Abstract
Epidemiological data are limited regarding risk factors of atrial fibrillation (AF) in patients with normal-sized left atria (LA). We evaluated whether traditional risk factors of AF differ between patients with normal-sized and dilated LA. This is a cross sectional study of community-dwelling participants of Atherosclerosis Risk in Communities Study. LA volume index (LAVI) was measured by 2-dimensional echocardiography. LAVI ≥29mm3/m2 defined dilated LA. Prevalent AF was defined by electrocardiogram and hospital discharge international classification of diseases - 9 codes. Multivariable adjusted logistic regression analysis was used to examine whether magnitude of association of risk factors with AF differ by LA cavity size. Interaction of risk factors by LA cavity size was evaluated to determine significance of these differential associations. Of 5496 participants (mean age 75±5 years, women 58%), 1230 (22%) had dilated LA. The prevalence of AF was 11% in individuals with normal-sized LA and 15% in individuals with dilated LA. Age >75 years [Odds Ratio (OR) 1.87; 95% confidence interval (CI) 1.49 – 2.35, interaction p=0.12] and heart failure (OR 5.43; 95% CI 3.77 – 7.87, interaction p=0.10) were stronger risk factors for AF in normal-sized LA than dilated-LA. Female sex (OR 1.67; 95% CI 1.01 – 2.77, interaction p=0.09), weight (OR 1.32; 95% CI 1.02 – 1.71, interaction p=0.19) and alcohol-use (OR 1.61; 95% CI 1.08 – 2.41, interaction p=0.004) were stronger risk factors for AF in individuals with dilated LA than normal-sized LA. In conclusion, risk factors of AF may differ by left ventricular cavity size.
Keywords: Atrial fibrillation, normal size left atrium, left atrium, risk factors, epidemiology
INTRODUCTION
Atrial fibrillation (AF) is the most common sustained cardiac arrhythmia, and currently affects 2.3 million individuals in the United States.1 Its prevalence is projected to increase to 5.6 million by 2050.2, 3 Current literature suggests traditional cardiovascular risk factors may lead to dilated left atrial (LA) size which acts as a substrate for AF.4-6 However, a sizable minority of patients with AF has normal LA.7 The aims of this study are to investigate traditional AF risk factors in patients with and without dilated LA, and to determine whether the association of these risk factors differs by LA cavity size.
METHODS
The ARIC study is a community based cohort study that began recruitment in 1987. At baseline, 15,792 participants aged 45 – 64 years were randomly recruited at 4 field centers in United States (Forsyth County, NC; suburban Minneapolis, MN; Washington County, MD; Jackson, MS). The details of the recruitment and baseline characteristics have been published previously.8 During the visit 5 examination that was conducted from 2011 – 2013, echocardiography was performed by certified technicians and LA volume was measured. Thus, this study only includes participants that survived until 5th examination. For the current analysis, we used the data from 5496 individuals that underwent 2-D echocardiography at the field centers during visit 5. Race was dichotomized into white and nonwhite categories for easier interpretation as there were only 15 individuals that were nonwhite and nonblack which were added to blacks.
Two-dimensional echocardiography was performed and echocardiographic parameters were measured at the core laboratory for Atherosclerosis Risk in Communities. LA volume index were measured by Simpson's method according to established protocol of the American Society of Echocardiography.9 We defined LA volume index of ≥29 mm3/m2 as atrial enlargement. 9, 10 Prevalent AF was defined as presence of AF during any of ARIC visits 1 to 5 by either study scheduled ECG or by hospital discharge international classification of diseases (ICD) 9 codes 427.3, 427.31, and 427.32 that were obtained by active surveillance of ARIC community hospitals until 2010. Random zero sphygmomanometers were used to measure systolic and diastolic blood pressures with participants in the sitting position after 5 minutes of rest. The average of two readings was recorded and hypertension was defined as systolic blood pressure ≥140 mmHg, diastolic blood pressure ≥90 mmHg, or antihypertensive medication use. Height and weight were measured in light clothing without shoes. Body mass index was calculated as weight in kilograms by the square of height in meters. Diabetes mellitus was defined as fasting blood glucose level ≥7.0 mmol/L, non-fasting blood glucose ≥11.0mmol/L or use of diabetic medication. Alcohol use and smoking status were determined by self-report. Physical activity was defined as frequency of exercise in days per week where exercise was at least 20 minutes of aerobic workout. Coronary artery disease was defined by adjudicated myocardial infarction and coronary heart disease events.11 Heart failure was identified by hospital discharge ICD 9 and 10 codes 428.0, 428.1, 428.2, 428.3, 428.4, 428.9 and death certificates code I50.0. 12 The coronary artery disease and heart failure events were available until 2010. Blood glucose and uric acid were determined by standard protocols. 13
Descriptive statistics were used to summarize the data. Continuous variables are expressed in mean ± standard deviation and categorical variables were given as percentages. For examining the differences, Student's t-test was used for continuous variables and Chi-square for categorical variables, wherever appropriate. We assessed association of traditional risk factors age, sex, race, height, weight, hypertension, diabetes, current smoking, current alcohol use, moderate to vigorous exercise (>1 times per week), coronary artery disease and heart failure with AF stratified by dilated or normal sized LA in a multivariate logistic regression model. We used interaction terms of dilated LA*traditional risk factor after adjusting for covariates given above, one at a time to assess association with AF to determine significant interactions. All p values were 2 sided and p <0.05 is considered significant. Since, the analysis was used for only screening for interactions and not testing a hypothesized interaction, we used an interaction p – value of 0.20 which gives power of 90% to detect interaction.14
RESULTS
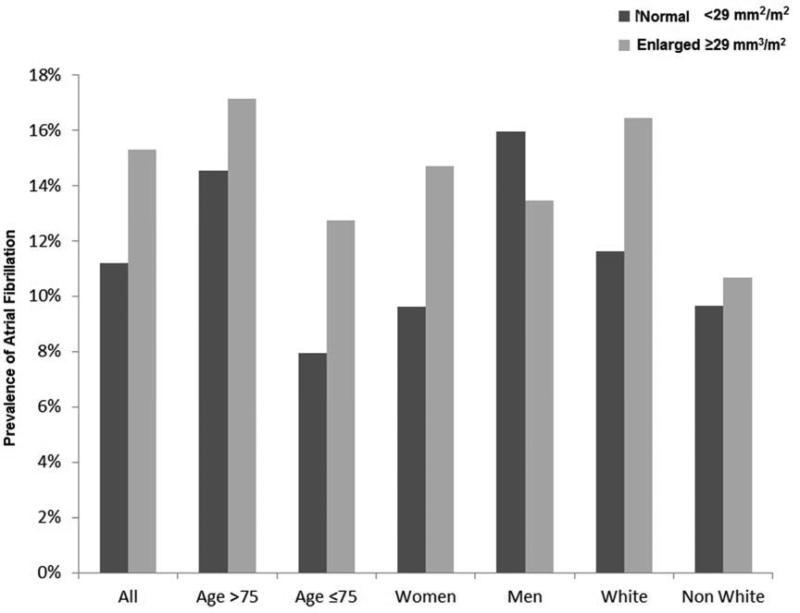
Of 5496 participants (mean age 75±5, women 58%), there were 665 (12%) individuals with prevalent AF. There were 1230 (22%) individuals with dilated LA diagnosed by echocardiography. AF occurred in 477 (11%) of the individuals with normal sized LA and in 188 (15%) of the individuals with dilated LA. Individuals with AF were more likely to be older, exercise <1 times per week and had heart failure. Individuals with AF with dilated LA were more likely to be of white race and consume alcohol, while individuals with AF with normal LA were more likely to be men, taller, hypertensive and have coronary artery disease (Table 1). When risk factors for all participants with AF were evaluated in a multivariable logistic regression model we found age >75 years, race, height, hypertension, coronary artery disease, and heart failure were directly associated with risk of AF and exercise >1 times per week was inversely associated with risk of AF (Table 2). Female sex, alcohol use and weight were stronger risk factors for AF in dilated LA group than normal-sized LA group. While, age >75 years and heart failure (p for interaction <0.20) were stronger risk factors for AF in normal sized LA group than dilated LA group. Figure 1 shows the prevalence of AF by demographic variables among individuals with dilated and normal sized LA. Prevalence of AF among groups of risk factors stratified by American Society of Echocardiography based classification of LAVI are given in appendix (Figure 1S – 3S).
Table 1.
Characteristics of the sample stratified by left atrial cavity size
| Characteristics |
Left Atrial Cavity Size |
|||||
|---|---|---|---|---|---|---|
| Increased |
Normal |
|||||
| AF | No AF | p | AF | No AF | p | |
| Number of patients | 188 | 1042 | 477 | 3789 | ||
| Age >75 years | 122 (65%) | 590 (57%) | 0.03 | 304 (64%) | 1787 (47%) | <0.0001 |
| Women | 96 (51%) | 557 (53%) | 0.54 | 244 (51%) | 2289 (60%) | 0.0001 |
| White race | 158 (84%) | 791 (76%) | 0.01 | 384 (80%) | 2919 (77%) | 0.09 |
| Height (cm) | 168±10 | 166±9 | 0.06 | 167±10 | 165±9 | 0.0003 |
| Weight (kg) | 82±20 | 81±17 | 0.49 | 81±17 | 78±17 | 0.001 |
| Hypertension | 141 (75%) | 747 (72%) | 0.32 | 320 (67%) | 2257 (60%) | 0.0009 |
| Diabetes mellitus | 48 (26%) | 267 (26%) | 0.98 | 122 (26%) | 1128 (30%) | 0.06 |
| Current alcohol use | 130 (69%) | 615 (59%) | 0.01 | 275 (58%) | 2317 (61%) | 0.13 |
| Current Smoking | 13 (7%) | 48 (5%) | 0.17 | 27 (6%) | 220 (6%) | 0.92 |
| Exercise > 1 day/week | 77 (41%) | 519 (49%) | 0.03 | 208 (44%) | 1886 (50%) | 0.02 |
| Coronary artery disease | 8 (4%) | 26 (2%) | 0.18 | 30 (6%) | 76 (2%) | <0.0001 |
| Heart failure | 24 (13%) | 40 (4%) | <0.0001 | 63 (13%) | 90 (2%) | <0.0001 |
Left atrial enlargement defined by left atrial volume index ≥ 29 mm3/m2. AF; Prevalent atrial fibrillation at visit 5 (2011 – 2013)
Table 2.
Differential association of risk factors of atrial fibrillation in individuals with dilated and normal - sized left atrial cavity
| Left Atrial Cavity Size | ||||
|---|---|---|---|---|
| Risk Factors | All participants αOR (95% CI) | Increased OR (95% CI) | Normal OR (95% CI) | Interaction - p |
| Number of Patients | 5496 | 1230 | 4266 | |
| Age >75 years | 1.74 (1.43 – 2.11) | 1.36 (0.93 – 1.97) | 1.87 (1.49 – 2.35) | 0.12 |
| Women | 1.20 (0.92 – 1.57) | 1.67 (1.01 – 2.77) | 1.06 (0.77 – 1.46) | 0.09 |
| White race | 1.44 (1.13 – 1.84) | 1.37 (0.84 – 2.23) | 1.48 (1.12 – 1.97) | 0.72 |
| Height, per 10 cm | 1.27 (1.11 – 1.46) | 1.44 (1.18 – 1.77) | 1.24 (1.05 – 1.46) | 0.48 |
| Weight, per 20 kg | 1.09 (0.97 – 1.23) | 1.32 (1.02 – 1.71) | 1.12 (0.98 – 1.29) | 0.19 |
| Hypertension | 1.32 (1.08 – 1.61) | 1.31 (0.87 – 1.98) | 1.31 (1.04 – 1.65) | 0.64 |
| Diabetes mellitus | 0.97 (0.78 – 1.20) | 1.15 (0.76 – 1.72) | 0.99 (0.77 – 1.26) | 0.20 |
| Alcohol use | 0.96 (0.79 – 1.16) | 1.61 (1.08 – 2.41) | 0.81 (0.64 – 1.01) | 0.004 |
| Smoking | 1.21 (0.82 – 1.77) | 1.54 (0.75 – 3.16) | 1.13 (0.71 – 1.78) | 0.30 |
| Exercise > Iday/week | 0.83 (0.69 – 1.00) | 0.81 (0.56 – 1.16) | 0.82 (0.66 – 1.02) | 0.86 |
| Coronary artery disease | 2.17 (1.40 – 3.37) | 1.82 (0.74 – 4.51) | 2.38 (1.44 – 3.94) | 0.35 |
| Heart failure | 4.76 (3.51 – 6.49) | 3.62 (2.03 – 4.50) | 5.43 (3.77 – 7.87) | 0.10 |
Logistic regression model was adjusted for age >75 years, sex, race, height per 10 cm, weight per 20 kg, hypertension, diabetes, alcohol use, smoking, exercise >1 day per week, coronary artery disease, heart failure and enlarged status of left atrium; dilated left atrium is defined by left atrial volume index ≥ 29 mm3/m2;
Figure 1.
Prevalence of atrial fibrillation among all participants and stratified by race, sex and median age among dilated (light colored) and normal (dark colored) left atrial groups
DISCUSSION
In this cross sectional study, we attempted to determine whether traditional risk factors for AF have different associations in older individuals with dilated vs. normal-sized LA. We found that women sex, alcohol consumption and weight had higher magnitude of association for AF individuals with dilated LA; while older age and heart failure had higher magnitude of association for AF individuals with normal sized LA. The study also provides us information related to prevalence of AF in normal sized LA that approaches close to that of individuals with dilated LA suggesting that this is not an uncommon phenotype of AF.
In this study we found weaker associations of modifiable risk factors with AF in normal sized LA compared with AF in dilated LA. A previous study in women from Women Health Initiative (WHI) Cohort found age and weight as stronger risk factors for AF in women with dilated LA size.15 Our study confirmed their finding of an association of weight with risk of AF in the dilated LA group. However, we found older age to be a stronger risk factor for AF with normal sized LA. We speculate that this finding might be due to differences in mean ages of both cohorts. The WHI cohort is a relatively younger cohort (mean age 54 years) than the cohort of this study (mean age 75 years). It may be possible that there might be a selective survival of individuals with normal sized LA enrolled in this cohort and thus this might have resulted in survival bias. Nevertheless, age remains a significant risk factor for both forms of AF. Understanding AF risk factors in septuagenarians is important, as outcomes in this group can be improved with appropriate therapy.16 Dilated LA size in AF is strongly associated with stroke and thus, risk factors that lead to increase in AF patients with dilated LA, may also increase the risk of stroke.17
Weight was also a stronger risk factor for AF in dilated LA group. Previous studies have shown obesity as a significant independent risk factor for AF.18, 19 However, this study suggests that obesity is a weaker risk factor of AF in the absence of enlargement (remodeling) of LA. Future research may be directed to evaluate the value of weight loss in individuals with normal LA size and reduction in incidence of AF.
Alcohol has consistently shown to be a risk factor for AF in the previous studies.20 Possible mechanisms include increased adrenergic tone,21 impaired vagal tone,22 shorter refractory period,23 increase in intra-atrial conduction time, 24 and atrial remodeling.25 Alcohol was a stronger risk factor for AF in the dilated LA group which was expected as alcohol has been known to lead to remodeling of atria and ventricles. 26, 27 There was an opposite direction of association of alcohol with AF in normal sized LA. Alcohol as a protective agent for AF has not been studied. However, moderate alcohol consumption has shown to be beneficial for other forms of cardiovascular diseases and may explain this.28 Nevertheless, we suggest caution in interpreting this finding until more data have been published about inverse non-significant association.
There are several strengths of this analysis. These include its large sample size, carefully measured risk factor information, long period of observation, older biracial cohort and use of standardized methods to read echocardiograms. Our study also faced some potential limitations such as cross sectional design which limits the information about temporal sequence. However, our main goal was not to identify these already established risk factors but to highlight the differences in risk factors between individuals with normal and dilated left atria. We also anticipate that there might be missed cases of AF that requires continuous Holter monitoring, however in large cohorts such as ARIC, it might not be feasible. Data regarding paroxysmal and permanent AF was not available. It is also possible that those who have permanent AF or AF with a longer period of time have had remodeling of the LA leading to enlargement. Hence, there is a possibility that the difference in the associations of risk factors with AF by LA cavity size is due to quicker progression of paroxysmal AF to permanent AF. These individuals might have started with normal sized LA. This could be further confirmed in a longitudinal study. Moreover, this cohort is an elderly cohort and results may differ from middle aged or younger cohorts due to strong survival and comorbidity biases.
Supplementary Material
HIGHLIGHTS.
Almost one in ten individuals of >65 years of age with normal sized left atrium suffer from atrial fibrillation and traditional risk factors for atrial fibrillation in normal sized left atria are not well studied
Older age and heart failure are stronger positive risk factors for atrial fibrillation in normal sized left atrium compared with enlarged sized left atrium
Women sex, weight and alcohol consumption are stronger positive risk factors for atrial fibrillation in enlarged sized left atrium compared with normal sized left atrium
ACKNOWLEDGEMENTS
The Atherosclerosis Risk in Communities Study is carried out as a collaborative study supported by National Heart, Lung, and Blood Institute contracts (HHSN268201100005C, HHSN268201100006C, HHSN268201100007C, HHSN268201100008C, HHSN268201100009C, HHSN268201100010C, HHSN268201100011C, and HHSN268201100012C). The authors thank the staff and participants of the ARIC study for their important contributions. WQ is funded by Ruth L. Kirschstein NRSA Institutional Training Grant 5T32HL076132-10.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
CONFLICTS OF INTEREST DISCLOSURE
None
References
- 1.Go AS, Hylek EM, Phillips KA, Chang Y, Henault LE, Selby JV, Singer DE. Prevalence of diagnosed atrial fibrillation in adults: National implications for rhythm management and stroke prevention: The anticoagulation and risk factors in atrial fibrillation (atria) study. JAMA. 2001;285:2370–2375. doi: 10.1001/jama.285.18.2370. [DOI] [PubMed] [Google Scholar]
- 2.Gersh BJ, Tsang TS, Seward JB. The changing epidemiology and natural history of nonvalvular atrial fibrillation: Clinical implications Trans. Am Clin Climatolog Assoc. 2004;115:149–159. [PMC free article] [PubMed] [Google Scholar]
- 3.Miyasaka Y, Barnes ME, Gersh BJ, Cha SS, Bailey KR, Abhayaratna WP, Seward JB, Tsang TS. Secular trends in incidence of atrial fibrillation in olmsted county, minnesota, 1980 to 2000, and implications on the projections for future prevalence. Circulation. 2006;114:119–125. doi: 10.1161/CIRCULATIONAHA.105.595140. [DOI] [PubMed] [Google Scholar]
- 4.Zatuchni J. Atrial fibrillation and left atrial size. Am Heart J. 1988;115:1339–1340. doi: 10.1016/0002-8703(88)90044-0. [DOI] [PubMed] [Google Scholar]
- 5.Garber EB, Morgan MG, Glasser SP. Left atrial size in patients with atrial fibrillation: An echocardiographic study. Am J Med Sci. 1976;272:57–64. doi: 10.1097/00000441-197607000-00007. [DOI] [PubMed] [Google Scholar]
- 6.Henry WL, Morganroth J, Pearlman AS, Clark CE, Redwood DR, Itscoitz SB, Epstein SE. Relation between echocardiographically determined left atrial size and atrial fibrillation. Circulation. 1976;53:273–279. doi: 10.1161/01.cir.53.2.273. [DOI] [PubMed] [Google Scholar]
- 7.Fogari R, Zoppi A, Maffioli P, Mugellini A, Preti P, Perrone T, Derosa G. Effect of telmisartan on paroxysmal atrial fibrillation recurrence in hypertensive patients with normal or increased left atrial size. Clin Cardiol. 2012;35:359–364. doi: 10.1002/clc.21994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.The atherosclerosis risk in communities (aric) study: Design and objectives. The aric investigators. Am J Epidemiol. 1989;129:687–702. [PubMed] [Google Scholar]
- 9.Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise JS, Solomon SD, Spencer KT, Sutton MS, Stewart WJ. Recommendations for chamber quantification: A report from the american society of echocardiography's guidelines and standards committee and the chamber quantification writing group, developed in conjunction with the european association of echocardiography, a branch of the european society of cardiology. J Am Soc Echocardiogr. 2005;18:1440–1463. doi: 10.1016/j.echo.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 10.Ilercil A, O'Grady MJ, Roman MJ, Paranicas M, Lee ET, Welty TK, Fabsitz RR, Howard BV, Devereux RB. Reference values for echocardiographic measurements in urban and rural populations of differing ethnicity: The strong heart study. J Am Soc Echocardiogr. 2001;14:601–611. doi: 10.1067/mje.2001.113258. [DOI] [PubMed] [Google Scholar]
- 11.Sorlie PD, Cooper L, Schreiner PJ, Rosamond W, Szklo M. Repeatability and validity of the rose questionnaire for angina pectoris in the atherosclerosis risk in communities study. J Clin Epidemiol. 1996;49:719–725. doi: 10.1016/0895-4356(96)00022-4. [DOI] [PubMed] [Google Scholar]
- 12.Eriksson H, Caidahl K, Larsson B, Ohlson LO, Welin L, Wilhelmsen L, Svardsudd K. Cardiac and pulmonary causes of dyspnoea--validation of a scoring test for clinical-epidemiological use: The study of men born in 1913. Eur Heart J. 1987;8:1007–1014. doi: 10.1093/oxfordjournals.eurheartj.a062365. [DOI] [PubMed] [Google Scholar]
- 13.National Heart L, and Blood Institute Atherosclerosis Risk in Communities (ARIC) Study. Operations manual 10. Clinical chemistry determinations. 1987 [Google Scholar]
- 14.Frongillo E. [June 21, 2014];Evaluating statistical interactions. 2004 http://www.cscu.cornell.edu/news/statnews/stnews64.pdf.
- 15.Conen D, Glynn RJ, Sandhu RK, Tedrow UB, Albert CM. Risk factors for incident atrial fibrillation with and without left atrial enlargement in women. Int J Cardiol. 2013;168:1894–1899. doi: 10.1016/j.ijcard.2012.12.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shariff N, Desai RV, Patel K, Ahmed MI, Fonarow GC, Rich MW, Aban IB, Banach M, Love TE, White M, Aronow WS, Epstein AE, Ahmed A. Rate-control versus rhythm-control strategies and outcomes in septuagenarians with atrial fibrillation. Am J Med. 2013;126:887–893. doi: 10.1016/j.amjmed.2013.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Piotrowski G, Banach M, Gerdts E, Mikhailidis DP, Hannam S, Gawor R, Stasiak A, Rysz J, Gawor Z. Left atrial size in hypertension and stroke. J Hypertension. 2011;29:1988–1993. doi: 10.1097/HJH.0b013e32834a98db. [DOI] [PubMed] [Google Scholar]
- 18.Tsang TS, Barnes ME, Miyasaka Y, Cha SS, Bailey KR, Verzosa GC, Seward JB, Gersh BJ. Obesity as a risk factor for the progression of paroxysmal to permanent atrial fibrillation: A longitudinal cohort study of 21 years. Eur J Heart. 2008;29:2227–2233. doi: 10.1093/eurheartj/ehn324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cheng TO. Obesity as a risk factor for atrial fibrillation. Int J Cardiol. 2007;114:145. doi: 10.1016/j.ijcard.2006.05.028. [DOI] [PubMed] [Google Scholar]
- 20.Samokhvalov AV, Irving HM, Rehm J. Alcohol consumption as a risk factor for atrial fibrillation: A systematic review and meta-analysis. Eur J Cardiovasc Prev Rehab. 2010;17:706–712. doi: 10.1097/HJR.0b013e32833a1947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Denison H, Jern S, Jagenburg R, Wendestam C, Wallerstedt S. Influence of increased adrenergic activity and magnesium depletion on cardiac rhythm in alcohol withdrawal. Br Heart J. 1994;72:554–560. doi: 10.1136/hrt.72.6.554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Maki T, Toivonen L, Koskinen P, Naveri H, Harkonen M, Leinonen H. Effect of ethanol drinking, hangover, and exercise on adrenergic activity and heart rate variability in patients with a history of alcohol-induced atrial fibrillation. Am J Cardiol. 1998;82:317–322. doi: 10.1016/s0002-9149(98)00299-9. [DOI] [PubMed] [Google Scholar]
- 23.Marcus GM, Smith LM, Whiteman D, Tseng ZH, Badhwar N, Lee BK, Lee RJ, Scheinman MM, Olgin JE. Alcohol intake is significantly associated with atrial flutter in patients under 60 years of age and a shorter right atrial effective refractory period. Pacing Clin Electrophysiol. 2008;31:266–272. doi: 10.1111/j.1540-8159.2008.00985.x. [DOI] [PubMed] [Google Scholar]
- 24.Steinbigler P, Haberl R, Konig B, Steinbeck G. P-wave signal averaging identifies patients prone to alcohol-induced paroxysmal atrial fibrillation. Am J Cardiol. 2003;91:491–494. doi: 10.1016/s0002-9149(02)03258-7. [DOI] [PubMed] [Google Scholar]
- 25.Preedy VR, Siddiq T, Why H, Richardson PJ. The deleterious effects of alcohol on the heart: Involvement of protein turnover. Alcohol. 1994;29:141–147. [PubMed] [Google Scholar]
- 26.Adam A, Nicholson C, Owens L. Alcoholic dilated cardiomyopathy. Nurs Stand. 2008;22:42–47. [PubMed] [Google Scholar]
- 27.Singh KJ, Cohen BE, Na B, Regan M, Schiller NB, Whooley MA. Alcohol consumption and 5-year change in left atrial volume among patients with coronary heart disease: Results from the heart and soul study. J Card Fail. 2013;19:183–189. doi: 10.1016/j.cardfail.2012.12.005. [DOI] [PubMed] [Google Scholar]
- 28.Roerecke M, Rehm J. The cardioprotective association of average alcohol consumption and ischaemic heart disease: A systematic review and meta-analysis. Addiction. 2012;107:1246–1260. doi: 10.1111/j.1360-0443.2012.03780.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.