Abstract
Objective
Analyse 2-year outcomes after MitraClip therapy and identify predictors of outcome.
Methods
Consecutive patients (n=74) undergoing MitraClip therapy were included in the MitraSWISS registry and followed prospectively.
Results
A reduction of mitral regurgitation (MR) to ≤ mild was achieved in 32 (43%) patients and to moderate in 31 (42%) patients; 16/63 (25%) patients with initially successful treatment developed recurrent moderate to severe or severe MR during the first year and only 1 patient did so during the second year. At 2 years, moderate or less MR was more frequently present in patients with a transmitral mean gradient <3 mm Hg at baseline (73% vs 23%, p < 0.01) and in patients with a left atrial volume index (LAVI) <50 mL/m2 at baseline (86% vs 52%, p=0.03). More than mild MR post MitraClip, N-terminal probrain natriuretic peptide ≥5000 ng/L at baseline, chronic obstructive pulmonary disease (COPD) and chronic kidney disease (CKD) were associated with reduced survival.
Conclusions
A mean transmitral gradient <3 mm Hg at baseline, an LAVI <50 mL/m2, the absence of COPD and CKD, and reduction of MR to less than moderate were associated with favourable outcome. Given a suitable anatomy, such patients may be excellent candidates for MitraClip therapy. Between 1 and 2 years follow-up, clinical and echocardiographic outcomes were stable, suggesting favourable, long-term durability of the device.
Keywords: VALVULAR DISEASE, INTERVENTIONAL CARDIOLOGY
Key messages.
Clinical and echocardiographic outcomes between 1 and 2 years were stable, suggesting favourable, long-term durability of the MitraClip procedure.
Patients with a mean transmitral gradient <3 mm Hg, an LAVI <50 mL/m2, without chronic obstructive pulmonary disease and chronic kidney disease had favourable outcomes and may thus be good candidates for the MitraClip procedure.
Since patients with residual moderate (2+) mitral regurgitation had worse outcome compared to patients with none/mild mitral regurgitation, the definition of procedural success may need to be re-evaluated.
Introduction
Mitral regurgitation (MR) is present in about 10% of patients >75 years of age and is the second most frequent valve disease in Europe that requires surgery.1–3 Some of these elderly patients with moderate to severe or severe MR are at high or even prohibitive surgical risk. The MitraClip device (Abbott Vascular, Menlo Park, California, USA) is a less invasive alternative to open heart surgery. The device achieves a reduction of MR by approximating the two mitral valve leaflets. Previous publications have shown that MR can be successfully reduced in the majority of patients up to 1 year after the procedure.4–9 Initially, the Endovascular Valve Edge-to-Edge Repair study (EVEREST) criteria were established and used for patient selection,10 but many registries did include patients who did not strictly apply these criteria. Currently, two of the most important open questions are long-term durability of the procedure and patient selection. To answer these questions, we analysed 2-year outcomes of consecutive patients undergoing MitraClip therapy and aimed to identify predictors of outcome.
Methods
Study population
Between February 2009 and December 2012, a total of 155 patients treated by MitraClip were included in the MitraSWISS registry. A total of 74 patients included between February 2009 and March 2011 who were treated at three Swiss centres (Cantonal Hospital Lucerne, Cardiocentro Ticino and University Hospital Zurich, Switzerland) had reached 2-year follow-up. These patients were analysed in the present study. All patients provided written informed consent.
Patient selection
Prior to the intervention, all patients were discussed by an interdisciplinary heart team. All patients had moderate to severe (3+) or severe (4+) MR on screening echocardiography. Patients were considered for MitraClip therapy if they had a high surgical risk defined by a logistic European System for Cardiac Operative Risk Evaluation (EuroSCORE) mortality >15% and/or additional surgical risk factors such as frailty, porcelain aorta or prior radiotherapy of the chest. The criteria applied in EVEREST were used as a reference but not as absolute inclusion or exclusion criteria.10 In particular, patients with flail leaflets were included even if they had a flail gap >10 mm, as long as the leaflets were approximating at least once during the cardiac cycle. In case of a functional MR, a leaflet coaptation length of <2 mm was not considered an exclusion criterion, as long as the leaflet margins were parallel for a short distance. Exclusion criteria included calcification or thickening of the posterior annulus reducing the visibility of the posterior leaflet. Also, patients with a very lateral regurgitation were excluded due to the risk of interference with the chordae.
Procedure, data collection and definitions
The MitraClip procedure has been described elsewhere previously.11 12 Patients were evaluated at baseline, at discharge and at 1 month, 6 months, 1 year and 2 years post MitraClip. All patients underwent clinical assessment and transthoracic echocardiography at each visit. A subset of patients (n=18) also underwent serial 6 min walk tests. Data were entered into a dedicated, prospective database. Two-year follow-up was complete in 71/74 (96%) patients. Three patients were lost to follow-up. Echocardiography was performed according to the guidelines of the American Society of Echocardiography.13 MR severity was graded as none, mild (1+), moderate (2+), moderate to severe (3+) and severe (4+).10 14 A successful procedure was defined as a reduction of MR to ≤ moderate (2+ or less).12 Left ventricular ejection fraction (LV-EF) and left atrial volume index (LAVI) were calculated using the biplane Simpson's method. Pulmonary pressure was calculated using transthoracic echocardiography. Chronic kidney disease (CKD) was defined as a baseline glomerular filtration rate <60 mL/min.
Statistical analysis
Continuous variables were described using means±SD. Categorical variables were described by frequencies and percentages. Differences between independent groups were tested using the χ2 test for categorical variables or the t test. In cases where the samples were paired, the paired t test was used. Survival rates at 2 years were graphed using the Kaplan-Meier method. A Cox regression model was used to estimate HRs and 95% CIs of baseline characteristics on mortality. Owing to the relatively low number of patients, no multivariable analyses were performed in the present study. Analyses were conducted with IBM SPSS Statistics V.18 (IBM Corporation, Somers, New York, USA) and tested using two-sided tests at a significance level of 0.05.
Results
A total of 74 patients with a mean age of 72±12 years underwent MitraClip therapy for severe (n=48, 65%) and moderate-to-severe (n=26, 35%) MR. The original EVEREST criteria were met by 56 patients (76%). MR was classified as functional in 46 (62%) patients and degenerative in 28 (38%) patients. Compared to degenerative MR, patients with functional MR had a higher logistic EuroSCORE, presented more frequently with coronary artery disease, CKD, atrial fibrillation and had a lower ejection fraction and larger left ventricles. Baseline characteristics are shown in table 1.
Table 1.
Baseline characteristics
| Variable (n=74) | All patients (n=74) | Functional MR (n=46) | Degenerative MR (n=28) | p Value* |
|---|---|---|---|---|
| Age (years) | 72±12 | 71±13 | 73±12 | 0.58 |
| Female sex (%) | 20 (27%) | 12 (26%) | 8 (29%) | 0.82 |
| Logistic EuroSCORE (%) | 21±17 | 28±20 | 15±10 | <0.01 |
| MR severity | ||||
| Severe | 48 (65%) | 26 (57%) | 22 (79%) | 0.05 |
| Moderate-severe | 26 (35%) | 20 (44%) | 6 (21%) | |
| Coronary artery disease (%) | 28 (38%) | 32 (70%) | 6 (21%) | <0.01 |
| COPD (%) | 16 (22%) | 10 (22%) | 6 (21%) | 0.98 |
| Chronic kidney disease (%) | 35 (47%) | 28 (61%) | 7 (25%) | <0.01 |
| Atrial fibrillation (%) | 26 (35%) | 23 (50%) | 3 (11%) | <0.01 |
| LV-EF (%) | 47±19 | 36±15 | 64±10 | <0.01 |
| LV-EDV (mL) | 161±96 | 185±109 | 120±43 | <0.01 |
| Mitral valve annulus (4Ch, mm) | 42±6 | 42±7 | 41±5 | 0.66 |
| Mean transmitral valve gradient (mm Hg) | 2.3±1.3 | 2.2±1.4 | 2.5±1.1 | 0.43 |
| LAVI (mL/m2) | 61±26 | 66±29 | 53±18 | 0.09 |
| PASP (mm Hg) | 48±16 | 48±14 | 47±18 | 0.70 |
| More than mild TR | 16 (22%) | 14 (30%) | 2 (7%) | <0.01 |
*p Values for comparisons between patients with functional and degenerative MR.
4Ch, four chamber view; COPD, chronic obstructive pulmonary disease; EuroSCORE, European System for Cardiac Operative Risk Evaluation; LAVI, left atrial volume index; LV-EDV, left ventricular end-diastolic volume; LV-EF, left ventricular ejection fraction; MR, mitral regurgitation; PASP, pulmonary artery systolic pressure; TR, tricuspid regurgitation.
Procedural and in-hospital data are summarised in table 2. One clip was implanted in 42 (57%) patients, two clips in 27 (39%) patients and three clips in 2 (3%) patients. In three patients (4%), no clip was implanted due to intraprocedural complications. A total of six patients (8%) had bleeding requiring transfusion, and one (1%) patient had a pericardial tamponade after rupture of the left atrium. There were no strokes.
Table 2.
Procedural characteristics
| Variable | All patients (n=74) | Functional MR (n=46) | Degenerative MR (n=28) | p Value* |
|---|---|---|---|---|
| Number of clips implanted | ||||
| 0 | 3 (4%) | 3 (7%) | 0 (0%) | 0.32 |
| 1 | 42 (57%) | 26 (57%) | 16 (57%) | |
| 2 | 27 (37%) | 15 (33%) | 12 (43%) | |
| 3 | 2 (3%) | 2 (4%) | 0 (0%) | |
| MR post procedure† | ||||
| None | 2 (3%) | 2 (4%) | 0 (0%) | 0.34 |
| Mild | 30 (57%) | 18 (39%) | 12 (43%) | |
| Moderate | 31 (42%) | 17 (37%) | 14 (50%) | |
| Moderate-severe | 5 (7%) | 3 (7%) | 2 (7%) | |
| Severe | 5 (7%) | 5 (11%) | 0 (0%) | |
| Transmitral gradient (mm Hg) | 4.0±2.9 | 4.0±3.1 | 4.1±2.7 | 0.89 |
| LV-EF (%) | 47±17 | 36±13 | 62±9 | <0.01 |
| PASP (mm Hg) | 40±13 | 41±13 | 38±13 | 0.37 |
| In-hospital mortality | 3 (4%) | 3 (7%) | 0 (0%) | 0.29 |
*p Values for comparisons between patients with functional and degenerative MR.
†Information not available in one patient who died intraprocedural.
LV-EF, left ventricular ejection fraction; MR, mitral regurgitation; PASP, pulmonary artery systolic pressure.
The procedural success rate was 63/74 (85%) patients with an immediate reduction of MR to none or mild in 32 (43%) patients and moderate in 31 (42%) patients. The procedural success rate did not differ between patients who met the EVEREST criteria (47/56, 84%) and those who did not (16/18, 89%, p=0.61).
Table 3 lists the management and outcomes of unsuccessful procedures. The mean transmitral gradient increased from 2.0±1.1 mm Hg at baseline to 4.0±3.1 mm Hg before discharge (p<0.01). Overall in-hospital mortality was 4.1% (3/74). In-hospital mortality was 0% (0/63) in patients with procedural success and 27% (3/11) in those without procedural success (p<0.01).
Table 3.
Management and outcome of patients with unsuccessful procedures (n=11)
| Event | Management | Outcome |
|---|---|---|
| Chordal rupture (no clip implanted) | Surgical MVR | Death 5 days post procedure |
| Papillary muscle rupture (no clip implanted) | Medical treatment | Intraprocedural death |
| Reduction of MR to 3+ | Medical treatment | Death 44 days post procedure |
| Reduction of MR to 3+ | Medical treatment | Patient alive at 2 years |
| No relevant reduction of MR with 1 clip; impossible to implant more clips | Medical treatment | Death 57 days post procedure |
| Clip only attached on 1 leaflet; not possible to grasp both leaflets | Medical treatment | Death 106 days post procedure |
| Reduction to 3+ MR | Medical treatment | Death 103 days post procedure |
| Reduction to 3+ MR | Re-do procedure | Patient alive at 2 years |
| No reduction of MR | Medical treatment | Patient alive at 2 years |
| Not possible to grasp both leaflets (no clip implanted) | Surgical MVR | Patient alive at 2 years |
| Reduction to 3+ MR | Medical treatment | Patient alive at 2 years |
MR, mitral regurgitation; MVR, mitral valve replacement.
MR severity
MR was reduced to ≤ moderate in 63 (85%) patients (37 (80%) patients with functional MR and 26 (93%) with degenerative MR). Of these, 17 patients (27%) developed recurrent moderate to severe (3+) or severe (4+) MR during the first year post MitraClip. Only one additional patient developed recurrent 3+ or 4+ MR during the second year (table 4). At 2-year follow-up, MR was ≤ moderate in 41 (58%) patients, more than moderate in 12 (17%) patients and 18 (25%) of the patients had died (figure 1). There was no significant difference between patients with functional and degenerative MR. At 2 years, ≤ moderate MR was more frequently present in patients with a transmitral mean gradient <3 mm Hg at baseline (35/48, 74%) than in those with a gradient ≥3 mm Hg (5/22, 23%, p<0.01) and in patients with an LAVI <50 mL/m2 at baseline (12/14, 86%) than in those with an LAVI ≥50 mL/m2 (23/44, 52%, p=0.03). An LAVI ≥50 mL/m2 was more frequently present in patients with CKD, atrial fibrillation, a higher logistic EuroSCORE and a higher pulmonary artery pressure. A mean transmitral gradient ≥3 mm Hg was more frequently found in patients with a smaller annulus diameter.
Table 4.
Clinical outcomes 1 and 2 years post MitraClip
| Variable | 1-year outcome | 2-year outcome |
|---|---|---|
| ≤ Moderate MR | 41 (58%) | 41 (58%) |
| Mortality | 14 (19%) | 18 (25%) |
| Partial clip detachment | 6 (8%) | 7 (10%) |
| Re-do MitraClip procedure | 1 (1%) | 7 (10%) |
| Mitral valve surgery | 4 (5%) | 4 (5%) |
| NYHA class I or IV | 13 (18%) | 15 (20%) |
MR, mitral regurgitation; NYHA, New York Heart Association.
Figure 1.

Severity of MR at BL, and at 1 month, 6 months, 1 year and 2 years post MitraClip. At 2-year follow-up, MR was ≤ moderate in 58%, more than moderate in 17% and 25% of the patients had died. BL, baseline; MR, mitral regurgitation.
Survival
Survival rates were 96%, 81% and 75% at 30 days, 1 year and 2 years, respectively. Cause of death was heart failure in 10 patients, exacerbated chronic obstructive pulmonary disease (COPD) in two patients, sepsis in two patients and unknown in four patients. A total of 15 patients had an LV-EF <30% at baseline. Survival rate at 2 years was 72% in patients with functional MR and 82% in those with degenerative MR (p=0.31). Survival rate at 2 years was 73% in those with an LV-EF <30% at baseline (n=15) and 76% in those with an LV-EF ≥30% (n=59, p=0.81). Significant predictors of reduced survival were residual MR severity post MitraClip (figure 2), N-terminal probrain natriuretic peptide (NT-proBNP) ≥5000 ng/L at baseline, the presence of COPD and the presence of CKD (table 5).
Figure 2.
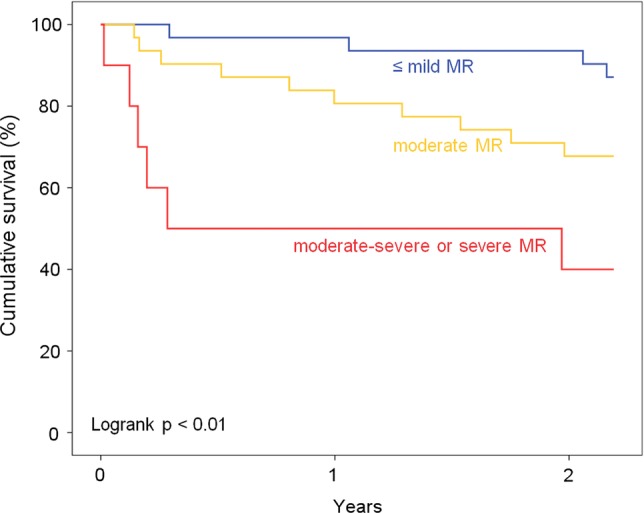
Survival according to residual MR post MitraClip. Residual more than mild MR post MitraClip was associated with reduced survival, suggesting that MR should be reduced as much as possible. MR, mitral regurgitation.
Table 5.
Univariate predictors of survival
| Variable | HR (95% CI) | p Value |
|---|---|---|
| Residual MR severity | 2.54 (1.45 to 4.46) | <0.01 |
| NT-proBNP ≥5000 ng/L | 6.18 (1.84 to 20.79) | <0.01 |
| COPD | 2.36 (1.04 to 5.36) | 0.04 |
| Chronic kidney disease | 3.29 (1.37 to 7.92) | <0.01 |
COPD, chronic obstructive pulmonary disease; MR, mitral regurgitation; NT-proBNP, N-terminal probrain natriuretic peptide.
Partial clip detachment
At 2 years, partial clip detachment had occurred in seven (10%) patients. Most of these events occurred within the first 30 days (n=4), or between 30 days and 1 year (n=2). There was one patient with a partial clip detachment 2 years post procedure. In 5/7 (71%) patients, partial clip detachment resulted in 3+ or 4+ MR. A re-do MitraClip procedure was performed in five patients, whereas the remaining two were treated medically. The re-do procedure reduced MR to ≤ moderate in 2/5 (40%) patients. The remaining three patients had persistent moderate to severe or severe MR. No differences were noted between patients with functional or degenerative mitral valve disease in terms of survival, partial clip detachment and need for surgical repair.
Functional and echocardiographic outcome
At 2 years, 37 patients (53%) were in the New York Heart Association (NYHA) class I or II, 13 (19%) in class III and 2 (3%) in class IV (figure 3). Six minutes walking distance improved from 425±104 m at baseline to 523±108 m at 2-year follow-up (p<0.01). Pulmonary artery pressure decreased from 48±16 mm Hg at baseline to 35±11 mm Hg at 2-year follow-up (p<0.01). Left ventricular end-diastolic volume was 161±96 mL at baseline and 137±61 mL at 2-year follow-up (p=0.18). LV-EF remained unchanged. LAVI was 61±26 mL/m2 at baseline and 55±21 mL/m2 at 2-year follow-up (p=0.54).
Figure 3.
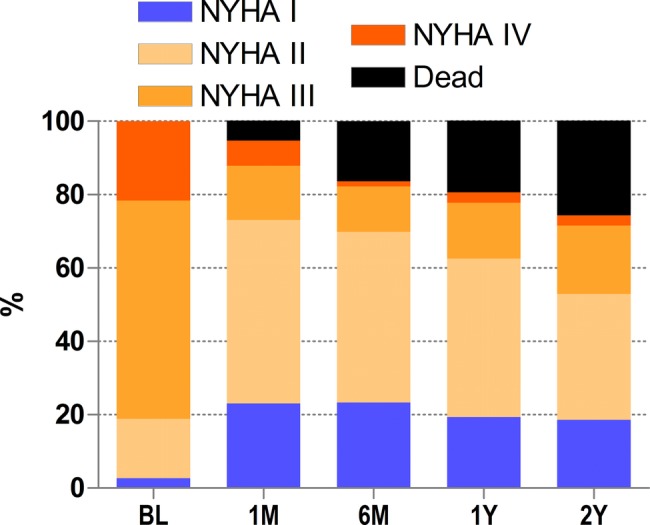
NYHA class over the 2-year study period. At 2 years, 53% of patients were in NYHA class I or II, 19% were in class III and 3% in class IV. BL, baseline; NYHA, New York Heart Association.
Discussion
Long-term clinical follow-up data are essential to judge the value of percutaneous mitral valve repair with the MitraClip. This study reports 2-year outcomes of the first 74 consecutive patients undergoing MitraClip therapy at three centres in Switzerland. The procedure successfully reduced MR to ≤ moderate in 63/74 (85%) patients. Of those patients with procedural success, 16/63 (25%) developed recurrent moderate to severe or severe MR during the first year post MitraClip. Only one additional patient developed moderate to severe or severe MR during the second year, suggesting that MR grade remained relatively stable beyond 1-year post procedure. As a consequence, the proportion of patients with ≤ moderate MR was 58% after both 1 and 2 years (43/74). No clip embolised during the 2-year period, but at 2 years, partial clip detachment had occurred in seven patients, in six patients during the first year and only in one patient during the second year. Nevertheless, the majority of re-do procedures were performed during the second year. Most of these patients were clinically compensated and a trial with medical therapy was usually performed. Treatment of MR with the MitraClip device resulted in less symptoms and an increase in 6 min walking distance, a decrease in pulmonary pressure, left ventricular end-diastolic volume and LAVI. LV-EF remained unchanged.
Mortality was low between 1 and 2 years (4/74 patients). However, overall 2-year morality was relatively high (25%) due to inclusion of elderly patients with comorbidities and/or low LV-EF. For comparison, the estimated 2-year mortality rate of people with similar age in Switzerland is about 7%.15
Predictors of clinical efficacy and survival
Currently, one of the remaining open questions is which patients should be selected for MitraClip therapy. Initially, the EVEREST criteria were used to select patients.10 We believe that the EVEREST inclusion criteria describe a population with a high likelihood of procedural success. However, carefully selected patients not fulfilling the EVEREST criteria may be treated equally successfully. In the present study, 18 (24%) patients did not meet the EVEREST criteria, but the procedural success rate was not lower in these patients. We identified a transmitral mean gradient <3 mm Hg at baseline and an LAVI <50 mL/m2 at baseline to be associated with a persistent clinical success (ie, persistent reduction of MR to ≤ moderate). This may be important when performing echocardiographies to screen patients for the MitraClip procedure. Residual MR post MitraClip, NT-proBNP ≥5000 ng/L at baseline, the presence of COPD and CKD affected survival and long-term outcome. Based on our results, MR should be reduced as much as possible, since residual moderate MR (which is still considered a procedural success) was associated with reduced survival compared to residual none/mild MR. The prognostic value of natriuretic peptides has been established in many different scenarios.16 17 Comorbidities, in particular COPD and CKD, have been found to be associated with worse prognosis in patients undergoing transcatheter aortic valve implantation.18
A low LV-EF <30% is considered as a high risk for mitral valve reconstruction since the acute rise in afterload may result in left ventricular deterioration. Interestingly, a low LV-EF did not affect outcome in the present study. Survival rate did not differ between patients with an LV-EF <30% and patients with an LV-EF ≥30% at baseline, although the number of patients with an LV-EF <30% was low (n=15, 20% of patients). In future, a score predicting the clinical success of mitral clipping may be developed, similar to the Wilkins Score predicting outcome after percutaneous balloon dilation of the mitral valve.
Comparison to previous studies
To the best of our knowledge, this is the first real-world study with a 2-year follow-up completed in 96% of patients. Two previous studies have reported outcomes after MitraClip beyond 12 months. The EVEREST II randomised trial which compared treatment with the MitraClip to surgery recently published results up to 4 years.19 In accordance with the results of the present study, they found that the majority of recurrent moderate to severe or severe MR occurred during the first year of follow-up. In line with our study results, only few patients developed recurrent MR between years 1 and 4. However, in the EVEREST trials, precise echocardiographic criteria had to be met, thus excluding many patients who might have potentially benefited from the MitraClip procedure. In addition, placement of more than one clip has been increasingly used after the publication of the EVEREST trial. This may explain the higher rate of procedural success in the present study (85% vs 77% in the EVEREST II trial).
Rudolph et al20 reported outcomes of a single-centre registry. Patients were followed for a median of 13.3 months. They found that in patients with degenerative (primary) MR, Logistic EuroSCORE, a lower forward stroke volume, left ventricular dysfunction in patients with coronary artery disease and renal failure were associated with reduced survival.
The ACCESS-EU study included a total of 567 patients, of whom 393 (69%) had functional MR.5 Procedural success was obtained in 91% of patients. Similar to this study, baseline characteristics differed between patients with functional and degenerative MR, but outcome at 30 days and 12 months was comparable.
Previous studies have identified an increase in cardiac index and a decrease in pulmonary artery and wedge pressures as predictors of favourable short-term outcomes.21 22 Two recent publications identified acute procedural success and residual discharge MR severity as predictors of 1-year survival post MitraClip therapy.23 24 However, these variables are all unknown at baseline and can therefore not serve for patient selection.
Study limitations
These patients represent the early experience of the three centres, and the level of experience (individual and overall) has increased since then. With better patient selection and higher experience, better results can be anticipated in future. Owing to the relatively low number of patients, no multivariable analyses were performed in the present study.
Clinical implications and conclusion
Clinical and echocardiographic outcomes were stable beyond 1 year, suggesting favourable long-term durability of percutaneous mitral valve reconstruction. Baseline predictors of favourable outcome were a mean transmitral gradient <3 mm Hg, an LAVI <50 mL/m2, the absence of COPD and the absence of CKD. These findings may have important implications for patient selection. In addition, patients with moderate MR post procedure had a worse outcome compared to patients with none/mild MR. In the light of these results, the definition of procedural success may need to be re-evaluated. In future, improved patient selection, experience and maybe concomitant utilisation with non-surgical mitral annuloplasty devices may lead to even better outcomes and a wider application of the MitraClip procedure.
Footnotes
Contributors: All authors intellectually contributed to the mansucript either in manuscript preparation, intellectual input, data analysis, and/or final approval.
Funding: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: OG, RC and TFL received an institutional grant and/or lecture fees from Abbott Vascular.
Ethics approval: Local Ethics Committees.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Vahanian A, Alfieri O, Andreotti F, et al. Guidelines on the management of valvular heart disease (version 2012). Eur Heart J 2012;33:2451–96 [DOI] [PubMed] [Google Scholar]
- 2.Nkomo VT, Gardin JM, Skelton TN, et al. Burden of valvular heart diseases: a population-based study. Lancet 2006;368:1005–11 [DOI] [PubMed] [Google Scholar]
- 3.Iung B, Baron G, Butchart EG, et al. A prospective survey of patients with valvular heart disease in Europe: The Euro Heart Survey on Valvular Heart Disease. Eur Heart J 2003;24:1231–43 [DOI] [PubMed] [Google Scholar]
- 4.Reichenspurner H, Schillinger W, Baldus S, et al. Clinical outcomes through 12 months in patients with degenerative mitral regurgitation treated with the MitraClip(R) device in the ACCESS-EUrope Phase I trial. Eur J Cardiothorac Surg 2013;44:e280–8 [DOI] [PubMed] [Google Scholar]
- 5.Maisano F, Franzen O, Baldus S, et al. Percutaneous mitral valve interventions in the real world: early and one year results from the ACCESS-EU, a prospective, multicenter, non-randomized post-approval study of the MitraClip(R) therapy in Europe. J Am Coll Cardiol 2013;62:1052–61 [DOI] [PubMed] [Google Scholar]
- 6.Grasso C, Capodanno D, Scandura S, et al. One- and twelve-month safety and efficacy outcomes of patients undergoing edge-to-edge percutaneous mitral valve pepair (from the GRASP registry). Am J Cardiol 2013;111:1482–7 [DOI] [PubMed] [Google Scholar]
- 7.Whitlow PL, Feldman T, Pedersen WR, et al. Acute and 12-month results with catheter-based mitral valve leaflet repair: the EVEREST II (Endovascular Valve Edge-to-Edge Repair) high risk study. J Am Coll Cardiol 2012;59:130–9 [DOI] [PubMed] [Google Scholar]
- 8.Baldus S, Schillinger W, Franzen O, et al. MitraClip therapy in daily clinical practice: initial results from the German transcatheter mitral valve interventions (TRAMI) registry. Eur J Heart Fail 2012;14:1050–5 [DOI] [PubMed] [Google Scholar]
- 9.Rudolph V, Knap M, Franzen O, et al. Echocardiographic and clinical outcomes of MitraClip therapy in patients not amenable to surgery. J Am Coll Cardiol 2011;58:2190–5 [DOI] [PubMed] [Google Scholar]
- 10.Feldman T, Kar S, Rinaldi M, et al. Percutaneous mitral repair with the MitraClip system: safety and midterm durability in the initial EVEREST (Endovascular Valve Edge-to-Edge REpair Study) cohort. J Am Coll Cardiol 2009;54:686–94 [DOI] [PubMed] [Google Scholar]
- 11.Pedrazzini GB, Faletra F, Vassalli G, et al. Mitral regurgitation. Swiss Med Wkly 2010;140:36–43 [DOI] [PubMed] [Google Scholar]
- 12.Feldman T, Foster E, Glower DG, et al. Percutaneous repair or surgery for mitral regurgitation. N Engl J Med 2011;364:1395–406 [DOI] [PubMed] [Google Scholar]
- 13.Gardin JM, Adams DB, Douglas PS, et al. Recommendations for a standardized report for adult transthoracic echocardiography: a report from the American Society of Echocardiography's Nomenclature and Standards Committee and Task Force for a Standardized Echocardiography Report. J Am Soc Echocardiogr 2002;15:275–90 [DOI] [PubMed] [Google Scholar]
- 14.Zoghbi WA, Enriquez-Sarano M, Foster E, et al. Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography. J Am Soc Echocardiogr 2003;16:777–802 [DOI] [PubMed] [Google Scholar]
- 15.Swiss Federal Administration. http://www.bfs.admin.ch/bfs/portal/de/index/themen/01/02/blank/key/alter/gesamt.Document.20563.xls (accessed 25 Sep 2013)
- 16.Jaberg L, Toggweiler S, Puck M, et al. Prognostic value of N-terminal pro-B-type natriuretic peptide in patients with acute coronary syndromes undergoing left main percutaneous coronary intervention. Circ J 2011;75:2648–53 [DOI] [PubMed] [Google Scholar]
- 17.Lopez-Otero D, Trillo-Nouche R, Gude F, et al. Pro B-type natriuretic peptide plasma value: a new criterion for the prediction of short- and long-term outcomes after transcatheter aortic valve implantation. Int J Cardiol 2012;168:1264–8 [DOI] [PubMed] [Google Scholar]
- 18.Toggweiler S, Humphries KH, Lee M, et al. 5-year outcome after transcatheter aortic valve implantation. J Am Coll Cardiol 2013;61:413–19 [DOI] [PubMed] [Google Scholar]
- 19.Mauri L, Foster E, Glower DD, et al. Four-year results of a randomized controlled trial of percutaneous repair versus surgery for mitral regurgitation. J Am Coll Cardiol 2013;62:317–28 [DOI] [PubMed] [Google Scholar]
- 20.Rudolph V, Lubos E, Schluter M, et al. Aetiology of mitral regurgitation differentially affects 2-year adverse outcomes after MitraClip therapy in high-risk patients. Eur J Heart Fail 2013;15:796–807 [DOI] [PubMed] [Google Scholar]
- 21.Gaemperli O, Moccetti M, Surder D, et al. Acute haemodynamic changes after percutaneous mitral valve repair: relation to mid-term outcomes. Heart 2012;98:126–32 [DOI] [PubMed] [Google Scholar]
- 22.Siegel RJ, Biner S, Rafique AM, et al. The acute hemodynamic effects of MitraClip therapy. J Am Coll Cardiol 2011;57:1658–65 [DOI] [PubMed] [Google Scholar]
- 23.Paranskaya L, D'Ancona G, Bozdag-Turan I, et al. Residual mitral valve regurgitation after percutaneous mitral valve repair with the MitraClip(R) system is a risk factor for adverse one-year outcome. Catheter Cardiovasc Interv 2013;81:609–17 [DOI] [PubMed] [Google Scholar]
- 24.Surder D, Pedrazzini G, Gaemperli O, et al. Predictors for efficacy of percutaneous mitral valve repair using the MitraClip system: the results of the MitraSwiss registry. Heart 2013;99:1034–40 [DOI] [PubMed] [Google Scholar]


