Abstract
Study Objectives:
To investigate the effects of one night's sleep deprivation on neurobehavioral functioning in adolescents.
Design:
Participants completed a neurobehavioral test battery measuring sustained attention, reaction speed, cognitive processing speed, sleepiness, and fatigue every 2 h during wakefulness. Baseline performance (defined as those test bouts between 09:00 and 19:00 on days 2 and 3, following two 10-h sleep opportunities) were compared to performance at the same clock time the day following total sleep deprivation.
Setting:
The sleep laboratory at the Centre for Sleep Research.
Participants:
Twelve healthy adolescents (6 male), aged 14-18 years (mean = 16.17, standard deviation = 0.83).
Measurements and Results:
Sustained attention, reaction speed, cognitive processing speed, and subjective sleepiness were all significantly worse following one night without sleep than following 10-h sleep opportunities (all main effects of day, P < 0.05). Sleep deprivation led to increased variability on objective performance measures. There were between-subjects differences in response to sleep loss that were task-specific, suggesting that adolescents may not only vary in terms of the degree to which they are affected by sleep loss but also the domains in which they are affected.
Conclusions:
These findings suggest that one night of total sleep deprivation has significant deleterious effects upon neurobehavioral performance and subjective sleepiness. These factors impair daytime functioning in adolescents, leaving them at greater risk of poor academic and social functioning and accidents and injuries.
Citation:
Louca M, Short MA. The effect of one night's sleep deprivation on adolescent neurobehavioral performance. SLEEP 2014;37(11):1799-1807.
Keywords: sleep, adolescence, attention, sleepiness, cognition
INTRODUCTION
Adolescence is an important and vulnerable stage of the lifespan.1 It is a period of significant brain maturation and myriad puberty-related biological and psychosocial changes.2,3 Sleep loss is endemic among adolescents.4 This is likely due to biological factors, such as changes to sleep homeostatic and circadian regulatory systems, and psychosocial changes including increased evening activities, more academic responsibilities and extracurricular activities, electronic media, and greater autonomy around sleep.5–7 Adolescence is also a period during which sleep may be especially important.8 Significant developmental milestones of this period, including completion of high school, forming more mature, adult relationships, and learning to drive rely upon skills and abilities known to be vulnerable to the deleterious effects of sleep loss. These include emotional regulation, risk taking, memory, attention, and executive functioning.6,9–13
Sleep is an essential restorative function necessary for optimal mental and physical health.8,14 In adults, sufficient sleep results in individuals who function better cognitively, physiologically, and emotionally.15–18 Well-rested adults are alert, mentally fast and accurate, focused, attentive, more emotionally stable, less risk taking, and have a good memory and sound executive decision making.19–21 However, it is unknown at what rate deficits of functioning accumulate in adolescents and whether this rate is different from that witnessed in adults. It is likely that adolescence is a sensitive period in which the effects of sleep restriction and deprivation are experienced more acutely due to a still-developing prefrontal cortex and greater sleep need.22–24 Studies of sleep loss in adolescent samples not only help to determine whether there is a differential vulnerability to sleep loss across development, but may also help to determine at what point sleep-related deficits cease to accumulate in adolescents and thus offer an additional line of evidence for recommendations regarding sleep need in this age group.25,26
To the authors' knowledge, only one study has investigated the effect of total sleep deprivation on cognitive functioning and sleepiness in adolescents. Carskadon et al. examined the effect of one night's sleep loss on subsequent nocturnal sleep, performance, and subjective and objective sleepiness. Participants exhibited a trend toward more sleepiness and faster sleep onset latencies during multiple sleep latency tests (MSLTs) throughout the day of sleep loss and had significantly worse performance on addition and word memory tests.27 Unfortunately, few studies have expanded on this seminal work using laboratory-based sleep deprivation protocols in adolescents.6,28–30 To date, experimental studies of sleep loss in adolescents have largely relied upon home-based protocols involving sleep restriction and/or sleep extension.6,31–35 These important studies reveal sleep-related deficits to processing speed and positive affect, anxiety during a catastrophizing task, worse quiz performance in a simulated classroom, and parent and self-reported sleepiness, inattention, worse behavior regulation, and deficits of metacognition. While these home-based studies have helped to inform the field, none examined total sleep deprivation. In addition, limitations are present in many home-based sleep restriction studies, including (1) inadequate control of confounding factors (i.e., light exposure, caffeine and substances known to affect alertness), (2) use of self-reports or parent-reports of sleep and functioning, and (3) concerns around compliance to study protocols.
The current study addresses this gap in the research by utilizing a tightly controlled laboratory protocol to investigate the effects of one night's sleep deprivation on neurobehavioral functioning and sleepiness in adolescents. It was hypothesized that adolescents would exhibit more lapses in attention, slower reaction times, slower cognitive processing speed, and increased sleepiness following one night of sleep deprivation compared to baseline performance following two 10-h sleep opportunities.
METHODS
Participants
Participants included 6 male and 6 female adolescents aged 14 to 18 years (mean = 16.17, standard deviation [SD] = 0.83) attending secondary schools in South Australia. Participants were physically and psychologically healthy, as determined through telephone screening using the Sleep, Medical, Education and Family History survey and a questionnaire battery including the School Sleep Habits Survey,36 Centre for Epidemiological Studies Depression Scale,37 Composite Morningness/ Eveningness Scale,38 Depression, Anxiety and Stress Scale (21 items),39 and Pediatric Daytime Sleepiness Scale.40 Participants were good sleepers, as determined by survey, sleep diary, and wrist actigraphy. Adolescents who indicated insufficient sleep (average < 8 h sleep/night41), sleep onset latencies > 30 min per night,42 weekend bedtime delay ≥ 2 h,43 or who were extreme morning or evening chronotypes28 were excluded from the study. Participants were not using any medication and had normal or corrected-to-normal vision.
All male participants and 2 female participants were Tanner stage 4 (late pubertal), and 2 female participants were Tanner stage 5 (post pubertal). The majority of participants lived with 2 parents (7 of 12); 4 lived with one parent (mother); and 1 lived with a grandparent. On average, participants reported that they usually obtained B grades at school, while none reported failing. This study had no attrition, with all participants completing the full protocol. Studies were run with groups of 4 participants in each study. In addition, at least 2 trained laboratory staff were present at all times during wakefulness. All studies were completed between April 2013 and July 2013.
The University of South Australia Human Research Ethics Committee approved this study. Written informed consent was obtained from each adolescent and their parent. Participants received an honorarium for their participation in the study.
Design
The study employed a repeated-measures design. The independent variables were day (baseline day 1, baseline day 2, and sleep deprivation) and time (09:00, 11:00, 13:00, 15:00, 17:00, and 19:00), and the dependent variables were PVT lapses, fastest 10% of PVT reaction times, cognitive processing speed, sleepiness, and fatigue. The baseline measures were drawn from Days 2 and 3 (which followed 10 h sleep opportunities in the laboratory), while the sleep deprivation measures were drawn from Day 4, which followed one night without sleep (Figure 1).
Figure 1.
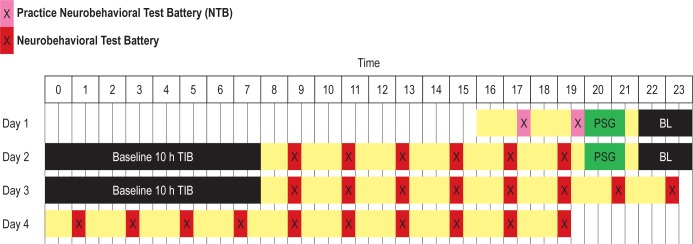
Schematic diagram of the study protocol. Time (24 h) is on the horizontal axis, and the vertical axis displays the 4 days of the study (adaptation, baseline day 1, baseline day 2, sleep deprivation day). Sleep opportunities are in black and wake times are in yellow. Pink crosses (X) indicate the timing of practice test batteries, red crosses indicate neurobehavioral test bouts, and PSG indicates the timing of PSG set-up in the evening.
Parents of potential participants underwent an initial telephone screen using the Sleep, Medical, Education and Family History Survey. Suitable participants were invited to attend an interview at the Centre for Sleep Research, where the adolescents completed a screening battery and were given a sleep diary and a wrist activity monitor (Actiwatch 2, Philips Respironics). Participants wore the activity monitor and completed a sleep diary for one week to measure sleep patterns. This involved recording daily bedtime, sleep onset and offset times, wake after sleep onset, as well as self-reported sleep quality and fatigue. For one week prior to the laboratory study, participants were required to maintain a regular sleep pattern, with bedtime at 22:00 and wake time at 07:00.41 Adherence was verified using sleep diaries and wrist activity monitors.
Participants spent 3 nights in the Sleep Laboratory of the Centre of Sleep Research, from 16:00 on Day 1 until 20:00 on Day 4 (Figure 1). The sleep laboratory is a sound attenuated, light and temperature controlled environment. Light exposure was < 50 lux during wake periods and < 1 lux during sleep periods. Ambient temperature was maintained at 21°C (± 1°C). Participants completed a neurobehavioral test battery (NTB), which included a 10-min Psychomotor Vigilance Task (PVT), Digit Symbol Substitution Task (DSST), Profile of Mood States-short form (not reported here), and the Karolinska Sleepiness Scale (KSS), every 2 h during wake, starting at 09:00 following the sleep periods to avoid any effects of sleep inertia on the first test bout. On the first 2 nights, a 10-h sleep opportunity was provided each night between 22:00 and 08:00 and measured using polysomnography (PSG). The polysomnographic montage included frontal (F3, F4), central (C3, C4), and occipital placements (O1, O2) referenced against A1/ A2; bilateral electrooculogram and electromyogram; and electrocardiogram. In between test bouts, participants could watch DVDs, play cards and board games, read, and complete jigsaw puzzles. Continuous behavioral monitoring ensured that participants remained awake during all designated wake periods.
Outcome Measures
Psychomotor Vigilance Task
The Psychomotor Vigilance Task (PVT-192, Ambulatory Monitoring) was used to measure sustained attention and reaction speed. The PVT is a reaction time task widely used in studies of sleep deprivation, as it is highly sensitive to sleep loss.44,45 Participants fixate on the apparatus screen and are required to press a button with their dominant hand when the stimulus appears. Inter-stimulus intervals ranged between 2 and 10 sec, and test bouts lasted for 10 minutes. Reaction speed (10% fastest reaction times) and number of PVT lapses (reaction times > 500 ms46) were obtained per trial. The PVT is argued to challenge participants to maintain cognitive output, provides test-retest stability, and reflects trait-like inter-individual differences.47 The PVT lapse criterion of reaction times > 500 ms and fastest 10% of reaction times are widely used in adult samples and have been validated for use in adolescent samples.46
Digit Symbol Substitution Task
The DSST involves the matching of digits (1-9) to symbols.48 The DSST used in the current study was a pencil and paper measure. It is a subject-paced task, and the number of correct responses in 60 sec was used as a measure of cognitive processing speed. The DSST is a subtest of the Wechsler Adult Intelligence Scale–Third Edition (WAIS-III) and has good validity and reliability (test-retest = 0.83; reliability coefficient = 0.93).49
Karolinska Sleepiness Scale
The KSS is a scale consisting of 10 statements relating to sleepiness, including “extremely sleepy, falls asleep all the time.”50 Participants select the statement that most accurately reflects their subjective sleepiness at the time. Scores range from 1 to 10, with higher scores indicating greater subjective sleepiness.
RESULTS
On average, adolescents obtained approximately 9 h of sleep on the baseline night (mean = 537.08 min, SD = 21.47 min), indicating that they likely obtained sufficient sleep prior to the sleep deprivation period and were unlikely to be carrying residual sleep debt. Assumption checking revealed that PVT lapses were not normally distributed (P < 0.05), having a significant positive skew. Transformation techniques failed to significantly reduce the skew. As repeated measures analysis of variance (ANOVA) is robust to violations of normality, parametric analyses were conducted using untransformed PVT lapse data. However, it is important to exercise caution when interpreting the ANOVA results for this variable.
A series of 3 (Day: baseline 1, baseline day 2, sleep deprivation) by 6 (Time: 09:00, 11:00, 13:00, 15:00, 17:00, 19:00) repeated measures ANOVAs were conducted to compare baseline neurobehavioral performance, sleepiness, and fatigue to the same measures following one night of total sleep deprivation at the same clock time. Due to the potential for changes in motivation over time to be confounded with the effects of sleep deprivation, both baseline days were included in the analyses. If motivation decreases over repeated presentations of the same test, we would expect performance to decline from baseline day 1 to baseline day 2, and not just from baseline day 2 to sleep deprivation. Thus, the inclusion of 2 baseline days helps to evaluate this competing explanation for any differences found between baseline and sleep deprivation days. Where violations of sphericity occurred in any analyses, significance levels were corrected using the Greenhouse-Geisser Epsilon.
Table 1 shows the results of the main effect of day (baseline 1, baseline 2, sleep deprivation) for mean PVT lapses, fastest 10% of reaction times, cognitive processing speed, sleepiness, and fatigue. ANOVA results showed a significant main effect of day on PVT lapses, with participants exhibiting significantly more lapses following sleep deprivation than on both baseline days, while there was no significant difference in lapses between baseline days. There was no significant main effect of time on PVT lapses, F5,55 = 1.37, P = 0.250 (partial η2 = 0.111); however, there was a significant interaction between day and time (F3.17, 34.89 = 3.33, P = 0.029 [partial η2 = 0.232]; see Figure 2). While lapses occurred more frequently following sleep deprivation than on both baseline days, the magnitude of this effect differed across time.
Table 1.
Means and standard errors of outcome measures at baseline and following sleep deprivation.
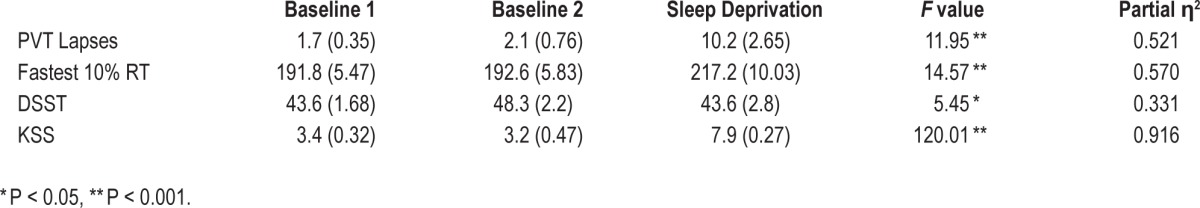
Figure 2.
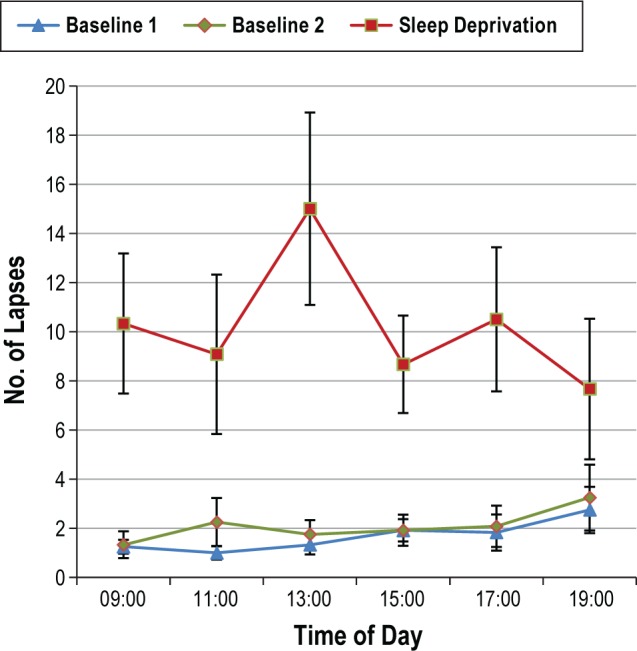
The estimated marginal means (± standard error) of Psychomotor Vigilance Task (PVT) lapses at each time point across baseline and sleep deprivation days.
When examining reaction speed, ANOVA results revealed a significant main effect of day, with slower reaction times recorded following sleep deprivation than on both baseline days (Table 1), but no significant difference between baseline days. There was no significant main effect of time (F5,55 = 0.62, P = 0.683 [partial η2 = 0.054]) and no significant interaction between day and time in their effect on reaction speed (F4.22, 46.40 = 1.67, P = 0.097 [partial η2 = 0.132]; Figure 3).
Figure 3.
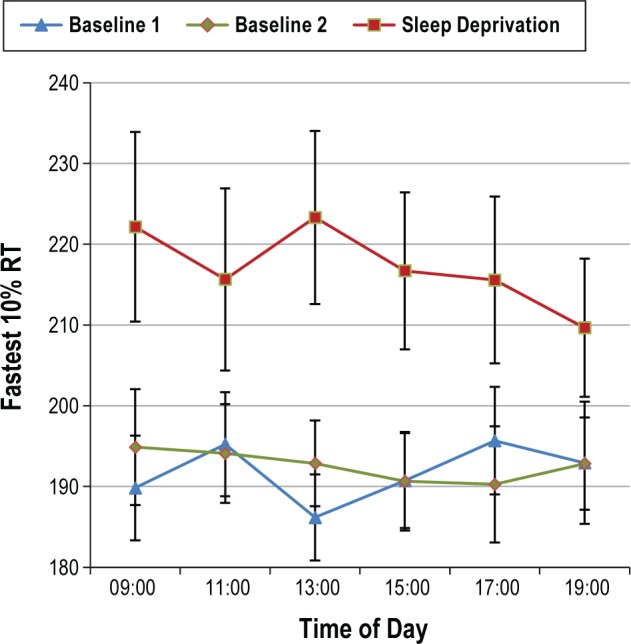
The estimated marginal means (± standard error) of Psychomotor Vigilance Task (PVT) fastest 10% reaction time at each time point across baseline and sleep deprivation days.
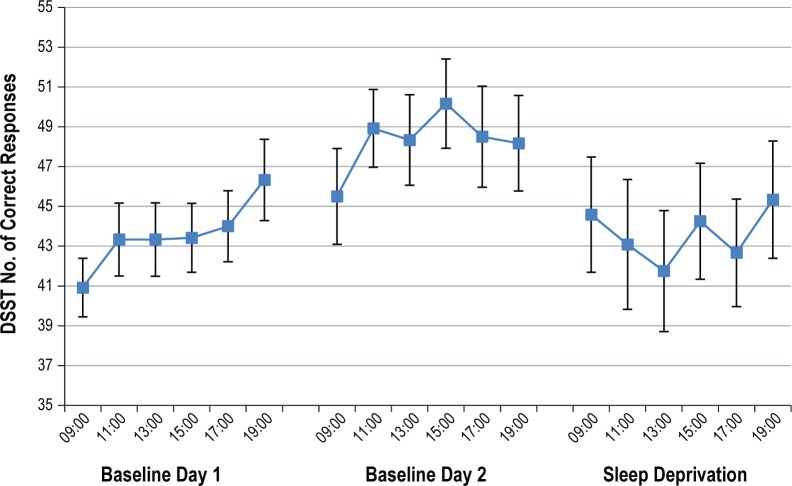
ANOVA results revealed a significant main effect of day on DSST correct responses. The number of correct responses was significantly higher on baseline day 2 than on baseline day 1. Participants made significantly fewer correct responses on the DSST subsequent to sleep deprivation than they did on baseline day 2 (Table 1). There was a significant main effect of time on cognitive processing speed (F5,55 = 4.74, P = 0.001 [partial η 2 = 0.301]), with participants generally recording fewer correct responses during trials earlier in the day lower than those later in the day. Both of these main effects reveal not only the effect of sleep deprivation, but also practice effects that are known to occur with this measure. As such, there is a normal pattern of improved performance over trials and improved performance from baseline day 1 to baseline day 2. This normal learning is arrested by sleep deprivation, with scores decreasing from baseline day 2 to sleep deprivation. There was also a significant interaction between day and time (F6.14, 67.49 = 2.91, P = 0.003 [partial η2 = 0.209] Figure 4). While the number of correct responses on the DSST tended to be lower after one night without sleep when compared to baseline, the magnitude of this difference varied over time.
Figure 4.
The estimated marginal means (± standard error) of number of Digit Symbol Substitution Task (DSST) correct responses at each time point across baseline and sleep deprivation days.
When examining ANOVA results for subjective sleepiness, a significant main effect of day on sleepiness was found. Significantly higher levels of sleepiness were reported following sleep deprivation than on either baseline day (Table 1). There was no significant main effect of time on sleepiness (F5,55 = 0.92, P = 0.473 [partial η2 = 0.077]); however, there was a significant interaction between day and time on their effect on sleepiness (F4.61, 50.70 = 2.31, P = 0.017 [partial η2 = 0.174]). Specifically, while sleepiness scores were uniformly higher during sleep deprivation than on baseline days, sleepiness scores increased at 19:00 on both baseline days (likely reflecting increased homeo-static sleep drive), while they decreased slightly at 19:00 on the sleep deprivation day (Figure 5). This decrease may reflect participants heightened alertness in anticipation of leaving the laboratory following the final test bout.
Figure 5.
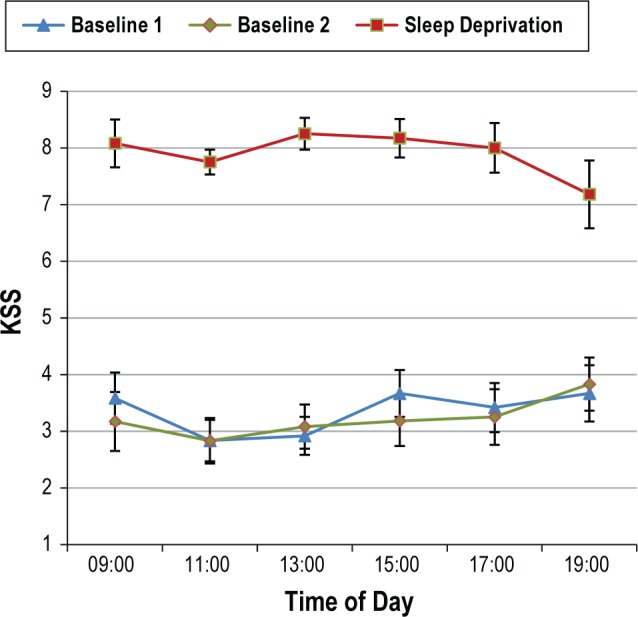
The estimated marginal means (± standard error) of sleepiness scores on the Karolinska Sleepiness Scale (KSS) at each time point across baseline and sleep deprivation days.
Sleep deprivation increased inter-individual variance in objective performance, with variability increasing following one night without sleep compared to baseline, as seen in the standard error values in Table 1. Standard deviation values at each time point were compared between baseline day 2 and sleep deprivation using paired samples t-tests. Results showed significantly higher standard deviation scores during sleep deprivation for lapses, fastest reaction times, and DSST (all P < 0.008). While there was a trend for variability to decrease in subjective sleepiness (with participants uniformly reporting higher subjective sleepiness following sleep deprivation), this was not significant.
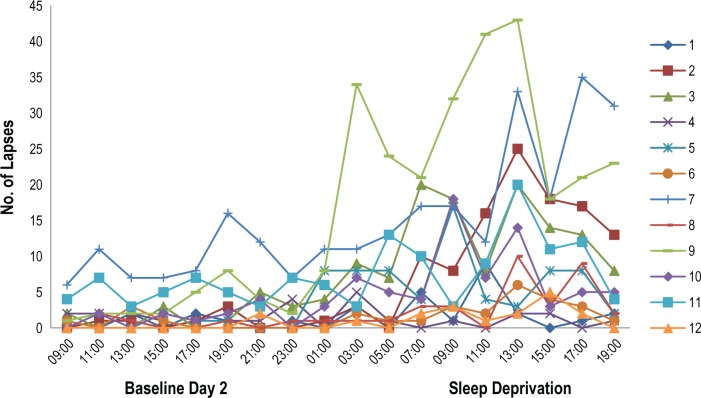
The large between-subjects variance in performance deficits following sleep deprivation was especially marked for sustained attention performance, with some participants able to maintain performance relatively well with ongoing wakefulness and others exhibiting marked deficits, as seen in Figure 6. One possible explanation for the smaller changes in performance seen in some individuals is that, in an effort to avoid lapses of attention (errors of omission), they may commit more premature responses (errors of commission). Errors of commission include both false starts (responding when no stimulus has been presented) and coincident responses (responses coincident with a stimulus, but that occur prior to a time most individuals can physiologically register the stimulus, in this case < 100 ms). To explore this possibility, a Pearson correlation was used to examine the relationship between changes in lapse scores between baseline day 2 and sleep deprivation with changes to errors of commission across these days. Results revealed a moderate, negative correlation, r (10) = −0.46, P = 0.129, although this did not reach statistical significance, likely due to the small sample size. Thus, there was a trend for those participants who experienced less performance decline on lapses to have greater performance deficits in terms of increased errors of commission.
Figure 6.
Psychomotor Vigilance Task (PVT) lapses per test bout for each participant at each time point.
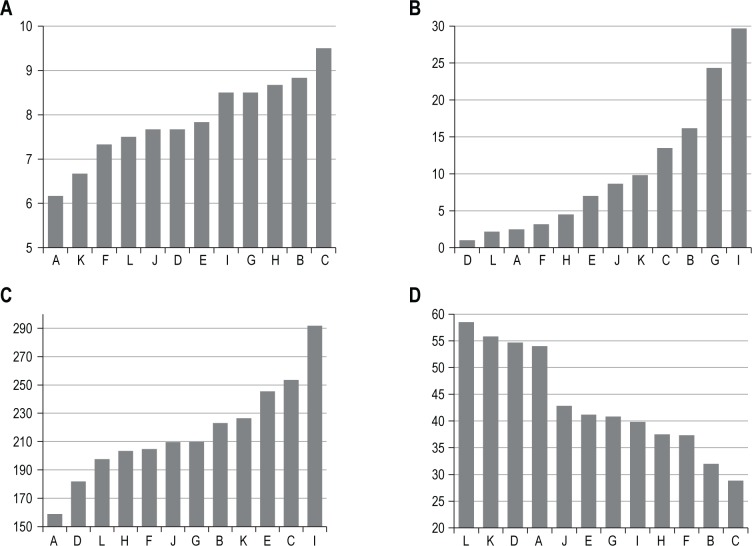
Between-subjects variability was not consistent across different domains. Figure 7 shows the ranked mean scores for each participant following sleep deprivation. While participants with the greatest performance deficits in one domain did not necessarily show deficits of the same magnitude in other domains, there were moderate to large associations between outcome measures. However, it is important to note that only the relationship between the PVT measures and that between the DSST and subjective sleepiness reached statistical significance.
Figure 7.
Ranked mean scores for each participant on the (A) Karolinska Sleepiness Scale (KSS), (B) Psychomotor Vigilance Task (PVT) lapses, (C) PVT fastest 10% reaction times, and (D) Digit Symbol Substitution Task (DSST) following sleep deprivation. Scores were ranked with individuals showing the best performance on the left of the x-axis and those with the worst performance on the right. Data were averaged from test bouts occurring from 09:00 until 19:00 on the sleep deprivation day. Pearson correlations: PVT lapses and DSST: r = -0.45, P = 0.14, PVT lapses and fastest RT: r = 0.72, P = 0.009, lapses and KSS: r = 0.53, P = 0.079, fastest RT and DSST: r = -0.52, P = 0.085, fastest RT and KSS: r = 0.57, P = 0.054, DSST and KSS: r = -0.79, P = 0.002.
DISCUSSION
The present study exposed adolescents to one night without sleep to test the hypotheses that adolescents would display significantly worse neurobehavioral performance, sleepiness, and fatigue following one night of sleep deprivation. As expected, neurobehavioral performance was significantly worse following sleep deprivation, with large effect sizes found for all measures. Performance did not significantly differ between baseline days 1 and 2, except for DSST correct responses, where this difference was consistent with anticipated practice effects. Thus, it is unlikely that the pattern of results witnessed result from decreased motivation with repeated presentations of the same test. Participants exhibited significantly more PVT lapses on sleep deprivation day compared to baseline day, suggesting that their ability to sustain attention was significantly impaired after one night without sleep. There was also a significant interaction between time and day in their effect on PVT lapses. During the baseline day, PVT performance in terms of lapses was relatively consistent. However, across the sleep deprivation day, the number of lapses varied both within and between participants. This may reflect greater instability of performance following sleep deprivation, consistent with the waking state instability hypothesis.51 This hypothesis considers performance lapses to be a result of fundamental increases in momentary variability of attention. This instability is influenced by the interaction of the homeostatic drive for sleep, the endogenous circadian promotion of wakefulness, and the redeeming effort by participants to perform.51 The critical feature of performance in this concept is variability, as the hypothesis does not assume that sleep loss completely eradicates any specific neurobehavioral function.51 Doran et al. found that participants exposed to total sleep deprivation exhibited much greater variability in performance as sleep loss continued, suggesting that the growing variability in PVT lapses was due to cumulative time awake.51 This increased variability was also witnessed in the current study.
Results also showed that, on average, the fastest 10% of reaction times were significantly slower following sleep deprivation compared to the baseline day, supporting the hypothesis. This suggests that adolescents' fastest reaction times, which reflect their peak responses, are significantly slowed by sleep deprivation, consistent with previous research in adults.21,51 It is likely that this slowing is a reflection of general state-related changes in brain activity. Brain regions affected by sleep deprivation can be largely task-dependent; however, certain areas such as the thalamus, anterior cingulate cortex, middle prefrontal gyrus, and inferior parietal lobes, appear to show hypoactivation after sleep deprivation across a large number of paradigms.21 This suggests that this brain network may be accountable for state-related changes in vigilance, which initiate a global slowing of reaction times.21 Adult research has shown that short-term sleep deprivation produces global decreases in brain activity, with larger reductions in the corticothalamic network that mediates attention and high-order cognitive processes.11,52
Cognitive processing speed, as measured by the DSST, significantly slowed following sleep deprivation. Once again, reduced cognitive speed in response to sleep deprivation has been related to decreases in brain activation.11,21,52 Thomas and colleagues11 found decreases in activation in the thalamus, parietal, and prefrontal cortices during sleep deprivation, which were correlated with cognitive performance over time. Deactivation in brain regions necessary to perform operations relevant to the task may be a potential mechanism which accounts for the reduction in cognitive processing speed of adolescents in the current study.
Results also showed that adolescent sleepiness was significantly heightened by one night of sleep deprivation. The findings of the current study are consistent with those of Carskadon et al.27 and sleep restriction paradigms with adolescent samples.31,32,35
When considering these findings, it is important to note that while overall results indicated substantial deficits in all outcome measures, large inter-individual differences were found in response to sleep deprivation. Individual variability in neurobehavioral impairment following sleep loss has been investigated by Van Dongen and colleagues53 in order to establish the extent to which neurobehavioral responses to sleep loss are a function of sleep history versus trait-like differential vulnerability. While observed differences in response subsequent to sleep deprivation can be partially explained through individual differences in sleep history, this does not explain the persistent individual differences in response to sleep deprivation that are encountered in sleep deprivation studies that control for prior sleep.53 Van Dongen demonstrated that inter-individual differences in neurobehavioral deficits from sleep loss reflect a trait-like differential vulnerability to sleep loss. This may account for the substantial individual differences witnessed in adolescent performance following sleep loss. Similar to the findings of Van Dongen, the present study also found that decrements in one domain do not necessarily generalize to the same extent across other domains. Thus, adolescents may not only vary from one another in terms of the degree to which they are affected by sleep loss, but also the domains in which they are affected.
Overall, these findings confirm the detrimental effects of one night of sleep deprivation to adolescent feeling and functioning. Sleep loss significantly affects domains of sustained attention, reaction speed, cognitive processing speed, and sleepiness, consistent with results found in adult studies.11,16,44,45 These abilities are imperative to sufficient daytime functioning for adolescents in a variety of settings. A study conducted by Drummond and colleagues found that healthy adults had an average increase of 2.3 PVT lapses per 10-minute test bout in the day following sleep deprivation and an average 14 ms slowing in fastest 10% of reaction times.45 In the current study, healthy adolescent participants had an average increase of 8.1 lapses per test bout in the day following one night without sleep and an average 24.6 ms slowing in fastest 10% reaction times. While this comparison must be interpreted with caution due to differences in protocol, these results indicate that adolescents may have a greater vulnerability to the effects of sleep loss and exhibit heightened performance deficits than adults exposed to the same degree of sleep loss.
The neurobehavioral deficits witnessed in the current study have serious applied ramifications. Two particularly salient aspects of this stage of development are completing a high school education and learning to drive. While lapses of attention may be relatively benign in the sleep laboratory environment, even a small lapse of attention in a novice driver could have life-threatening consequences. Pizza and colleagues found that sleep complaints among adolescents significantly predicted their self-reported crash risk.12 It is also important when driving to have an optimal reaction time in order to respond to stimuli on the road. Adolescents' peak reaction times were significantly slower following sleep loss, indicating that even when they are sustaining vigilant attention, they are unable to respond as quickly to stimuli. Recently, just one night of sleep restricted to 4 hours has also been shown to lead to more risky pedestrian behavior in adolescents,54 highlighting the broader safety risks associated with insufficient sleep.
Cognitive processing speed is important for the fluent processing of information and efficient thinking and learning. This cognitive capacity significantly affects executive functions and academic achievement.35 The slowing of cognitive processing witnessed in DSST performance following sleep deprivation may negatively affect classroom learning. When sleep deprived adolescents attend school or attempt to sit an exam, slowing of cognitive processing speed, together with lapses of attention, slowed peak response times, and heightened subjective sleepiness mean that their capacity to learn and to perform the many cognitive tasks that are underpinned by these basic constructs are likely to be diminished.55 The decrements to cognitive processing speed following sleep deprivation are even more striking when considering that the DSST is susceptible to learning effects. As such, with repeated trials, performance is expected to increase. The present study found that, not only did performance not improve, but rather it substantially declined with continual wakefulness.
The current study has a number of strengths. Firstly, this study utilized objective measurements of attention, reaction time, and cognitive processing speed. This extends the limited work in this area, which has primarily used subjective measures. The use of objective performance tasks avoids many of the response biases that are inherent in subjective reports. Secondly, the use of a within-subjects design increases the power of the study to detect significant differences by reducing the error variances associated with individual differences. Thirdly, the current study was conducted within a sleep laboratory setting, which allowed for control of extraneous factors such as light exposure, use of caffeine and other stimulants, and adherence to protocol.
There are also a number of limitations of this study, which are important to consider when interpreting these findings. One limitation is the reduced ecological validity of the laboratory environment. It is likely that adolescents who endure one night without sleep outside of a laboratory setting would employ various countermeasures to bolster their alertness. In addition, the laboratory environment itself may affect participants in ways that might affect their performance and subjective alertness.56 The use of a true experimental design which included a non-sleep deprived condition would address this limitation. In addition, the present study utilized a group of highly screened adolescent participants who were healthy, good sleepers. As such, the degree to which the pattern of results witnessed in the present study can be generalized to other adolescents, particularly naturally long or short sleepers, is unknown. Lastly, while adolescence is a developmental period in which sleep deprivation is more likely to occur, chronic sleep restriction is likely to be more common than acute total sleep deprivation. At present, these findings are being extended to included laboratory-based sleep restriction protocols to investigate this more common form of sleep loss in adolescents.
To the authors' knowledge, the current study is one of the few to revisit adolescent total sleep deprivation since the early 1980s. Future research in the area of adolescent sleep deprivation would profit from examining other aspects of cognition, emotional regulation, and risk-taking, all of which have considerable applied relevance to this age group. This would provide a wider insight to other possible deficits associated with one night of sleep loss in adolescents. The results of the current study provide a concerning insight to the severity of deficits associated with one night without sleep in the developing adolescent.
DISCLOSURE STATEMENT
This was not an industry supported study. This work was performed at the Centre for Sleep Research, University of South Australia and was funded by a University of South Australia Divisional Research Performance grant. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The authors thank the editors and reviewers for their generous and thoughtful feedback. We thank Alex Agostini, Alex Chatburn, Scott Coussens, Rachel Hadcroft, Bel James, Nick Scalzi, and Jasper Wolfe for their assistance in implementing the study protocol, Alastair King, Natarsha Kallios, Morgan Peele, and Sheridan Comer for assistance with data entry, and Dr. Helen Wright, Dr. Jillian Dorrian, and Gabrielle Rigney for their feedback on earlier drafts of this manuscript. We also thank our adolescent participants and their parents for making this study a joy to run.
REFERENCES
- 1.Dagys N, McGlinchey EL, Talbot LS, Kaplan KA, Dahl RE, Harvey AG. Double trouble? The effects of sleep deprivation and chronotype on adolescent affect. J Child Psychol Psychiatry. 2012;53:660–7. doi: 10.1111/j.1469-7610.2011.02502.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Paus T. Mapping brain maturation and cognitive development during adolescence. Trends Cogn Sci. 2005;9:60–8. doi: 10.1016/j.tics.2004.12.008. [DOI] [PubMed] [Google Scholar]
- 3.Lerner R. Adolescent maturational changes and psychosocial development: A dynamic interactional perspective. J Youth Adolesc. 1985;14:355–72. doi: 10.1007/BF02089239. [DOI] [PubMed] [Google Scholar]
- 4.Calamaro CJ, Mason TB, Ratcliffe SJ. Adolescents living the 24/7 lifestyle: effects of caffeine and technology on sleep duration and daytime functioning. Pediatrics. 2009;123:e1005–10. doi: 10.1542/peds.2008-3641. [DOI] [PubMed] [Google Scholar]
- 5.Hagenauer MH, Perryman JI, Lee TM, Carskadon MA. Adolescent changes in the homeostatic and circadian regulation of sleep. Dev Neurosci. 2009;31:276–84. doi: 10.1159/000216538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Talbot LS, McGlinchey EL, Kaplan KA, Dahl RE, Harvey AG. Sleep deprivation in adolescents and adults: changes in affect. Emotion. 2010;10:831–41. doi: 10.1037/a0020138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Short MA, Gradisar M, Lack LC, et al. A cross-cultural comparison of sleep duration between US And Australian adolescents: the effect of school start time, parent-set bedtimes, and extracurricular load. Health Educ Behav. 2013;40:323–30. doi: 10.1177/1090198112451266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dahl RE, Lewin DS. Pathways to adolescent health sleep regulation and behavior. J Adolesc Health. 2002;31:175–84. doi: 10.1016/s1054-139x(02)00506-2. [DOI] [PubMed] [Google Scholar]
- 9.Nilsson JP, Söderström M, Karlsson AU, et al. Less effective executive functioning after one night's sleep deprivation. J Sleep Res. 2005;14:1–6. doi: 10.1111/j.1365-2869.2005.00442.x. [DOI] [PubMed] [Google Scholar]
- 10.Turner TH, Drummond SP, Salamat JS, Brown GG. Effects of 42 hr of total sleep deprivation on component processes of verbal working memory. Neuropsychology. 2007;21:787–95. doi: 10.1037/0894-4105.21.6.787. [DOI] [PubMed] [Google Scholar]
- 11.Thomas M, Sing H, Belenky G, et al. Neural basis of alertness and cognitive performance impairments during sleepiness. I. Effects of 24 h of sleep deprivation on waking human regional brain activity. J Sleep Res. 2000;9:335–52. doi: 10.1046/j.1365-2869.2000.00225.x. [DOI] [PubMed] [Google Scholar]
- 12.Pizza F, Contardi S, Antognini AB, et al. Sleep quality and motor vehicle crashes in adolescents. J Clin Sleep Med. 2010;6:41–5. [PMC free article] [PubMed] [Google Scholar]
- 13.O'Brien EM, Mindell JA. Sleep and risk-taking behavior in adolescents. Behav Sleep Med. 2005;3:113–33. doi: 10.1207/s15402010bsm0303_1. [DOI] [PubMed] [Google Scholar]
- 14.Short MA, Banks S. The functional impact of sleep deprivation, sleep restriction, and sleep fragmentation. In: Bianchi MT, editor. Sleep deprivation and disease. New York: Springer; 2014. pp. 13–26. [Google Scholar]
- 15.Durmer JS, Dinges DF. Neurocognitive consequences of sleep deprivation. Semin Neurol. 2005;25:117–29. doi: 10.1055/s-2005-867080. [DOI] [PubMed] [Google Scholar]
- 16.Franzen PL, Siegle GJ, Buysse DJ. Relationships between affect, vigilance, and sleepiness following sleep deprivation. J Sleep Res. 2008;17:34–41. doi: 10.1111/j.1365-2869.2008.00635.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Giuditta A, Ambrosini MV, Montagnese P, et al. The sequential hypothesis of the function of sleep. Behav Brain Res. 1995;69:157–66. doi: 10.1016/0166-4328(95)00012-i. [DOI] [PubMed] [Google Scholar]
- 18.Spiegel K, Leproult R, Van Cauter E. Impact of sleep debt on metabolic and endocrine function. Lancet. 1999;354:1435–9. doi: 10.1016/S0140-6736(99)01376-8. [DOI] [PubMed] [Google Scholar]
- 19.Van Dongen HP, Maislin G, Mullington JM, Dinges DF. The cumulative cost of additional wakefulness: dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation. Sleep. 2003;26:117–26. doi: 10.1093/sleep/26.2.117. [DOI] [PubMed] [Google Scholar]
- 20.Belenky G, Wesensten NJ, Thorne DR, et al. Patterns of performance degradation and restoration during sleep restriction and subsequent recovery: a sleep dose-response study. J Sleep Res. 2003;12:1–12. doi: 10.1046/j.1365-2869.2003.00337.x. [DOI] [PubMed] [Google Scholar]
- 21.Lim J, Dinges DF. Sleep deprivation and vigilant attention. Ann N Y Acad Sci. 2008;1129:305–22. doi: 10.1196/annals.1417.002. [DOI] [PubMed] [Google Scholar]
- 22.Beebe DW. Cognitive, behavioral, and functional consequences of inadequate sleep in children and adolescents. Pediatr Clin North Am. 2011;58:649–65. doi: 10.1016/j.pcl.2011.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Carskadon MA, Harvey K, Duke P, Anders TF, Litt IF, Dement WC. Pubertal changes in daytime sleepiness. Sleep. 1980;2:453–60. doi: 10.1093/sleep/2.4.453. [DOI] [PubMed] [Google Scholar]
- 24.Anderson P. Assessment and development of executive function (EF) during childhood. Child Neuropsychol. 2002;8:71–82. doi: 10.1076/chin.8.2.71.8724. [DOI] [PubMed] [Google Scholar]
- 25.Feinberg I. Recommended sleep durations for children and adolescents: the dearth of empirical evidence. Sleep. 2013;36:461–2. doi: 10.5665/sleep.2520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Matricciani L, Blunden S, Rigney G, Williams MT, Olds TS. Children's sleep needs: is there sufficient evidence to recommend optimal sleep for children? Sleep. 2013;36:527–34. doi: 10.5665/sleep.2538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Carskadon MA, Harvey K, Dement WC. Sleep loss in young adolescents. Sleep. 1981;4:299–312. doi: 10.1093/sleep/4.3.299. [DOI] [PubMed] [Google Scholar]
- 28.Copes K, Rosentswieg J. The effects of sleep deprivation upon motor performance of ninth-grade students. J Sports Med Phys Fitness. 1972;12:47–53. [PubMed] [Google Scholar]
- 29.Jenni OG, Achermann P, Carskadon MA. Homeostatic sleep regulation in adolescents. Sleep. 2005;28:1446–54. doi: 10.1093/sleep/28.11.1446. [DOI] [PubMed] [Google Scholar]
- 30.McGlinchey EL, Talbot LS, Chang KH, Kaplan KA, Dahl RE, Harvey AG. The effect of sleep deprivation on vocal expression of emotion in adolescents and adults. Sleep. 2011;34:1233–41. doi: 10.5665/SLEEP.1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Beebe DW, Fallone G, Godiwala N, et al. Feasibility and behavioral effects of an at-home multi-night sleep restriction protocol for adolescents. J Child Psychol Psychiatry. 2008;49:915–23. doi: 10.1111/j.1469-7610.2008.01885.x. [DOI] [PubMed] [Google Scholar]
- 32.Jiang F, VanDyke RD, Zhang J, Li F, Gozal D, Shen X. Effect of chronic sleep restriction on sleepiness and working memory in adolescents and young adults. J Clin Exp Neuropsychol. 2011;33:892–900. doi: 10.1080/13803395.2011.570252. [DOI] [PubMed] [Google Scholar]
- 33.Dewald-Kaufmann JF, Oort FJ, Meijer AM. The effects of sleep extension on sleep and cognitive performance in adolescents with chronic sleep reduction: An experimental study. Sleep Med. 2013;14:510–7. doi: 10.1016/j.sleep.2013.01.012. [DOI] [PubMed] [Google Scholar]
- 34.Beebe DW, Rose D, Amin R. Attention, learning, and arousal of experimentally sleep-restricted adolescents in a simulated classroom. J Adolesc Health. 2010;47:523–5. doi: 10.1016/j.jadohealth.2010.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fallone G, Acebo C, Arnedt JT, Seifer R, Carskadon MA. Effects of acute sleep restriction on behavior, sustained attention, and response inhibition in children. Percept Mot Skills. 2001;93:213–29. doi: 10.2466/pms.2001.93.1.213. [DOI] [PubMed] [Google Scholar]
- 36.Wolfson AR, Carskadon MA, Acebo C, et al. Evidence for the validity of a sleep habits survey for adolescents. Sleep. 2003;26:213–6. doi: 10.1093/sleep/26.2.213. [DOI] [PubMed] [Google Scholar]
- 37.Radloff L. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:16. [Google Scholar]
- 38.Smith CS, Reilly C, Midkiff K. Evaluation of three circadian rhythm questionnaires with suggestions for an improved measure of morningness. J Appl Psychol. 1989;74:728. doi: 10.1037/0021-9010.74.5.728. [DOI] [PubMed] [Google Scholar]
- 39.Antony MM, Bieling PJ, Cox BJ, Enns MW, Swinson RP. Psychometric properties of the 42-item and 21-item versions of the Depression Anxiety Stress Scales in clinical groups and a community sample. Psychol Assess. 1998;10:176. [Google Scholar]
- 40.Drake C, Nickel C, Burduvali E, Roth T, Jefferson C, Pietro B. The pediatric daytime sleepiness scale (PDSS): sleep habits and school outcomes in middle-school children. Sleep. 2003;26:455–8. [PubMed] [Google Scholar]
- 41.Roberts RE, Roberts CR, Duong HT. Sleepless in adolescence: prospective data on sleep deprivation, health and functioning. J Adolesc. 2009;32:1045–57. doi: 10.1016/j.adolescence.2009.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lichstein KL, Durrence HH, Taylor DJ, Bush AJ, Riedel BW. Quantitative criteria for insomnia. Behav Res Ther. 2003;41:427–45. doi: 10.1016/s0005-7967(02)00023-2. [DOI] [PubMed] [Google Scholar]
- 43.Short MA, Gradisar M, Gill J, Camfferman D. Identifying adolescent sleep problems. PloS One. 2013;8:e75301. doi: 10.1371/journal.pone.0075301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Basner M, Dinges DF. Maximizing sensitivity of the psychomotor vigilance test (PVT) to sleep loss. Sleep. 2011;34:581–91. doi: 10.1093/sleep/34.5.581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Drummond SP, Bischoff-Grethe A, Dinges DF, Ayalon L, Mednick SC, Meloy MJ. The neural basis of the psychomotor vigilance task. Sleep. 2005;28:1059–68. [PubMed] [Google Scholar]
- 46.Fallone G, Carskadon MA. PVT performance among children in comparison to adults. Sleep. 2002;25:A433. Abstract Suppl. [Google Scholar]
- 47.Dorrian J, Rogers NL, Dinges DF. Psychomotor vigilance performance: A neurocognitive assay sensitve to sleep loss. In: Kushida C, editor. Sleep deprivation: clinical issues. New York: Marcel Dekker; 2005. [Google Scholar]
- 48.Wechsler D. Manual for the Wechsler Adult Intelligence Scale - Revised. New York, NY: Psychological Corporation; 1981. [Google Scholar]
- 49.Jamison RN, Schein JR, Vallow S, Ascher S, Vorsanger GJ, Katz NP. Neuropsychological effects of long-term opioid use in chronic pain patients. J Pain Symptom Manage. 2003;26:913–21. doi: 10.1016/s0885-3924(03)00310-5. [DOI] [PubMed] [Google Scholar]
- 50.Akerstedt T, Gillberg M. Subjective and objective sleepiness in the active individual. Int J Neurosci. 1990;52:29–37. doi: 10.3109/00207459008994241. [DOI] [PubMed] [Google Scholar]
- 51.Doran SM, Van Dongen HP, Dinges DF. Sustained attention performance during sleep deprivation: evidence of state instability. Arch Ital Biol. 2001;139:253–67. [PubMed] [Google Scholar]
- 52.Wu JC, Gillin JC, Buchsbaum MS, et al. The effect of sleep deprivation on cerebral glucose metabolic rate in normal humans assessed with positron emission tomography. Sleep. 1991;14:155–62. [PubMed] [Google Scholar]
- 53.Van Dongen HP, Baynard MD, Maislin G, Dinges DF. Systematic interindividual differences in neurobehavioral impairment from sleep loss: evidence of trait-like differential vulnerability. Sleep. 2004;27:423–33. [PubMed] [Google Scholar]
- 54.Davis AL, Avis KT, Schwebel DC. The effects of acute sleep restriction on adolescents' pedestrian safety in a virtual environment. J Adolesc Health. 2013;53:785–90. doi: 10.1016/j.jadohealth.2013.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jackson ML, Gunzelmann G, Whitney P, et al. Deconstructing and reconstructing cognitive performance in sleep deprivation. Sleep Med Rev. 2013;17:215–25. doi: 10.1016/j.smrv.2012.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Paterson JL, Dorrian J, Ferguson SA, et al. Changes in structural aspects of mood during 39-66 h of sleep loss using matched controls. Appl Ergon. 2011;42:196–201. doi: 10.1016/j.apergo.2010.06.014. [DOI] [PubMed] [Google Scholar]