Abstract
Background:
The purpose of this study was to describe the frequency of mechanical restraint use in an acute psychiatric ward and to analyze which variables may have significantly influenced the use of this procedure. Methods: This retrospective study was conducted in the Servizio Psichiatrico di Diagnosi e Cura (SPDC) of Modena Centro. The following variables of our sample, represented by all restrained patients admitted from 1-1-2005 to 31-12-2012, were analyzed: age, gender, nationality, psychiatric diagnoses, organic comorbidity, state and duration of admission, motivation and duration of restraints, nursing shift and hospitalization day of restraint, number of patients admitted at the time of restraint and institutional changes during the observation period. The above variables were statistically compared with those of all other non-restrained patients admitted to our ward in the same period. Results: Mechanical restraints were primarily used as a safety procedure to manage aggressive behavior of male patients, during the first days of hospitalization and night shifts. Neurocognitive disorders, organic comorbidity, compulsory state and long duration of admission were statistically significantly related to the increase of restraint use (p<.001, multivariate logistic regression). Institutional changes, especially more restricted guidelines concerning restraint application, were statistically significantly related to restraint use reduction (p<.001, chi2 test, multivariate logistic regression). Conclusion: The data obtained highlight that mechanical restraint use was influenced not only by clinical factors, but mainly by staff and policy factors, which have permitted a gradual but significant reduction in the use of this procedure through a multidimensional approach.
Keywords: Acute psychiatric ward, clinical factors, mechanical restraints, organizational factors, reduced application, retrospective analysis.
INTRODUCTION
During the last decades, health professionals have increasingly focused their attention on containment of violence in the workplace and, in the meantime, on safeguarding the safety, freedom and dignity of both patients and professionals [1-3].
At the beginning of the 70s in the USA, a new political strategy on violence in the health sector, the so-called “zero tolerance strategy”, indicated that no violent, antisocial or criminal behavior of patient against health professionals should remain unpunished [4]. Later, in 1999, in Britain, a campaign against violence in the health sector was launched in order to increase the professionals’ awareness on this issue and encourage them to report any violent act [5]. The World Health Organization has favored research on risk factors to find appropriate preventive strategies, since it considers violence a major health problem [6]. The National Institute of Occupational Safety and Health [7] has defined violence in the workplace “any act of physical assault, threatening behavior or verbal abuse occurring in the workplace” and the term “clinical violence” has been coined in order to indicate aggressive behavior from the patient against professionals in healthcare settings [8].
The containment of aggressive behavior is a frequent event in psychiatry settings, where violence are almost daily occurrences, as most studies reported [9-13]. Nurses who work in psychiatric wards are the professionals most exposed to this risk [14-16]. According to a recent survey conducted in a General Hospital in Modena, in the psychiatric ward, violent behavior is more frequent and more dangerous than in other medical settings; it is mostly shown by male patients affected by severe psychiatric conditions [17].
Aggressiveness is a multi-dimensional phenomenon, characterized by many cognitive and emotional processes, which is potentially present in all psychiatric disorders [11, 18]. It is not necessarily associated with a specific psychiatric disease, but it may represent an expression of personality traits as well as reactive frustrations encountered by the individual in his social context. Even intoxication by alcohol or other substances of abuse may be frequently associated with aggressive behavior [8].
The aggressiveness of the patient, more than other clinical situations, brings into play the psychological and professional skills of professionals. In a short span of time, professionals who manage the aggressive behavior of the patient have to understand the psychological reasons for disruptive behavior, to assess risk and possible consequences of this behavior and to take appropriate therapeutic measures, all in order to protect the safety of patient and others and, in the meantime, to preserve the dignity of patient. In this regard, professional has to take into account his feelings of intolerance, anger and frustration that always accompany the patient assault in order to avoid symmetric aggressive reaction toward the patient which could trigger an escalation of violence [19].
The choice of containment to be applied in case of violence is determined by the diagnostic and the prognostic assessment of clinical situations and risks [20-22]. Coercive measures such as seclusion, physical and mechanical restraint or forced medication are widely used in many western countries, although they constitute controversial clinical, ethical and legal issues [23-26]. The restraint is defined by the Health Care Financing Administration [27] as a physical or mechanical procedure [28, 29] to reduce the patient’s freedom of movement and action [19, 30]. Even physical confinement of the patient in a closed space (“seclusion room”) can be considered a restraining method [30].
Since it is universally recognized that the restraint methods restrict the freedom of individuals and should be used in cases of extreme danger [31], this procedure can be accepted only when all other therapeutic measures of containment of the patient in imminent danger to himself or others, fail.
In Italy, as in other countries [32-34], the coercive measures are not yet precisely regulated. The use of restraints is identified as a non-therapeutic tool which is not recommended by most Italian Mental Health Departments [35]. According to current Italian Laws, the application of physical restraint could be authorized in compulsory admission even if it should be reserved for exceptionally severe, not otherwise manageable, situations which can jeopardize the safety of the patient and/or others, identified as the so-called “state of necessity” (art. 54 of the Criminal Code), that requires a “statement of guardianship” from professionals (art. 40 of the Criminal Code).
In legislation on mental health, the interpretation of human rights differs by country. The debate on this topic reflects the dilemma of patients’ individual rights versus society interest in public safety [36].
The few systematic reviews about the effectiveness of this procedure carried out so far have shown no definitive conclusions, so the use of restraints is not supported by sufficient scientific evidence [37, 38].
The risks of physical and psychological consequences induced by restraint procedures, frequently reported in various studies, have contributed to its much more rigorous application [39]. Restraint application can be a traumatic experience for the patient and can favor regressive behavior and dependence on institutions, as frequently occurred in the past within asylums [19, 40].
Many direct and indirect physical injuries, as lung disease [41], deep vein thrombosis [42], nerve damage [43], ischemic lesions, and sudden death induced by restraint application have been recorded [44]. In the United Kingdom [45], the increase of physical injuries and deaths related to methods of restraint have drastically reduced its application. After some tragic deaths of restrained patients, many health agencies are currently oriented towards abolishing restraint use [46, 47].
In health care settings, many recent political and organizational strategies aimed at reducing restraint use have permitted not only the effective reduction of incidents reported by patients and professionals but also the decrease of violent assaults from patients [48, 49].
The purposes of this study were:
1) to describe the frequency of mechanical restraint use in an acute psychiatric ward during a long period of time characterized by many institutional changes;
2) to analyze which variables related to patients and/or staff may have significantly influenced the use of this procedure.
MATERIALS AND METHODOLOGY
This study, conducted in accordance with the principles of the Declaration of Helsinki and good clinical practice, was approved by a Human Subjects Review Committee. Written informed consent was obtained by all inpatients at the admission to our ward.
This retrospective study was conducted in the 15-bed public psychiatric ward, Servizio Psichiatrico di Diagnosi e Cura (SPDC) of Modena Centro, located in a General Hospital (NOCSAE of Az-USL-Modena), where patients (catchment area of about 250,000 people) affected by acute psychiatric disorders are hospitalized in voluntary or compulsory treatment, as required by Italian Law 180 [50].
Procedure of Mechanical Restraints
In our ward, mechanical restraint is carried out through the use of wrist restraints for both upper and lower limbs, which allow the immobilization of the patient on the bed in the supine position (in some cases abdominal belt of restraint is applied). The procedure can only be prescribed by a ward psychiatrist when other methods of containment have previously failed. The patient has to be constantly monitored by the nursing staff and the restraint application has to be re-evaluated by the ward psychiatrist every half hour. Date, time, duration of restraint, motivation, signature of the prescribing physician and the nurse concerning restraints have to be registered on the restraint log. During the period of restraint, drug therapy or psychological support are prescribed with the specific intent to resolve the condition that led to restraint use. This procedure is regulated by Department guidelines in accordance with regional recommendations that encourage its almost complete suppression.
Data Collection
Demographic and clinical data for all restrained in-patients admitted to our ward from 1-1-2005 to 31-12-2012 were retrospectively collected from medical charts. Data relative to physical restraints of inpatients were extrapolated from nurse restraint forms. All data were registered in a computerized database in order to be statistically analyzed.
We analyzed the following variables:
1. Restrained Patients (n=305):
• age, sex and nationality.
2. Hospitalizations with Restraint (n=560):
• psychiatric diagnosis at discharge, in accordance with the International Classification of Diseases, 9th Revision, Clinical Modification (ICD -9-CM), [51],
• presence of organic comorbidity,
• voluntary or compulsory state of hospitalization according to Italian Law “180”,
• length of hospitalization (days).
3. Characteristics of Mechanical Restraints (n=1224):
• reason for use of restraints divided into the following categories according to the most frequent reasons registered in our ward and the literature indications [52]: A) control of dangerous, violent, or aggressive behavior; B) prevention of injury or necessity of urgent therapy,
• frequency of restraint use in the nursing shifts (morning, from 7:00 a.m. to 1:00 p.m.; afternoon, from 1:00 p.m. to 8:00 p.m.; night, from 8:00 p.m. to 7:00 a.m.),
• duration of restraints (hrs),
• day of restraint use during hospitalization,
• number of all patients hospitalized in our ward at the moment of restraint use.
• Institutional changes in SPDC during the observation period: in 2008, 3 of 5 ward psychiatrists were replaced; in 2009, nurses per shift increased from three to four units and SPDC was moved to a larger and more comfortable ward; in 2011, new more restricted guidelines concerning restraint application were implemented by the new director of Mental Health and Pathological Addiction Department. The nurse staff and the nurse matron remained almost unchanged during the observation period. All staff was involved in many audits, work conferences and internal ward debates dedicated to this topic over the 8-year period.
All mechanical restraints were always combined with sedative therapy in order to resolve the situations which required the restraint application.
No restraint accidents for patients or for professionals were registered during the observation period.
Statistical Analysis
The variables of “restrained patients” and “hospitalizations with restraint”, were compared with those of all other non-restrained inpatients and hospitalizations in SPDC-Modena Centro during the observation period (chi2, t-test, multivariate logistic regression) [53, 54].
The characteristics of restraints were analyzed and correlated with the variables collected (chi2 test, multivariate logistic regression, Cox model of survival analysis, Kaplan Meier) curve [54-56].
Statistical analysis was processed by the statistical program of STATA 12 [57].
RESULTS
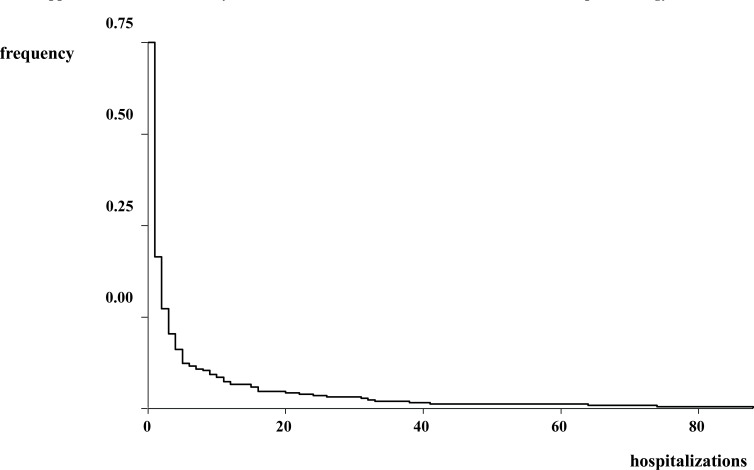
Our sample of restrained patients (n=305) was mostly represented by males (61.97%), Italians (76.72%), with a mean age of 46 years (Table 1). The mechanical restraints recorded (n=1224) were applied 4.01 times per patient on average, mainly motivated by the need to control aggressive behavior (64.60%), with the duration of 6 hours on average, more frequently applied during the night shifts (42.48%) and in the first days of hospitalization (Table 2 and Fig. 1). We highlighted that patients with altered state of consciousness were more frequently restrained during night shifts (Pearson chi2 = 17.9312, p<.001) and patients with lucid consciousness were more frequently restrained due to aggressive behavior (Pearson chi2 = 25.9860, p<.001).
Table 1.
Demographic Data of restrained and non-restrained patients (N=2660) in SPDC-modena centro (from 1-1-2005 to 31-12-12).
| Demographic Variables | Restrained Patients | Non-restrained Patients | |
|---|---|---|---|
| Gender N (%) | Males | 189 (7%) | 1211 (46%) |
| Females | 116 (4%) | 1144 (43%) | |
| Nationality N (%) | Italian | 234 (9%) | 1904 (72%) |
| European Union | 10 (0.2%) | 79 (2.8%) | |
| Extra-European Union | 61 (2%) | 363 (14%) | |
| Age (years) | mean±SD | 45.79 ±18.75 | 44.79±16.45 |
Table 2.
Characteristics of mechanical restraint (N=1224) in SPDC-modena centro (from 1-1-2005 to 31-12-12).
| Reasons for Restraint Application | N | % |
|---|---|---|
| Control of Dangerous, Violent or Aggressive Behavior | 791 | 64.60% |
| Prevention of Injury or Necessity of Urgent Therapy | 433 | 35.40% |
| Nurse Shifts | N | % |
| MORNING (hrs 7-13) | 228 | 18.63% |
| AFTERNOON (hrs 13-20) | 302 | 24.67% |
| NIGHT (hrs 20-7) | 520 | 42.48% |
| More than one shift | 174 | 14.22% |
| Duration of Restraint (hours) mean±SD | 6.12±5.08 | |
| Day of Mechanical Restraint median | 6th day of hospitalization | |
| Number of Hospitalized Patients at the Moment of Restraint Application mean±SD | 19.61±5.79 | |
Fig. (1).
Mechanical restraint application and day of hospitalization.
At the moment of restraint application, 19 patients on average were hospitalized in our ward, which should admit no more than 15 patients, as required by Italian 180 Law [50].
Over the 8-year observation period, we reported 2.19 restraints on average in 560 hospitalizations with restraints. The most frequent psychiatric discharge diagnosis was “schizophrenia and other psychoses” (31.61%), which was the most frequent diseases among all patients admitted in our wards (Table 3). The second most frequent psychiatric diagnosis was represented by “organic psychosis” (19.46%), followed by the category of “bipolar disorder” (14.11%). In hospitalizations with restraint, both organic comorbidity (p<.001, chi-square) and compulsory state of admission (p<.001, chi-square) were more frequently recorded (Table 4). The average length of hospitalizations with restraint was statistically significantly higher than other hospitalizations in the same period of time (24.90 ± 35.49 vs. 11.35 ± 12.60, t =-17.8251, p<.001, t-test) (Table 4).
Table 3.
Psychiatric Diagnosis related to hospitalizations with and without mechanical restraints from 1-1-2005 to 31-12-20012 (N=4835).
| Psychiatric Diagnosis (ICD-9-CM) | Hospitalization without Mechanical Restraints | Hospitalization with Mechanical Restraints | ||||
|---|---|---|---|---|---|---|
| I Psychiatric Diagnosis N | II Psychiatric Diagnosis N | III Psychiatric Diagnosis N | I Psychiatric Diagnosis N | II Psychiatric Diagnosis N | III Psychiatric Diagnosis N | |
| Schizophrenia and other psychotic disorders (295-295.9) | 1584 | 40 | 6 | 177 | 8 | - |
| Organic psychoses (290-294.9) | 276 | 47 | 17 | 109 | 17 | 19 |
| Bipolar disorders (296-296.9) | 720 | 29 | 9 | 79 | 6 | - |
| Neurotic disorders (300-300.9) | 578 | 140 | 19 | 45 | 11 | 4 |
| Personality disorders (301-301.9) | 577 | 286 | 37 | 64 | 29 | 5 |
| Alcohol and other substance abuse and dependence (303-305.9) | 431 | 528 | 150 | 62 | 54 | 9 |
| Mental retardation (317-319) | 85 | 69 | 9 | 18 | 11 | - |
| Others | 24 | 33 | 10 | 6 | 1 | - |
Table 4.
Variables related to hospitalizations with and without mechanical restraints from 1-1-2005 to 31-12-20012 (N=305).
| Hospitalizations without Mechanical Restraints | Hospitalizations with Mechanical Restraints | ||
|---|---|---|---|
| Organic Comorbidity | Absent N (%) | 3348 (69%) | 386 (8%) |
| Present N (%) | 927 (19%) | 174 (4%) | |
| State of Admission | Compulsory admissions N (%) | 3361 (70%) | 308 (6%) |
| Voluntary admissions N (%) | 914 (19%) | 252 (5%) | |
| Length of Hospitalization | (days) mean±SD | 11.36±12.60* | 24.9 ±35.49** *vs**, t-test, p<0.001 |
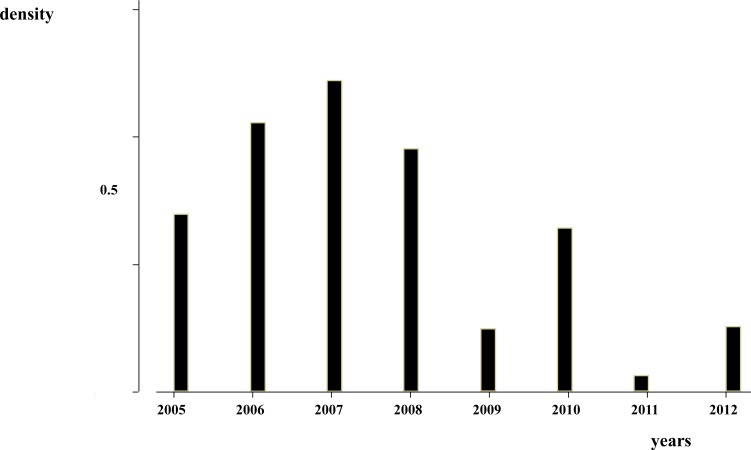
The number of restraints per year progressively declined during the 8-year period (Fig. 2). The reduction of restraints was statistically significantly related to all the institutional changes that occurred in the observation period: the change of medical staff in 2008 (Pearson chi2 = 157.0559, p<.001), the increase in nurses per shift and the ward relocation in 2009 (Pearson chi2 = 112.0902, p<.001) and the implementation of more restricted guidelines for restraint application in 2011 (Pearson chi2 = 157.0559, p<.001).
Fig. (2).
Number of restraints in the 8-year period of observation.
The comparison between hospitalizations with and without restraint showed that the following variables were statistically significantly related to restraint use (multivariate logistic regression) (Table 5):
Table 5.
The variables statistically significantly related to hospitalizations with mechanical restraints (multivariate logistic regres-sion).
| Variables | Odds Ratio | Standard Error | Probability | Confidence Interval (95%) |
|---|---|---|---|---|
| Gender: Female | 0.71 | 0.07 | p<.001 | 0.580-0.870 |
| Nazionality: Extra-European | 1.75 | 0.25 | p<.001 | 1.323-2.307 |
| I Psychiatric Diagnosis (ICD-9-CM) | ||||
| Schizophrenia and other psychoses | 0.26 | 0.12 | p<.005 | 0.100-0.652 |
| Bipolar disorders | 0.34 | 0.16 | p<.05 | 0.133-0.870 |
| Neurotic disorders | 0.28 | 0.14 | p<.01 | 0.107-0.728 |
| Personality disorders | 0.36 | 0.18 | p<.05 | 0.137-0.940 |
| II Psychiatric Diagnosis (ICD-9-CM): Organic psychoses | 2.57 | 0.94 | p<.01 | 1.252-5.272 |
| III Psychiatric Diagnosis (ICD-9-CM): Organic psychoses | 5.15 | 2.06 | p<.001 | 2.354-11.281 |
| Organic Comorbidity: Present | 1.47 | 0.17 | p<,001 | 1.171-1.852 |
| State of Admission: TSO | 2.92 | 0.31 | p<.001 | 2.368-3.610 |
| Length of Hospitalization (days) | 1.03 | 0 | p<.001 | 1.025-1.038 |
| Institutional Changes | ||||
| Medical staff replacement (2008) | 0.45 | 0.054 | p<.001 | 0.3526872-0.5662116 |
| More restricted guidelines for restraint application (2011) | 0.22 | 0.050 | p<.001 | 0.1369291-0.341403 |
- female gender (p<.001), the diagnosis of “schizophrenia and other psychoses” (p<.005), “bipolar disorder” (p<.05), “neurotic disorders” (p<.01) and “personality disorders” (p<.05) were protective factors;
- extra-European nationality (p<.001), “organic psychoses”, as second and third psychiatric diagnosis (p<.01, p<.001), organic comorbidity (p<.001), compulsory state of hospitalization (p<.001), and long duration of hospitalization (p<.001) were risk factors for restraint application;
- among the institutional modifications, only the replacement of medical staff (p<.001) and the implementation of more restricted guidelines for restraint application (p<.001) represented protective factors.
The correlations between restraints and the selected variables were further confirmed by nested multiple logistic regression (Table 6) [58].
Table 6.
The variables statistically significantly related to hospitalizations with mechanical restraints (nested multivariate logistic regression).
| Variables | F | Pr > F | R2 | Change in R2 |
|---|---|---|---|---|
| Patients with >1 hospitalization | 27.18 | 0.0000 | 0.0056 | - |
| Gender | 5.90 | 0.0152 | 0.0073 | 0.0012 |
| Nazionality | 14.85 | 0.0001 | 0.0103 | 0.0030 |
| I Psychiatric Diagnosis (ICD-9-CM) | 5.71 | 0.0169 | 0.0115 | 0.0012 |
| II Psychiatric Diagnosis (ICD-9-CM) | 5.46 | 0.0195 | 0.0126 | 0.0011 |
| Organic Comorbidity | 22.71 | 0.0000 | 0.0178 | 0.0046 |
| State of Admission: | 153.66 | 0.0000 | 0.0481 | 0.0304 |
| Length of Hospitalization (days) | 240.01 | 0.0000 | 0.0933 | 0.0452 |
| Medical Staff Replacement (2008) | 98.66 | 0.0000 | 0.1115 | 0.0182 |
| More Restricted Guidelines for Restraint Application (2011) | 27.24 | 0.0000 | 0.1165 | 0.0050 |
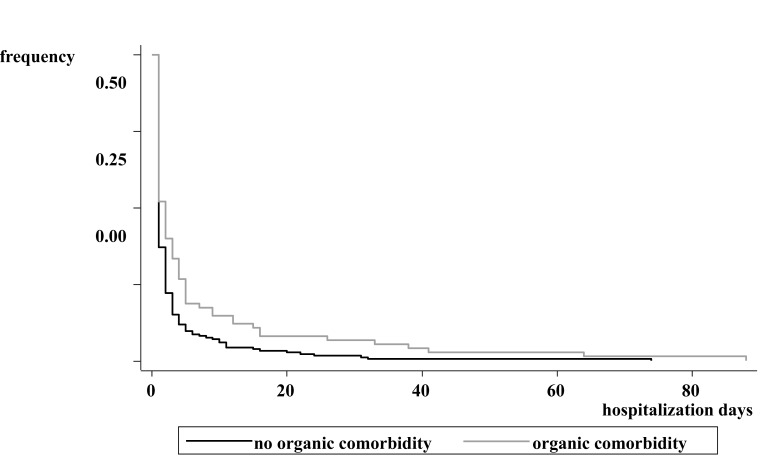
The presence of organic comorbidity was the only variable responsible for postponing restraint application during hospitalization (Fig. 3) (Cox model, p<.05).
Fig. (3).
The presence of organic comorbidity favored postponed restraint application during hospitalization (Cox model, p<.05).
DISCUSSION
The data of this retrospective analysis overlap those of the literature: mechanical restraints were most frequently applied to control aggressive behavior in male patients affected by schizophrenia and other psychoses [12, 13, 18, 48].
Our study highlights that female gender can be a protective factor in restraint application since males were more frequently restrained than females, probably due to greater aggressiveness, genetically and culturally conditioned [13]. Restrained patients were more frequently Italian people as they were the majority of patients admitted to our ward, but non-European patients showed statistically significant risk of being restrained: this data may indicate the difficulty in treating people who differ culturally and speak another mother-tongue language in acute severe psychiatric conditions [59].
The highest frequency of restraint in the group of patients with “schizophrenia and other psychoses” can be explained by the highest frequency presence in our ward of patients suffering from this pathology, highly prevalent in the general population, between 0.3 and 0.7% [60]. Otherwise, the organic psychosis was the only pathology which favored the risk of restraint application according to our statistical analysis. This data shows that the application of restraint in our ward was mainly dictated by the need to avoid vital risks in severe diseases, poorly responsive to different modalities of containment.
Mechanical restraints were mainly applied during the early days of hospitalization, as urgent and not routine procedures, with the exception of the cases characterized by organic comorbidity, which induced the application of restraints throughout the whole period of hospitalization.
The primary reason for restraint use was the need to control aggressive behavior, probably because the aggressiveness, common symptom of many psychiatric disorders, was the main cause of hospitalization [61].
Therefore, according to our data, we can emphasize that the use of mechanical restraint can be considered a marker of clinical severity and complexity. In fact, patients involuntarily admitted due to hostility and lack of cooperation, and patients hospitalized longer due to many critical issues reporting discharge were more frequently restrained [62].
The more frequent restraint application during the night shift (42.48%) could be explained not only by some clinical variables (circadian rhythms, exacerbation of mental confusion during the night, etc.) [63], but also by different staff work organization (reduced nurses, psychiatrists and therapeutic activities, etc.). During morning shifts, when the team was complete and dedicates to more inpatient health activities, reduced numbers of restraints were applied in comparison to other shifts. This result indirectly suggests that the highest number of professionals and the presence of all members of staff can reduce the use of this measure probably due to both the inhibition of patient aggressive behaviors and the reinforcement of staff reassurance [64].
During the application of restraints, the mean number of inpatients was greater than the maximum number permitted by law, suggesting that overcrowding could be a risk factor for the use of restraint, probably due to the increase of conflicts within an acute psychiatric environment, as noted by other researchers [65, 66]. In Italy [67], as in other countries [23], a community-based therapeutic approach has led to a decrease of beds in psychiatric hospitals, resulting in a potential increase of patients affected by severe psychiatric disorders admitted to acute psychiatric public wards (approximately 20% of patients were compulsorily admitted to SPDC - Modena Centro during the observation period of this study).
The analysis of restraint use over the 8-year observation period highlights its progressive reduction, which was statistically significantly related to all structural and organization improvements that took place during those years, as reported in literature [68]. Nevertheless, in accordance with our statistical analysis, we have to underline that only the replacement of medical staff and the promotion of more restrictive guidelines on restraint use were the variables statistically significantly related to the reduction of restraint application. This last result leads us to speculate that the modification of ward strategies can more dramatically influence the application of this procedure, which always arises from the interaction between patients and professionals [69] The reduced application of mechanical restraints did not foster any accident for patients or professionals and permitted a less restrictive and more respectful treatment. We have to underline that institutional innovations such as the closure of asylums have dramatically changed the manifestations of psychiatric diseases. So, we can infer that a different modality to deal with violence from patients could in the meantime favor more adapted and less aggressive behavior and, paradoxically, reduce the risk of dependence on institutions. Finally, we suggest that, as for all psychological therapies therapeutic, the non-symmetric behavior of therapists and institutions could represent the more appropriate and effective answer also for treating patient violence.
Despite the limitations related to the retrospective methods, our study helps to better identify the institutional and organizational factors that, in an acute psychiatric ward, reduced the use of the restraint procedure which is potentially burdened by negative physical and psychological consequences for patients and professionals [70, 71]. As indicated by the latest research on this topic [8], the limitation or elimination of restraint use could reduce not only physical and psychological damage reported by restrained patients, but also incidents reported by health professionals, and so increasing their job satisfaction and reducing the risk of their “burn-out”.
CONCLUSION
We can conclude that in our ward, mechanical restraints were primarily applied as an extreme tool to contain aggressiveness in order to avoid imminent risks in the most severe and complex clinical situations. Restraint use was conditioned not only by clinical factors but mainly by organizational factors related to staff, structure and health guidelines which, over an 8-year period, allowed its significant reduction. Only a multidimensional approach [72-74] could face out almost completely this procedure since violence is a complex and multi-faceted phenomenon [75]. Other studies aimed to explore the relationship between patients and staff are necessary to better identify innovative strategies for reducing violence in health settings [76].
ACKNOWLEDGEMENTS
Declared none.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
REFERENCES
- 1.Bowers L, Nijman J, Allan T, Simpson A, Warren J, Turner L. Prevention and management of aggression training and violent incidents on, U.S acute psychiatric wards. Psychiatr Serv. 2006;57:1022–6. doi: 10.1176/ps.2006.57.7.1022. [DOI] [PubMed] [Google Scholar]
- 2.Winstanley S, Whittington R. Violence in a general hospital comparison of assailant and other assault-related factors on accident and emergency and inpatients wards. Acta Psychiatr Scand. 2002;106:144–7. doi: 10.1034/j.1600-0447.106.s412.31.x. [DOI] [PubMed] [Google Scholar]
- 3.Winstanley S, Whittington R. Aggression towards health care staff in a UK general hospital variation among professions and departments. J Clin Nurs. 2004;13:3–10. doi: 10.1111/j.1365-2702.2004.00807.x. [DOI] [PubMed] [Google Scholar]
- 4.VandenBos GR, Bulatao E. Workpalce violence its scope and the issues the Violence in on the job. . In: VandenBos GR, Bulatao E, editors. American Psychological Association . Washington, DC.: 1996. [Google Scholar]
- 5.Health Service Circular NHS Zero Tolerance Zone Campaign Tackling Violence in Primary Care, Ambulance, Mental Health, and Community Settings. London Department of Health. 1999 [Google Scholar]
- 6.Krug EG, Dahlberg LL, Mercy JA , et al. World report on violence and health Geneva, World Health Organization 2002. Available at http //whqlibdoc.who.int/publications/2002/9241545615_eng.pdf.
- 7.National Institute for Occupational Safety and Health (NIOSH) Violence Occupational Hazards in Hospitals Columbia Parkway Cincinnati, DHHS, 2002. Available at http //www.cdc.gov/niosh/ pdfs/2002-101.pdf.
- 8.Duxbury J, Whittington R. Causes and management of patient aggression and violence staff and patient perspectives. J Adv Nurs. 2005;50:469–78. doi: 10.1111/j.1365-2648.2005.03426.x. [DOI] [PubMed] [Google Scholar]
- 9.Foster C, Bowers L, Nijman H. Aggressive behavior on acute psychiatric wards prevalence, severity and management. J Adv Nurs. 2007;58:140–9. doi: 10.1111/j.1365-2648.2007.04169.x. [DOI] [PubMed] [Google Scholar]
- 10.Gadon L, Cooke DJ, Johnstone L. Situational variables and institutional violence A systematic review of the literature. Clin Psychol Rev. 2006;26:515–34. doi: 10.1016/j.cpr.2006.02.002. [DOI] [PubMed] [Google Scholar]
- 11.Link BG, Stueve T. Evidence bearing on mental illness and possible causes of violent behavior. Epidemiol Rev. 1995;17:172–81. doi: 10.1093/oxfordjournals.epirev.a036173. [DOI] [PubMed] [Google Scholar]
- 12.Goldstein AM, Monahan J, editors. New York : New York John Wiley & Sons Press; 2003. Violence risk assessment in Handbook of Psychology. [Google Scholar]
- 13.Nijman HLI. A model of aggression in psychiatric hospitals. Acta Psychiatr Scand. 2002;106:142–3. doi: 10.1034/j.1600-0447.106.s412.30.x. [DOI] [PubMed] [Google Scholar]
- 14.Peek-Asa C, Casteel C, Allareddy V , et al. Workplace violence prevention programs in psychiatric units and facilities. Arch Psychiatr Nurs. 2009;23:166–76. doi: 10.1016/j.apnu.2008.05.008. [DOI] [PubMed] [Google Scholar]
- 15.Islam SS, Edla SR, Mujuru P, Doyle EJ, Ducatman AM. Risk factors for physical assault State managed worker's compensation experience. Am J Prev Med. 2003;25:31–7. doi: 10.1016/s0749-3797(03)00095-3. [DOI] [PubMed] [Google Scholar]
- 16.Nan E, Albini E, Zoni S, Lucchini R. Misurazione degli episodi di violenza nei lavoratori della sanità: un metodo di indagine. G Ital Med Lav Ergon. 2007;29:362–4. [PubMed] [Google Scholar]
- 17.Ferri P, Reggiani F, Di Lorenzo R. I comportamenti aggressivi nei confronti dello staff in tre differenti aree sanitarie. Prof Inferm. 2011;64:143–50. [PubMed] [Google Scholar]
- 18.Steinert T. Prediction of inpatient violence. Acta Psychiatr Scand. 2002;106:133–41. doi: 10.1034/j.1600-0447.106.s412.29.x. [DOI] [PubMed] [Google Scholar]
- 19.Di Lorenzo R, Baraldi S, Ferrara M, Mimmi S, Rigatelli M. Physical restraints in an italian psychiatric ward clinical reasons and staff organization problems. Perspect Psychiatr Care. 2012;48:95–107. doi: 10.1111/j.1744-6163.2011.00308.x. [DOI] [PubMed] [Google Scholar]
- 20.National Collaborating Centre for Nursing and Supportive Care (UK) Violence The short term management of disturbed/violent behavior in in-patient psychiatric settings and emergency departments. London Royal College of Nusing. 2005 [PubMed] [Google Scholar]
- 21.Winship G. Further thoughts on the process of restraint. J Psychiatr Ment Health Nurs. 2006;13:55–60. doi: 10.1111/j.1365-2850.2006.00913.x. [DOI] [PubMed] [Google Scholar]
- 22.Cantaro P, Scarlata S. Raccomandazione per prevenire gli atti di violenza a danno degli operatori sanitari Roma, Ministero della Salute, 2007. Available at http //www.salute.gov.it/imgs/ C_17_pubblicazioni_721_allegato.pdf.
- 23.Steinert T, Lepping P, Bernhardsgrütter R , et al. Incidence of seclusion and restraint in psychiatric hospitals A literature review and survey of international trends. Soc Psychiatry Psychiatr Epidemiol. 2010;45:889–97. doi: 10.1007/s00127-009-0132-3. [DOI] [PubMed] [Google Scholar]
- 24.O'Grady JC. Commentary A British perspective on the use of restraint and seclusion in correctional mental health care. J Am Acad Psychiatry Law. 2007;35:439–43. [PubMed] [Google Scholar]
- 25.Jarrett M, Bowers L, Simpson A. Coerced medication in psychiatric inpatient care literature review. J Adv Nurs. 2008;64:538–48. doi: 10.1111/j.1365-2648.2008.04832.x. [DOI] [PubMed] [Google Scholar]
- 26.Kallert TW. Coercion in psychiatry. Curr Opin Psychiatry. 2008;21:485–9. doi: 10.1097/YCO.0b013e328305e49f. [DOI] [PubMed] [Google Scholar]
- 27.Weick MD. Eye on elders from FDA nurses physical restraints an FDA update. Am J Nurs. 1992;92:74–80. [PubMed] [Google Scholar]
- 28.Stubbs B, Leadbetter D, Paterson B, Yorston G, Knight C, Davis S. Physical intervention a review of the literature on its use, staff and patient views, and the impact of training. J Psychiatr Ment Health Nurs. 2009;16:99–105. doi: 10.1111/j.1365-2850.2008.01335.x. [DOI] [PubMed] [Google Scholar]
- 29.Evans D, Wood J, Lambert L. A review of physical restraint minimization in the acute and residential care settings. J Adv Nurs. 2002;40:616–25. doi: 10.1046/j.1365-2648.2002.02422.x. [DOI] [PubMed] [Google Scholar]
- 30.Husum TL, Bjørngaard JH, Finset A, Ruud T. A cross-sectional prospective study of seclusion, restraint and involuntary medication in acute psychiatric wards patient, staff and ward characteristics. BMC Health Serv Res. 2010;6:10–89. doi: 10.1186/1472-6963-10-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Petrini C. Ethical considerations for evaluating the issue of physical restraint in psychiatry. Ann Ist Super Sanit . 2013;49:281–5. doi: 10.4415/ANN_13_03_08. [DOI] [PubMed] [Google Scholar]
- 32.Hellerstein DJ, Staub AB, Lequesne E. Decreasing the use of restraint and seclusion among psychiatric inpatients. J Psychiatr Pract. 2007;13:308–17. doi: 10.1097/01.pra.0000290669.10107.ba. [DOI] [PubMed] [Google Scholar]
- 33.Steinert T, Lepping P. Legal provisions and practice in the management of violent patients.A case vignette study in 16 European countries. Eur Psychiatry. 2009;24:135–41. doi: 10.1016/j.eurpsy.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 34.Lay B, Nordt C, Rössler W. Variation in use of coercive measures in psychiatric hospitals. Eur Psychiatry. 2011;26:244–51. doi: 10.1016/j.eurpsy.2010.11.007. [DOI] [PubMed] [Google Scholar]
- 35.Fascio V. La contenzione fisica reclusione o nursingκ. Available at http //www.infermierionline.net/index.php?option=com_content&view=article&id=726: la-contenzione-fisica-in-psichiatria-reclusione-o-nursing&catid=144: psichiatria&Itemid=53.
- 36.Janssen WA, van de Sande R, Noorthoorn EO , et al. Methodological issues in monitoring the use of coercive measures. Int J Law Psychiatry. 2011;34:429–381. doi: 10.1016/j.ijlp.2011.10.008. [DOI] [PubMed] [Google Scholar]
- 37.Sailas E, Fenton M. Seclusion and restraint for people with serious mental illnesses. Cochrane Database Syst Rev. 2000;2:CD001163. doi: 10.1002/14651858.CD001163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Muralidharan S, Fenton M. Containment strategies for people with serious mental illness. Cochrane Database Syst Rev. 2006;3:CD002084. doi: 10.1002/14651858.CD002084.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Food and drug administration.FDA safety alert Potential hazards with restraint devices Rockville MD US. Department of Health and Human Services. 1992 [Google Scholar]
- 40.Frueh BC, Knapp RG, Cusack KJ , et al. Special Section on Seclusion and Restraint Patients' reports of traumatic or harmful experiences within the psychiatric setting. Psychiatr Serv. 2005;56:1123–33. doi: 10.1176/appi.ps.56.9.1123. [DOI] [PubMed] [Google Scholar]
- 41.Parkes J. Sudden death during restraint Do some positions affect lung functionκ. Med Sci Law. 2008;48:137–41. doi: 10.1258/rsmmsl.48.2.137. [DOI] [PubMed] [Google Scholar]
- 42.Dickson BC. Fatal thromboembolic disease A risk in physically restrained psychiatric patients. J Forensic Leg Med. 2009;16:284–6. doi: 10.1016/j.jflm.2008.12.008. [DOI] [PubMed] [Google Scholar]
- 43.Scott TF, Gross JA. Brachial plexus injury due to vest restraint. N Engl J Med. 1989;320:598. doi: 10.1056/NEJM198903023200918. [DOI] [PubMed] [Google Scholar]
- 44.Parkes J. A review of the literature on positional asphyxia as a possible cause of sudden death during restraint. Br J Forensic Pract. 2002;4:24–30. [Google Scholar]
- 45.Independent inquiry into the death of David Bennet Norfolk, Suffolk and Cambridgeshire Strategic Health Authority, 2004. Available at http //image.guardian.co.uk/sys-files/Society/documents/ 2004/02/12/Bennett.pdf.
- 46.Gaskin CJ, Elsom SJ, Happel B. Interventions for reducing the use of seclusion in psychiatric facilities Review of the literature. Br J Psychiatry. 2007;191:298–303. doi: 10.1192/bjp.bp.106.034538. [DOI] [PubMed] [Google Scholar]
- 47.Barton SA. Achieving restraint-free on an inpatient behavioral health unit. J Psychosoc Nurs Ment Health Serv. 2009;47:34–40. doi: 10.3928/02793695-20090101-01. [DOI] [PubMed] [Google Scholar]
- 48.Flannery RB, Rachlin S, Walker A. Characteristics of repetitively assaultive patients ten year analysis of the Assaulted Staff Action Program (ASAP). Int J Emerg Ment Health. 2002;72:59–69. [PubMed] [Google Scholar]
- 49.Forster PL, Cavness C, Phelps MA. Staff training decreases use of seclusion and restraint in an acute psychiatric hospital. Arch Psychiatr Nurs. 1999;13:269–71. doi: 10.1016/s0883-9417(99)80037-5. [DOI] [PubMed] [Google Scholar]
- 50.Legge 13 Maggio 1978 n 180: Accertamenti e trattamenti sanitari volontari e obbligatori, Gazzetta Ufficiale, 16: maggio 1978 n133. Available at http //www.salute.gov.it/imgs/ C_17_normativa_888_allegato.pdf.
- 51.Ministero del Lavoro, della Salute e delle.Politiche Sociali Classificazione delle malattie e dei traumaismi degli interventi chirurgici e delle procedure diagnostiche e terapeutiche Versione italiana della ICD-9-CM ''International Classification of Diseases-9th revision-Clinical Modification'' 2007. Roma Istituto Poligrafico e Zecca dello Stato. 2008.
- 52.Kaltiala-Heino R, Tuohimaki G, Korkeila J, Lehtinen V. Reasons for using seclusion and restraint in psychiatric inpatient care. Int J Law Psychiatry. 2003;26:139–49. doi: 10.1016/s0160-2527(02)00210-8. [DOI] [PubMed] [Google Scholar]
- 53.Siegel S, Castellan JN, editors. Boston: The McGraw-Hill International Book Company; 1988. Nonparametric statistics for the behavioral sciences. [Google Scholar]
- 54.Berk RA. A Constructive Critique. Pennsylvania Sage Publicaions: 2004. Regression Analysis. [Google Scholar]
- 55.Cox DR, Oakes D, editors. London Chapman and Hall. 1984. Analysis of Survival Data. [Google Scholar]
- 56.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Statistical Association. 1958;53:457–81. [Google Scholar]
- 57.Stata Statistical Software Release 12.: College Station TX Stata Corp LP.; 2011. Stata Version 12. [Google Scholar]
- 58.Acock AC, editor. 3rd ed. Collge Station Texas: 2010. A gentle introduction to STATA, . [Google Scholar]
- 59.Bacon L, Bourne R, Oakley C , et al. Immigration policy implications for mental health services. Adv Psychiatr Treat. 2010;16:124–32. [Google Scholar]
- 60. 5th ed. Washington DC.: 2013. American Psychiatric Association, Diagnostic and Statistical Manual of Mental Disorders, [Google Scholar]
- 61.Biancosino B, Delmonte S, Grassi L , et al. Violent behavior in acute psychiatric inpatient facilities a National survey in Italy. J Nerv Ment Dis. 2009;197:772–78. doi: 10.1097/NMD.0b013e3181bb0d6b. [DOI] [PubMed] [Google Scholar]
- 62.Di Lorenzo R, Formicola V, Carra E, Piemonte C, Ferri P. Risk factors for long-stay in an Italian acute psychiatric ward a 7-year retrospective analysis. J Nurs Educ Pract. 2014;4:68–80. [Google Scholar]
- 63.Wulff K, Gatti S, Wettstein JG, Foster RG. Sleep and circadian rhythm disruption in psychiatric and neurodegenerative disease. Nat Rev Neurosci. 2010;11:589–99. doi: 10.1038/nrn2868. [DOI] [PubMed] [Google Scholar]
- 64.Wynn R. Staff's attitudes to the use of restraint and seclusion in a Norwegian university psychiatric hospital. Nord J Psychiatry. 2003;7:453–9. doi: 10.1080/08039480310003470. [DOI] [PubMed] [Google Scholar]
- 65.Ng B, Kumar S, Ranclaud M, Robinson E. Ward crowding and incidents of violence on an acute psychiatric inpatient unit. Psychiatr Serv. 2001;52:521–5. doi: 10.1176/appi.ps.52.4.521. [DOI] [PubMed] [Google Scholar]
- 66.Virtanen M, Vahtera J, David Batty G , et al. Overcrowding in psychiatric wards and physical assaults on staff Data-linked longitudinal study. Br J Psychiatry. 2011;198:149–55. doi: 10.1192/bjp.bp.110.082388. [DOI] [PubMed] [Google Scholar]
- 67.Bersani G. The Italian Law 180 thirty years after from the unmet needs of sick people and families to the duty of a critical reflection. Ann Ist Super Sanit . 2009;45:27–32. [PubMed] [Google Scholar]
- 68.van der Schaaf PS, Dusseldorp E, Keuning FM, Janssen WA, Noorthoorn EO. Impact of the physical environment of psychiatric wards on the use of seclusion. Br J Psychiatry. 2013;202:142–9. doi: 10.1192/bjp.bp.112.118422. [DOI] [PubMed] [Google Scholar]
- 69.Winston PA, Morelli P, Bramble J, Friday A, Sanders JB. Improving patient care through implementation of nurse-driven restraint protocols. J Nurs Care Qual. 1999;13:32–46. doi: 10.1097/00001786-199908000-00005. [DOI] [PubMed] [Google Scholar]
- 70.Needham I, Abderhalden C, Halfens RJG, Fisher JE, Dassen T. Non-somatic effects of patient aggression on nurses a systematic review. J Adv Nurs. 2005;49:283–96. doi: 10.1111/j.1365-2648.2004.03286.x. [DOI] [PubMed] [Google Scholar]
- 71.Fornes J, Cardoso M, Castello JM, Gili M. Psychological harassment in the nursing place an observational study. Arch Psychiatr Nurs. 2011;25:185–94. doi: 10.1016/j.apnu.2010.08.008. [DOI] [PubMed] [Google Scholar]
- 72.Paterson B, Leadbetter D, Miller G. Beyond zero tolerance, a varied approach to workplace violence. Br J Nurs. 2005;14:746–53. doi: 10.12968/bjon.2005.14.15.18598. [DOI] [PubMed] [Google Scholar]
- 73.Huizing AR, Hamers JPH, de Jonge J, Candell M, Berger MP. Organizational determinants of the use of physical restraints a multilevel approach. Soc Sci Med. 2007;65:924–33. doi: 10.1016/j.socscimed.2007.04.030. [DOI] [PubMed] [Google Scholar]
- 74.Georgieva I, Mulder CL, Noorthoorn E. Reducing seclusion through involuntary medication a randomized clinical trial. Psychiatry Res. 2013;30:48–53. doi: 10.1016/j.psychres.2012.08.002. [DOI] [PubMed] [Google Scholar]
- 75.Callaghan P, Oud N, Bjorngaard JH, Jones D. Violence in the Workplace an endemic, but not an inevitable problem of 21st century healthcare delivery Proceedings of the 8th European Congress on Violence in Clinical Psychiatry, Ghent, Belgium, 23-26/10/2013. Amsterdam Kavanah wingeloo & Oud Consultancy. 2013 [Google Scholar]
- 76.Stratmann D, Vinson MH, Magee R, Hardin SB. The effects of research on clinical practice The use of restraints. Appl Nurs Res. 1997;19:39–43. doi: 10.1016/s0897-1897(97)80078-x. [DOI] [PubMed] [Google Scholar]