Abstract
High blood pressure (HBP) or hypertension (HTN) is one of the leading causes of cardiovascular (CV) morbidity and mortality throughout the world. Despite this fact, there is widespread agreement that the treatment of HBP, over the last half century, has been a great achievement. However, after the release of the new Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure-8 (JNC-8) guidelines, there have been heated debates with regard to what are the most evidence-based blood pressure goals. While JNC-8 claims that the goal blood pressure for otherwise healthy patients with mild hypertension (systolic blood pressure ≥140–159 mm Hg and diastolic blood pressure ≥90–99 mm Hg) should be <140/90 mm Hg; a recent Cochrane meta-analysis is in direct conflict with these recommendations. Indeed, a 2012 Cochrane meta-analysis indicated that there is no evidence that treating otherwise healthy mild hypertension patients with antihypertensive therapy will reduce CV events or mortality. Additionally, the Cochrane meta-analysis showed that antihypertensive therapy was associated with a significant increase in withdrawal due to adverse events. Thus, the current evidence in the literature does not support the goals set by the JNC-8 guidelines. In this review we discussed the strengths and limitations of both lines of evidence and why it takes an evidence-based medication to reduce CV events/mortality (eg, how a goal blood pressure is achieved is more important than getting to the goal). As medications inherently cause side effects and come at a cost to the patient, the practice of evidence-based medicine becomes exceedingly important. Although the majority of HTN studies claim great advantages by lowering HBP, this review finds severe conflicts in the findings among the various HTN studies, as well as serious epistemological, methodological and statistical problems that cast doubt to such claims.
Keywords: Myocardial Infarction
Key messages.
There are significant conflicts in the conclusions of hypertension studies that cannot be explained statistically as these studies are based on large sample sizes. The reasons for the conflicts are due to the methodological, epistemological and statistical deficiencies of the hypertension studies. These reasons must be accepted and remedied in order to improve the scientific standing of medicine.
It is uncertain if treating otherwise healthy mild hypertensive patients with antihypertensive therapy will reduce morbidity and mortality.
The current evidence in the literature does not support the blood pressure goals set by the JNC-8 guidelines.
Introduction
High blood pressure (HBP), or hypertension (HTN), is a common medical condition, estimated to occur in about one in three young adults, increasing to about 60% for those over 60 and affects more than three of four people older than 70.1 A new study in The Lancet2 asserts that in 2010 HBP was the leading risk factor for global disease burden. Furthermore, the US government's Centers for Disease Control and Prevention (CDC)3 lists the yearly age-adjusted deaths attributed to HTN and hypertensive heart disease at 17.3/100 000 (about the same as diabetes mellitus). In medical journals there are great numbers of published studies about HTN with a widespread agreement among them that “the treatment of hypertension has been one of medicine's major successes of the past half-century. The remarkable advances in therapy have provided the newfound capability for lowering blood pressure (BP) in almost every person with hypertension.”4 The medical studies agree that there is room for saving additional lives as a significant proportion of hypertensives are not aware of their condition. This is often because there are no symptoms caused by HBP to warn of its existence. Indeed HTN is often referred to as the ‘silent killer’ in the medical literature.5 Is the treatment of HTN one of medicine's major successes? Or is it part of the well-known and convincingly demonstrated problems6–8 of medical research?
The conflicting findings in studies between hypertensives and normotensives
There are a great number of medical studies comparing the life expectancy and cardiovascular (CV) and related diseases between normotensives and hypertensives. This section reviews some of these studies and challenges meta-analyses concluding that9: “throughout middle and old age, usual blood pressure is strongly and directly related to vascular (and overall) mortality, without any evidence of a threshold down to at least 115/75 mm Hg.”
More than 5-year loss in life expectancy
A major, often-cited study10 published by Franco and co-authors, based on the widely used Framingham data, concluded “Compared with hypertensives, total life expectancy was 5.1 and 4.9 years longer for normotensive men and women respectively.”
The Whitehall study11 based on examining 18 863 men employed in the Civil Service in London, England, concluded that the difference in life expectancy between men with the lowest systolic BP (SBP) and those with the highest was 5.2 years (see table 3, p.6 of this study), in other words a result very similar to that reported by Franco et al using the Framingham data.
Five years loss of life expectancy due to HTN seems extremely large if the total gain for all preventive and curative measures is 5 years according to the seminal paper by Bunker, Frazier and Mostellar12 and between less than 1 month to slightly more than 1 year to people at average risk according to Wright and Weinstein.13 Moreover, the 5-year loss is an average for all hypertensives. This means that it would be more than twice that for people at high risk like heavy smokers, those with high cholesterol, those engaging in no exercise, the obese and individuals with an SBP of 190 or more. Such an estimate is too high even for people at especially high risk. Finally, estimates of huge losses in life expectancy due to HBP cannot be supported at the population level. If the loss in life expectancy in the USA, with 23.5% hypertensives, is on average 5 years, what would the loss in life expectancy be in Japan where the average prevalence is 50.1%14? This would seemingly indicate that patients in Japan would die younger than those in the USA due to such high prevalence of HTN, however, the life expectancy in Japan (the highest in the world) is 4.8 years more than that of the USA. The same conclusion would apply to several European countries and Canada with a much higher prevalence of HTN than the USA but longer life expectancy.
Minor losses in life expectancy
One of the new studies by Ford15 based on the US National Health and Nutrition Examination Survey (NHANES) I and NHANES III data, which included close to 23 000 participants, arrived at the conclusion that, among all hypertensive participants, the age-adjusted mortality rate was 18.8/1000 person-years for NHANES I and 14.3 for NHANES III, while the corresponding rates for non-hypertensive people were 13.3 and 9.1/1000 person-years, respectively.
Thus, there were 5.5 more deaths (18.8–13.3)/1000 person-years for NHANES I and 5.2 (14.3–9.1)/1000 person-years for NHANES III, or 0.55% and 0.52% (two extremely consistent rates) more deaths, respectively, between hypertensive and non-hypertensive participants. These percentages indicate that for every 182 deaths of non-hypertensive people there will be 183 deaths in hypertensives in NHANES I and 192 and 191, respectively, in NHANES III. These results, as well as those referring to CV diseases (CVD), are considerably lower than in the Franco et al and Whitehall studies. In addition, Ford, concludes when discussing the clinical perspective of his study:
The current study's results show that the age-adjusted mortality rate from all causes decreased by 4.6 per 1000 person-years in 2 national cohorts of hypertensive adults who were recruited from 1971 to 1975 and from 1988 to 1994. However, this decrease was comparable to the decrease of 4.2 per 1000 person-years among nonhypertensive adults.
In other words, there was a decrease in mortality rates between 1971 to 1975 and 1988 to 1994 among hypertensives that was bigger than among normotensives. Although the difference in the rates of decrease was small, only 0.4/1000 person-years, it is statistically significant because of the large number of participants included in the studies.
The conclusions of Port et al16 concerning the Framingham data disagreed about the effects of HBP on CV deaths. They assert
Contrary to widely cited interpretations, reanalysis of the Framingham 18-year data showed that the relation between systolic blood pressure and all-cause and cardiovascular mortality is not strictly increasing. The linear logistic model used to generate that relation was rejected by the Framingham data. Instead, risk is unrelated to systolic pressure to at least the 70th percentile for each age and sex, and sharply increases with blood pressure higher than the 80th percentile.
Figure 1, taken from Port and coauthors, shows that overall deaths related to HBP hardly increase until an SBP of around 175 is reached. But even if SBP increases to about 185, the number of deaths rises from around 15 to 28, an increase of 13/1000 or 1.3%. Only when SBP exceeds the 185 mark does the number of deaths start to increase steeply. In this case, the difference between normal SBP and that over 190 is 27 (15–42) extra deaths/1000, or 2.7%.
Figure 1.
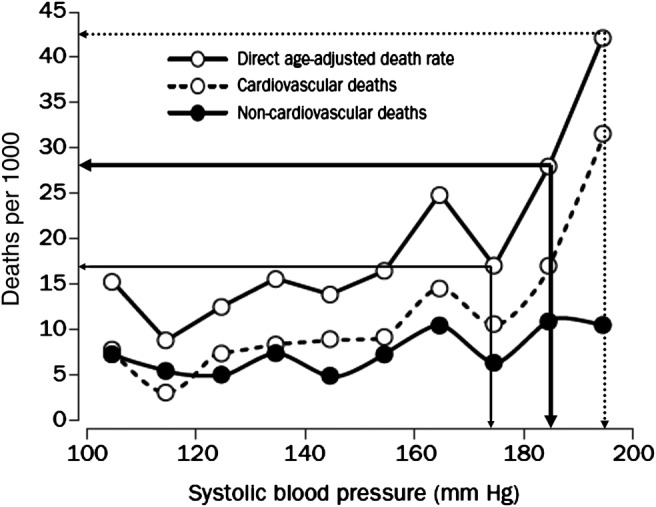
Actual age-adjusted rates for men aged 45–74 years related to systolic blood pressure (based on age-specific rates in Framingham study). The direct age-adjusted rate is the sum of the lower two curves (taken from Ref.16 while the horizontal and vertical straight lines have been added by the author).
Other studies, although most agree that HBP increases the risk of CVD and related diseases and reduces life expectancy, arrived at widely diverging estimates that are in between those already mentioned.
Major epistemological concern: HTN studies do not prove causality
The great majority of HTN studies compare the differences in total and CV mortality between hypertensives and normotensives by demonstrating statistically significant differences or by demonstrating important correlations between the two groups. But such differences and correlations cannot prove causality. HTN may be caused by stress, in which case major coronary heart disease (CHD) could be the result of such stress rather than HBP. Many studies have shown significant differences in HBP among people in various regions (in rural India for instance the age-adjusted HTN rate is 5.5% while in urban areas it is 30.7%17), countries,2 races18 and of course ages. This means that many factors can be responsible for HBP. Proving causality (ie, that HBP causes extra deaths) is, therefore, practically impossible as a number of confounding factors can be responsible for these deaths. In addition to stress, cultural traits, lifestyle factors, marital status, personality characteristics, dietary habits, genetic factors or some other, unknown reason may cause HBP. Alternatively, it may be that with age some organ or body part malfunctions and that HBP is required to minimise the negative consequences of such malfunction, the same way that fever helps fight disease. Indeed, patients with CHD may have greater HBP to properly perfuse vital organs and a drop in BP could even precipitate myocardial ischaemia and a subsequent CHD event.19 Although, it is common to attribute causality based on high correlations and/or strong relationship, it is absolutely clear from statistical theory and hard sciences that doing so encompasses great dangers and must be avoided. Finally, finding out that HBP, or type 2 diabetes mellitus (T2DM) increases death rates may improve our knowledge but holds no practical value. What patients with hypertension or T2DM need to know is if they will benefit from treatment of their disease and if the benefits for doing so would outweigh the cost (monetary and negative side effects) involved.
Comparing treated and non-treated hypertensives
The correct epistemological question is: How much is total and CV mortality decreased if HTN is treated? The number of studies attempting to answer this question are considerably fewer than those comparing normotensives and hypertensives, most of them refer to older people20–23 and they compare the effectiveness of various types of drugs to treat HTN.24–27 Overall, the findings of these studies are even more conflicting than the studies comparing normotensives to hypertensives. Their conclusions range from considerable increases in mortality rates and CV and related disease to significant benefits if HTN is not treated.
A meta-analysis26 on the effects of treatment concluded that “treatment with any commonly-used regimen reduces the risk of total major CV events, and larger reductions in blood pressure produce larger reductions in risk.” A study by Gu et al,28 based on 5086 hypertensive participants with a higher than 140/90 BP, concluded that “uncontrolled and untreated hypertension was associated with increased risk of total and CV mortality among the general hypertensive population.” Another study by Barengo et al29 found that in men, all-cause and CVD mortality was significantly higher in the hypertensive subgroups compared with the normotensive group but in treated and controlled hypertensive women at baseline there was no increase in CVD or all-cause mortality. One more study by Dahlöf et al30 on people between 70 and 84 years old, found highly significant and clinically relevant reductions in CV morbidity and mortality among patients who treated their HBP.
A study by Gudmundsson et al31 based on 19 390 participants (9328 men and 10 062 women) aged 33–37 years at the time of attendance from 1967 to 1996 concluded that there were no significant benefits by treating HTN with drugs. Another study24 investigating the association between CV outcomes and antihypertensive drug treatment for around 30 000 older women found that those receiving no medications compared to those receiving diuretics as monotherapy had a smaller (not statistically significant) risk for CHD, stroke and CVD death. However, the crude CV death rate of hypertensives taking no medication was the lowest (0.011%) compared to those receiving one or two drugs (0.035%) occurring among those taking diuretics and calcium channel blockers. These results occurred even though the baseline SBP of the no medications group was higher (149 mm Hg) than for those receiving drug treatment; the SBPs of the women who were receiving therapy before they began the therapy was unknown.
A newer study by Almgren et al32 that compared treated hypertensives and normotensives concluded
In spite of a substantial reduction of their blood pressure, treated hypertensive middle-aged men had a highly increased risk of stroke, MI and mortality from coronary heart disease compared with nonhypertensive men of similar age. The increased risk of cardiovascular complications escalated during the latter course of the study.
A meta-analysis by the Cochrane foundation identified (going all the way back to 1953) only 11 published randomised control trials comparing the effects of treatment33 of those who were mildly hypertensive (those with BP between 140–160 and 90–100). From these 11 studies, 4 passed the criteria and were included in the meta-analysis. Consequently, after the treatment of 7080 participants for 4–5 years with antihypertensive drugs as compared to placebo, it was concluded that treatment did not reduce CHD, stroke or total CV events. In addition, it found that withdrawals due to adverse effects by drug therapy reached 9%. Finally, a study investigating the long-term effects of a randomised, placebo-controlled, clinical trial (Systolic Hypertension in the Elderly Program, SHEP)21 of patients aged 60 years or older with isolated systolic hypertension, with SBP of more than 160 mm Hg, found moderate gains of 105 days for all-cause mortality and 158 days for CV death. In addition, the active treatment group had higher survival free from CV death versus the placebo group but similar survival for all-cause mortality.
Treated, uncontrolled hypertensives: methodological issues
There is a big paradox4 associated with the treatment of HTN. Although the number of people treated for HTN increases over time, so does its prevalence, and worse, the number of treated hypertensives with ‘uncontrolled BP’ (defined as treated hypertensives whose BP is greater than the 140/90 therapeutic goal). For instance, in the Gu et al28 study mentioned above, 62% of treated hypertensives did not achieve the therapeutic goal of lowering their BP below 140/90. The percentages of treated, ‘uncontrolled’ hypertensives reported in the paper by Chobanian4 ranged from 10% to 35%, while that cited by Jeffrey and co-authors34 was between 26% and 35%. However, a study by Lindholm35 concludes that “Population surveys indicate that the proportion of patients achieving even conservative blood pressure targets may be only 20% or lower.” Other studies36–38 mention treatment-resistant HTN (when BP cannot be lowered to below the 140/90 level, even after the patients have taken more than three hypertensive-lowering drugs) that could affect 20–30% of hypertensives, masked and even malignant HTN.39 The high percentages of uncontrolled HTN are disturbing and are probably the major cause of dropout rates from treatment that approach 10% of all patients.
There are three major methodological issues when categorising people with HBP:
First, can uncontrolled hypertensives receiving treatment be classified in the category of ‘hypertensives’? Definitionally speaking they are hypertensives since their BP is greater than the 140/90 limit. Methodologically, however, there is a major flaw for doing so as the reason for the inability to lower HTN with medical drugs may be caused by pathologies that increase the chances of death or CV-related diseases.36
Second, can treated, uncontrolled hypertensives be classified in the category of normotensives, even though they are technically hypertensives? Methodologically this cannot also be correct. Until now, some studies, like that of Franco et al10 included as hypertensives all those with a BP greater than 140/90, with no regard to whether they were treated or not. Other studies, as that by Ford,14 included as ‘non-hypertensives’ all treated persons whether or not their BP was lower than the 140/90 mm Hg level. This definitional difference of who is included as hypertensive/non-hypertensive may explain part or all of the huge difference in the conclusions of these two studies as the number of treated, uncontrolled hypertensives was particularly high at the time the Framingham data was collected.
Third, how should people who have dropped out of treatment, after receiving BP-lowering medication for a period of time, be dealt with? These people constitute a special category as they may suffer from treatment-resistant HTN that encouraged them to quit treatment. In addition, their body may have lost all, or part of its ability to control BP on its own after getting used to the BP-lowering medication.
It is simpler, of course, to design and implement studies classifying people as ‘normotensives’ and ‘hypertensives’ but this is not methodologically correct. The classification must have at least the following four categories
Normotensives,
Hypertensives non-treated,
Hypertensives treated and controlled,
Hypertensives treated but uncontrolled.
And possible two additional categories
Hypertensives not aware of their HBP,
Hypertensives that for various reasons drop out from their treatment.
The total and CV mortality rates can vary considerably in each category and would need to be analysed separately to determine the benefits of treatment in each category.
A somewhat recent paper40 surveyed HTN treatment and control in five European countries (Germany, Sweden, England, Spain and Italy) and two North American ones (the USA and Canada) and another paper41 reported about treatment and control in Japan. HTN treatment in the European countries and Japan is about half that of the USA, while the control of HTN is between 5% and 10% in these countries versus around 30% in the USA, yet all of these countries, as aforementioned, have a higher life expectancy than the USA. Such numbers are difficult to decipher, at least at the population level, if indeed the treatment and control of HTN reduces mortality rates (realising that other factors, including dietary intakes, exercise, smoking, etc also influence CVD and survival in various populations).
Statistical concerns
In addition to epistemological and methodological issues, there are also statistical concerns with medical studies in general and HTN in specific. As in all statistical studies, there are measurement errors that influence the results. Such errors can be due to differences in measuring BP by direct or indirect instruments42 43 or between successive times.44 Furthermore, there are problems with ‘white coat’45 and ‘masked HTN’46 as well as the maximum BP47 that seems to be even more important than the average. These errors can and do seriously affect the findings of HTN studies in particular when BP is measured only once using non-standardised procedures.
A bigger problem than measurement errors is the way that statistical models are developed. In theory, one or more prior hypotheses must exist and then tested with the collected data to accept or reject it/them. Researchers, however, rarely follow theoretical prescriptions. Instead they test many hypotheses depending on what can be inferred from the data (in statistical parlance this is referred to as ‘fishing expedition’). In the process, if some results or relationships are contrary to conventional wisdom they are ignored and not reported. But in ‘fishing expeditions’ when many hypotheses are considered, some will be found to be significant by chance while others may exist because of spurious correlations. An example is a paper by Yates et al48 analysing the factors that distinguish male participants that reached 90 years of age (called the survivors) and those that did not. Two statistically significant factors of survivors were ‘shorter’ height and ‘arthritis’, clearly spurious findings contributed to reaching the age of 90. At the same time, information about the participants who had their HTN treated and those who did not, although known, was ignored, and its effects not reported, even though it would have been much more important than most of the other information presented by the authors.
Many HTN studies use regression as the primary statistical tool to explain life expectancy, or deaths, and the statistically significant factors involved. However, it is customary among statisticians and econometricians to report R2 when presenting regression results49 where R2 is a goodness-of-fit statistic. If, for example, the objective of regression is to measure losses in life expectancy associated with, say, the variables smoking, obesity and cholesterol, it indicates the percentage of such losses explained by these three variables. It may well be that the influence of all variables is statistically significant, as the results are based on large data sets collected through big surveys, but this is not enough if R2 is small. If R2, for instance, is 0.15 it means that the three variables used (smoking, obesity and cholesterol) explain only 15% of the variation in losses in life expectancy, while the remaining 85% is unaccountable. In addition, it is imperative that the residuals of the regression model must be tested to make sure that they are random. Moreover, small R2 coupled with non-random residuals can further diminish the explanatory power of regression and even render its results useless. Unfortunately, it is rare for the medical studies on HTN to report the value of R2, or state that the residuals are random. Some medical studies outside the HTN area50 have reported R2 values, which are extremely small, as little as 0.01, or rarely exceeding 0.3. With such small values the explanatory power of regression is minimal and its results cannot be trusted (generally any R2 value less than 0.5 or 0.6 is associated with a huge uncertainty, making any kind of prediction unreliable). This is particularly true when wanting to predict future cases that will inevitably be different than those when a model was fitted to past data. There is no doubt that there are conflicting conclusions in the various HT studies. The authors believe that the reasons for these conflicting conclusions are mainly due to the statistical concerns mentioned in these sections.
Lack of practicing evidence-based medicine
Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure-8 (JNC-8) does not recommend one thiazide diuretic over another, despite the fact that chlorthalidone and not hydrochlorothiazide (HCTZ) has the broadest amount of evidence for reducing CV events.51 Moreover, most clinicians do not seem to be practicing EBM, as greater than 1 million people received a prescription for HCTZ (monotherapy) in 2008, whereas only 25 000 people received chlorthalidone.52 Not only has chlorthalidone shown superiority over HCTZ for reducing CV events in the Multiple Risk Factor Intervention Trial (MRFIT)53 and a network meta-analysis,54 but chlorthalidone has shown superior reduction in left ventricular hypertrophy55 and reductions in heart failure54 vs HCTZ. Additionally, HCTZ has been shown to increase CV death and CHD in hypertensive patients compared to placebo or usual care in two large randomised trials, respectively.51 This begs the question, why is chlorthalidone not preferentially recommended over HCTZ in JNC-8? And has the treatment of HTN actually advanced? While a 22-year follow-up from the SHEP trial indicated that life expectancy gain with chlorthalidone was 105 days (95% CI −39 to 242; p=0.07) for all-cause mortality and 158 days (95% CI 36 to 287; p=0.009) for CV death.21 This translated into only a 1-day extension in life expectancy for each month of chlorthalidone treatment. Thus, to live just 1-year longer, an individual would have to be on chlorthalidone for 30 years. This begs the question, is the 1-year life extension worth the added cost and side effects of taking a prescription medication for 30 years? While each clinical scenario will determine the risk versus the benefit, an extension of life is not the only potential gain with antihypertensive therapy, as reductions in CV events and their consequences (eg, aphashia after a stroke) are also important to take into consideration. Regardless, a reduction in CV events/mortality will only be achieved through the practice of EBM.
JNC-8 versus the 2012 Cochrane meta-analysis
Recently, JNC-8 has recommended that the goal BP for all Americans should remain at <140/90 mm Hg.56 The exception is those who are 60 and older, where the goal BP has been raised to <150/90 mm Hg (unless the patient has diabetes or non-diabetic chronic kidney disease). However, one of the authors of a 2012 Cochrane meta-analysis has called for retraction of the JNC-8 guidelines, as they do not seem to match the current evidence in the literature. Indeed, the 2012 Cochrane meta-analysis found four randomised trials and looked at only healthy individuals with mild hypertension (SBP 140–159 mm Hg and diastolic BP 90–99 mm Hg).33 The meta-analysis found no reduction in CV events or mortality with antihypertensive therapy. Moreover, there was an almost fivefold significant increase in withdrawal due to adverse events. These data call into question the JNC-8 recommended BP goals of <140/90 and <150/90 mm Hg in these individuals.
Making things even more confusing, five authors of JNC-8 published a ‘minority view’, believe that JNC-8's recommendation for a BP goal of <150/90 mm Hg in those 60 and older should remain at <140/90 mm Hg.57 These authors inappropriately cite SHEP and HYVET (Hypertension in the Very Elderly Trial), as support for the more stringent goals, as these trials showed benefit of treating hypertension to an SBP goal between 140 and 145 mm Hg.57–59 However, these trials were in patients with a starting SBP of 160 mm Hg or higher, with the average SBP being much higher than 160 mm Hg. Thus, these do not apply to patients with mild hypertension (and thus should not support a BP goal of <140/90 mm Hg in these older individuals). Additionally, only three antihypertensive medications have evidence in this population, that being chlorthalidone (SHEP) and indapamide/perindoipril (HYVET). Thus, the use of any other antihypertensive medication(s) in this setting would strictly be considered non-evidence based; yet the JNC-8 guidelines have no preferential recommendation for these EBMs. In order to reduce CV risk, EBM needs to be integrated into HTN guidelines, and in all guidelines for that matter.
Despite the fact that the 2012 Cochrane meta-analysis is the most up-to-date evidence in the literature (and seemingly does not support the JNC-8 BP goals), it is important to note certain limitations with both lines of evidence. The Cochrane meta-analysis only contained four trials (and only 2 of them had a moderate amount of CV events/mortality). Additionally, none of the included trials used EBMs such as ACE inhibitors (ACE-Is) or amlodipine, both of which have been shown to reduce CV events (and mortality eg, ACE-Is) in other settings.60–62 Lastly, the Cochrane meta-analysis included trials that used antihypertensive medications that are rarely prescribed today (eg, pindolol, propranolol, reserpine, hydralazine, clonidine and chlorothiazide), limiting its generalisability.
The JNC-8 guidelines did not look at systematic reviews or meta-analyses when making their BP goal decisions, nor did they perform their own systematic review and meta-analysis. Thus, the JNC-8 guidelines are not completely comprehensive, partly explaining why their recommendations do no match the 2012 Cochrane meta-analysis.
Conclusions
In his widely cited paper Ioannidis6 states “There is increasing concern that in modern (medical) research, false findings may be the majority or even the vast majority of published research claims.” What are the reasons for such an extraordinary statement that renders medical research practically useless, as it makes impossible to separate the false from the true findings? We believe that the reasons have a lot to do with the epistemological, methodological and statistical concerns reported in this paper. Popper's theory advocates ‘falsifiability’ as the criterion distinguishing science from non-science. According to Popper even one single study whose results are contrary to the accepted theory is enough to falsify it. Given the extent of falsification in HTN studies findings would need to be applied with extreme care.
Medicine can be extremely useful when treating major CHD, strokes or traumas from car accidents. The same is true with the use of antibiotics to cure infectious diseases and most of vaccinations. But in many other cases, the harm from treatment can exceed the benefits, producing iatrogenics as with Galen's ‘medicine’, bloodletting and tonsillectomy and all the way to the widespread utilisation of preventive breast and prostate cancer tests. According to Taleb63 iatrogenics, concerned with costs and benefits, is linked to small and visible benefits coupled with large, delayed and hidden non-linear costs and this may well be the case with the treatment of HTN. Are the benefits from such treatment greater than the monetary costs and especially the negative side effects, including a life-long dependence on medical drugs? This is a critical question that must be answered by objective, scientific evidence.
There is a lot that can be done to deal with medicine's problems and avoid iatrogenics. First, patients must be provided with the truth in an objective and balanced way. In psychology the importance of framing64 is well known. If the results are presented in a negative fashion, decisions can be completely different than if presented in a positive way. It is obvious that if hypertensives are told that their life expectancy will be reduced by 5 years, they will be more likely to take drugs to lower it than if they are told that it will only be a few months or that various studies have come up with highly conflicting estimates and that the actual loss is highly uncertain. It would also help patients to make the right decision if they knew that in a study48 of male doctors, it was found that among those who reach the age of 90, 41.6% were hypertensives and among those who reached the age of 87.6, 49.1% were hypertensives. It would also be useful if patients are told that although about 67% of people over 70 are hypertensive about 0.04% between 65 and 74, 0.1% between 75 and 84 and 0.39% over 85 die each year due to their HBP (including hypertensive heart disease) according to the USA CDC. This means that the great majority of older people die from something else even though they have HBP. In addition, the negative side effects (ranging from sexual dysfunctions to depression and increased suicide rates) of HTN must be made clear. Potential patients should also be told that the majority of people treated to reduce their BP would not achieve the therapeutic level of 140/90, even if they take three or more drugs to do so and that the dropout rates from treatment approaches 10%.
HBP is a symptom, possibly like fever, and apart from a few cases, it is not known what is causing it. Could it be that there are beneficial reasons for HBP? For instance, a study of patients with acute heart failure found that those with lower SBP at admission had higher in-hospital and postdischarge mortality rates, while higher SBP at admission was associated with lower in-hospital mortality rates.65 Does this mean that high SBP helps patients recover from acute heart failures? Are there additional benefits of HBP we do not know? As a study found that if you are a man your best alternative is not to be aware of your HTN while the worse was to treat it but not manage to control it? This study29 separated men and women into five categories ((1) normotensives, (2). hypertensives treated whose BP has been controlled, (3) hypertensives treated whose BP has not been controlled, (4) hypertensives aware of their HBP but not treated and (5) hypertensives not aware of the HBP) and showed that if you are a hypertensive man you would minimise your chances of overall as well as CV-related mortality if you do not find out about it. If you find out, your chances of dying increases but according to this study, you should still not treat your HTN. If you are a hypertensive woman and if drug(s) manage to control your hypertension, then the benefits will be somehow better than if you were not aware of it, but you will be much worse off if your hypertension could not be controlled (around 60% of cases). This evidence is consistent with the vast literature of Self-Rated Health (SRH),66–68 which advocates that the way we feel today is the best predictor of how long we will live. Is Mother Nature wiser that we think, in particular if HBP serves some useful therapeutic function?
Ioannidis concludes that “false findings may be the majority or even the vast majority of published research claims” are not alone in raising serious concerns about recommendations to enter into a hypertension therapy. A recent Economist editorial69 argues that ‘science has changed the world but now it needs to change itself’ to end ‘flawed’ research and the risks of ‘shoddy’ conclusions. Finally, a new book by Gøtzsche shows the undue influence of pharma firms in recommending therapy and drugs and the potential dangers of such drugs that often exceed their assumed benefits.70
Footnotes
Contributors: SM and JJD wrote the manuscript. SM and JJD take responsibility for the overall content.
Funding: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None.
Provenance and peer review: Commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Estimates according to the USA National Heart, Lung, and Blood Institute. http://www.nhlbi.nih.gov/health/health-topics/topics/hbp/ (accessed 14 Jun 2013).
- 2.Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2224–60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. CDC (Source: NVSS) Mortality by underlying cause, ages 18+: US/State, 2001–2009. http://205.207.175.93/hdi/ReportFolders/ReportFolders.aspx?IF_ActivePath=P,21.
- 4.Chobanian AV. The hypertension paradox—more uncontrolled disease despite improved therapy. N Engl J Med 2009;361:878–87 [DOI] [PubMed] [Google Scholar]
- 5.According to a High Blood Pressure In-Depth Report of the New York Times. http://health.nytimes.com/health/guides/disease/hypertension/print.html
- 6.Ioannidis JP. Why most published research findings are false. PLoS Med 2005;2:e124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ioannidis JP. Contradicted and initially stronger effects in highly cited clinical research. JAMA 2005;294:218–28 [DOI] [PubMed] [Google Scholar]
- 8.Gawande A. The Cost Conundrum: what a Texas town can teach us about health care. New Yorker, 1 June 2009
- 9.Lewington S, Clarke R, Qizilbash N, et al. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002;360:1903–13 [DOI] [PubMed] [Google Scholar]
- 10.Franco OH, Peeters A, Bonneux L, et al. Blood pressure in adulthood and life expectancy with cardiovascular disease in men and women: life course analysis. Hypertension 2005;46:280–6 [DOI] [PubMed] [Google Scholar]
- 11.Clarke R, Emberson J, Fletcher A, et al. Life expectancy in relation to cardiovascular risk factors: 38 year follow-up of 19 000 men in the Whitehall study. BMJ 2009;339:b3513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bunker JP, Frazier HS, Mostellar F. Improving health: measuring effects of medical care. Milbank Q 1994;72:225–58 [PubMed] [Google Scholar]
- 13.Wright JC, Weinstein MC. Gains in life expectancy from medical interventions—standardizing data on outcomes. N Engl J Med 1998;339:380–6 [DOI] [PubMed] [Google Scholar]
- 14.Turin TC, Murakami Y, Miura K, et al. Hypertension and life expectancy among Japanese: NIPPON DATA80. Hypertens Res 2012;35:954–8 [DOI] [PubMed] [Google Scholar]
- 15.Ford ES, Trends in mortality from all causes and cardiovascular disease among hypertensive and nonhypertensive adults in the United States. Circulation 2011;123:1737–44 [DOI] [PubMed] [Google Scholar]
- 16.Port S, Demer L, Jennrich R, et al. Systolic blood pressure and mortality. Lancet 2000;355:175–80 [DOI] [PubMed] [Google Scholar]
- 17.Kearney PM, Whelton M, Reynolds K, et al. Global burden of hypertension: analysis of worldwide data. Lancet 2005;365:217–23 [DOI] [PubMed] [Google Scholar]
- 18.Burt VL, Cutler JA, Higgins M, et al. Trends in the prevalence, awareness, treatment, and control of hypertension in the adult US population: data from the Health Examination Surveys, 1960 to 1991. Hypertension 1995;26:60–9 [DOI] [PubMed] [Google Scholar]
- 19.Messerli FH, Panjrath GS. The J-curve between blood pressure and coronary artery disease or essential hypertension: exactly how essential? J Am Coll Cardiol 2009;54:1827–34 [DOI] [PubMed] [Google Scholar]
- 20.Banegas JR, Guallar-Castillón P, Rodríguez-Artalejo F, et al. Association between awareness, treatment, and control of hypertension, and quality of life among older adults in Spain. Am J Hypertens 2006;19:686–93 [DOI] [PubMed] [Google Scholar]
- 21.Kostis JB, Cabrera J, Cheng JQ, et al. Association between chlorthalidone treatment of systolic hypertension and long-term survival. JAMA 2011;306:2588–93 [DOI] [PubMed] [Google Scholar]
- 22.Beckett NS, Peters R, Fletcher AE, et al. Treatment of hypertension in patients 80 years of age or older. N Engl J Med 2008;358:1887–98 [DOI] [PubMed] [Google Scholar]
- 23.Gasowski J, Tikhonoff V, Stolarz-Skrzypek K, et al. Treatment of hypertension in the elderly in 2010: a brief review. Expert Opin Pharmacother 2010;11:2609–17 [DOI] [PubMed] [Google Scholar]
- 24.Wassertheil-Smoller S. Association between cardiovascular outcomes and antihypertensive drug treatment in older women. JAMA 2004;292:2849–59 [DOI] [PubMed] [Google Scholar]
- 25.Petrella R, Michailidis P. Retrospective analysis of real-world efficacy of angiotensin receptor blockers versus other classes of antihypertensive agents in blood pressure management. Clin Ther 2011;33:1190–203 [DOI] [PubMed] [Google Scholar]
- 26.Turnbull F; Blood Pressure Lowering Treatment Trialists’ Collaboration. Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials. Lancet 2003;362:1527–35 [DOI] [PubMed] [Google Scholar]
- 27.Pahor M, Psaty BM, Alderman MH, et al. Health outcomes associated with calcium antagonists compared with other first-line antihypertensive therapies. Lancet 2000;356:1949–54 [DOI] [PubMed] [Google Scholar]
- 28.Gu Q, Dillon CF, Burt VL, et al. Association of hypertension treatment and control. Am J Hypertens 2010;23:38–45 [DOI] [PubMed] [Google Scholar]
- 29.Barengo NC, Kastarinen M, Antikainen R, et al. The effects of awareness, treatment and control of hypertension on cardiovascular and all-cause mortality in a community-based population control of hypertension. J Hum Hypertens 2009;23:808–16 [DOI] [PubMed] [Google Scholar]
- 30.Dahlöf B, Lindholm LH, Hansson L, et al. Morbidity and mortality in the Swedish Trial in old patients with hypertension (STOP-hypertension). Lancet 1991;338:1281–5 [DOI] [PubMed] [Google Scholar]
- 31.Gudmundsson LS, Johannsson M, Thorgeirsson G, et al. Risk profiles and prognosis of treated and untreated hypertensive men and women in a population-based longitudinal study: the Reykjavik Study. J Hum Hypertens 2004;18:615–22 [DOI] [PubMed] [Google Scholar]
- 32.Almgren T, Persson B, Wilhelmsen L, et al. Stroke and coronary heart disease in treated hypertension—a prospective cohort study over three decades. J Intern Med 2005;257:496–502 [DOI] [PubMed] [Google Scholar]
- 33.Diao D, Wright JM, Cundiff DK, et al. Pharmacotherapy for mild hypertension. Cochrane Database Syst Rev 2012;8:CD006742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cutler JA, Sorlie PD. Trends in hypertension prevalence, awareness, treatment, and control rates in United States adults between 1988–1994 and 1999–2004. Hypertension 2008;52:818–27 [DOI] [PubMed] [Google Scholar]
- 35.Lindholm LH. The problem of uncontrolled hypertension. J Hum Hypertens 2002;16:S3–8 [DOI] [PubMed] [Google Scholar]
- 36.Doumas M, Papademetriou V, Douma S, et al. Benefits from treatment and control of patients with resistant hypertension. Int J Hypertens 2010;2011:318549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Calhoun DA, Jones D, Textor S, et al. Resistant hypertension: diagnosis, evaluation and treatment. Hypertension 2008;117:510–26 [Google Scholar]
- 38.Egan BM, Zhao Y, Axon RN, et al. Uncontrolled and apparent treatment resistant hypertension in the United States, 1988-2008. Circulation 2011;124:1046–58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Papadopoulos DP, Makris TK. Masked hypertension definition, impact, outcomes: a critical review. J Clin Hypertens (Greenwich) 2007;9:956–63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wolf-Maier K, Cooper RS, Kramer H, et al. Hypertension treatment and control in five European countries, Canada, and the United States. Hypertension 2004;43:10–17 [DOI] [PubMed] [Google Scholar]
- 41.Sekikawa A, Hayakawa T. Prevalence of hypertension, its awareness and control in adult population in Japan. J Hum Hypertens 2004;18:911–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Roberts LN, Smiley JR, Manning GW. A comparison of direct and indirect blood-pressure determinations. Circulation 1953;8:232–42 [DOI] [PubMed] [Google Scholar]
- 43.Breit SN, O'Rourke MF. Comparison of direct and indirect arterial pressure measurements in hospitalized patients. Aust N Z J Med 1974;4:485–91 [DOI] [PubMed] [Google Scholar]
- 44.Parati G. Blood pressure variability: its measurement and significance in hypertension. J Hypertens Suppl 2005;23:S19–25 [DOI] [PubMed] [Google Scholar]
- 45.Ohkubo T, Kikuya M, Metoki H, et al. Prognosis of ‘masked’ hypertension and ‘white-coat’ hypertension detected by 24-h ambulatory blood pressure monitoring: 10-year follow-up from the Ohasama Study. J Am Coll Cardiol 2005;46:508–15 [DOI] [PubMed] [Google Scholar]
- 46.Pickering TG, Davidson K, Gerin W, et al. Masked hypertension. Hypertension 2002;40:795–6 [DOI] [PubMed] [Google Scholar]
- 47.Rothwell PM, Howard SC, Dolan E, et al. Prognostic significance of visit-to-visit variability, maximum systolic blood pressure, and episodic hypertension. Lancet 2010;375:895–905 [DOI] [PubMed] [Google Scholar]
- 48.Yates LB, Djoussé L, Kurth T, et al. Exceptional longevity in men modifiable factors associated with survival and function to age 90 years. Arch Intern Med 2008;168:284–90 [DOI] [PubMed] [Google Scholar]
- 49.Makridakis SG, Wheelwright SC, Hyndman RJ. Forecasting: methods and applications. 3rd edn New York: Wiley and Sons, 1998 [Google Scholar]
- 50.Iezzoni LI, Ash AS, Coffman GA, et al. Predicting in-hospital mortality. A comparison of severity measurement approaches. Med Care 1992;30:347–59 [DOI] [PubMed] [Google Scholar]
- 51.DiNicolantonio JJ. Hydrochlorothiazide: is it a wise choice? Expert Opin Pharmacother 2012;13:807–14 [DOI] [PubMed] [Google Scholar]
- 52.Ernst ME, Lund BC. Renewed interest in chlorthalidone: evidence from the Veterans Health Administration. J Clin Hypertens 2010;12:927–34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Dorsch MP, Gillespie BW, Erickson SR, et al. Chlorthalidone reduces cardiovascular events compared with hydrochlorothiazide: a retrospective cohort analysis. Hypertension 2011;57:689–94 [DOI] [PubMed] [Google Scholar]
- 54.Roush GC, Holford TR, Guddati AK. Chlorthalidone compared with hydrochlorothiazide in reducing cardiovascular events: systematic review and network meta-analyses. Hypertension 2012;59:1110–17 [DOI] [PubMed] [Google Scholar]
- 55.Ernst ME, Neaton JD, Grimm RH, Jr, et al. Long-term effects of chlorthalidone versus hydrochlorothiazide on electrocardiographic left ventricular hypertrophy in the Multiple Risk Factor Intervention Trial. Hypertension 2011;58:1001–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.James PA, Oparil S, Carter BL, et al. 2014 Evidence-based guideline for the management of high blood pressure in adults: report from the Panel Members Appointed to the Eighth Joint National Committee (JNC 8). JAMA 2013;311:507–20 [DOI] [PubMed] [Google Scholar]
- 57.Wright JT, Jr, Fine LJ, Lackland DT, et al. Evidence supporting a systolic blood pressure goal of less than 150 mm Hg in patients aged 60 years or older: the minority view. Ann Intern Med 2014;160:499–503 [DOI] [PubMed] [Google Scholar]
- 58.No authors listed]. Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Final results of the Systolic Hypertension in the Elderly Program (SHEP). SHEP Cooperative Research Group. JAMA 1991; 265:3255–64 [PubMed] [Google Scholar]
- 59.Beckett NS, Peters R, Fletcher AE, et al. ; HYVET Study Group. Treatment of hypertension in patients 80 years of age or older. N Engl J Med 2008;358:1887–98 [DOI] [PubMed] [Google Scholar]
- 60.Fox KM, EURopean trial On reduction of cardiac events with Perindopril in stable coronary Artery disease Investigators. Efficacy of perindopril in reduction of cardiovascular events among patients with stable coronary artery disease: randomised, double-blind, placebo-controlled, multicentre trial (the EUROPA study). Lancet 2003;362:782–8 [DOI] [PubMed] [Google Scholar]
- 61.Yusuf S, Sleight P, Pogue J, et al. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. The Heart Outcomes Prevention Evaluation Study Investigators. N Engl J Med 2000;342:145–53 [DOI] [PubMed] [Google Scholar]
- 62.Nissen SE, Tuzcu EM, Libby P, et al. CAMELOT Investigators. Effect of antihypertensive agents on cardiovascular events in patients with coronary disease and normal blood pressure: the CAMELOT study: a randomized controlled trial. JAMA 2004;292:2217–25 [DOI] [PubMed] [Google Scholar]
- 63.Taleb NN. Antifragile: things that gain from disorder. New York: Random House, 2012 [Google Scholar]
- 64.Kahneman D, Tversky A. Choices, values, and frames. Cambridge: Cambridge University Press, 2000 [Google Scholar]
- 65.Gheorghiade M, Abraham WT, Albert NM, et al. Systolic blood pressure at admission, clinical characteristics, and outcomes in patients hospitalized with acute heart failure. JAMA 2006;296:2217–26 [DOI] [PubMed] [Google Scholar]
- 66.Mossey JM, Shapiro E. 2005, Self-rated health: a predictor of mortality among the elderly. J Epidemiol Community Health 2007;59:794–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.DeSalvo KB, Bloser N, Reynolds K, et al. Mortality prediction with a Single General Self-Rated Health Question: a meta-analysis. J Gen Intern Med 2005;20:267–75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Jylha M. What is self-rated health and why does it predict mortality? Towards a unified conceptual model. Soc Sci Med 2009;69:307–16 [DOI] [PubMed] [Google Scholar]
- 69.Problems with scientific research: How science goes wrong. The Economist, 19 October 2013
- 70.Gøtzsche PC. Deadly medicines and organized crime: how big pharma has corrupted healthcare. London/New York: Radcliffe, 2013 [Google Scholar]


