Abstract
Average life expectancy is increasing in the western world resulting in a growing number of frail individuals with coronary heart disease, often associated with comorbidities. Decisions to proceed to invasive interventions in elderly frail patients is challenging because they may gain benefit, but are also at risk of procedure-related complications. Current risk scores designed to predict mortality in cardiac procedures are mainly based on clinical and angiographic factors, with limitations in the elderly because they are mainly derived from a middle-aged population, do not account for frailty and do not predict the impact of the procedure on quality of life which often matters more to elderly patients than mortality. Frailty assessment has emerged as a measure of biological age that correlates well with quality of life, hospital admissions and mortality. Potentially, the incorporation of frailty into current risk assessment models will cause a shift towards more appropriate care. The need for a more accurate method of risk stratification incorporating frailty, particularly for elderly patients is pressing. This article reviews the association between frailty and cardiovascular disease, the impact of frailty on outcomes of cardiac interventions and suggests ways in which frailty assessment could be incorporated into cardiology clinical practice.
Introduction
Increasing life expectancy is resulting in a corresponding rise in the average age of patients presenting with cardiovascular diseases (CVDs). Ageing is characterised by a reduction in functional reserve. Frailty is an increased vulnerability to minor stressors that develops because of age-related decline. With frailty, this decline is accelerated and homoeostatic mechanisms start to fail.1 Apoptosis, senescence, repair, inflammation and immune activation have all been implicated as pathways responsible for this decline (figure 1).
Figure 1.
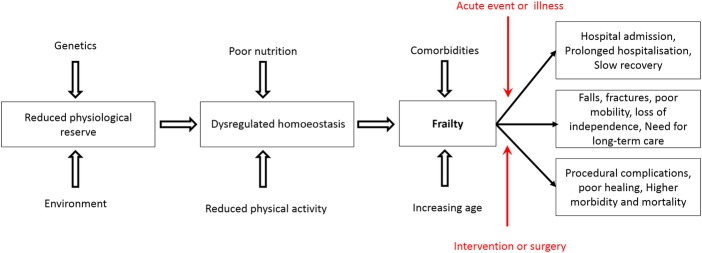
Schematic representation of the pathophysiology of frailty.
‘Biological age’ is often taken as a crude index of frailty, while chronological age is a poor correlate. Indeed up to 75% of patients over the age of 85 years are not frail.2 Frailty assessment correlates well with quality of life (QoL), hospital admissions and mortality.3–5 The importance of frailty has been acknowledged by the American Heart Association (AHA) which has called for a better understanding of frailty in cardiac care.6 They have suggested that trials should include improved characterisation of the elderly population and the evaluation of the influence of frailty and cognitive decline on outcomes.
The need to include frailty assessment in decision-making is pressing. Treating an elderly patient often involves high-risk, high-gain treatments.7 Incorporation of frailty in risk stratification may help distinguish older patients who may benefit from intervention from those who will gain little benefit or may even be harmed by aggressive intervention.7 This article reviews the association between frailty and CVD, the impact of frailty on outcomes of cardiac interventions, how to incorporate frailty assessment in clinical practice and proposes future directions in this field.
Assessment of frailty
There is no consensus as to how frailty should be assessed. A report from six major international, European and US societies in geriatric medicine recommends that all patients >70 years should be screened for frailty.8 Yet, they give no recommendation on how to identify frailty.
Subjective ‘end-of-the-bed’ test
Traditionally, assessment of frailty was based purely on clinical judgement. This ‘end-of-the-bed test’ still plays a key role and is an attempt to assess the patient's frailty based on simple visual appearance. However, frailty may not be visually obvious and ‘apparent frailty’ can vary between encounters, depending on the specific environment (hospital, community, clinic), the time of day, recent sleep disturbance, nutritional status and mood. A subjective approach to assessment therefore has limitations and potential bias. A simple, objective, universal and readily available test or score would be useful.
Frailty scores
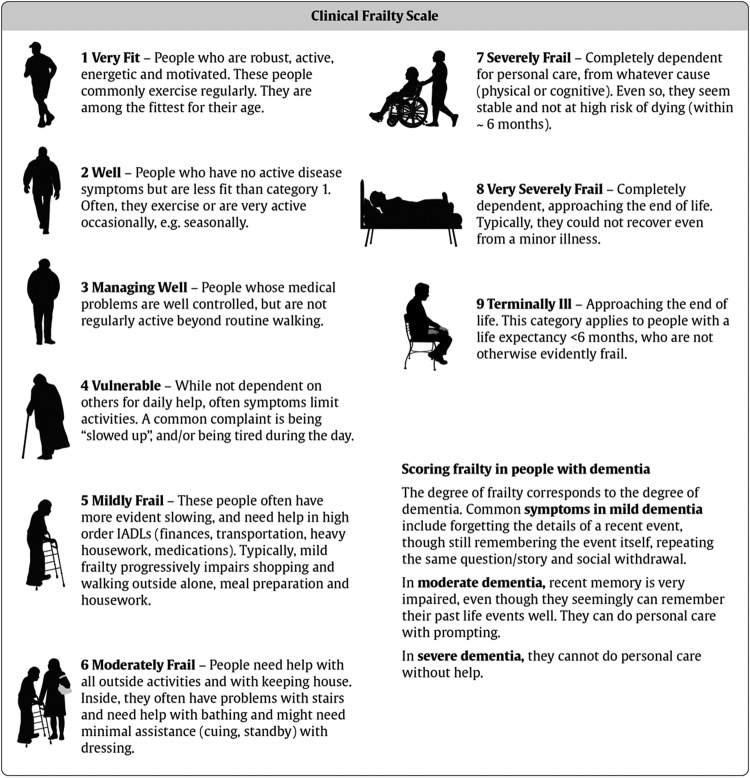
A number of frailty scores have been designed by geriatricians comprising a combination of functional tests, laboratory tests, questionnaires, descriptive scales, disability assessments and comorbidity assessments. High scores in these are associated with adverse outcomes in elderly patient populations and may aid clinical management. The most commonly used scores are summarised in table 1. Comprehensive geriatric assessment takes into consideration the multiple interacting medical and social needs of patients, how illness impacts on function and how each of these affect healthcare outcomes.9 Comprehensive Assessment of Frailty (CAF) is a tool to assess prognosis in elderly cardiac surgery patients.10 However, it is complex and takes 10–20 min to perform. The practicality of incorporating it into routine preoperative cardiac assessment would be challenging. A study has compared frailty scores with disability scores and cardiac risk scoring systems. The frailty scores assessed were the Cardiovascular Health Study (CHS) scale, the expanded CHS scale, the MacArthur Study of Successful Ageing (MSSA) scale and gait speed alone. They applied these to 152 patients, aged >70 years undergoing coronary artery bypass graft (CABG) and/or valve surgery.11 Frailty prevalence ranged from 20% to 46%, depending on the frailty score. The addition of frailty and disability to the Society of Thoracic Surgeons (STS) score improved model discrimination. The most predictive frailty score was 5 m gait speed.11 Another study using gait speed to measure frailty demonstrated an increased risk of cardiovascular events after ST-elevation myocardial infarction (STEMI) in patients with slow gait.12 Gait speed was measured prior to discharge. Although this is useful to allow prediction of future events, it is not helpful at presentation. Therefore, for frailty to be incorporated into preprocedural risk assessment, a different form of assessment is required. We and others have found that Canadian Study of Health and Ageing score (figure 2) is an easy and reliable tool to assess frailty.13–15
Table 1.
Frailty risk assessment scores
| FFS | MSSA | MFS | CAF | FORECAST | |
|---|---|---|---|---|---|
| Number of indicators | 5 | 4 | 5 | 6 | 5 |
| Weight loss >5 kg in preceding year | Y | Y | |||
| Grip strength >16 kg | Y | Y | Y | Y | |
| Low levels of physical activity | Y | Y | |||
| 6 min walk <210 m | Y | Y | Y | ||
| SF-36 <40% for energy and vitality | Y | ||||
| MMSE <24 | Y | Y | |||
| Get-up-and-go >17 s | Y | ||||
| FEV1 <30% | Y | ||||
| Put on and remove jacket | Y | ||||
| Pick up a pen from floor | Y | ||||
| Balance | Y | ||||
| Get up and down from a chair—performed three times | Y | Y | |||
| Feeling weak over the past 2 weeks | Y | ||||
| Serum creatinine | Y | ||||
| Stair climb assessment | Y | ||||
| CSHA Clinical Frailty Scale | Y |
CAF, comprehensive assessment of frailty; CSHA, Canadian study of health and ageing; FEV1, forced expiratory volume in 1 s; FFS, Fried frailty score; FORECAST, Frailty predicts death 1 year after Elective Cardiac Surgery Test; MFS, motor fitness scale; MMSE, Mini-Mental State Examination; MSSA, McArthur study of successful ageing.
Figure 2.
Canadian study of health and ageing score.
Challenges in frailty assessment
The utilisation of frailty assessment in healthcare is not without its potential limitations. There is a subjective element in the majority of frailty scores, allowing for some potential incongruity. Yet this is still less subjective than a poorly documented (or not performed) ‘end-of-the-bed’ test. This subjectivity could predispose clinicians calculating a risk score to shape a desired figure. With the publication of outcomes across surgical specialties and interventional cardiology, this is even more relevant. The use of an objective measure of frailty would prevent this. Additionally, frailty is a dynamic risk factor and could vary significantly between clinic encounters. However, health status is also dynamic and this could just shadow this. Further research on the stability of frailty measurement as a risk factor is required.
Impact of frailty on health and clinical outcomes
Frailty has been explored in a number of disease-specific cohorts. For example, frailty independently predicts mortality in patients undergoing haemodialysis and following community-acquired pneumonia.16 The European Male Ageing Study Group identified frailty as a predictor of all-cause mortality.17 Similarly, frailty is associated with increased mortality in patients attending acute medical units and in those being admitted from emergency departments.13 18 Frailty has also been associated with surgical outcomes, including postoperative mortality and rehospitalisation.19
Frailty and CVD
Frailty is a predictor of mortality in patients with CVD independent of age, underlying disease severity, comorbidities and disability (table 2).20 21 The link between frailty and CVD was first noted in a secondary analysis of a study of community dwelling elders. Of the frail patients, 62% had coexisting CVD compared with 28% of the ‘non-frail’.22 The CHS disclosed a threefold increase in the presence of frailty in patients with CVD, a relationship extending to subclinical CVD including increased left ventricular (LV) mass and ECG abnormalities.23 In another study of 2515 individuals, an increase in the frailty score by one point of five was associated with a 35% increase in the risk of having CVD and a 20% increase in the risk of having hypertension.24 In the Women's Health Initiative observational study the presence of coronary artery disease (CAD), stroke, hypertension or diabetes in non-frail patients was predictive of frailty developing during 3 years of follow-up. The development of frailty was, in turn, predictive of all-cause mortality.25 Frailty is a risk factor for the development and progression of CVD, while CVD can lead to frailty. It is, therefore, conceivable that treating one might improve the other. ACE inhibitors, a standard treatment to improve morbidity and mortality in heart failure, also improve functional status and exercise capacity in elderly patients with no history of heart failure or LV systolic dysfunction.26
Table 2.
Summary of most relevant studies of frailty in cardiovascular disease
| Authors | Study cohort and size | Frailty criteria | Findings |
|---|---|---|---|
| Chin et al 51 | Age 69–89, n=450 | Inactivity combined with low energy intake, weight loss or low body mass index | 62% of frail patients had coexisting cardiovascular disease compared with 28% of the ‘non-frail’ |
| Newman et al 23 | Community dwelling older adults, n=4735 | 3/5 of: self-reported weight loss, low grip strength, low energy, slow gait speed, and low physical activity | Threefold increase in frailty in patients with cardiovascular disease |
| Klein et al 52 | Population based study of mid-western adults, n=2515 | Gait speed, handgrip strength, peak respiratory flow rate, ability to stand from a sitting position without using arms, and corrected visual acuity | Increase in frailty score by 1/5 was associated with a 35% increase in the presence of cardiovascular disease |
| Woods et al 25 | Women aged 65–79, n=40 657 | Self-reported muscle weakness/impaired walking, exhaustion, low physical activity, and unintended weight loss | Baseline frailty independently predicted risk of death (HR 1.71, 95% CI 1.48 to 1.97) |
| Mcnallan et al 27 | Heart failure, n=448 | 3 or more of the following: unintentional weight loss, exhaustion, weak grip strength, and slowness and low physical activity | Frailty was associated with a 92% increased risk of emergency department visits and 65% increased risk of hospitalisation |
| Polidoro et al 28 | Patients with AF, n=140 | Standard score of accumulated deficits | Increased number of frail patients in AF cohort (88.6% vs 67.1%, p=0.004) |
| Matsuzawa et al 12 | Patients with NSTEMI and >75 years old, n=472 | Gait speed | Gait speed was a significant independent predictor of cardiovascular events |
| Sunderman et al 53 | CABG, valve surgery or TAVI, n=400 | CAF score | Significant correlation between frailty score and 30-day mortality |
| Schoenenberger et al 39 | TAVI, n=106 | Frailty index | Frailty strongly predicted functional decline after TAVI |
| Singh et al 46 | >65 years undergoing PCI, n=628 | Fried frailty scale | Frailty was associated with mortality/MI at 3 years (HR 2.61, 95% CI 1.52 to 4.50) |
AF, atrial fibrillation; CAF, Comprehensive Assessment of Frailty; CABG, coronary artery bypass graft; MI, myocardial infarction; NSTEMI, non-ST-elevation myocardial infarction; PCI, percutaneous coronary intervention; TAVI, transcatheter aortic valve implantation.
Frailty, heart failure and atrial fibrillation
Heart failure in the elderly is a major public health problem and the prevalence is rising. The prognosis remains poor. Frailty has been identified as a major predictor of mortality in elderly patients with heart failure. One study examined the effect of frailty on healthcare utilisation in patients with heart failure. Frailty was associated with a 92% increased risk of hospital attendance and a 65% increased risk of admission.27 A relationship between frailty and atrial fibrillation (AF) has also recently been described. Polidoro et al28 assessed patients with AF for frailty and compared them to age-matched and sex-matched controls. AF was strongly associated with high frailty score.28 AF might, therefore, be a surrogate for frailty. Indeed, it is well described that AF is associated with a significant increase in morbidity and mortality after the adjustment for pre-existing cardiovascular conditions with which AF is associated.29 The impact of associated ‘frailty’ could contribute to this.
Frailty and acute coronary syndromes
Frailty can help predict adverse outcomes in elderly patients with CAD.30 Of 307 patients aged over 75 years with non-STEMI. In total, 149 (48.5%) were frail and experienced increased rates of re-infarction, revascularisation, hospitalisation, major bleeding, stroke and need for dialysis and mortality compared with non-frail.14 Another study undertaken in patients following STEMI demonstrated an increased risk of future cardiovascular events in those with increased frailty.12 In the highest tertile, 36.7% experienced cardiovascular events compared with 3.2% in the lowest tertile.
Frailty and neurovascular diseases
Frailty has also been associated with neurovascular diseases including stroke, dementia and vascular depression. Frailty has been shown to have an association with stroke and cognitive impairment, independent of age, physical activity level and muscle mass.31 Frail individuals also have greater cognitive decline with the passage of time as compared with age-matched non-frail participants.32 A prospective study at three French centres assessed 5480 community dwellers aged 65–95 years and followed them up for 7 years. Frailty was independently associated with incident vascular dementia but not with other types of dementia including Alzheimer’s disease.33 It has also been suggested that vascular depression is a prodrome for frailty.34 These associations have important bearings on the assessment of frailty because it may be difficult to distinguish mental and physical frailty and they may impact the management of associated comorbidities, compliance with medication and especially the decision to embark on invasive cardiovascular therapies.
Frailty and cardiac interventions
The number of elderly patients undergoing all forms of cardiac interventional procedures including revascularisation, valve replacement and the implantation of pacemakers and other devices has increased in recent years. Hence, frailty is particularly relevant in all these areas.
Frailty and cardiac surgery
Sundermann et al10 made a CAF in 400 patients aged 74 years and older undergoing elective cardiac surgery. Patients underwent CABG (n=90), isolated valve surgery (n=128), transcatheter valve implantation (n=59) or a combined procedure (n=123). One hundred and ninety-nine were not frail, 170 had intermediate frailty and 31 were frail. Frailty was a risk factor for 30-day mortality (p<0.05). Patients who died had a significantly higher frailty score compared with those who survived (p=0.001). However, CAF is complex and time consuming. The investigators therefore also tested a simplified version of the CAF (FORECAST), which took 3–5 min to complete and was also associated with increased 1-year mortality. This relationship was confirmed in a study of 3826 patients undergoing cardiac surgery.35 Frailty was an independent predictor of hospital mortality, delayed discharge and mid-term survival. Afilalo et al examined the effect of frailty alongside the STS score. Using a logistic regression model containing the STS score, frailty was an independent predictor of mortality and morbidity and incorporation into the STS model increased the performance of the latter.36
Frailty and transcatheter aortic valve implantation
Transcatheter aortic valve implantation (TAVI) has emerged as a less invasive alternative to surgical aortic valve replacement for high-risk patients with severe aortic stenosis. These patients are typically elderly with multiple comorbidities. Green et al evaluated the impact of frailty on periprocedural complications and 1-year mortality. There was no impact of frailty on periprocedural complications, but it was associated with 1-year mortality.37 A Canadian group found frailty to be a predictor of late mortality alongside chronic obstructive pulmonary disease, renal impairment and AF.38 These associations were independent of each other. Schoenenberger et al39 found that the frailty index strongly predicted functional decline after TAVI whereas neither the EuroSCORE nor STS did (p=0.35 and 0.13, respectively).
Frailty and implantable cardiac device therapy
The mean age of patients included in large randomised trials of cardiac device therapies was typically 60–65 years and patients with multiple comorbidities were usually excluded. Yet the US Healthcare Cost and Utilization Project40 indicates that approximately 45% of patients receiving cardiac resynchronisation therapy (CRT) and 28% of patients receiving implantable cardioverter defibrillator (ICD) are aged 75 or older. Three or more comorbidities were present in at least 20% of these patients, suggesting that a substantial proportion were frail. The role of implantable cardiac devices in frail elderly patients has yet to be fully explored and there remains considerable doubt about their clinical value in this setting. Frailty assessment in studies of CRT, bradycardia pacing, biventricular pacing and implantable cardioverter defibrillators (ICD) seems overdue. Flint et al41 proposed the incorporation of frailty assessment into the assessment of patients for left ventricular assist devices implantation. There are no studies that have formally explored this.
Frailty and percutaneous coronary intervention
A 3-year study characterised frailty and health status in percutaneous coronary intervention (PCI)-treated patients over 65. Of 545 patients, 21% were not frail while others had some degree of frailty. Frail patients had more comorbidities and more frequent left main coronary artery or multivessel disease. The Angina questionnaire and QoL scores were lower in frail patients.42 Singh et al assessed frailty comorbidity and QoL in 628 patients over the age of 65 years who underwent PCI. One hundred and thirty were not frail while 415 (66%) patients had some degree of frailty. Frail patients had more comorbidities and were more likely to have multivessel disease than non-frail patients. Three-year mortality was 28% for frail patients and 6% for non-frail. The addition of frailty to the Mayo clinic risk score increased the accuracy for the prediction of mortality.43
Frailty in risk stratification for revascularisation
In a study of 15 382 patients >70 years who underwent coronary revascularisation, 4-year adjusted actuarial survival rates for CABG, PCI and medical therapy were 95%, 93.8% and 90.5%, respectively. For patients >80 years corresponding rates were 77.4%, 71.6% and 60.3%, respectively.7 Elderly patients undergoing coronary revascularisation had a better health status than age-matched controls who did not undergo intervention.44
Risk stratification in PCI
The highest in-hospital mortality rates following PCI are seen among elderly patients, however, overall mortality has decreased in recent years, with the largest absolute reduction seen in patients >80 years.45 These patients represent both high risk and high benefit, and the decision-making process should rely on accurate risk modelling incorporating frailty. Numerous risk stratification models for PCI and CABG have been developed, but they perform poorly in elderly patients with multiple comorbidities. Most current models of risk in the field of CVD are heavily weighted towards age. With all other variables used in the scores kept the same, risk continues to increase with age alone. Thus, an otherwise healthy 80-year-old individual has a significantly higher risk score than a 60 year-old, regardless of how healthy, independent or non-frail he or she is (figure 3). The presence of comorbidities is used as a surrogate of frailty. However, this neglects those that are frail without significant comorbidities. Additionally, overestimation of risk in the elderly non-frail can occur.
Figure 3.
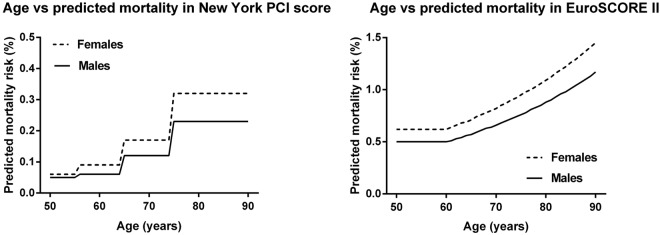
Age versus predicted mortality in the EuroSCORE and New York percutaneous coronary intervention scores, with all other variables kept as normal.
PCI is increasingly used for treating elderly patients with acute coronary syndrome, often with little or no opportunities for any form of frailty assessment. Predicting risks and benefits is challenging because the proportion of elderly patients in randomised revascularisation trials is lower than seen in the ‘real world’. Existing models for outcome after PCI lack assessment of long-term prognosis. For example, the Mayo clinic score predicts in-hospital mortality but not long-term outcomes or QoL.43 The addition of frailty to the Mayo clinic risk score increased the accuracy of the prediction (using the c-statistic) of mortality from 0.63 to 0.68 and of mortality/MI from 0.57 to 0.61.46 Further studies addressing the ability of frailty scores to improve prediction of morbidity and mortality associated with coronary revascularisation are needed.
Risk stratification in cardiac surgery
The two most widely used models of perioperative risk in cardiac surgery are the EuroSCORE II and the STS score both of which, like most risk models, are inaccurate in estimating individual risk.10 47 In both, medical diagnoses and comorbidities are heavily weighted, yet frailty is not represented. Although these allude to a prediction of frailty, this is not comprehensive and a role for frailty in risk stratification independent of both age and comorbidities exists. The updated EuroSCORE II includes ‘poor mobility’ as a risk factor. This allows a representation of frailty and improves the accuracy of the score. However, mobility alone does not necessarily equate to frailty. It may be a simple surrogate in some circumstances, but the score does not define poor mobility or permit its quantification beyond a simple ‘present’ or ‘absent’. With ageing of the patient population, these models underestimate risk at higher levels.48 The incorporation of frailty into these scores has the potential to increase their accuracy. The correlations between the CAF and EuroSCORE and STS scores are low (0.35 and 0.42, respectively),10 suggesting that CAF overlaps only partly with EuroSCORE and STS score and may therefore augment them. Afilalo et al36 found no correlation between frailty as assessed by time taken to walk 5 m and STS score and showed that incorporation of frailty into the STS model increased the performance of the latter.
Current recommendations and future directions
Frailty is increasingly recognised as a specific clinical condition associated with poorer outcomes in many areas of medicine and surgery. Recommendations related to frailty have already been incorporated into medical guidelines for diabetes. With further work, this could be replicated in other areas including cardiology and cardiac surgery. It is important that cardiologists and cardiothoracic surgeons are aware of how to assess frailty and of its potential impact on clinical outcomes. At present, there is no consensus on how to assess frailty and a number of clinical trials are using different frailty scales. Which of these scores has the best predictive power, and which is most appropriate in specific clinical settings remains to be determined. However, it is clear that a simple, universally applicable and readily understood frailty ‘score’ is much needed. In addition, many studies simply split frailty into ‘frail’ or ‘non-frail’, which does not accurately represent the typical patient population, most of which have some degree of frailty. It is perhaps better to use a gradation of frailty; for example, the Canadian study of health and ageing score, or a score, which allows discrimination of severely frail high-risk individuals could also be helpful. It is possible that a universal tool would not be applicable in all settings and that each specialty may need to find a frailty tool that suits their own needs. The concept of a community-based frailty score for all elderly patients is an attractive idea and one that could be readily achieved within the primary care contractual system (QoF). This would ensure that all frail patients presenting acutely to secondary care services would be flagged in advance and decision-making could be modified accordingly.
Frailty still plays little formal part in most decision-making processes in CVD. In line with contemporary guidelines, decisions are ideally made in multidisciplinary team meetings (the ‘heart-team’).49 The majority of the team will have never met the patient, and rely on a subjective patchy and probably inaccurate description of health status together with cardiac imaging. A formal assessment of frailty could help in providing more objective and transparent decision-making in this setting. With increasing evidence highlighting the predictive power of frailty across cardiovascular medicine, our focus needs to be directed at how we can incorporate this into current methods of risk assessment. The Royal College of Emergency Medicine has suggested developing specialised ‘Frailty Units’ for frail elderly patients. A recent practical example of using frailty in decision-making has been established by the European Working Group on target guidelines for diabetes by recommending a conservative glycated haemoglobin in frail patients compared with age-matched non-frail.50 In keeping with the AHA guidelines, more elderly and frail people should be included in future trials, as well as focusing on QoL outcomes in addition to mortality. Incorporating frailty assessment in risk scoring and decision-making will help to decide whether a frail patient should undergo a procedure or whether it might improve QoL.
Conclusion
Frailty is an independent risk factor for adverse outcomes in CVD and following cardiac intervention. As we are faced with an increased number of elderly patients with CVD and frailty, frailty assessment can help in risk stratification and decision-making, thereby improving outcomes and QoL, and preventing unnecessary harm in the most frail. We need to measure frailty in a consistent way in clinical studies, and find a way to incorporate measures of frailty in outcome studies.
Footnotes
Contributors: JI and JG conceived the idea. RR and RM-K wrote the first draft. All authors critically reviewed the paper and approved the final version.
Competing interests: None.
Provenance and peer review: Not commissioned; internally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Clegg A, Young J, Iliffe S, et al. Frailty in elderly people. Lancet 2013;381:752–62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Song X, Mitnitski A, Rockwood K. Prevalence and 10-year outcomes of frailty in older adults in relation to deficit accumulation. J Am Geriatr Soc 2010;58:681–7 [DOI] [PubMed] [Google Scholar]
- 3.Mitnitski AB, Graham JE, Mogilner AJ, et al. Frailty, fitness and late-life mortality in relation to chronological and biological age. BMC Geriatr 2002;2:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Masel MC, Graham JE, Reistetter TA, et al. Frailty and health related quality of life in older Mexican Americans. Health Qual Life Outcomes 2009;7:70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carlson JE, Zocchi KA, Bettencourt DM, et al. Measuring frailty in the hospitalized elderly: concept of functional homeostasis. Am J Phys Med Rehabil 1998;77:252–7 [DOI] [PubMed] [Google Scholar]
- 6.Alexander KP, Newby LK, Armstrong PW, et al. Acute coronary care in the elderly, part II: ST-segment-elevation myocardial infarction: a scientific statement for healthcare professionals from the American Heart Association Council on Clinical Cardiology: in collaboration with the Society of Geriatric Cardiology. Circulation 2007;115: 2570–89 [DOI] [PubMed] [Google Scholar]
- 7.Graham MM, Ghali WA, Faris PD, et al. Survival after coronary revascularization in the elderly. Circulation 2002;105:2378–84 [DOI] [PubMed] [Google Scholar]
- 8.Morley JE, Vellas B, van Kan GA, et al. Frailty consensus: a call to action. J Am Med Dir Assoc 2013;14:392–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lacas A, Rockwood K. Frailty in primary care: a review of its conceptualization and implications for practice. BMC Med 2012;10:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sundermann S, Dademasch A, Rastan A, et al. One-year follow-up of patients undergoing elective cardiac surgery assessed with the Comprehensive Assessment of Frailty test and its simplified form. Interact Coardiovasc Thorac Surg 2011;13:119–23 [DOI] [PubMed] [Google Scholar]
- 11.Afilalo J, Mottillo S, Eisenberg MJ, et al. Addition of frailty and disability to cardiac surgery risk scores identifies elderly patients at high risk of mortality or major morbidity. Circulation 2012;5:222–8 [DOI] [PubMed] [Google Scholar]
- 12.Matsuzawa Y, Konishi M, Akiyama E, et al. Association between gait speed as a measure of frailty and risk of cardiovascular events after myocardial infarction. J Am Coll Cardiol 2013;61:1964–72 [DOI] [PubMed] [Google Scholar]
- 13.Conroy S, Dowsing T. The ability of frailty to predict outcomes in older people attending an acute medical unit. Acute Med 2013;12:74–6 [PubMed] [Google Scholar]
- 14.Ekerstad N, Swahn E, Janzon M, et al. Frailty is independently associated with 1-year mortality for elderly patients with non-ST-segment elevation myocardial infarction. Eur J Prev Cardiol Published Online First: 3 May 2013. doi:10.1177/2047487313490257 [DOI] [PubMed] [Google Scholar]
- 15.Moretti C, Fenning S, Parviz Y, et al. Frailty assessment as a prognostic tool in elderly acute coronary syndrome patients to identify those approaching end-of-life: results from prospective multicenter FATE-ACS study. European Heart Journal 2013;34(Suppl 1):3083 [Google Scholar]
- 16.Ma HM, Yu RH, Woo J. Recurrent hospitalisation with pneumonia is associated with higher 1-year mortality in frail older people. Intern Med J 2013;43:1210–15 [DOI] [PubMed] [Google Scholar]
- 17.Ravindrarajah R, Lee DM, Pye SR, et al. The ability of three different models of frailty to predict all-cause mortality: results from the European Male Aging Study (EMAS). Arch Gerontol Geriatr 2013;57:360–8 [DOI] [PubMed] [Google Scholar]
- 18.Hastings SN, Purser JL, Johnson KS, et al. Frailty predicts some but not all adverse outcomes in older adults discharged from the emergency department. J Am Geriatr Soc 2008;56:1651–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Robinson TN, Wu DS, Pointer L, et al. Simple frailty score predicts postoperative complications across surgical specialties. Am J Surg 2013;206:544–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Koller MT, Steyerberg EW, Wolbers M, et al. Validity of the Framingham point scores in the elderly: results from the Rotterdam study. Am Heart J 2007;154:87–93 [DOI] [PubMed] [Google Scholar]
- 21.Rathore SS, Weinfurt KP, Foody JM, et al. Performance of the thrombolysis in myocardial infarction (TIMI) ST-elevation myocardial infarction risk score in a national cohort of elderly patients. Am Heart J 2005;150:402–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chin APMJ, Dekker JM, Feskens EJ, et al. How to select a frail elderly population? A comparison of three working definitions. J Clin Epidemiol 1999;52:1015–21 [DOI] [PubMed] [Google Scholar]
- 23.Newman AB, Gottdiener JS, McBurnie MA, et al. Associations of subclinical cardiovascular disease with frailty. J Gerontol A Biol Sci Med Sci 2001;56:M158–66 [DOI] [PubMed] [Google Scholar]
- 24.Klein BEK, Klein R, Knudtson MD, et al. Frailty, morbidity and survival. Arch Gerontol Geriatr 2004;41:141–9 [DOI] [PubMed] [Google Scholar]
- 25.Woods NF, LaCroix AZ, Gray SL, et al. Frailty: emergence and consequences in women aged 65 and older in the Women's Health Initiative Observational Study. J Am Geriatr Soc 2005;53:1321–30 [DOI] [PubMed] [Google Scholar]
- 26.Sumukadas D, Witham MD, Struthers AD, et al. Effect of perindopril on physical function in elderly people with functional impairment: a randomized controlled trial. CMAJ 2007;177:867–74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McNallan SM, Singh M, Chamberlain AM, et al. Frailty and healthcare utilization among patients with heart failure in the community. JACC Heart Fail 2013;1:135–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Polidoro A, Stefanelli F, Ciacciarelli M, et al. Frailty in patients affected by atrial fibrillation. Arch Gerontol Geriatr 2013;57:325–7 [DOI] [PubMed] [Google Scholar]
- 29.Benjamin EJ, Wolf PA, D'Agostino RB, et al. Impact of atrial fibrillation on the risk of death: the Framingham Heart Study. Circulation 1998;98:946–52 [DOI] [PubMed] [Google Scholar]
- 30.Singh M, Alexander K, Roger VL, et al. Frailty and its potential relevance to cardiovascular care. Mayo Clinic Proc 2008;83:1146–53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lee JS, Auyeung TW, Leung J, et al. Physical frailty in older adults is associated with metabolic and atherosclerotic risk factors and cognitive impairment independent of muscle mass. J Nutr Health Aging 2011;15:857–62 [DOI] [PubMed] [Google Scholar]
- 32.Samper-Ternent R, Al Snih S, Raji MA, et al. Relationship between frailty and cognitive decline in older Mexican Americans. J Am Geriatr Soc 2008;56:1845–52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Avila-Funes JA, Carcaillon L, Helmer C, et al. Is frailty a prodromal stage of vascular dementia? Results from the Three-City Study. J Am Geriatr Soc 2012;60:1708–12 [DOI] [PubMed] [Google Scholar]
- 34.Paulson D, Lichtenberg PA. Vascular depression and frailty: a compound threat to longevity among older-old women. Aging Mental Health 2013;17:901–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lee DH, Buth KJ, Martin BJ, et al. Frail patients are at increased risk for mortality and prolonged institutional care after cardiac surgery. Circulation 2010;121:973–8 [DOI] [PubMed] [Google Scholar]
- 36.Afilalo J, Eisenberg MJ, Morin JF, et al. Gait speed as an incremental predictor of mortality and major morbidity in elderly patients undergoing cardiac surgery. J Am Coll Cardiol 2010;56:1668–76 [DOI] [PubMed] [Google Scholar]
- 37.Green P, Woglom AE, Genereux P, et al. The impact of frailty status on survival after transcatheter aortic valve replacement in older adults with severe aortic stenosis: a single-center experience. JACC Cardiovasc Interv 2012;5:974–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rodes-Cabau J, Webb JG, Cheung A, et al. Long-term outcomes after transcatheter aortic valve implantation: insights on prognostic factors and valve durability from the Canadian multicenter experience. J Am Coll Cardiol 2012;60:1864–75 [DOI] [PubMed] [Google Scholar]
- 39.Schoenenberger AW, Stortecky S, Neumann S, et al. Predictors of functional decline in elderly patients undergoing transcatheter aortic valve implantation (TAVI). Eur Heart J 2013;34:684–92 [DOI] [PubMed] [Google Scholar]
- 40.Zhan C, Baine WB, Sedrakyan A, et al. Cardiac device implantation in the United States from 1997 through 2004: a population-based analysis. J Gen Intern Med 2008;23(Suppl 1):13–19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Flint KM, Matlock DD, Lindenfeld J, et al. Frailty and the selection of patients for destination therapy left ventricular assist device. Circ Heart Fail 2012;5:286–93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gharacholou SM, Roger VL, Lennon RJ, et al. Comparison of frail patients versus nonfrail patients >/=65 years of age undergoing percutaneous coronary intervention. Am J Cardiol 2012;109:1569–75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Singh M, Holmes DR, Lennon RJ, et al. Development and validation of risk adjustment models for long-term mortality and myocardial infarction following percutaneous coronary interventions. Circ Cardiovasc Interv 2010;3:423–30 [DOI] [PubMed] [Google Scholar]
- 44.Graham MM, Norris CM, Galbraith PD, et al. Quality of life after coronary revascularization in the elderly. Eur Heart J 2006;27:1690–8 [DOI] [PubMed] [Google Scholar]
- 45.Singh M, Peterson ED, Roe MT, et al. Trends in the association between age and in-hospital mortality after percutaneous coronary intervention: National Cardiovascular Data Registry Experience. Circ Cardiovasc Interv 2009;2:20–6 [DOI] [PubMed] [Google Scholar]
- 46.Singh M, Rihal CS, Lennon RJ, et al. Influence of frailty and health status on outcomes in patients with coronary disease undergoing percutaneous revascularization. Circ Cardiovasc Qual Outcomes 2011;4:496–502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sundermann S, Dademasch A, Praetorius J, et al. Comprehensive assessment of frailty for elderly high-risk patients undergoing cardiac surgery. Eur J Cardiothorac Surg 2011;39:33–7 [DOI] [PubMed] [Google Scholar]
- 48.Gogbashian A, Sedrakyan A, Treasure T. EuroSCORE: a systematic review of international performance. Eur J Cardiothorac Surg 2004;25:695–700 [DOI] [PubMed] [Google Scholar]
- 49.Iqbal J, Serruys PW, Taggart DP. Optimal revascularization for complex coronary artery disease. Nat Rev Cardiol 2013;10: 635–47 [DOI] [PubMed] [Google Scholar]
- 50.Sinclair APG, Castro M, Bourdel-Marchasson I, et al. European diabetes working party for older people 2011 clinical guidelines for type 2 diabetes mellitus. Executive summary. Diab Metab 2011;37:527–38 [DOI] [PubMed] [Google Scholar]
- 51.Chin APMJ, Dekker JM, Feskens EJ, et al. How to select a frail elderly population? A comparison of three working definitions. J Clin Epidemiol 1999;52:1015–21 [DOI] [PubMed] [Google Scholar]
- 52.Klein BE, Klein R, Knudtson MD, et al. Frailty, morbidity and survival. Arch Gerontol Geriatr 2005;41:141–9 [DOI] [PubMed] [Google Scholar]
- 53.Sundermann S, Dademasch A, Rastan A, et al. One-year follow-up of patients undergoing elective cardiac surgery assessed with the Comprehensive Assessment of Frailty test and its simplified form. Interact Cardiovasc Thorac Surg 2011;13:119–23 [DOI] [PubMed] [Google Scholar]