Abstract
Background
Subsequent surgeries have a profound impact on patient satisfaction and outcome following primary anterior cruciate ligament (ACL) reconstruction (ACLR). There have been no prospective studies to date describing the rate of all subsequent knee surgeries at short- and midterm follow-up along with analysis of surgical and patient variables that are associated with subsequent surgeries.
Purpose
To report rate of all subsequent surgeries at short- and midterm follow-up, along with associated patient variables
Study Design
Prospective, Longitudinal Cohort
Methods
Nine hundred eighty patients (540 male) were prospectively enrolled in a multicenter cohort from January 2002 to December 2003. Two- and 6-year follow-up for subsequent procedures were obtained. Operative reports were obtained, and all procedures were recorded.
Results
One hundred eighty-five patients had a subsequent surgery on the ipsilateral leg (18.9%) and 100 on the contralateral knee (10.2%) at 6-year follow-up. On the ipsilateral knee, there was a 7.7% rate of ACL revisions, 13.3% rate of cartilage procedures, 5.4% rate of arthrofibrosis procedures, and 2.4% rate of procedures related to hardware. For the contralateral knee, there was a 6.4% rate of primary ACL ruptures.
Conclusions
At 6-year follow-up 18.9% of ACLR patients underwent subsequent surgeries on the ipsilateral knee. The ipsilateral ACLR graft vs. contralateral normal ACL tear was similar (7.7% vs. 6.4%). Younger age at index surgery and the use of allograft were risk factors for subsequent surgery. Revision ACLR, female sex, body mass index (BMI), and surgical exposure were not significant.
Key Terms: Anterior cruciate ligament reconstruction, subsequent surgery
Introduction
Anterior cruciate ligament (ACL) injury is a common athletic injury. ACL reconstructions (ACLR) are also common, with an estimated 175,000–200,000 occurring annually in the United States alone.10,12
Subsequent surgeries, on the ipsilateral and contralateral leg, effect patient satisfaction and outcome following ACLR. In addition to effects on patient outcome, there is a significant cost associated with subsequent surgeries, and the rate of these procedures needs to be known for patient education, as well as future quality and comparative effectiveness analyses.
A meta-analysis of prospective studies looking at the rate of ipsilateral graft and contralateral ACL rupture at a minimum of five years following ACLR found that the ipsilateral ACL graft rupture rate ranged from 1.8% to 10.4% (pooled percentage of 5.8%) and the contralateral injury rate ranged from 8.2% to 16.0% (pooled percentage of 11.8%).13 Predictors of these injuries could not be determined.
The importance of subsequent surgery data can be seen in the Knee Anterior Cruciate Ligament, Nonsurgical versus Surgical Treatment (KANON) Study.6 At early follow-up in this study, there were equivalent knee outcome scores (KOOS) between the early ACLR group (surgery within 10 weeks) and the group undergoing structured rehabilitation plus optional delayed ACLR. However, 23/62 patients in the rehabilitation group opted for delayed ACLR, and there were more meniscal procedures in the rehabilitation group (50 vs. 40). The early ACLR group had more subsequent procedures (13 vs. 4); however, they had almost double the length of follow-up from ACLR. In a comparative effectiveness study using the KANON data, the early ACLR was determined to be more cost effective (unpublished data, 2012).8
There have been no prospective studies to date describing the rate and predictors of all subsequent surgeries at short- and midterm follow-up. Our aim was to describe these from our multicenter prospective cohort study.
Methods
Study Design
Nine hundred eighty patients were enrolled between January 2002 and December 2003 as part of a multicenter prospective longitudinal cohort study. IRB approval was obtained, and all patients who underwent ACLR at 6 sites were targeted for enrollment in 2002 and 2003.
Data Sources and Measurement
After documentation of informed consent, participants completed a 13-page questionnaire examining self-reported demographics, injury characteristics, sports participation history, comorbidities, and health status. Regarding the latter, the following validated instruments were included: SF-36[Brazier BMJ 1992][Ware Med Care 1992], IKDC[Irrgang AJSM 2001], KOOS[Roos 1998 J Orthop Sports Phys Therap], which includes the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC)[Bellamy J Rheum 1988], and the Marx activity scale[Marx AJSM 2001]. This was given to the patients prior to surgery and completed within 2 weeks of the surgery date. At the time of the index surgery, surgeons completed a 49-page questionnaire that included sections on history of the knee injury and/or surgery on both knees, the findings from the general knee examination done under anesthesia, recording of all intra-articular injuries and treatments to the meniscus and articular cartilage, and the surgical technique used for the ACLR. Classification of the general knee examination findings followed the recommendations of the updated 1999 IKDC guidelines. Surgeon documentation of articular cartilage injury was recorded utilizing the modified Outerbridge classification.9 Meniscal injuries were classified by size, location, partial versus complete tears, and treatment method (not treated, repaired, or extent of resection). Completed data forms were mailed from the participating sites to the data coordinating center. Data from both the patient and surgeon questionnaires were subsequently scanned and read with Teleform software (Cardiff Software, Inc, Vista, CA) using optical character recognition to avoid manual data entry, and the scanned data were then verified and exported to a database.
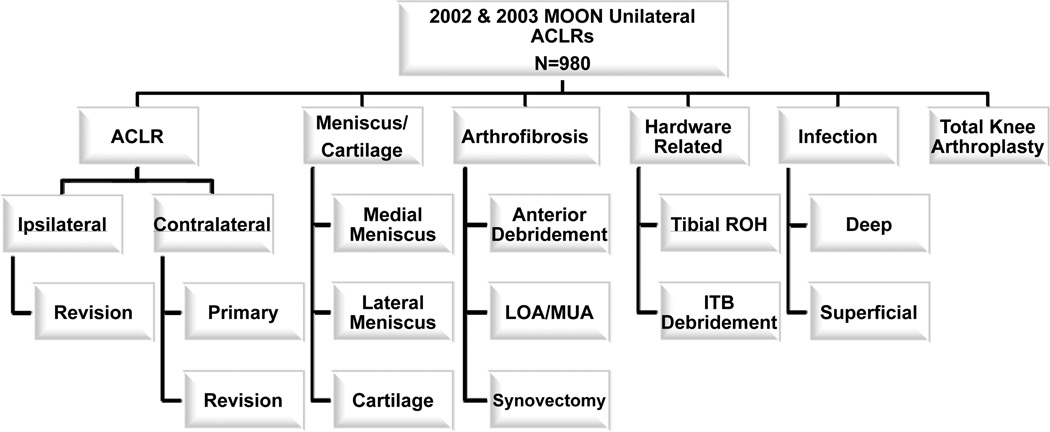
At 2- and 6-year follow-up, patients were asked if they had any subsequent surgeries on either knee. If they responded affirmatively, either on the questionnaire or by telephone, attempts were made to obtain the operative report. If an operative report could not be obtained but the patient reported an ACLR, surgery for infection, or total knee replacement (TKA), these were recorded as such. If the patient reported any other type of procedure, patient accuracy in reporting exact procedures performed was less certain, and the procedure was recorded as ”unknown.” These twenty-six “unknown”s were included in counts as subsequent procedures, but excluded from categorical analysis.. Operative reports were obtained and read, and all procedures were categorized and recorded, along with the surgical date. If multiple procedures were done during an operation, all were recorded. A diagram depicting the categories and subcategories of the subsequent procedures is shown in Figure 1.
Figure 1.
Branching diagram depicting categories and subcategories of subsequent surgical procedures. Articular cartilage procedures included chondroplasty, microfracture, autologous chondrocyte implantation, and osteochondral autograft transplantation. The meniscus categories include both meniscectomy and repair. ACLR = anterior cruciate ligament reconstruction; LOA/MUA = lysis of adhesions/manipulation under anesthesia; ITB= iliotibial band; ROH = removal of hardware.
Data regarding simultaneous bilateral ACL reconstructions, ACL avulsion repairs, or ACL reconstruction surgeries that included surgical procedures to the posterior cruciate ligament (PCL), medial collateral ligament (MCL), lateral collateral ligament (LCL) or meniscal transplants were excluded from analysis. Data from patients with prior surgery of any type to either knee, including ACL reconstruction on the contralateral knee, were included.
Study Size
Sample size considerations guided variable selection to generate a model as complex as the data would allow without overfitting the data using the ratio p = m/10 as the minimum acceptable ratio for reliable models (p = number of parameters in model; m = effective sample size).
To examine the association between subsequent surgeries and risk factors, a logistic regression model was used in which the dependent variable was the presence or absence of a subsequent surgery, and independent variables were age, body mass index (BMI), sex, graft choice (BTB, hamstring, tibialis), femoral fixation, surgical exposure, and allograft vs. autograft. Interquartile range odds ratios (IQROR) are given for continuous variables, which demonstrate the effect of increasing a baseline variable from its first quartile to its third quartile. We did not assume linearity of covariate effects but only assumed smoothed relationships, using restricted cubic regression splines. Missing values of predictor variables were imputed using multiple imputation incorporating predictive mean matching and flexible additive imputation models as implemented in the aregImpute function available in the Hmisc package in R statistical software. Statistical analysis was performed with free open-source R statistical software (www.r-project.org).
Results
Nine hundred eighty patients enrolled in 2002 and 2003 were included in the study. Of these, 440 (44.9%) were female, and the median age was 25 years. Baseline patient characteristics stratified by patient sex can be seen in Table 1. Two year surgical follow-up information was obtained on 904 (92.3%) subjects. Questionnaires were obtained on 845 with a mean follow-up of 112.5 weeks +/− 10.2 weeks. An additional 59 subjects provided subsequent surgery information by phone. Of the 76 that we were unable to obtain 2 year follow-up data on, 65 were not reached, 6 refused further participation, 3 were incarcerated, and 2 had died. Six year surgical follow-up information was obtained on 905 (92.3%) subjects. Questionnaires were obtained on 858 with a mean follow-up of 349 weeks +/− 17.4 weeks (6.7 years). Phone follow-up was provided by 47, of whom 3 had TKAs and thus questionnaires were not requested. From the 75 subjects who did not provide additional surgery information, the number of those incarcerated and refusing rose to 4 and 11, respectively, although the number of the deceased remained at 2. Fifty-eight were not reached at this time point.
Table 1. Baseline Patient Characteristics by Sex.
For body mass index (BMI) and Marx activity scores there were 12 individuals with unreported data. For age, BMI, and Marx, 25th percentile, median, and 75th percentile are shown.
| Male | Female | Combined | |||||||
|---|---|---|---|---|---|---|---|---|---|
| N=540 | N=440 | N=980 | |||||||
| 25% | Median | 75% | 25% | Median | 75% | 25% | Median | 75% | |
| Age at Surgery | 18 | 25 | 35 | 17 | 21 | 33 | 17 | 23 | 34 |
| Baseline BMI* | 23.7 | 25.8 | 28.7 | 21.1 | 23.0 | 26.3 | 22.3 | 25.0 | 28.0 |
| Baseline Marx* | 8 | 12 | 16 | 8 | 12 | 16 | 8 | 12 | 16 |
| Smoke | |||||||||
| Never | 418 (77%) | 355 (81%) | 773 (79%) | ||||||
| Quit | 54 (10%) | 39 (9%) | 93 (9%) | ||||||
| Current | 63 (12%) | 43 (10%) | 106 (11%) | ||||||
| Unreported | 5 (1%) | 3 (1%) | 8 (1%) | ||||||
| Ethnicity | |||||||||
| White | 450 (83%) | 372 (85%) | 822 (84%) | ||||||
| Black | 37 (7%) | 32 (7%) | 69 (7%) | ||||||
| Asian | 16 (3%) | 15 (3%) | 31 (3%) | ||||||
| Hispanic | 3 (1%) | 6 (1%) | 9 (1%) | ||||||
| Other | 14 (3%) | 7 (2%) | 21 (2%) | ||||||
| Unreported | 20 (4%) | 8 (2%) | 28 (2%) | ||||||
| Marital Status | |||||||||
| Single | 315 (58%) | 296 (67%) | 611 (62%) | ||||||
| Married | 175 (32%) | 111 (25%) | 286 (29%) | ||||||
| Divorced | 13 (2%) | 13 (3%) | 26 (3%) | ||||||
| Separated | 6 (1%) | 2 (0%) | 8 (1%) | ||||||
| Widowed | 2 (0%) | 1 (0%) | 3 (0%) | ||||||
| Unreported | 29 (5%) | 17 (4%) | 46 (5%) | ||||||
12 unreported
Eight hundred eighty-eight (91%) of the index surgeries were primary ACLRs. The revision ACLR surgeries were included, and revision was used as an independent variable in the statistical modeling. Seven hundred fifty (77%) of the procedures used autograft tendons. All baseline knee characteristics stratified by sex are included in Table 2, including data on meniscus and ligament status at the time of index surgery.
Table 2.
Baseline knee characteristics stratified by sex.
| Male | Female | Combined | |
|---|---|---|---|
| N=540 | N=440 | N=980 | |
| Reconstruction Type | |||
| Primary | 487 (90%) | 401 (91%) | 888 (91%) |
| Revision | 53 (10%) | 39 (9%) | 92 (9%) |
| Graft Type | |||
| Autograft | 406 (75%) | 344 (78%) | 750 (77%) |
| Allograft | 134 (25%) | 94 (21%) | 228 (23%) |
| Both | 0 (0%) | 2 (<1%) | 2 (<1%) |
| Surgical Exposure | |||
| Two Incision | 181 (34%) | 128 (29%) | 309 (32%) |
| Endoscopic | 359 (66%) | 312 (71%) | 671 (68%) |
| ACL Graft Source | |||
| BTB | 276 (51%) | 195 (44%) | 469 (47%) |
| Hamstring | 169 (31%) | 174 (39%) | 343 (36%) |
| Tibialis Anterior | 93 (17%) | 72 (16%) | 165 (17%) |
| Achilles | 2 (<1%) | 1 (<1%) | 3 (<1%) |
| Medial Meniscus | |||
| Normal | 321 (59%) | 290 (66%) | 611 (62%) |
| Partial Tear | 44 (8%) | 28 (6%) | 72 (7%) |
| Complete Tear | 175 (32%) | 122 (28%) | 297 (30%) |
| Lateral Meniscus | |||
| Normal | 303 (56%) | 257 (58%) | 560 (57%) |
| Partial Tear | 53 (10%) | 55 (13%) | 108 (11%) |
| Complete Tear | 184 (34%) | 128 (29%) | 312 (32%) |
| MCL Status | |||
| Normal | 480 (89%) | 406 (92%) | 886 (90%) |
| Grade I | 28 (5%) | 14 (3%) | 42 (4%) |
| Grade II | 30 (6%) | 15 (3%) | 45 (5%) |
| Grade III | 2 (<1%) | 5 (1%) | 7 (1%) |
| LCL Status | |||
| Normal | 531 (98%) | 435 (99%) | 966 (99%) |
| Grade I | 3 (1%) | 2 (<1%) | 5 (1%) |
| Grade II | 5 (1%) | 2 (<1%) | 5 (1%) |
| Grade III | 1 (<1%) | 1 (<1%) | 2 (<1%) |
On the ipsilateral knee, 185 patients (18.9%) underwent at least one subsequent procedure. Eighty-nine (9.1%) patients had 1, 57 (5.8%) patients had 2, 24 (2.4%) patients had 3, 9 (0.9%) patients had 4, 3 (0.3%) had 5, none had 6, 1 (0.1%) had 7, and 1 (0.1%) patient had 8 subsequent procedures. One hundred patients (10.2%) underwent at least one procedure on the contralateral knee by 6-year follow-up.
On the ipsilateral knee, the rate of revision ACLR was 7.7%, medial meniscus procedures - 5.7%, lateral meniscus procedures - 3.7%, articular cartilage procedures - 3.9%, anterior debridement/cyclops - 4.2%, tibial removal of hardware - 1.3%, iliotibial band (ITB) debridement - 1.1%, and lysis of adhesions - 0.6%. The rate of procedures due to deep infections was 0.5%, with 2 patients having early infections (within 3 weeks, although 1 required multiple procedures) and 1 patient with late infection (7 months) postoperatively -- 2 of these were in tibialis allograft, 1 in hamstring autograft. Ipsilateral subsequent surgeries stratified by 2- and 6-year follow-up are listed in Table 3.
Table 3. Ipsilateral Subsequent Procedures.
Ipsilateral subsequent procedures, overall numbers and stratified to 2- and 6-year follow-up. Median time to follow-up in months is also reported. Percentages shown represent the number of each type of subsequent procedure performed divided by the number of ACL surgeries in the cohort. Thirteen of the 75 ACL revisions and 2 of the 4 TKAs were unconfirmed by operative report.
| Overall | 0 – 2 year |
2 – 6 year |
Median (months) |
|
|---|---|---|---|---|
| Revision ACLR | 75 (7.7%) | 47 (63%) | 28 (37%) | 17.1 |
| Cartilage/Meniscus | ||||
| Medial Meniscus | 56 (5.7%) | 26 (46%) | 30 (54%) | 26.0 |
| Lateral Meniscus | 36 (3.7%) | 23 (64%) | 13 (36%) | 15.6 |
| Cartilage | 38 (3.9%) | 18 (47%) | 20 (53%) | 26.4 |
| Arthrofibrosis | ||||
| Anterior Debridement | 41 (4.2%) | 30 (73%) | 11 (27%) | 13.1 |
| LOA/MUA | 6 (0.6%) | 6 (100%) | 0 | 2.2 |
| Synovectomy | 6 (0.6%) | 4 (67%) | 2 (33%) | 18.2 |
| Tibial Removal of Hardware | 13 (1.3%) | 6 (46%) | 7 (54%) | 30.3 |
| ITB Debridement | 11 (1.1%) | 10 (91%) | 1 (9%) | 5.6 |
| Deep Infection | 5 (0.5%) | 5 (100%) | 0 | 0.9 |
| TKA | 3 (0.3%) | 0 | 3 (100%) | 82.9 |
Six hundred seventy-one of the reconstructions were by single-incision technique, of which there was a 9.1% rate of revision ACL reconstruction, 15.1% rate of cartilage/meniscus procedures, 6.3% rate of procedures for arthrofibrosis, and 2.8% rate for hardware removal. Three hundred twelve were done by 2-incision technique, and rates for these surgeries were 4.5%, 9.4%, 3.6%, and 1.6%, respectively.
For the contralateral knee, there were 63 primary ACLRs (6.4%) and 5 revision ACLRs. Contralateral subsequent surgeries by 2- and 6-year follow-up are listed in Table 5.
Table 5. Contralateral Subsequent Procedures.
Contralateral subsequent procedures, overall numbers and stratified to 2- and 6-year follow-up. Median time to follow-up in months is also reported. Percentages shown represent the number of each type of subsequent procedure performed divided by the number of ACL surgeries in the cohort. Fourteen of the 63 primary ACL reconstructions and 1 of the 5 ACL revisions were unconfirmed by operative report.
| Overall | 0 – 2 year |
2 – 6 year |
Median (months) |
|
|---|---|---|---|---|
| Primary ACLR | 63 (6.4%) | 25 | 38 | 27.3 |
| Revision ACLR | 5 (0.5%) | 2 | 3 | 34.5 |
| Cartilage/Meniscus | ||||
| Medial Meniscus | 39 (4.0%) | 19 | 20 | 24.5 |
| Lateral Meniscus | 26 (2.7%) | 10 | 16 | 26.4 |
| Cartilage | 21 (2.1%) | 8 | 13 | 29.6 |
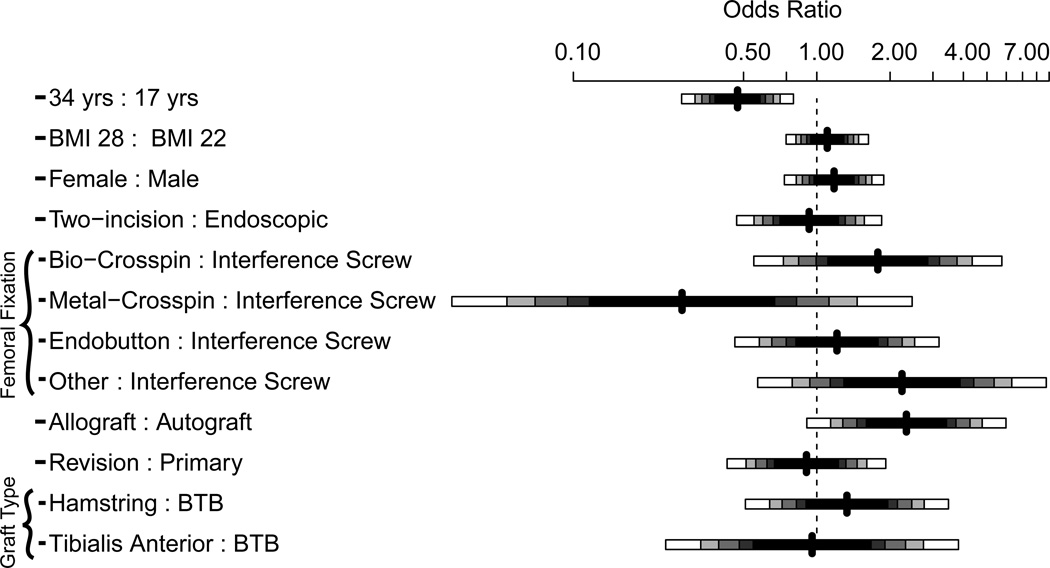
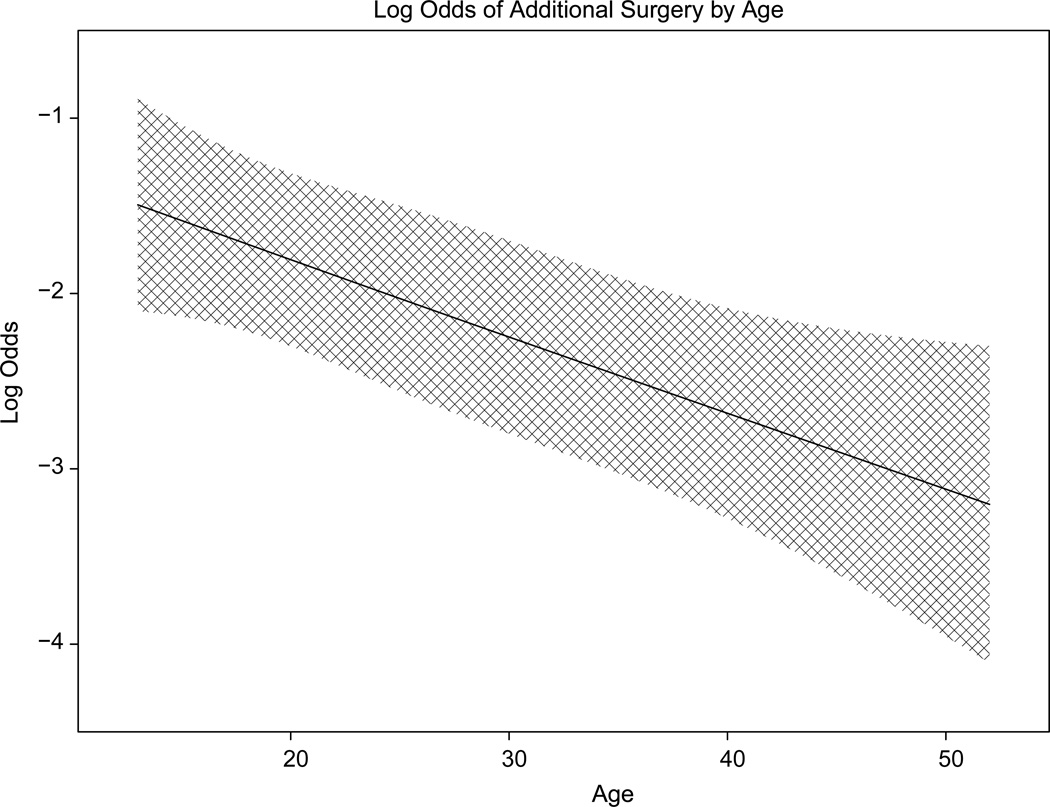
Logistic regression modeling demonstrated that subsequent surgery was associated with younger age at index surgery (IQROR = 0.47, 95% CI: 0.32–0.71, p = 0.0001) and allograft (OR = 2.33, 95% CI: 1.14–4.78, p = 0.0205). It was not associated with revision surgery (p = 0.73), sex (p = 0.37), BMI (p = 0.80), exposure (p = 0.79), fixation (p= 0.08), or graft choice (p = 0.60). A plot showing odds ratios for subsequent surgery by risk factor is shown in Figure 2. A partial effects plot depicting the risk (odds ratio) of subsequent surgery based on age of the patient is shown in Figure 3.
Figure 2.
Plot depicting the odds ratio for subsequent surgery. For age, it is the ratio of subsequent surgery at 34 vs. 17 years of age, BMI (body mass index) is for 28 vs. 22. All femoral fixation devices are as compared to interference screws, and grafts (tibialis anterior and hamstring are both compared to bone-tendon-bone). BMI = body mass index; HG = hamstring; BTB = bone-tendon-bone; IS = interference screw.
Figure 3.
Chart depicting the risk for subsequent surgery based on age.
Discussion
This study examined the rate of subsequent procedures at 2 and 6 year follow-up. At 6-year follow-up 18.9% of ACLR patients underwent subsequent surgeries on the ipsilateral knee. The ipsilateral ACLR graft rupture and contralateral normal ACL tear were similar (7.7% vs. 6.4%). In a systematic review of level 1 and 2 studies in the literature, Wright et al. reported a 5.8% rate of graft rupture and 11.8% rate of tearing the contralateral ACL.13 While the ipsilateral rupture rate is similar, our study had a much lower rate of contralateral ACL rupture. Shelbourne et al. in a prospective cohort with 5-year follow-up had a 5.3% rate of contralateral and 4.3% ipsilateral ACL rupture.11 These rates are similar to our findings, and the rate of contralateral is equivalent to ipsilateral, as in our study. In a previous publication of 235 patients at 2-year follow-up in this patient population, there was a 3.0% rate of rupture in both the ipsilateral and contralateral knee.14 By 6 year follow-up this rate had more than doubled. While the results of this study are comparable for ACL rupture, these surgeries only account for a portion of subsequent procedures post-operatively, with this study being one of the first to describe these other procedure rates.
Subsequent surgery was associated with younger age at index procedure. Shelbourne et al.11 found that the rate of subsequent injury to the ACL was age dependent, 17% for patients less than 18 years of age, 7% for patients aged 18–25, and 4% for patients older than 25. Individuals that rupture their ACLs at a younger age may be more active, less compliant with postoperative instructions, or have a genetic predisposition to collagen disruption affecting ACL re-tear rates as well as meniscal and collagen damage.
Multivariable modeling showed that use of allograft was associated with subsequent surgery (OR = 2.33), while there was not a statistically significant association between rate of subsequent surgery and revision surgery, BMI, female sex, graft choice, surgical exposure, or femoral fixation. This was the only modifiable risk factor identified.
Lyman et al.,7 using a database of all hospital admissions and ambulatory surgery in New York State, found a subsequent surgery rate of 6.5 percent for either knee at 1 year. Of these, 28.7% underwent another ACL reconstruction, 28.0% underwent lysis of adhesions, 24.5% underwent a meniscectomy, and 18.8% had another knee procedure. The reason for the subsequent knee surgery was infection in 11.8% of the cases; a pathological patellar condition in 1.6%; and a variety of indications, including knee pain and complications from previous surgery, in 5.4%. Predictors of subsequent knee surgery included being female, having concomitant knee surgery, and being operated on by a lower-volume surgeon. Differences in predictors of subsequent surgery may be attributed to the differences between the data sources, as well as the data in the NYS system only listed laterality in the minority of cases.
In a retrospective study of an administrative database for active duty soldiers who underwent ACLR with up to 9-year follow-up, 12.7% underwent reoperation after their index procedure.5 Of these, 2.3% underwent surgery on their lateral meniscus, 4.9% on their medial meniscus, and 4.5% on the cartilage. The rate of reoperation for the soldiers that did not undergo ACLR was 32.6%. ACLR led to a 56% reduction in surgery on the lateral meniscus and 42% decrease in reoperation on the medial meniscus. ACLR overall reduced the risk of subsequent reoperation by 66%.5
The 0.5% infection rates in this study are similar to those previously reported in the literature. Benner et al. reported an infection rate of 0.35% in BTB grafts taken from the ipsilateral knee and 0.14% in grafts taken from the contralateral knee.3 Barker et al. in a retrospective cohort study of over 3000 patients found a 0.58% infection rate overall, 0.44% in allografts, 0.49% in autograft BTB, and 1.44% in hamstring autografts.2
Some studies have reported higher reoperation rates in females overall.4,7 Shelbourne et al.11 reported a higher incidence in females in the contralateral knee. Our study is consistent with others in the literature that did not find a difference between males and females in subsequent reoperation rates.1,5
Limitations of this study include that surgeries were only included if an operative report was obtained. While more than 95% of the operative reports were available, these percentages may slightly underestimate the true rate of subsequent surgery. Additionally, this study only looked at reoperation rates at 2 and 6 years, not re-injury rates.
This study provides rates of subsequent surgery and predictors after ACLR at short- and midterm follow-up in a prospective, multicenter cohort. At 6-year follow-up 18.9% of ACLR patients underwent subsequent surgeries on the ipsilateral knee. The ipsilateral ACLR graft vs. contralateral normal ACL tear was similar (7.7% vs. 6.4%). Younger age at index surgery and the use of allograft were risk factors for subsequent surgery. Revision ACLR, female sex, body mass index (BMI), and surgical exposure were not significant.
Table 4. Ipsilateral Procedures by Exposure and Graft Type.
Subsequent procedures by surgical approach (single-incision vs. two-incision) and BTB vs. hamstring vs. tibialis anterior. The N shown is the number of each type of surgery in the cohort. Percentages shown represent the number of each type of subsequent procedure performed divided by the number of surgeries of each type in the cohort.
| Endoscopic | Two Incision |
BTB | Hamstring | Tibialis Anterior |
|
|---|---|---|---|---|---|
| N= 671 | N = 309 | N = 469 | N = 343 | N= 165 | |
| Revision ACL | 61 (9.1%) | 14 (4.5%) | 19 (4.1%) | 21 (6.1%) | 35 (21.2%) |
| Cartilage/Meniscus | 101 (15.1%) | 29 (9.4%) | 49 (10.4%) | 40 (11.7%) | 41 (24.8%) |
| Arthrofibrosis | 42 (6.3%) | 11 (3.6%) | 17 (3.6%) | 21 (6.1%) | 15 (9.1%) |
| Hardware | 19 (2.8%) | 5 (1.6%) | 5 (1.1%) | 13 (3.8%) | 6 (3.6%) |
What is known about the subject
Previous prospective studies reported on the rate of graft rupture and contralateral ACL rupture.
What this study adds to existing knowledge
First prospective cohort reporting on rates of all subsequent procedures.
References
- 1.Barber-Westin SD, Noyes FR, Andrews M. A rigorous comparison between the sexes of results and complications after anterior cruciate ligament reconstruction. Am J Sports Med. 1997;25(4):514–526. doi: 10.1177/036354659702500415. [DOI] [PubMed] [Google Scholar]
- 2.Barker JU, Drakos MC, Maak TG, Warren RF, Williams RJ, 3rd, Allen AA. Effect of graft selection on the incidence of postoperative infection in anterior cruciate ligament reconstruction. Am J Sports Med. 2010;38(2):281–286. doi: 10.1177/0363546509346414. [DOI] [PubMed] [Google Scholar]
- 3.Benner RW, Shelbourne KD, Freeman H. Infections and patellar tendon ruptures after anterior cruciate ligament reconstruction: a comparison of ipsilateral and contralateral patellar tendon autografts. Am J Sports Med. 2011;39(3):519–525. doi: 10.1177/0363546510388163. [DOI] [PubMed] [Google Scholar]
- 4.Cox JS, Lenz HW. Women midshipmen in sports. Am J Sports Med. 1984;12(3):241–243. doi: 10.1177/036354658401200315. [DOI] [PubMed] [Google Scholar]
- 5.Dunn WR, Lyman S, Lincoln AE, Amoroso PJ, Wickiewicz T, Marx RG. The effect of anterior cruciate ligament reconstruction on the risk of knee reinjury. Am J Sports Med. 2004;32(8):1906–1914. doi: 10.1177/0363546504265006. [DOI] [PubMed] [Google Scholar]
- 6.Frobell RB, Roos EM, Roos HP, Ranstam J, Lohmander LS. A randomized trial of treatment for acute anterior cruciate ligament tears. New Engl J Med. 22. 2010;363(4):331–342. doi: 10.1056/NEJMoa0907797. [DOI] [PubMed] [Google Scholar]
- 7.Lyman S, Koulouvaris P, Sherman S, et al. Epidemiology of anterior cruciate ligament reconstruction: trends, readmissions, and subsequent knee surgery. J Bone J Surg--Am. 2009;91(10):2321–2328. doi: 10.2106/JBJS.H.00539. [DOI] [PubMed] [Google Scholar]
- 8.Mather RC, Hettrich CM, Dunn WR, Bach BR, Spindler KP. Cost effectiveness analysis of early reconstruction vs. rehabilitation and delayed reconstruction for ACL Tears. Poster presentation at American Academy of Orthopaedic Surgeons; February 2012; San Francisco, California. [Google Scholar]
- 9.Outerbridge RE. The etiology of chondromalacia patellae. J Bone Joint Surg Br. 1961;43(4):752–757. doi: 10.1302/0301-620X.43B4.752. [DOI] [PubMed] [Google Scholar]
- 10.Paxton ES, Kymes SM, Brophy RH. Cost-effectiveness of anterior cruciate ligament reconstruction: a preliminary comparison of single-bundle and double-bundle techniques. Am J Sports Med. 2010;38(12):2417–2425. doi: 10.1177/0363546510375545. [DOI] [PubMed] [Google Scholar]
- 11.Shelbourne KD, Gray T, Haro M. Incidence of subsequent injury to either knee within 5 years after anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med. 2009;37(2):246–251. doi: 10.1177/0363546508325665. [DOI] [PubMed] [Google Scholar]
- 12.Spindler KP, Wright RW. Clinical practice. Anterior cruciate ligament tear. New Engl J Med. 2008;359(20):2135–2142. doi: 10.1056/NEJMcp0804745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wright RW, Magnussen RA, Dunn WR, Spindler KP. Ipsilateral graft and contralateral ACL rupture at five years or more following ACL reconstruction: a systematic review. J Bone Joint Surgery--Am. 2011;93(12):1159–1165. doi: 10.2106/JBJS.J.00898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wright RW, Dunn WR, Amendola A, et al. Risk of tearing the intact anterior cruciate ligament in the contralateral knee and rupturing the anterior cruciate ligament graft during the first 2 years after anterior cruciate ligament reconstruction: a prospective MOON cohort study. Am J Sports Med. 2007;35(7):1131–1134. doi: 10.1177/0363546507301318. [DOI] [PubMed] [Google Scholar]