Abstract
The neuroactive steroids dehydroepiandrosterone (DHEA), its sulfate ester DHEA sulfate (DHEAS), and allopregnanolone (Allo), produced by the CNS and the adrenals, appear to exert a protective effect in hippocampal and cortical neuron ischemia- and excitotoxicity-induced injury. We hypothesized that they may also play a protective role on the adrenal medulla, an important part of the sympathetic nervous system, and the tissue adjacent to their primary site of production. DHEA, DHEAS, and Allo protected rat chromaffin cells and the rat pheochromocytoma PC12 cell line, an established model for the study of adrenomedullary cell apoptosis and survival, against serum deprivation-induced apoptosis. Their effects were time- and dose-dependent, with EC50 1.8, 1.1, and 1.5 nM, respectively. The antiapoptotic effect of DHEA DHEAS and Allo was compared to that of a long list of structurally related compounds and was found to be structure-specific, confined mainly to conformation 3β-OH-Δ5 for androstenes and 3α-OH for pregnanes. Indeed, 3-keto, Δ4, or C7 hydroxylated androstenes and 3β pregnanes were ineffective. The prosurvival effect of DHEA(S) and Allo was N-methyl-D-aspartate-, GABAA-, sigma1-, or estrogen receptor-independent. It involved the antiapoptotic Bcl-2 proteins, their role being sine qua non for their action because Bcl-2 antisense oligonucleotides reversed their effects. Finally, DHEA(S) and Allo activated cAMP response element-binding protein and NF-κB, upstream effectors of antiapoptotic Bcl-2 protein expression. They also activated the antiapoptotic kinase PKCα/β, a posttranslational activator of Bcl-2 protein. Our findings suggest that decline of DHEA(S) and Allo during aging or stress may leave the adrenal medulla unprotected against proapoptotic challenges.
The neuroactive steroids dehydroepiandrosterone (DHEA), its sulfate ester DHEA sulfate (DHEAS) and allopregnanolone (Allo) are produced in the brain and the adrenals (1–3). Their production rate and levels in serum and adrenals decrease gradually with advancing age (4–7). Physical or emotional stress may decrease them, characteristic paradigms being depression (8) and chronic inflammation (9). The decline of their levels is associated with neuronal dysfunction and degeneration (10–12), most probably because these steroids protect CNS neurons against noxious agents (13–15). Indeed, both DHEA and DHEAS [DHEA(S)] protects rat hippocampal neurons against N-methyl-D-aspartate (NMDA)-induced excitotoxicity (16), whereas Allo ameliorates NMDA-induced excitotoxicity in human neurons (17).
Based on these findings, we hypothesized that DHEA(S) and Allo may also play a protective role on the adrenal medulla, an important part of the sympathetic nervous system, and the tissue adjacent to their primary site of production. We first tested the ability of DHEA(S) and Allo to protect freshly prepared rat adrenal chromaffin and PC12 rat pheochromocytoma cells from serum deprivation-induced apoptosis. The latter is a well established NMDA- and GABAA-receptor negative (18, 19) model for the study of sympathoadrenal cell apoptosis (20–23). Subsequently, to assess the specificity of their action, we compared their antiapoptotic activity to a long list of androstene-, pregnane-, and pregnene-related compounds. Furthermore, to define their mechanism of action, we examined the possible receptors involved in this event, including intracellular and membrane estrogen-binding sites and the σ1 receptors (σ1R), known to have antiapoptotic activities (24, 25). Thus, the effect of DHEA(S) and Allo was examined in the presence of specific antagonists of these receptors. In addition, their protective effect was studied on a postreceptor level, starting with the antiapoptotic members of the Bcl-2 family, Bcl-2 and Bcl-xL, which play a central role in cell survival and are shown to be crucial in sympathetic neurons and PC12 cells (21, 26). Finally, we tested the effect of DHEA(S) and Allo on the activation of upstream effectors of prosurvival Bcl-2 gene expression and activation, including the transcription factors NF-κB, cAMP response element-binding protein (CREB), and PKCα/β. Indeed, the promoter regions of Bcl-2 and Bcl-xL genes contain a NF-κB-sensitive motif and cAMP response element (27–28), both being positive regulators of Bcl-2 and Bcl-xL gene expression and involved in the protection of neurons and PC12 cells (26, 29). PKCα/β has been shown to be involved in the activation of the Bcl-2 protein through phosphorylation at serine 70 (30, 31).
Materials and Methods
PC12 and Rat Chromaffin Adrenal Medulla Cells. PC12 cells were obtained from M. Greenberg (Children's Hospital, Boston). Cells were cultured at 5% CO2 and 37°C in RPMI medium 1640 containing 2 mM l-glutamine, 15 mM Hepes, 100 units/ml penicillin, 0.1 mg/ml streptomycin, and 10% horse serum, 5% FCS (both charcoal stripped for removing endogenous steroids), and different steroids at various concentrations, diluted in ethanol. The final concentration of ethanol in each well, including controls, was 0.1%. All steroids were purchased from Steraloids (Newport, RI). Chromaffin cells were isolated from rat adrenals surgically removed from adult female Sprague–Dawley rats, according to our protocol (32). Chromaffin cells of medulla were cultured for 5 days in DMEM-NUT FIX F12 medium containing 15 mM Hepes, 100 units/ml penicillin, 0.1 mg/ml streptomycin, and 10% charcoal-stripped FCS.
Quantitative Measurement of Apoptosis and FACS Analysis. The APOPercentage Apoptosis Assay (Biocolor, Belfast, Northern Ireland) was used to quantify apoptosis, according to the manufacturer's instructions (33). FACS analysis of apoptotic cells was performed according to our protocol (34). Flow cytometry was performed with FACScan (Becton Dickinson), and the results were analyzed with the FACScan cellquest software.
Western Blot Analysis. PC12 cells lysates were electrophoresed through a 12% SDS polyacrylamide gel, then proteins were transferred to nitrocellulose membranes, which were processed according to standard Western blotting procedures, as described (21). To detect protein levels, membranes were incubated with the appropriate antibodies: Bcl-2 (C-2, sc-7382, Santa Cruz Biotechnology, dilution 1:100) Bcl-xL (AMT no. 2762, Cell Signaling Technology, Beverly, MA; dilution 1:100). To detect the phosphorylated forms of CREB and PKC, the following antibodies were used: phospho-CREB, and phospho-PKCα/β (antibodies from Cell Signaling Technology, dilution 1:100). A personal computer-based image analysis program was used to quantify the intensity of each band (Image Analysis, Ontario, PQ, Canada).
To normalize for protein content, the blots were stripped and stained with antiactin antibodies (Chemicon, dilution 1:400); the concentration of each target protein was normalized vs. actin. Where phosphorylation of CREB and PKC was measured, membranes were first probed for the phosphorylated form of the protein, then stripped and probed for the total protein. The quantity of the phosphorylated proteins was expressed as the ratio of the phosphorylated protein divided by the total protein in each case.
RT-PCR. Total RNA was extracted from PC12 cells by using the Trizol Reagent (Invitrogen Life Technologies). One microgram of total RNA was reverse transcribed by using the Thermo-Script RT-PCR System (Invitrogen). The cDNA was amplified by PCR (Perkin–Elmer). PCR was performed in a Perkin–Elmer DNA Thermal Cycler with the following conditions: 30 s at 94°C, 30 s at 60°C (55°C for actin), and 60 s at 72°C for 35 cycles to detect the product at the exponential phase of the amplification. Ten microliters of the amplified products (242 bp for Bcl-2, 264 bp for Bcl-xL, and 174 bp for actin) was separated on a 2% agarose gel and visualized by ethidium bromide staining.
Primers for Bcl-2 were 5′-CTCGTCGCTACCGTCGTGACTTCG-3′ (sense), and 5′-CAGATGCCGGTTCAGGTACTCAGTC-3′ (antisense) and for Bcl-xL were 5′-AGGCTGGCGATGAGTTTGAACTGCG-3′ (sense) and 5′-GGCTCTAGGTGGTCATTCAGGTAGG-3′ (antisense). Primers for actin were 5′-CAT CCT GTC GGC AAT GCCAGG-3′ (sense) and 5′-CTT CCT GGG CAT GGA GTC CTG-3′ (antisense). Oligonucleotides were synthesized by MWG Biotech (Munich).
Bcl-2 Antisense Oligonucleotide Experiments. PC12 cells cultured in the absence or presence of steroids at 10–7 M were simultaneously exposed to antisense or nonsense 20-mer phosphorothioate oligodeoxynucleotides directed to the translation initiation site of Bcl-2 transcripts. Oligodeoxynucleotides were purchased from MWG Biotech: 5′-CAGCGTGCGCCATCCTTCCC-3′ (antisense), 5′-GGGAAGGATGGCGCACGCTG-3′ (sense), and 5′-TCGCCACTCGATCCTGCCCG-3′ (nonsense). Oligonucleotides were added to PC12 cultures to a final concentration of 50 μmol per liter.
Electrophoretic Mobility Shift Assay (EMSA). Nuclear extracts of PC12 cells treated with the three steroids at 10–7 M or with PMA for 1 h. The protein in each nuclear lysate was quantitated by using the Bradford assay (BioRad). One microgram of nuclear extracts was incubated with 5 × 105 cpm of a 32P-labeled double-stranded DNA probe representing the classical NF-κB-binding site (5′-ACAAGGGACTTTCCGCTGGGGACTTTCCAGGG-3′). Incubation was carried out for 30 min on ice in a binding buffer containing 20 mM Hepes (pH 7.5), 0.5 mM EDTA, 5 mM MgCl2, 50 μg/ml BSA, 0.005% Nonidet P-40, 60 mM KCl, 10 mM DTT, 10% glycerol, and 1.5 μg of poly(dI/dC).
Immunofluorescence Confocal Microscopy. PC12 cells were grown on glass or chamber slides and treated with steroids at 10–7 M for 1 h. At the end of the incubation, cells were fixed in 2% (wt/vol) formaldehyde for 10 min, permeabilized in 0.2% (wt/vol) Triton X-100 for 10 min, blocked in 1% FCS in PBS for 15 min, and then incubated overnight at 4°C with a rabbit p65 NF-κB antibody (sc-109, Santa Cruz Biotechnology) diluted 1:100 in PBS containing 1% FCS. Samples were washed with PBS and incubated for 1 h with fluorescein isothiocyanate-conjugated secondary anti-rabbit polyclonal antibody diluted 1/100. Cells were visualized under a confocal laser scanning microscope (TCS-NT, Leica, Heidelberg, Germany).
Statistical Analysis. For the statistical evaluation of our data, we have used analysis of variance, post hoc comparison of means followed by the Fisher's least significance difference test. For data expressed as percent changes, we have used the nonparametric Kruskal–Wallis test for several independent samples.
Results
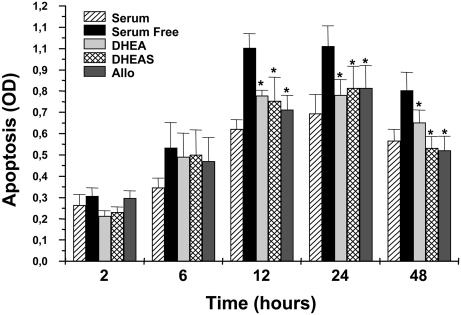
DHEA(S) and Allo Exerted an Antiapoptotic Effect on Normal and Tumoral Adrenal Chromaffin Cells. The effect of DHEA, DHEAS, and Allo was evaluated in primary cultures of serum-deprived freshly isolated rat adrenomedullary cells compared to parallel serum-supplemented cells. All three steroids exhibited a statistically significant protective effect on primary serum-deprived adrenomedullary cells (Fig. 1). Specifically, chromaffin cells cultured for 12 h in serum free medium in the absence of steroids showed an apoptosis rate of 1.10 ± 0.01 (expressed as OD units), compared to 0.77 ± 0.02, 0.75 ± 0.01, and 0.66 ± 0.03 apoptosis rates measured in the presence of DHEA, DHEAS, and Allo, respectively (mean ± SD, n = 3, P < 0.001). For comparison, serum supplementation for 12 h showed an apoptosis rate of 0.61 ± 0.04. Inhibition of apoptosis in chromaffin cells was retained for at least 48 h.
Fig. 1.
DHEA(S) and Allo protected rat chromaffin cells in culture against serum deprivation-induced apoptosis. Freshly isolated rat chromaffin cells were cultured either in complete or serum-free media containing 10–7 M DHEA, DHEAS, or Allo for various time periods (2–48 h). Apoptosis was quantified by the APOPercentage assay. Values represent mean ± SD of three independent experiments. Each measurement was performed in triplicate (*, P < 0.05).
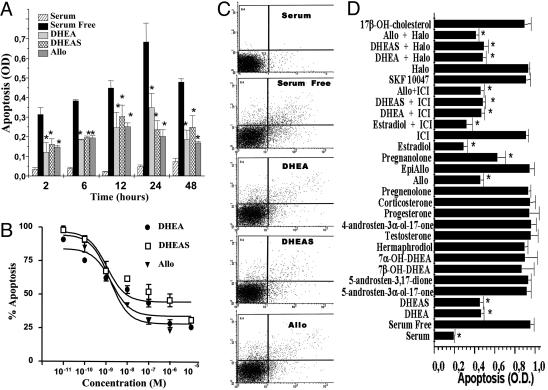
Based on these data, additional experiments were carried out by using the well established in vitro model of chromaffin cell apoptosis, the PC12 rat pheochromocytoma cell line (20). As expected, serum deprivation had a deleterious effect on PC12 cell cultures. FACS analysis revealed that 25% of PC12 cells maintained in serum-free medium underwent apoptosis within 24 h (Fig. 2C). Apoptosis of PC12 cells after serum deprivation became apparent as early as 2 h, peaking at 24 h (Fig. 2A), confirming previously published observations (21).
Fig. 2.
DHEA(S) and Allo protected PC12 rat pheochromocytoma cells against serum deprivation-induced apoptosis. Cells were cultured either in complete media (serum-supplemented) or serum-free media containing steroids as per protocol. (A) Time course. Cells cultured for various time periods (2–48 h) in serum-free medium in the absence or presence of 10–7 M DHEA, DHEAS, or Allo. Apoptosis was quantified by the APOPercentage assay, depicted as OD. Values represent mean ± SD of six separate experiments, each performed in triplicate (*, P < 0.05). (B) Dose response. Cells cultured for 24 h in serum-free medium containing different steroid concentrations ranging from 10–11 to 10–5 M. Apoptosis was quantified by the APOPercentage assay, depicted as percent of serum-free parallel controls. Values represent mean ± SD of three separate experiments, each performed in triplicate (*, P < 0.05). (C) Representative FACS analysis. Cells were cultured in 24-well plates (106 cells per well) for 24 h in serum-free media in the absence or presence of 10–7 M DHEA, DHEAS, or Allo. The x axis represents Annexin V-FITC, whereas the y axis represents the number of events. A total of 10,000 cells were assigned per treatment. (D) Cells were cultured for 24 h in serum-free media with various steroids at 10–7 M in the absence or the presence of 10–5 M of estrogen receptor antagonist ICI 182,780 or the σ1R antagonist haloperidol. Apoptosis was quantified by the APOPercentage assay, depicted as OD. Values represent mean ± SD of four separate experiments, each performed in triplicate (*, P < 0.05).
The effects of steroids were examined in serum-deprived PC12 cells and were compared to the protective effect of serum, according to the conditions used in the case of chromaffin cells. DHEA, DHEAS, and Allo exerted a strong time-dependent antiapoptotic effect (Fig. 2A). The antiapoptotic effect became apparent as early as 2 h and was maintained for at least 48 h, reaching its maximum at 24 h. Indeed, PC12 cells cultured for 24 h in serum-free medium in the absence of steroids showed an apoptosis rate of 0.69 ± 0.09, compared to 0.35 ± 0.07, 0.24 ± 0.04, and 0.20 ± 0.03 apoptosis rates measured in the presence of DHEA, DHEAS, and Allo, respectively (mean ± SD, n = 6, P < 0.001). Thus, all three steroids tested strongly inhibited serum deprivation-induced apoptosis by >50%, to the extent that their protective effects were also easily visualized under optical microscopy. For comparison, serum supplementation for 24 h showed an apoptosis rate of 0.047 ± 0.008, resulting, as expected, in higher protection. The antiapoptotic effects were dose-dependent with EC50 at 1.8, 1.1, and 1.5 nM for DHEA, DHEAS, and Allo, respectively (Fig. 2B)
Cytoprotection was also shown by using Annexin V/propidium iodine staining of apoptotic cells and subsequent FACS analysis. Fig. 2C depicts a mean 40% inhibition of serum deprivation-induced apoptosis in PC12 cells exposed to three steroids. Indeed, the percentage of apoptotic cells cultured in serum-free medium in the absence of steroids was 24.6%, compared to 15.1%, 16.9%, and 10.8% for DHEA, DHEAS, and Allo, respectively. This profile of FACS analysis was highly reproducible in at least three independent experiments.
The Antiapoptotic Effect of DHEA(S) and Allo Was Structure-Specific. To assess the specificity of the cytoprotective action of DHEA, DHEAS, and Allo, a host of structurally related compounds were also tested in parallel to our steroids. Structure–activity analysis revealed the following data. (i) Androstenes: (a) conformations 3α-OH, 3-keto, Δ4 (double bond at C4-C5) were inactive. Thus, the Δ4-3-keto steroids, including testosterone, progesterone, corticosterone, and 4-androsten-3β-ol-17-one, 5-androsten-3α-ol-17-one, and 5-androsten-3,17-dione, did not have any antiapoptotic activity in serum-starved cells (Fig. 2D); (b) hydroxylation at C7 (7α-hydroxy-DHEA, 7β-hydroxy-DHEA) or C17 (hermaphrodiol) resulted in loss of antiapoptotic activity (Fig. 2D). (ii) Pregnanes: Conformation 3α-OH was crucial because the 3β-OH analog of Allo, epi-Allo, had no effect (Fig. 2D). On the other hand, the α or β conformation of C5 was not critical for antiapoptotic activity, because pregnanolone and its sulfate ester were effective (Fig. 2D). Estradiol was used as an additional positive control (25) and was shown to effectively rescue serum-deprived PC12 cells from apoptosis, assessed with both the Apopercentage assay (Fig. 2D) and FACS analysis (data not shown).
The Antiapoptotic Effect of DHEA(S) and Allo Was Not Affected by Estrogen and σ1R Antagonists. Classically, it is assumed that for DHEA(S) to exert biological effects, they should first convert into androgens or estrogens. Our data indicated that the antiapoptotic effect of these steroids did not involve conversion, because routine immunoassay techniques failed to detect estradiol, estrone, and testosterone in our culture media of cells exposed to DHEA(S). Radiolabeled steroid-binding assays identified very low levels of intracellular estrogen (but not progesterone or androgen) receptors in cytosolic preparations of our cells (data not shown), confirming previous reports (35, 36). Additionally, the cytoprotective effects of DHEA(S) and Allo were not altered by the presence of a 100-fold molar excess (10–5 M) of estrogen receptor antagonist ICI 182,780 (Fig. 2D). Furthermore, dose–response curves and EC50 of DHEA(S) and Allo action were not affected by the presence of 10–5 M ICI 182,780 (data not shown). ICI 182,780 was also not effective in blocking the cytoprotective effect of estradiol (Fig. 2D). Recently identified membrane estrogen-binding sites were associated with the neuroprotective actions of estrogens in septal SN56 cells (37). We have thus tested the hypothesis that DHEA(S) and Allo have been cytoprotective in our system via binding on similar membrane sites. However, all three steroids, tested at concentrations from 10–12 to 10–6 M, failed to displace [3H]estradiol from its binding to PC12 membrane preparations (Fig. 7, which is published as supporting information on the PNAS web site). Membrane binding of [3H]estradiol was potent (IC50:10.5 nM) and highly specific, not displaceable by testosterone or progesterone.
Several 7-hydroxylated (7α-hydroxy-DHEA and 7β-hydroxy-DHEA) and 17-hydroxylated (hermaphrodiol) metabolites of DHEA or 7-hydroxylated DHEA precursor molecules (7-hydroxy-cholesterol) may serve as targets of apoptosis-associated intracellular receptors (38). In our hands, these four molecules were ineffective in rescuing PC12 serum-deprived cells from apoptosis (Fig. 2D). It thus appears that cytoprotection of serum-deprived cells by DHEA(S) cannot be attributed to their conversion to estrogens, androgens of active 7-hydroxylated metabolites, and subsequent activation of conventional steroid hormone receptors.
DHEA(S) and Allo interact with σ1Rs in various systems (39, 40), whereas several σ1R ligands are reported to have neuroprotective actions (24). Because PC12 cells express functional σ1Rs (41), we have tested the hypothesis that these neuroactive steroids may exert their antiapoptotic effects in serum-deprived cells through σ1R. However, the cytoprotective effect of DHEA(S) and Allo was not affected by the presence of a 100-fold molar excess (10–5 M) of σ1R antagonist haloperidol, and σ1R agonist SKF 10047 showed no cytoprotective properties (Fig. 2D). Additionally, dose–response curves and EC50 of DHEA(S) and Allo action were not affected by the presence of 10–5 M haloperidol (data not shown).
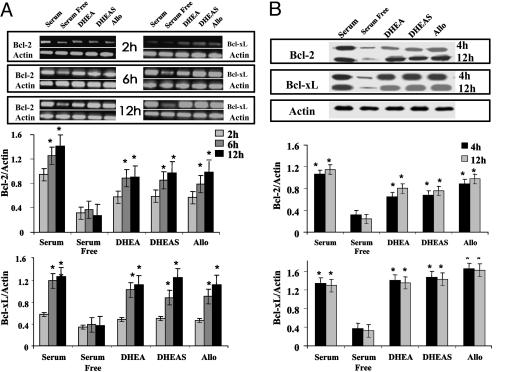
The Antiapoptotic Effect of DHEA(S) and Allo Was Mediated by Antiapoptotic Bcl-2 Proteins. Fig. 3 depicts serum deprivation suppression of antiapoptotic Bcl-2 and Bcl-xL mRNA and protein levels in PC12 cells. DHEA(S) and Allo were preventing this effect as early as 4 h to levels comparable to those of serum supplementation (Fig. 3B). Fig. 3A depicts their effect on the transcriptional level.
Fig. 3.
DHEA(S) and Allo induced the expression of the antiapoptotic Bcl-2 proteins in serum-deprived PC12 cells. Cells were cultured for 2–12 h either in complete or serum-free media containing 10–7 M DHEA, DHEAS, or Allo. Cellular extracts containing total mRNA or total proteins were collected, and levels of Bcl-2 and Bcl-xL mRNAs (A) and proteins (B) were measured either by semiquantitative RT-PCR or by Western blot, as described in Materials and Methods and normalized per actin mRNA or protein content, respectively. Values represent mean ± SD of three independent experiments (*, P < 0.05).
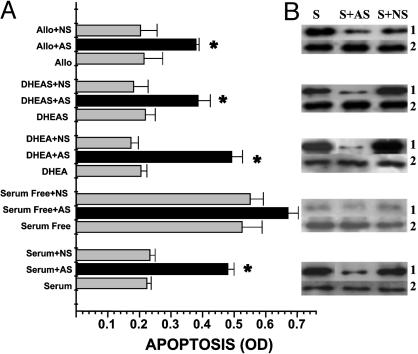
To confirm these data, further experiments were carried out by using Bcl-2 antisense oligonucleotides, which reversed the antiapoptotic cytoprotective effects of DHEA(S), and Allo (Fig. 4A). This effect was specific to AS treatment, because nonsense oligonucleotides were ineffective (Fig. 4A), and sense oligonucleotides (data not shown) did not show any significant effect in blocking steroid-induced cytoprotection. Western blot analysis showed that the Bcl-2 antisense manipulation was effective in inhibiting Bcl-2 protein production, except in the case of serum-deprived cells, cultured in the absence of steroids, where basal expression of Bcl-2 was already very low (Fig. 4B).
Fig. 4.
Antisense oligonucleotides against the Bcl-2 transcript reversed the cytoprotective effects of DHEA(S) and Allo on serum-deprived PC12 cells. Cells were cultured for 24 h in serum-free media containing 10–7 M DHEA, DHEAS, or Allo in the absence or the presence of 50 μmol per liter of nonsense (NS) or antisense (AS) 20-mer phosphorothioate oligodeoxynucleotides directed toward the translation-initiation site of the Bcl-2 transcript. Apoptosis was quantified by the APOPercentage assay (A) and the Bcl-2 proteins by Western blot (B). Values represent the mean ± SD of three independent experiments (*, P < 0.05); S, steroid; 1, Bcl-2; 2, actin).
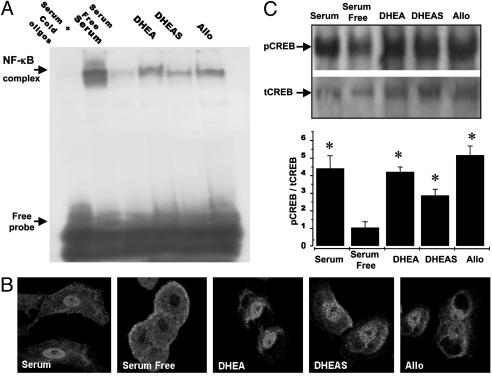
Effect of DHEA(S) and Allo on Prosurvival Transcription Factors NF-κB and CREB. In EMSA analysis shown in Fig. 5A, serum supplementation strongly induced NF-κB activity, which was almost blunted when PC12 cells were cultured in serum free media. The shift band (corresponding to NF-κB p50/p65 heterodimers) was completely eliminated when nuclear extracts from serum-supplemented PC12 cells were incubated with excess unlabeled cold NF-κB oligonucleotides (Fig. 5A). In serum-deprived cells, DHEA(S) and Allo were able to partially maintain NF-κB-binding activity, the most efficient being DHEA and Allo. Similar results were obtained in two additional EMSA experiments.
Fig. 5.
DHEA(S) and Allo activated transcription factors NF-κB and CREB in serum-deprived PC12 cells. Cells were cultured in complete or serum-free media containing 10–7 M DHEA, DHEAS, or Allo. (A) Representative EMSA assay, performed with 1 μg of nuclear extract of cells treated with steroids for 60 min, combined with 5 × 105 cpm of a 32P-labeled double-stranded DNA probe representing the NF-κB-binding site. Similar results were obtained in two additional independent experiments. (B) Confocal laser-scanning microscopy of cells grown on chamber slides and treated with steroids for 1 h were fixed and incubated with a rabbit anti-p65 NF-κB antibody and visualized by using FITC-conjugated secondary anti-rabbit polyclonal antibody. Cells were analyzed by using confocal laser-scanning microscopy (×400). (C) Western blot analysis of cells treated with steroids for 60 min, with antibodies specific for phosphorylated (pCREB) and total CREB (tCREB). Values are expressed as pCREB/tCREB ratio and represent mean ± SD of three independent experiments (*, P < 0.05).
Confocal laser scanning microscopy localization of p65 NF-κB corroborated to our EMSA data. Indeed, in PC12 cells cultured in serum-supplemented media NF-κB was almost exclusively localized within the nucleus, whereas in cells maintained in serum-free media NF-κB was found in the cytoplasm (Fig. 5B). In serum-deprived cells, exposed to steroids, NF-κB staining was mainly seen within the nucleus, as in the case of serum-supplemented cells (Fig. 5B).
Western blot analysis was performed for the phosphorylated and total forms of CREB. Serum deprivation resulted in a sharp, within 1 h, decrease of phosphorylated CREB, compared to serum-supplemented PC12 cells (1.05 ± 0.3 in serum-deprived compared to 4.41 ± 0.7 in serum-supplemented cells, n = 3, P < 0.005) (Fig. 5C). In serum-deprived cells exposed to steroids, levels of phosphorylated CREB were maintained to those seen in the presence of serum (DHEA, 4.21 ± 0.3; DHEAS, 2.87 ± 0.3; Allo, 5.16 ± 0.5; n, 3; P < 0.005) (Fig. 5C).
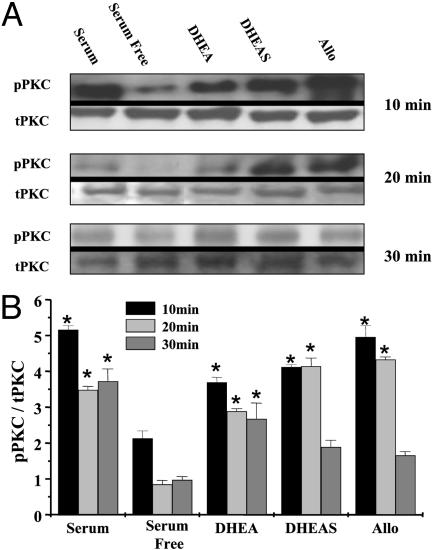
Effect of DHEA(S) and Allo on the Antiapoptotic Isoforms of PKC. Western blot analysis was performed for the phosphorylated and total forms of PKCα/β. Serum deprivation resulted in a acute (within 10 min) decrease of phosphorylated PKCα/β, compared with cells cultured in the presence of serum (2.13 ± 0.2 in serum-deprived compared to 5.16 ± 0.1 in serum-supplemented PC12 cells, n = 3, P < 0.05) (Fig. 6). In serum-deprived cells exposed to steroids for 10 min, levels of phosphorylated PKCα/β were maintained to those seen in the presence of serum (DHEA, 3.69 ± 0.2; DHEAS, 4.12 ± 0.1; Allo, 4.96 ± 0.3; n, 3; P < 0.05) (Fig. 6). The ability of neuroactive steroids to restore PKCα/β phosphorylation under serum deprivation was retained for at least 20 min.
Fig. 6.
DHEA(S) and Allo induced the phosphorylation of PKC in serum-deprived PC12 cells. Cells were cultured for 10–30 min either with complete or serum-free media, containing 10–7 M DHEA, DHEAS, or Allo. Western blot analysis was performed by using antibodies specific for phosphorylated (pPKC) and total (tPKC) conventional PKCα/β. Values are expressed as pPKC/tPKC ratio and represent mean ± SD of three independent experiments (*, P < 0.05).
Discussion
In human adrenals, the DHEA(S)- and Allo-producing cortical cells of zona reticularis and the chromaffin cells of the medulla are interwoven to suggest paracrine interactions, possibly via DHEA and Allo. Apart from the anatomical proximity, the decline of DHEA and Allo production and levels in serum and adrenals with advancing age and the parallel adrenomedullary malfunction further suggest interaction between these two parts of the adrenal gland. It should be noted that adrenomedullary cells divide throughout life, constantly requiring the presence of growth factors including nerve growth factor, insulin-like growth factor-II, and fibroblast growth factor type 2 (20, 42). Our findings suggest that DHEA(S) and Allo function as prosurvival agents against fluctuations in the local presence of growth factors. The decline of these steroids with aging or during chronic stress may leave the adrenal medulla unprotected against proapoptotic challenges. This effect appears to be structure-specific, requiring for DHEA an intact D5-3β-OH conformation and for Allo the conformation 3α-OH.
The protective effect of DHEA(S) and Allo appears independent of most known receptors, associated with neurodegenerative/neuroprotective processes. Our model, the PC12 cells, does not express functional NMDA and GABAA receptors (18, 19), and estrogen receptor and σ1R antagonists failed to reverse their antiapoptotic actions. The rapid onset of prosurvival signaling supports the hypothesis that these neuroactive steroids may use a membrane receptor system, although an intracellular receptor cannot be excluded. A DHEA-specific Gα protein-coupled membrane receptor has been identified in human and bovine endothelial cells, which, however does not bind DHEAS or Allo (43). It is thus possible that different binding sites mediate the action of DHEA(S) or Allo. This hypothesis is also supported by the differential structural requirements for cytoprotection of PC12 cells, between androstenes (DHEA) and pregnanes (Allo). It is also remarkable that in the same system, estrogen receptor (ER) antagonist ICI 182,780 failed to reverse the cytoprotective action of estradiol, suggesting that it does not seem to act through intracellular ER either. It is possible that estradiol exerts its cytoprotective action through the specific membrane-binding sites we identified in PC12 membrane preparations. Similar estrogen-binding sites, involved in cytoprotection from β amyloid toxicity, were recently reported in septal SN56 cells (37). The possibility of DHEA–Allo and E2 acting through the same membrane binding is weak, because DHEA(S) and Allo failed to displace tritiated estradiol from its binding on PC12 cell membranes. The exact nature of the receptor system mediating DHEA(S) and Allo cytoprotective actions in sympathoadrenal cells remains unknown. It is of note that various neuroactive steroids (DHEA and pregnenolone) were recently reported to bind on microtubule-associated proteins (44, 45), known to play a central role in neuronal cell death and survival (46).
Our data suggest that the prosurvival effect of DHEA(S) and Allo uses the major antiapoptotic pathway in sympathoadrenal cells, the antiapoptotic Bcl-2 proteins. Indeed, DHEA(S) and Allo induce the antiapoptotic Bcl-2 and Bcl-xL proteins. The role of these proteins appears crucial, because inhibition of their production by antisense oligonucleotides (directed toward the translation initiation site of the Bcl-2 transcript) resulted in an almost complete abolition of the protective effect of neuroactive steroids. The prosurvival pathway also included activation of the transcription factors NF-κB and CREB and the antiapoptotic kinase PKCα/β.
Finally, it should be mentioned that in diabetic rats, DHEA protects hippocampal neurons by preventing nitric oxide-induced activation of NF-κB (47) and in mice with experimental allergic encephalitis, DHEAS decreases demyelinization mediated by a decrease in activation and translocation of NF-κB (48). DHEAS also protects against glutamate-induced neurotoxicity via induction of NF-κB activity (49). In the present study, where the proapoptotic stimulus derived from an absence of growth factors, DHEA(S) and Allo reversed this deleterious effect via activation of the Bcl-2 prosurvival machinery. The observed activation of NF-κB and its role in inducing Bcl-2 and Bcl-xL protein production may suggest tissue and stimulus specificity in the downstream effectors of DHEA(S) and Allo. This is not unexpected, because it is known that NF-κB can act as either a proor an antiapoptotic effector, depending on cell type and internal milieu.
Supplementary Material
Acknowledgments
We thank Dr. G. P. Chrousos for helpful comments and discussions. This work was supported by a grant from the General Secretariat of Research and Technology (ΠENEΔ2001-EΔ258).
This paper was submitted directly (Track II) to the PNAS office.
Abbreviations: CREB, cAMP response element-binding protein; DHEA, dehydroepiandrosterone; DHEAS, DHEA sulfate; Allo, allopregnanolone; DHEA(S), both DHEA and DHEAS; σ1R, σ1 receptor.
References
- 1.Baulieu, E. E. & Robel, P. (1998) Proc. Natl. Acad. Sci. USA 95, 4089–4091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mensah-Nyagan, A. G., Do-Rego, J. L., Beaujean, D., Luu-The, V., Pelletier, G. & Vaudry, H. (1999) Pharmacol. Rev. 51, 63–81. [PubMed] [Google Scholar]
- 3.Compagnone, N. A & Mellon, S. H. (2000) Front. Neuroendocrinol. 21, 1–56. [DOI] [PubMed] [Google Scholar]
- 4.Orentreich, N., Brind, J. L., Rizer, R. L. & Vogelman, J. H. (1984) J. Clin. Endocrinol. Metab. 59, 551–555. [DOI] [PubMed] [Google Scholar]
- 5.Bélanger, A., Candas, B., Dupont, A., Cusan, L., Diamond, P., Gomez, J. L. & Labrie, F. (1994) J. Clin. Endocrinol. Metab. 79, 1086–1090. [DOI] [PubMed] [Google Scholar]
- 6.Genazzani, A. R., Petraglia, F., Bernardi, F., Casarosa, E., Salvestrone, C., Tonetti, A., Nappi, R. E., Luisi, S, Palumbo, M., Purdy, R. H., et al. (1998) J. Clin. Endocrinol. Metab. 83, 2099–2103. [DOI] [PubMed] [Google Scholar]
- 7.Bernardi, F., Salvestrone, C., Casarosa, E., Nappi, R. E., Lanxone, A., Luisi, S., Purdy, R. H., Petraglia, F. & Genazzani, A. (1998) Eur. J. Endocrinol. 138, 316–321. [DOI] [PubMed] [Google Scholar]
- 8.Wolkowitz, O. M., Epel, E. S. & Reus, V. I. (2001) World J. Biol. Psychiatry 2, 115–143. [DOI] [PubMed] [Google Scholar]
- 9.Straub, P. H., Lehne, K., Herfart, H., Weber, M., Falk, W., Preuner, J. & Scholmerich J. (2002) Eur. J. Endocrinol. 146, 365–374. [DOI] [PubMed] [Google Scholar]
- 10.Sapolsky, R. M. (1992) Stress, the Aging Brain and the Mechanism of Neuron Death (MIT Press, Cambridge, MA).
- 11.Seals, D. R. & Esler, M. (2000) J. Physiol. 528, 407–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Esler, M., Lambert, G., Kaye, D., Rumantir, M., Hastings, J. & Seals, D. (2002) Biogerontology 3, 45–49. [DOI] [PubMed] [Google Scholar]
- 13.Bastianetto, S., Ramassamy, C., Poirier, J. & Quirion, R. (1999) Brain Res. Mol. Brain Res. 66, 35–41. [DOI] [PubMed] [Google Scholar]
- 14.Cardounel, A., Regelson, W. & Kalimi, M. (1999) Proc. Soc. Exp. Biol. Med. 22, 145–149. [DOI] [PubMed] [Google Scholar]
- 15.Lapchak, P. A., Chapman, D. F., Nunez, S. Y. & Zivin, J. A. (2000) Stroke 31, 1953–1956. [DOI] [PubMed] [Google Scholar]
- 16.Kimonides, V. G., Khatibi, N. H., Svendsen, C. N., Sofroniew, M. V. & Herbert, J. (1998) Proc. Natl. Acad. Sci. USA 95, 1852–1857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lockhart, E., Warner, D., Pearlstein, R., Penning, D., Mehrabani, S. & Boustany, RM. (2002) Neurosci. Lett. 238, 33–36. [DOI] [PubMed] [Google Scholar]
- 18.Saito, Y., Tsuzuki, K., Yamada, N., Okado, H., Miwa, A., Goto, F. & Ozawa, S. (2003) Brain Res. Mol. Brain Res. 110, 159–168. [DOI] [PubMed] [Google Scholar]
- 19.Hales, T. G. & Tyndale, R. F. (1994) J. Neurosci. 14, 5429–5436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Greene, L. A. (1978) J. Cell Biol. 78, 747–755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dermitzaki, E., Chatzaki, E., Gravanis, A. & Margioris, A. N. (2000) J. Neurochem. 74, 960–969. [DOI] [PubMed] [Google Scholar]
- 22.Rong, P., Bennie, A. M., Ruwan-Epa, W. & Barret, G. L. (1999) J. Neurochem. 72, 2294–2300. [DOI] [PubMed] [Google Scholar]
- 23.Dermitzaki, E., Tsatsanis, C., Gravanis, A. & Margioris, A. N. (2002) J. Biol. Chem. 277, 12280–12287. [DOI] [PubMed] [Google Scholar]
- 24.Nakazawa, M., Matsuto, K. & Mita, S. (1998) Neurochem. Int. 32, 337–343. [DOI] [PubMed] [Google Scholar]
- 25.Gallapudi, L. & Oblinger, M. (1999) J. Neurosci. Res. 56, 99–108. [DOI] [PubMed] [Google Scholar]
- 26.Riccio, A., Ahn, S., Davenport, C. M., Blendy, J. A. & Ginty, D. D. (1999) Science 286, 2358–2361. [DOI] [PubMed] [Google Scholar]
- 27.Tamatani, M., Che, Y. O., Matsuzaki, H., Ogawa, S., Okado, H., Miyake, S. H., Mizuno, T. & Tohyama, M. (1999) J. Biol. Chem. 274, 8531–8538. [DOI] [PubMed] [Google Scholar]
- 28.Mori, N., Fujii, M., Cheng, G., Ikeda, S., Yamasaki, Y., Yamada, Y., Tomonaga, M. & Yamamoto, N. (2001) Virus Genes 22, 279–287. [DOI] [PubMed] [Google Scholar]
- 29.Mattson, M. P., Culmesee, C., Yu, Z. & Camandola, S. (2000) J. Neurochem. 74, 443–456. [DOI] [PubMed] [Google Scholar]
- 30.Ito, T., Deng, X., Carr, B. & May, W. (1997) J. Biol. Chem. 272, 11671–11673. [DOI] [PubMed] [Google Scholar]
- 31.Ruvolo, P., Deng, X., Carr, B. & May, W. S. (1998) J. Biol. Chem. 273, 25436–25442. [DOI] [PubMed] [Google Scholar]
- 32.Venihaki, M., Gravanis, A. & Margioris, A. N. (1997) Endocrinology 138, 698–704. [DOI] [PubMed] [Google Scholar]
- 33.Johnson, J. D., Ahmed, N. T., Luciani, D. S., Han, Z., Tran, H., Fujita, J., Misler, S., Edlund, H. & Polonsky, K. S. (2003) J. Clin. Invest. 111, 1147–1160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Makrigiannakis, A., Zoumakis, E., Kalantaridou, S., Coutifaris, C., Margioris, A. N., Rice, C. K., Chrousos, G. P. & Gravanis, A. (2001) Nat. Immunol. 2, 1018–1024. [DOI] [PubMed] [Google Scholar]
- 35.Lustig, R. H., Hua, P., Smith, L. S., Wang, C. & Chang C. (1994) Mol. Cell. Neurosci. 5, 587–596. [DOI] [PubMed] [Google Scholar]
- 36.Lustig, R. H., Hua, P., Yu, W., Ahmad, F. J. & Baas, P. W. (1994) J. Neurosci. 14, 3945–3957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Marin, R., Guerra, B., Morales, A., Diaz, M. & Alonso, R. (2003) J. Neurochem. 85, 1180–1189. [DOI] [PubMed] [Google Scholar]
- 38.Lathe, R. (2002) Steroids 67, 967–977. [DOI] [PubMed] [Google Scholar]
- 39.Maurice, T., Urani, A., Phan, V. L. & Romieu, P. (2001) Mol. Brain Res. 37, 116–132. [DOI] [PubMed] [Google Scholar]
- 40.Monnet, F. P., Mahe, V., Robel, P. & Baulieu, E. E. (1995) Proc. Natl. Acad. Sci. USA 92, 3774–3778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Takebayashi, M., Hayashi. T. & Su, T. P. (2002) J. Pharmacol. Exp. Ther. 303, 1227–1237. [DOI] [PubMed] [Google Scholar]
- 42.Unsicker, K. (1993) Exp. Neurol. 123, 167–173. [DOI] [PubMed] [Google Scholar]
- 43.Liu, D. & Dillon, J. S. (2002) J. Biol. Chem. 277, 21379–21388. [DOI] [PubMed] [Google Scholar]
- 44.Murakami, K., Fellous, A., Baulieu, E. E. & Robel, P. (2000) Proc. Natl. Acad. Sci. USA 97, 3579–3684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Laurine, E., Lafitte, D., Gregoire, C., Seree, E., Loret, E., Douillard, S., Michel, B., Briand, C. & Vernier, J. M. (2003) J. Biol. Chem. 276, 29979–29986. [DOI] [PubMed] [Google Scholar]
- 46.Sheetz, M., Pfister, K., Bulinski, J. C. & Cotman, C. W. (1998) Prog. Neurobiol. 55, 577–594. [DOI] [PubMed] [Google Scholar]
- 47.Aragno, M., Mastrocola, R., Brignardello, E., Catalano, M., Robino, G., Manti, R., Parola, M., Danni, O. & Boccuzzi, G. (2002) Endocrinology 143, 3250–3258. [DOI] [PubMed] [Google Scholar]
- 48.Du, C., Khalil, M. & Sriram, S. (2001) J. Immunol. 167, 7094–7101. [DOI] [PubMed] [Google Scholar]
- 49.Mao, X. & Barger, S. W. (1998) NeuroReport 9, 759–763. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.