.11.1054. [DOI] [PubMed] [Google Scholar]
- 45.da Costa BR, Hilfiker R, Egger M. PEDro's bias: summary quality scores should not be used in meta-analysis. J Clin Epidemiol. 2013;66:75–7. doi: 10.1016/j.jclinepi.2012.08.003. [DOI] [PubMed] [Google Scholar]
- 46.Mohler R, Bartoszek G, Kopke S, et al. Proposed criteria for reporting the development and evaluation of complex interventions in healthcare (CReDECI): guideline development. Int J Nurs Stud. 2012;49:40–6. doi: 10.1016/j.ijnurstu.2011.08.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.