Abstract
Background
Syphilitic alopecia is not common in patients with secondary syphilis. Though the clinical and histopathological findings of syphilitic alopecia have been described, the trichoscopy features are unknown yet.
Main observation
A 42-year-old Chinese man was admitted to our clinic with a complaint of hair loss. The patient presented clinically with moth-eaten alopecia over the whole scalp without any previous discomfort or skin rashes. The serology for syphilis was positive. Trichoscopy showed black dots, focal atrichia, hypopigmentation of hair shaft and yellow dots.
Conclusions
On the basis of trichoscopy, along with serology testing syphilitic alopecia can be differentiated from other hair loss diseases with similar clinical presentation.
Keywords: alopecia, dermoscopy, dermatoscopy, hair loss, sexually transmitted diseases, syphilis, venereal diseases
Introduction
Syphilis as a "great mimic" can present various manifestations indistinguishable from other diseases. Syphilitic alopecia is an uncommon clinical manifestation of secondary syphilis with an incidence of 2.9%-11.2%.[1,2] The clinical manifestations and histopathological features of syphilitic alopecia have been described in detail, but the trichoscopic features of syphilitic alopecia have not been described yet. Here we present a case of syphilitic alopecia, and describe the clinical and trichoscopic features.
Case Report
A 42-year-old Chinese man came to our clinic with a complaint of hair loss for 2 weeks, without scalp pruritus or pain. He also complained about being under high mental stress recently. He was heterosexual and was engaging in casual sex. He denied having any skin lesions in the genital area before the hair loss, i.e., the clinical manifestations of primary syphilis. The patient had a past history of asthma and diabetes mellitus, but no history of hair loss.
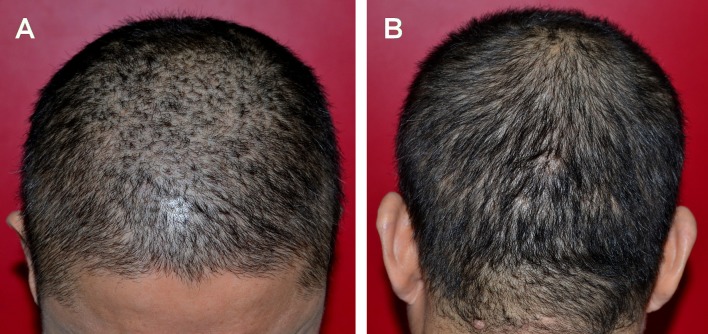
On physical examination of the scalp area, numerous small scattered non-scarring hairless patches with incomplete hair loss were observed. The patches were irregular in size without defined borders, ranged from 0.2cm-0.5cm in diameter, distributed over the whole scalp giving the appearance of moth-eaten alopecia [Fig. 1]. The hairless areas showed no signs of inflammation or desquamation. The gentle pull test was negative. Under trichoscopy black dots, focal atrichia, hypopigmentation of hair shafts and yellow dots were observed [Fig. 2]. The empty ostia of hair follicle were presented. No skin rash was found all over the body. Up till now, the primary clinical impressions include syphilitic alopecia (SA) and alopecia areata (AA).
Figure 1.
Global pictures of moth-eaten alopecia scattered among the whole scalp from frontalparietal (A) and occipital (B) view.
Figure 2.
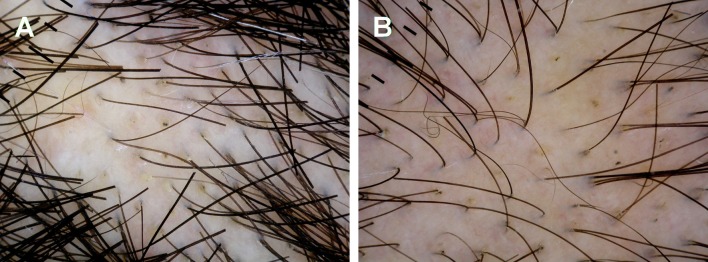
Trichoscopy signs of moth-eaten syphilitic alopecia. (A) Small patches of hair loss with black dots and yellow dots inside. (B) Black dots, focal atrichia, hypopigmentation of hair shaft and yellow dots were presented in the hair loss region.
Blood tests were performed including blood count, total IgE, antinuclear autoantibodies tests, serology for HIV and syphilis. The results of serology for syphilis were positive: rapid plasma reagin test (RPR) with titer of 1:64 and Treponema pallidum particle assay (TPPA) with titer of 1:2560. No any other abnormality was with the rest of results. The patient was unwilling to accept a biopsy when under request.
Therefore the diagnosis was established as syphilitic alopecia, i.e., second stage of syphilis. The antisyphilitic treatment was installed right after the diagnosis was confirmed by serological tests, with intramuscular injection of benzathine benzylpenicillin, a weekly dose of 2.4 million unit for 3 weeks. Regrowth of hair was observed 12 weeks after the start of the treatment.
Discussion
According to the classification of McCarthy made in 1940, secondary SA was divided into two types: symptomatic SA and essential SA.[3] Essential SA, characterized by alopecia without any other visible syphilitic lesions on the scalp, may appear as one of three different clinical patterns: moth-eaten or patchy alopecia, diffuse alopecia and mixed pattern of alopecia.[3] Among them, the moth-eaten pattern alopecia has been considered the most common and characteristic form of secondary syphilis.[4,5]
In this case, the patient presented with moth-eaten alopecia of essential SA as the first and only manifestation of secondary syphilis, without any skin rashes and preceding history of genital chancre. Moreover, the pattern of nonscarring, moth-eaten alopecia was not only seen in SA, it was also found in other diseases, e.g., alopecia areata, trichotillomania, or tinea capitis.[6] Therefore, a carefully differential diagnosis is necessary and important, especially when patients presented with non-scarring alopecia.
In addition to the global view of the hair loss region, the application of trichoscopy (hair and scalp dermoscopy) helps greatly in the differential diagnosis. To our knowledge, specific trichoscopy features for SA have not been described in literature up to date. Here in this case, the trichoscopy signs for SA included black dots, focal atrichia, hypopigmentation of hair shafts and yellow dots, and the scalp showed no obvious signs of inflammation or desquamation. Absence of exclamation hair, coma hair, flame hairs or v-sign can be used to exclude AA, tinea capitis and trichotillomania, respectively.[7,8,9] The diagnosis of SA in this case was confirmed by patient’s sexual history and positive serological tests for RPR and TPPA. Although SA resembles AA clinically, lack of exclamation hair and uneven diameter of hairs under trichoscopy can be used to differentiate these two conditions.
Histopathology examination of the hair loss region is required to further confirm the diagnosis. Unfortunately, we were unable to receive patient’s consent for biopsy. The histopathology findings of SA usually include a normal epidermis with areas of follicular hyperkeratosis, a marked reduced number of anagen follicles and an increasing number of catagen and telogen follicles.[3,10] A presence of a perivascular and perifollicular (especially in the peribulbar region) lymphocytic dermal infiltration with scattered plasma cells was observed in some cases.[5,11,12] Besides, Treponema pallidum DNA was detected in lesional follicles of SA by molecular methods,[5] and immunohistochemistry showed the presence of spirochetes in hair follicles, usually in the perifollicular and peribulbar regions.[11] The above histopathological findings in SA lesions differ from AA, tinea capitis and trichotillomania, useful in differential diagnosis.
Conclusion
Our findings indicate that trichoscopy may facilitate the diagnosis of syphilitic alopecia in a patients who presents with hair loss of unknown origin. Clinical presentation, serological screening for syphilis, and scalp histopathology should be taken into consideration for final diagnosis.
Trichoscopy signs of syphilitic alopecia in our patient included black dots, focal atrichia, hypopigmentation of hair shaft and yellow dots.
References
- Vafaie J, Weinberg JM, Smith B, Mizuguchi RS. Alopecia in association with sexually transmitted disease: a review. Cutis. 2005;76:361–366. [PubMed] [Google Scholar]
- Hira SK, Patel JS, Bhat SG, Chilikima K, Mooney N. Clinical manifestations of secondary syphilis. Int J Dermatol. 1987;26:103–107. doi: 10.1111/j.1365-4362.1987.tb00532.x. [DOI] [PubMed] [Google Scholar]
- Hernández-Bel P, Unamuno B, Sánchez-Carazo JL, Febrer I, Alegre V. Syphilitic alopecia: a report of 5 cases and a review of the literature. Actas Dermosifiliogr. 2013;104:512–517. doi: 10.1016/j.ad.2012.02.009. [DOI] [PubMed] [Google Scholar]
- Cuozzo DW, Benson PM, Sperling LC, Skelton HG 3rd. Essential syphilitic alopecia revisited. J Am Acad Dermatol. 1995;32(5 Pt 2):840–843. doi: 10.1016/0190-9622(95)91543-5. [DOI] [PubMed] [Google Scholar]
- Friedli A, Chavaz P, Harms M. Alopecia syphilitica: report of two cases in Geneva. Dermatology. 2001;202:376–377. doi: 10.1159/000051688. [DOI] [PubMed] [Google Scholar]
- Bi MY, Cohen PR, Robinson FW, Gray JM. Alopecia syphilitica report of a patient with secondary syphilis presenting as moth-eaten alopecia and a review of its common mimickers. Dermatol Online J. 2009;15:6. [PubMed] [Google Scholar]
- Inui S, Nakajima T, Nakagawa K, Itami S. Clinical significance of dermoscopy in alopecia areata: analysis of 300 cases. Int J Dermatol. 2008;47:688–693. doi: 10.1111/j.1365-4632.2008.03692.x. [DOI] [PubMed] [Google Scholar]
- Slowinska M, Rudnicka L, Schwartz RA, Kowalska-Oledzka E, Rakowska A, Sicinska J, Lukomska M, Olszewska M, Szymanska E. Comma hairs: a dermoscopic marker for tinea capitis: a rapid diagnostic method. J Am Acad Dermatol. 2008;59(5 Suppl):S77–79. doi: 10.1016/j.jaad.2008.07.009. [DOI] [PubMed] [Google Scholar]
- Rakowska A, Slowinska M, Olszewska M, Rudnicka L. New Dermoscopy Findings in Trichotillomania: Flame Hairs, V-sign, Hook Hairs, Hair Powder, Tulip Hairs. Acta Derm Venereol. 2014;94:303–306. doi: 10.2340/00015555-1674. [DOI] [PubMed] [Google Scholar]
- Lee JY, Hsu ML. Alopecia syphilitica, a simulator of alopecia areata: histopathology and differential diagnosis. J Cutan Pathol. 1991;18:87–92. doi: 10.1111/j.1600-0560.1991.tb00133.x. [DOI] [PubMed] [Google Scholar]
- Nam-Cha SH, Guhl G, Fernández-Peña P, Fraga J. Alopecia syphilitica with detection of Treponema pallidumin the hair follicle. J Cutan Pathol. 2007;34 Suppl 1:37–40. doi: 10.1111/j.1600-0560.2006.00726.x. [DOI] [PubMed] [Google Scholar]
- Mindel A, Tovey SJ, Timmins DJ, Williams P. Primary and secondary syphilis, 20 years’ experience. 2. Clinical features. Genitourin Med. 1989;65:1–3. doi: 10.1136/sti.65.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]