Abstract
Periprosthetic joint infection (PJI) after total knee arthroplasty remains a challenging problem. The aim of this study was to evaluate the accuracy of diagnostic knee aspiration and serum inflammatory markers in diagnostic of a PJI after total knee arthroplasty. Within 2011 and 2012, 46 patients received a one- or two-stage revision arthroplasty of the knee joint. These patients received a total number of 77 operations. A preoperative aspiration was performed in each case. We analyzed the microbiological and histological examinations of the samples from the aspiration and from the revision operation and additionally estimated serum inflammatory markers. The diagnostic aspiration had a specificity of 0.87, a sensitivity of 0.39, a positive predictive value of 0.67 and a negative predictive value of 0.68. For C-reactive protein the specificity was 0.61 and the sensitivity was 0.48, the serum white blood cell count had a specificity of 0.98 and a sensitivity of 0.23. Our data queries whether diagnostic joint aspiration or serum inflammatory markers are sufficient to verify or exclude a PJI.
Key words: diagnostic aspiration, periprosthetic joint infection, total joint arthroplasty, serum inflammatory marker
Introduction
There is no gold standard in the diagnosis and treatment of periprosthetic joint infection (PJI). PJI is one of the most common indications for revision total knee arthroplasty (TKA) with published incidence rates between 1% and 3%.1-4 Revision arthroplasty is a challenge for the surgeon, the patient, and the economics of health care. Several risk factors have been previously identified to develop a PJI including previous revision arthroplasty, tobacco use, rheumatoid arthritis, diabetes mellitus and wound healing complications.5,6 Most published diagnostic algorithms include preoperative radiographs, diagnostic joint aspiration, serum inflammatory markers, intraoperative cultures and pathology specimen. Parvizi and colleagues compared six published diagnostic algorithms and checked their prognosis on the basis of an own patient collective.7 They found eminent variations in prognosis security. A common thread among five of these six algorithms was the preoperative aspiration, which has been found to be an important tool for the diagnosis of PJI, with a sensitivity and specificity approaching 1.0. This is confirmed by other authors.1,7-13 The aim of the current study was to examine our experience with diagnostic criteria in a group of patients undergoing one-stage and two-stage revision knee arthroplasty.
Materials and Methods
Institutional review board approval was obtained. A retrospective study was performed, analyzing all cases of one- and two-stage revision knee arthroplasty between January 2011 and December 2012. The study consists of 16 male and 30 female patients. The mean age was 66.1±11.3 years. The revision arthroplasty was performed 46.4±39.2 month after primary TKA. There were 31 patients who received a two-stage revision and 15 patients with a one-stage revision of the knee joint. In cases with two-stage revision an aspiration was performed prior to explantation. Additionally an aspiration was performed prior to reimplantation of the prosthesis with an interval of 2 weeks to antibiotic treatment. Hence a diagnostic aspiration was performed in 77 cases. Three patients were excluded due to a dry tap at the time of aspiration and one patient developed an infection of another location between aspiration and revision surgery. The results of culture and histological examination both of the aspiration and of the intraoperative frozen sections were analyzed. At aspiration an infection was diagnosed when an infecting organism was found or the synovial white blood cell count (WBC) and synovial polymorphonuclear percentage (PNM%) was elevated. Intraoperative an infection was diagnosed when at least in two of five samples an infecting organism was found or when purulence appeared. In addition we estimated the levels of the serum inflammatory markers C-reactive protein (CRP) and serum WBC. The values and parameters were adapted from the Musculoskeletal Infection Society.13
The statistical analysis was performed with Graph Prism 5 (GraphPad Software, Inc., La Jolla, CA, USA) determining the sensitivity, specificity, positive and negative predictive value. The values are expressed with 95% confidence interval.
Results
An infection was diagnosed in 31 cases. The causative agent after final cultures was found to be Staphylococcus epidermidis in 15 cases, Proprionibacterium acnes in 5 cases, Staphylococcus aureus in 4 cases (3 of which were MRSA), Staphylococcus capitis in 3 cases, and in 1 case each Enterococcus faecalis, Corynebacterium jeikeium, Bacillus halodurans. In four cases two infecting organisms were found. In 5 cases no bacterium was found but the histology indicated an ongoing infection. The diagnostic aspiration had positive criteria for an infection in 18 cases. In 59 cases the aspiration did not indicate an infection. In this study the diagnostic aspiration had a specificity of 0.87 (0.74-0.95) and a positive predictive value of 0.67 (0.41-0.87). The negative predictive value was 0.68 (0.54-0.79) and the sensitivity was 0.39 (0.22-0.58) (Figure 1).
Figure 1.
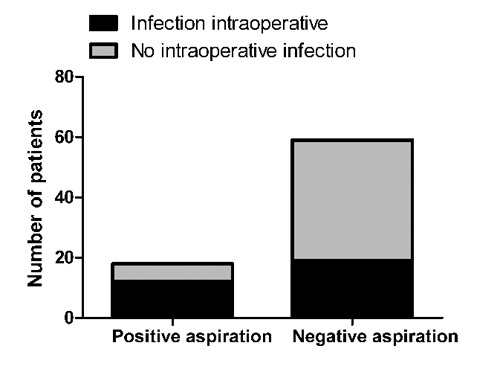
The diagnostic aspiration had a high value for Specificity but lower values for positive predictive values, sensitivity and negative predictive value.
C-reactive protein had a threshold of 0.5 mg/dL. It was elevated in 33 cases and it has had a normal value in 44 cases. The specificity was 0.61 (0.45-0.75), the sensitivity 0.48 (0.30-0.67), the positive predictive value 0.45 (0.28-0.64) and the negative predictive value 0.64 (0.48-0.78) (Figure 2). A threshold of 2.3 mg/dL leads to a specificity of 0.89 (0.76-0.96), a sensitivity of 0.29 (0.14-0.48), a positive predictive value of 0.64 (0.35-0.87) and a negative predictive value of 0.65 (0.52-0.77)
Figure 2.
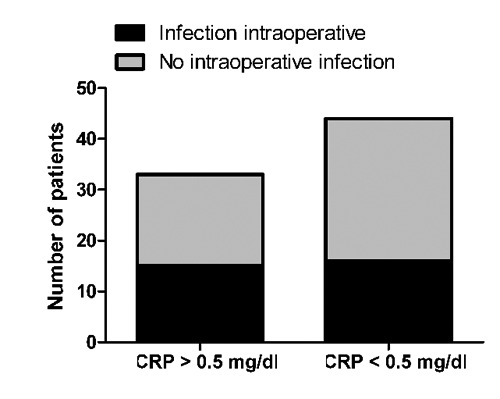
The values for sensitivity and positive predictive value were lower than 0.50. C-reactive protein had a specificity 0.61 and a negative predictive value of 0.64.
The serum WBC was elevated in 7 cases. In 90 cases the serum WBC was normal. The threshold was 10 thousand for female and 9.1 thousand for male. The sensitivity of the serum WBC for detecting an ongoing infection was 0.23 (0.1-0.4), the specificity 0.98 (0.88-1.0), the positive predictive value 0.88 (0.47-1.0) and the negative predictive value 0.65 (0.53-0.76) (Figure 3).
Figure 3.
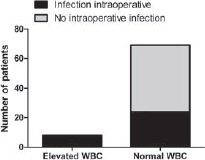
Serum white blood cell had high values for specificity and the positive predictive value.
Discussion
In cases of PJI a proper diagnosis is critical in determining surgical treatment. In cases of known infection, we perform a two-stage revision arthroplasty rather than a single stage revision that we perform in cases of aseptic failure. Thus the presumptive diagnosis has a big effect on therapy pathway that is affecting especially the patient. In recent literature there are several algorithms published.7 They generally combine pre- and intraoperative examinations.
The intraoperative examinations do not help with decision between one- or two-stage revisions. In addition the algorithms are often based on preoperative joint aspiration as a main diagnostic tool.7,8,10,11 The results of this study challenge the relevance of the preoperative aspiration to determine an ongoing infection. That does not count for specificity and positive predictive value. Here our data look alike to Duff’s study.11 But more important are sensitivity and negative predictive value. The aim is to perform a one-stage revision when an infection is excluded. And to perform a prosthesis re-implantation when an ongoing infection is excluded after occurred infection. Therefor the aspiration seems to be not sufficient. Schindler published likewise a sensitivity of 0.58. He found a better negative predictive value of 0.84. But he concluded that the meaning of the aspiration in diagnosis of periprosthetic joint infection has to be questioned.14
C-reactive protein does not seem to be accurate to indicate an ongoing infection. This is likewise to the published data. Kusuma and colleagues could not verify a serological parameter that indicates or excludes an infection.12 Only very high values for CRP have a better validity. This corresponds to a publication from Alijanipours and colleagues. They describe that the threshold of serum inflammatory markers has to be higher in cases of PJI. Thereby their accuracy is better.15 Simultaneous in cases of highly elevated CRP commonly the serum WBC is elevated. In this study it were just 8 of 77 cases. Then the specificity was 0.98 and an ongoing infection very probable. At once the serum WBC is not sufficient to exclude an ongoing infection due to a low sensitivity. There are not many alternatives for diagnosing an ongoing infection. Published algorithms mention open joint biopsies or arthroscopic biopsies.1,2,7 And there are additional serum markers like IL-6 and procalcitonin. But their accuracy was as poor as the accuracy of CRP.16
Conclusions
A proper diagnosis of a periprosthetic joint infection remains difficult. The reliability of standard diagnostic parameters is challenged by the present study. That points up the meaning of developing new diagnostic tools and to increase the scientific effort.
References
- 1.Parvizi J, Ghanem E, Sharkey P, et al. Diagnosis of infected total knee: findings of a multicenter database. Clin Orthop Relat Res 2008;466:2628-33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Peersman G, Laskin R, Davis J, Peterson M.Infection in total knee replacement: a retrospective review of 6489 total knee replacements. Clin Orthop Relat Res 2001;392:15-23 [PubMed] [Google Scholar]
- 3.Lange J, Troelsen A, Thomsen RW, Soballe K.Chronic infections in hip arthroplasties: comparing risk of reinfection following one-stage and two-stage revision: a systematic review and meta-analysis. Clin Epidemiol 2012;4:57-73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zmistowski B, Tetreault MW, Alijanipour P, et al. Recurrent periprosthetic joint infection: persistent or new infection? J Arthroplasty 2013;28:1486-9 [DOI] [PubMed] [Google Scholar]
- 5.Del Pozo JL, Patel R.Clinical practice. Infection associated with prosthetic joints. N Engl J Med 2009;361:787-94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tigani D, Trisolino G, Fosco M, et al. Two-stage reimplantation for periprosthetic knee infection: Influence of host health status and infecting microorganism. Knee 2013;20:9-18 [DOI] [PubMed] [Google Scholar]
- 7.Parvizi J, Jacovides C, Zmistowski B, Jung KA.Definition of periprosthetic joint infection: is there a consensus? Clin Orthop Relat Res 2011;469:3022-30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Squire MW, Della Valle CJ, Parvizi J.Preoperative diagnosis of periprosthetic joint infection: role of aspiration. AJR Am J Roentgenol 2011;196:875-9 [DOI] [PubMed] [Google Scholar]
- 9.Mortazavi SM, Schwartzenberger J, Austin MS, et al. Revision total knee arthroplasty infection: incidence and predictors. Clin Orthop Relat Res 2010;468:2052-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bedair H, Ting N, Jacovides C, et al. The Mark Coventry Award: diagnosis of early postoperative TKA infection using synovial fluid analysis. Clin Orthop Relat Res 2011;469:34-40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Duff GP, Lachiewicz PF, Kelley SS.Aspiration of the knee joint before revision arthroplasty. Clin Orthop Relat Res 1996;331:132-9 [DOI] [PubMed] [Google Scholar]
- 12.Kusuma SK, Ward J, Jacofsky M, et al. What is the role of serological testing between stages of two-stage reconstruction of the infected prosthetic knee? Clin Orthop Relat Res 2011;469:1002-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Workgroup Convened by the Musculoskeletal Infection Society. New definition for periprosthetic joint infection. J Arthroplasty 2011;26:1136-8 [DOI] [PubMed] [Google Scholar]
- 14.Schindler M, Christofilopoulos P, Wyssa B, et al. Poor performance of microbiological sampling in the prediction of recurrent arthroplasty infection. Int Orthop 2011;35:647-54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alijanipour P, Bakhshi H, Parvizi J.Diagnosis of Periprosthetic joint infection: the threshold for serological markers. Clin Orthop Relat Res 2013;471:3186-95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Glehr M, Friesenbichler J, Hofmann G, et al. Novel biomarkers to detect infection in revision hip and knee arthroplasties. Clin Orthop Relat Res 2013;471:2621-8 [DOI] [PMC free article] [PubMed] [Google Scholar]


