Abstract
Background
Evidence suggests that emotional distress and objective demands of cancer caregiving are comparable to those of dementia caregiving, yet little research has focused on the physical health of cancer caregivers. Whether the stress leads directly to changes in health or whether the stress leads to changes in health behaviors, which in turn affect health, has not been systematically examined.
Objective
The objective of this study was to review the research literature regarding changes in health behaviors associated with caring for an individual with cancer.
Methods
Literature was reviewed from multiple databases including CINAHL (Cumulative Index to Nursing and Allied Health Literature), CINAHL Plus, PsycNET, PubMed, SCOPUS, EMBASE, and Web of Science. Key words included “health behavior,” “health promotion,” ”caregivers/caregiving,” “cancer/oncology,” “diet/nutrition,” “exercise/physical activity,” “stress management,” “smoking” and “alcohol.” Studies were included if they involved informal adult caregivers and at least 1 behavior associated with a healthy lifestyle. Of the 866 studies identified, 8 met the criteria.
Results
Studies revealed conflicting information, with some suggesting deleterious changes in behaviors, whereas others found the changes protective.
Conclusions
The lack of uniformity of terminology and conflicting findings make it difficult to conclude the impact of the caregiving experience on the health behaviors of cancer caregivers. Something is placing caregivers at risk for illness and early death, but the mechanisms behind the risk and the role of unhealthy behaviors are not clear.
Implications for Practice
At a minimum, cancer caregivers should be screened for behavior changes and disease risk. Developing standardized measures for future research including controlled, longitudinal studies is needed.
Keywords: Burden, Cancer, Caregivers, Health behaviors, Screening, Stress
Simply defined, health behaviors refer to those actions taken or avoided by an individual that impact one’s health. These actions, often embedded in one’s lifestyle, focus on illness prevention, detection, and management1 (Table 1). Behaviors associated with illness prevention are further categorized as health-promoting behaviors (healthy diet, physical activity) or health-risk behaviors (tobacco use, drug, or alcohol abuse). The evidence connecting unhealthy behaviors with morbidity and mortality is substantial. Numerous studies have shown that unhealthy diets,2,3 physical inactivity,4,5 cigarette smoking,6,7 and excessive alcohol consumption8,9 are associated with cardiovascular disease, cancer, and premature death.
Table 1.
Categories of Health Behaviors
| Illness Prevention | |||||
|---|---|---|---|---|---|
| Category | Health Promoting | Health Risk | Health Responsibility | Illness Detection | Illness Management |
| Behavior |
|
|
|
|
|
Stress also places individuals at increased risk for these diseases, and it exacerbates health-risk behaviors.10 High levels of stress are associated with increased consumption of tobacco,11 alcohol,12 fat, and sugar11,13,14 and decreased exercise.11 Conversely, engaging in health-promoting behaviors, such as eating a healthy diet15 and exercising,16 can moderate the effects of stress and decrease the risk of morbidity and mortality.17–20
Caring for an individual with cancer is perceived as a stressor and is associated with changes in one’s psychological and physical health.21 The average cancer caregiver provides 8.3 hours of care per day for 13.7 months.22 Cancer caregivers report sleep disturbances, lifestyle interferences, and social isolation, all of which are associated with poor health outcomes.21 The stress of caregiving in general places one at increased risk of morbidity and mortality23,24 with a recent study documenting that informal caregivers (n = 5688) are more likely to use negative health behaviors including smoking and poor nutrition25 compared with noncaregivers (n = 12 941). A good deal of evidence suggests that the stress of caregiving has deleterious health effects, but most of the evidence has focused on caregiving for the elderly or individuals with dementia.24,26–28 Although the physical demands of cancer caregiving have been found comparable to the stress and demands of dementia caregiving, they are greater than that of elderly caregiving,29 raising questions about the ability to generalize the research in this area to cancer caregivers.
In the handful of studies examining the physical health of caregivers of cancer patients, researchers have documented biological changes that suggest dysregulation of the autonomic nervous system30 and inflammatory31 processes, as well as problems with sleep.32 These same effects are commonly associated with a chronic stress state33 and are linked to an increased risk for cardiovascular disease,34 namely, hypertension34 and stroke.35 Data from the Nurses’ Health Study, a large prospective study of 54 412 women with no baseline evidence of cardiovascular disease, found that women who cared for a disabled or ill spouse for 9+ hours per week had an age-adjusted relative risk of cardiovascular disease of 1.93 (95% confidence interval [CI], 1.16–3.20) compared with noncaregivers.36 However, these studies have focused on the negative downstream effects of cancer caregiving, with little attention to changes in behaviors that may contribute to increased morbidity and mortality in this population.
Although the evidence is clear that adopting healthy behaviors can significantly lower morbidity and mortality,17–20 safeguarding one’s own health while caring for a cancer patient may be far from the caregiver’s mind. Cancer caregivers report having to negatively modify their lifestyles to meet caregiving demands,37 and they tend to prioritize the patient’s healthcare needs over their own.38 At a time when their stress levels are high, and they are most in need of good nutrition, exercise, and relaxation, cancer caregivers have little time and possibly dwindling financial resources available to meet these needs. Instead, they plow forward, often overwhelmed with psychological impairment, sleep disturbances, and deterioration in their physical health.21,32,37
Clearly, something is placing caregivers at risk of illness and early death, but the mechanisms behind the risk have not been well explored. Whether the stress of cancer caregiving leads directly to changes in biomarkers of health or whether the stress of cancer caregiving leads to changes in health behaviors, which in turn affect biomarkers of health, has not been systematically examined. Before research can be conducted examining the connection between the stress of cancer caregiving and health behaviors, 2 basic questions need to be asked: (1) Has the relationship between the stress of cancer caregiving and health behaviors been examined in the research literature? And, if so, (2) does the existing body of research adequately address whether the stress of cancer caregiving leads to unhealthy behaviors?
The purpose of this article was to answer these questions by reviewing the research literature regarding changes in health behaviors associated with caring for an individual with cancer. This article was developed using the Health Belief Model (HBM) as a guide.39 This model focuses on the determinants of an individual’s readiness to take action and change his/her behavior(s) for the betterment and preservation of his/her health. Cancer caregiving, particularly as it becomes a major component of one’s life, may well pose a perceived barrier to one’s ability to take action in bettering or preserving one’s health.
Methods
Review questions were formulated, and studies were evaluated using the PICOS approach to research study evaluation.40 Using this approach, studies are evaluated based on the study Population, Interventions or exposures (type and extent of cancer caregiving, for example), use of Comparators, outcomes assessed, and study design. In order to cast the widest net, an a priori decision was made to focus the review on cancer caregivers in general, including past and present caregivers of all types of cancer patients.
Studies were included if they involved (1) adult caregivers of adult cancer patients, (2) informal caregivers (family or friends), and (3) at least 1 behavior associated with a healthy lifestyle. Behaviors such as healthy eating, physical activity, alcohol and tobacco use, or those related to stress management and health responsibility (eg, screening, illness detection, and illness management) were included, as opposed to studies focusing on health indicators such as blood cholesterol, cholesterol levels, and/or obesity.
Studies were identified by searching multiple literature databases, including Cumulative Index to Nursing and Allied Health Literature (CINAHL), CINAHL Plus, PsycNET, PubMed, SCOPUS, EMBASE, and Web of Science, for the period of 1994 to July 2011. The key words/MESH terms “health behavior,” “health promotion,” “caregivers OR caregiving,” and “cancer OR oncology” were used in various combinations. Individual behaviors such as “diet or nutrition,” “exercise or physical activity,” “stress management,” “smoking,” and “alcohol” then were included. The reference list from each appropriate study was also reviewed for additional studies that were not identified in the computer search. Three reviewers independently performed the searches, using the described plan. Discrepancies between the reviewers were resolved by discussion between the reviewers.
Results
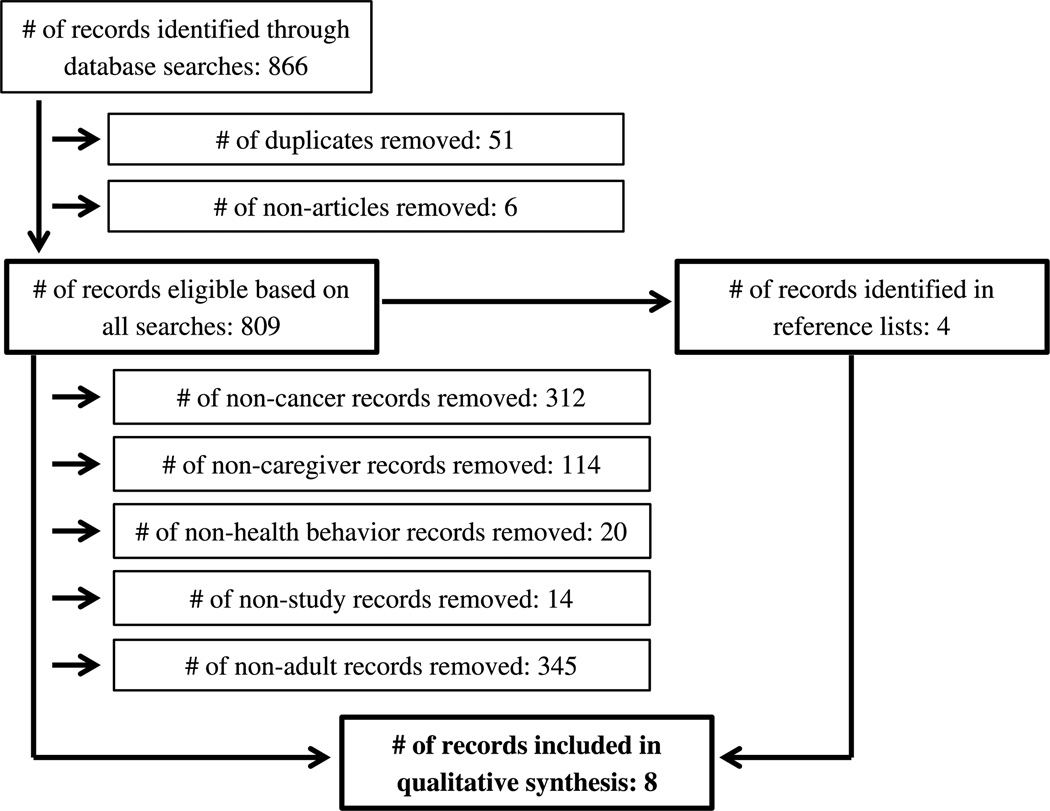
The search strategy resulted in 866 publications (Figure). After removing duplicates and nonresearch articles (n = 57), the remaining studies were reviewed based on the inclusion criteria previously determined. This process of review excluded additional articles that did not specifically pertain to adult cancer caregivers (n = 771) or were not research articles focusing on health behaviors (n = 32). After adding 4 publications from the reference lists and excluding 2 studies that dealt with health behaviors in the aggregate without discussing individual health behaviors, 8 studies remained. These 8 studies are included in this review (Table 2).
Figure.
Process of systematic review of health behaviors of cancer caregivers.
Table 2.
Health Behavior Studies in Caregivers of Cancer Patients
| Author and Publication Date |
Design | Sample and Study Location | Health Behavior Instrument(s) |
|---|---|---|---|
| Mazanec et al46 (2011) | Cross-sectional |
|
|
| Son et al47 (2011) | Matched case control |
|
|
| Weaver et al43 (2011) | Cross-sectional |
|
|
| Beesley et al42 (2011) | Cross-sectional |
|
|
| Willette-Murphy et al41 (2009) | Cross-sectional |
|
|
| Humpel et al45 (2007) | Cross-sectional |
|
|
| Bowman et al44 (2005) | Cross-sectional |
|
|
| Kershaw et al48 (2004) | Cross-sectional |
|
|
Abbreviations: BMI, body mass index; NR, no response.
Methodology Used in the Studies
All but 1 study41 utilized survey methodology. All used cross-sectional study designs. Two studies were secondary analyses from large national health survey studies not specific to cancer caregivers.42,43
Participants
The 8 studies involved a total of 2036 caregivers. Six studies focused on caregivers of patients with multiple forms of cancer.41,43–47 Two studies focused specifically on caregivers of individuals with ovarian42 and breast cancer.48 Cancer stage was reported in 4 of the studies.42,43,46,48Whereas 5 studies reported at least a percentage of patients undergoing active cancer treatment,42,43,45,46,48 only 1 study focused exclusively on caregivers of patients currently undergoing active treatment for cancer41,43 (Table 2).
Outcomes
Six studies examined health behaviors as the primary outcome of the study.42–47 The remaining 2 studies reported at least 1 health behavior as it related to another primary outcome (eg, alcohol use as an avoidant coping behavior).41,48
Results of Individual Studies
Son et al47 compared behavioral risk factors and use of preventive health services in 100 Korean spousal cancer caregivers and 400 age- and sex-matched control subjects chosen from the Korea National Health and Nutritional Examination Survey III. Of the caregivers, 63% were female, and 83% were considered primary caregivers, providing care for 4 or more days per week for patients with a variety of cancers including lung (22%), colorectal (18%), breast (14%), stomach (12%), and lymphoma (8%), among others (26%). Patients were divided into those who were less than 1 year (49%), between 1 and 2 years (19%), between 2 and 3 years (13%), and more than 3 years (19%) from diagnosis.
The authors found no differences between caregivers and control subjects for regular checkups. However, caregivers obtained cancer screening services more than did control subjects including screenings for gastric cancer (55.9% vs 30%, P < .001), colon cancer (53.5% vs 24.9%, P < .001), cervical cancer (69.4% vs 39.5%, P < .001), and breast cancer (67.2% vs 34.5%, P < .001). No significant group differences were found between caregivers and control subjects in current levels of smoking (23.6% vs 11.8%, P = .054), physical inactivity (76.9% vs 85.0%, P = .084), or high-risk drinking (36.3% vs 27.9%, P = .474). These findings remained unchanged even after controlling for education status and income, both of which may impact the outcomes and were significantly lower in the caregivers compared with the control subjects. The authors found no significant relationship between years from cancer diagnosis and any of the caregivers’ health behaviors.
Beesley et al42 used mailed surveys to examine health behaviors in 101 family caregivers (75% male) of women enrolled in a quality-of-life substudy of the Australian Ovarian Cancer Study. Although the substudy was longitudinal in nature, data in this study were from a single timepoint (1.5–6 years after cancer diagnosis). Outcome measures included physical activity, body mass index and waist circumference, fruit and vegetable consumption, smoking status, and alcohol intake. In addition, subjects were questioned about changes in the level of these behaviors since their loved one’s cancer diagnosis. Seventy-one percent of the caregivers were classified as overweight or obese, with 42% of all caregivers reporting having decreased their physical activity and 35% having gained weight since the diagnosis. Whereas only 20% of caregivers reported reducing their intake of fruits and vegetables after diagnosis, 80% consumed inadequate servings (<5) based on Australian guidelines. Alcohol consumption above the recommended level (>2 per occasion) was an issue for 37% of the caregivers, with 12% of the total caregivers reporting increasing their alcohol after the diagnosis. One of 13 smokers reported an increase in smoking after diagnosis.
Not all of the changes were negative, as 14% reported increasing their physical activity, 20% reported needed weight loss, and 3 of 13 smokers quit smoking since their family member’s diagnosis. Fruit and vegetable consumption increased in a small percentage (7% and 13%, respectively). However, more than half of all caregivers (56%) reported at least 1 negative health change since their loved one’s diagnosis. The authors also found those individuals with limited education were 3 times more likely to report at least 1 negative health behavior after their family member’s diagnosis (odds ratio [OR], 3.0; 95% CI, 1.1–8.4; P = .04). Other predictors of negative health behaviors or weight gain included those experiencing anxiety or depression (OR, 3.4; 95% CI, 1.1–10.1; P = .03) and those caring for a woman whose condition had worsened to the point of impacting her ability to perform her usual daily activities (OR, 4.3; 95% CI, 1.3–13.2; P = .01). One shortcoming in this study was the exclusion of any sort of control group against whom to compare the findings.
In a cross-sectional Australian study involving a convenience sample of 113 cancer survivors (41.6% breast cancer) and 544 of their friends and family members, Humpel et al45 used anonymously mailed surveys to examine self-reported, post–cancer diagnosis changes in physical activity, diet, smoking levels, and sun-safe practices (81.4% female; mean age, 46 ± 15 years). Among individuals with a friend or family member diagnosed with cancer, 36.2% of smokers reported quitting, 24.3% reported increasing physical activity, 58.5% reported increased consumption of fruits and vegetables, 53.2% reported decreasing their fat intake, and 59% reported increasing sun-safe behaviors. Age had a positive influence on health behaviors among family and friends, with increases in fiber (χ2 = 18.908, P < .001), fruit and vegetable consumption (χ2 = 7.094, P < .05), and sun-safe behaviors (χ2 = 25.704, P < .001), as well as decreases in fat consumption (χ2 = 9.851, P < .01) associated with increasing age. The authors found no significant relationship between cancer type and health behaviors. The authors concluded that cancer survivors and their friends and family members made a number of positive health behavior changes after their diagnosis and suggested that these individuals might be motivated to improve their health as a result of the “teachable moment”45(p628) offered by the cancer diagnosis.
Although encouraging, these results must be interpreted with some skepticism, as the subjects were self-reported family and friends, not necessarily primary caregivers of cancer patients. This study primarily involved cancer survivors, with the large majority of subjects (71.2%) more than 2 years post–cancer diagnosis and only 27% currently undergoing any sort of cancer treatment. Finally, the sample was recruited from the registry of a walking event, which may be a more motivated and health-conscious population than is typical of cancer caregivers.
Bowman et al44 found similar positive findings in a cross-sectional study using survey methodology to examine health maintenance practices of 109 spouses and adult children caregivers of long-term cancer survivors. Participants were mostly older (mean, 61.0 ± 14 years), white (n = 70; 64.1%), and female (n = 80; 73.4%). In general, caregivers reported practicing a number of health-promoting activities including exercising (74%), getting enough rest (84%), limiting alcohol intake (51%), avoiding tobacco (57%), managing their weight (70%), performing routine medical checkups, and praying (59%). A number of factors were related to health maintenance activities during the survivorship phase including being older (β = .31; P < .01), being white (β = −.19; P < .05), and being a caregiver during cancer diagnosis and treatment (r = 0.32; P < .01).
Like Humpel et al,45 the authors concluded that there may be a positive aspect of cancer caregiving in that individuals, as a result of their experience, may take a more active role in the protection of their health. However, it should be emphasized that this study involved caregivers of cancer survivors, the majority of whom participated in caregiving over 12 years prior to the study. It is unclear from this study whether active caregivers, in the midst of cancer diagnosis and treatment, would fare so well. The fact that black caregivers reported poorer health maintenance activities than did white caregivers is also of interest and warrants further investigation.
Caregivers of individuals diagnosed with early stages of cancer fared more favorably in psychological, physical, and total wellbeing than those caring for individuals in more advanced stages of cancer, and individuals providing short-term care reported better spiritual and social well-being than did those providing long-term care. These findings are important and imply that the greater the burden of caregiving, either in gravity or duration, the worse the outcome for the caregiver. Although not the primary outcome, the researchers reported significant inverse relationships between emotional strain subscales of overload (P = .05) and isolation (P = .01) with health behaviors, indicating that caregivers experiencing more emotional strain report practicing fewer healthy behaviors.
In a cross-sectional study involving a convenience sample of 70 caregivers of individuals with advanced cancer who were enrolled in a palliative care clinical trial, Mazanec et al46 examined caregivers’ health promotion behaviors, caregiver burden, social support, depression, anxiety, and work productivity. Using mailed surveys, the investigators explored overall health, physical activity, rest, diet, smoking, and healthcare utilization. Caregivers were predominantly female (n = 49; 70%), white (n = 58; 82%), and married (n = 53; 75.7%). The majority were spouses of the care recipient (n = 44; 62.9%), and 11 (15.7%) were daughters. The mean age of the caregivers was 57.01.
The majority of caregivers reported their health as good or excellent (n = 53; 75.7%) and their diet as healthy (n = 42; 60%). Sixty percent (n = 42) believed that caregiving did not interfere with their ability to get adequate exercise. No relationship was found between physical activity and hours of caregiving or patient functional status. However, greater than 50% reported levels of physical activity below the recommended guidelines. Male caregivers were more likely to participate in physical activity than were females (rs = 0.46, P < .001). Caregivers who reported higher levels of physical activity reported better health (rs = 0.25, P < .05), and investigators found an inverse relationship between physical activity and both the level of social support (rs = −0.28, P < .05) and the number of reported health problems (rs = −0.23, P < .05).
A strength of this study was that, unlike many studies of cancer caregivers that are retrospective and thus focus on cancer survivors, the large majority (n = 50; 80.6%) of the care recipients in this study were currently receiving cancer treatment for stage III (n = 30; 43.5%) or stage IV (n = 37; 53.6%) cancer. However, the cross-sectional nature of the study involving a convenience sample makes it difficult to generalize the findings beyond the study sample.
Citing the significant relationship between sleep disturbances with morbidity and mortality,49 Willette-Murphy et al41 used a cross-sectional design to examine the relationship between physical activity and sleep in 68 female family caregivers of males beginning radiation therapy for lung, prostate, or brain cancer. Sleep was assessed using subjective measures (Pittsburg Sleep Quality Index50 and the General Sleep Disturbance Scale51), as well as wrist actigraphy. The researchers found that inactive women (n = 38) took longer to fall asleep (t = 2.2; P < .05) and slept a shorter duration (t = −2.2; P < .05) than did active women (n = 30). The inactive women also exhibited more comorbid conditions (t = 2.05; P = .05), more problems with attention (t = −2.77; P < .01), and more daytime sleep (t = 2.36; P < .05) than did the active women.
This study is valuable for a number of reasons. First, it is one of the few studies that utilized objective measures (wrist actigraphy) to examine health behaviors. Second, unlike retrospective studies that focus on caregivers of cancer survivors, all of the caregivers were providing care to individuals currently undergoing cancer treatment. Finally, it is one of the few studies to focus on the link between a specific health behavior (physical activity) and negative health consequences. However, the cross-sectional nature of the study and the fact that the researchers utilized a convenience sample limit the generalizability of the findings.
Using data from the CanCORS (Cancer Care Outcomes Research and Surveillance) and CanCORS Caregiver studies, Weaver et al43 examined the relationship of smoking with mental health and quality of life in 742 lung (n = 383) and colorectal (n = 359) cancer patient–caregiver dyads. When controlling for gender, age, race/ethnicity, education, relationship with cancer patient, and cancer stage, colorectal and lung cancer caregivers who smoked reported significantly higher levels of anxiety (B = 0.19, P < .05; B = 0.23, P < .05, respectively) than did nonsmoking caregivers; colorectal caregivers also reported significantly higher rates of depression (B = 1.98, P < .05). Compared with nonsmoking dyads, cancer caregivers in dyads where 1 or more members continued to smoke after a cancer diagnosis reported lower mental health (but not physical health) quality of life; only lung cancer caregivers perceived that the burden and financial strain due to caregiving were greater when the cancer patient continued to smoke. The rates of smoking in the caregiving participants (22.1%) were slightly higher than the national average of 20.3%. Although the study found a number of interesting findings related to the effects of caregiver and/or patient smoking as it relates to caregivers, the study did not examine whether rates or amount of smoking increased in caregivers as a result of the caregiving experience.
One final study examined alcohol and drug use as an avoidant coping strategy in 189 family caregivers of individuals with advanced breast cancer.48 A substudy of a larger randomized clinical trial examining the effect of a family intervention on the quality of life of women with advanced breast cancer and their caregivers52 included only women with stages III and IV cancer. The average age of caregivers was 52 (SD, 13.4) years, and the majority were husbands (59%), followed by adult daughters (14%), sisters (8%), and adult sons (5%), in addition to other relatives and friends (14%). The majority of caregivers were males (67.2%) versus females (32.8%). Using the Brief COPE Scale53 to assess a variety of coping strategies including alcohol and drug use, caregivers exhibited higher scores in the use of alcohol and drugs as a coping strategy than did the patients (2.38 ± 1.1 vs 2.11 ± 0.4, P < .004). Further analyses revealed that gender did not play a significant role in these findings.
Because the focus of the study was on active versus avoidant coping strategies and quality of life, the findings related to alcohol use represent only a small fraction of the results. Alcohol and drug use was not measured by quantity consumed but instead with a 4-point Likert scale in response to “I’ve been using alcohol or other drugs to help me get through it.” The authors acknowledged that, although caregivers were more likely than patients to turn to alcohol or a drug as a means of coping, this represented the least used avoidant coping mechanism in either patients or caregivers.
Synthesis of Results
A synthesis of the results of the review is provided in Table 3. Of the 6 studies that examined health promotion behaviors in cancer caregivers, all 6 focused on physical activity. The results regarding the impact of cancer caregiving on physical activity were mixed, both across and within studies. The majority in 1 study reported that caregiving did not interfere with physical activity, yet half reported physical activity levels below that recommended for health.46 The majority of subjects in the study of Bowman et al44 reported regular exercise, and a quarter of those in the study of Humpel et al45 reported that their physical activity increased after their patient’s diagnosis. On the contrary, 42% of the subjects in the study of Beesley et al42 reported that their physical activity levels had decreased as a result of caregiving. Son et al47 found no difference in levels of physical activity between caregivers and control subjects. Willette-Murphy et al41 found that those caregivers with lower levels of physical activity exhibited more problems with sleep.
Table 3.
Synthesis of the Evidence Regarding the Relationship Between Caregiving and Health Behaviors
| Behavior | Synthesis of Results | |
|---|---|---|
| Illness prevention | ||
| Health promoting | Physical activity41,42,44–47 | Results are conflicting and inconclusive |
| Healthy eating42,45,46 | Results are conflicting and inconclusive | |
| Health risk | Tobacco use42–45,47 | Results are conflicting and inconclusive |
| Drug and alcohol abuse42,44,47,48 | Results are conflicting and inconclusive | |
| Health responsibility | Screening practices and routine care44–47 | Evidence exists that caregivers seek health screenings and medical examinations at rates higher than control or comparison subjects |
| Illness detection | Seeking care for illness | No evidence found |
| Illness management | Health maintenance | No evidence found |
Three of the 6 studies that focused on health promotion in cancer caregivers examined healthy eating. Like physical activity, the evidence regarding healthy eating was conflicting. In 2 studies, the majority of cancer caregivers reported consuming a healthy diet46 and increased fruits and vegetables,45 whereas a third study that examined intake found inadequate consumption of fruits and vegetables.42
Five studies examined the health-risk behavior of tobacco use in cancer caregivers. Whereas 1 study found no difference in smoking rates in caregivers and matched control subjects,47 3 of the remaining 4 studies related somewhat positive findings; at least a small percentage of caregivers reported either quitting or avoiding the use of tobacco after their patient’s diagnosis.42,44,45 One final study reported that smoking rates in cancer caregivers were higher than those in the general population, and smoking in these caregivers was associated with significantly higher mental distress.43
Another health-risk behavior, alcohol and drug abuse, was examined in 4 studies and yielded conflicting results. In 1 study, there were no differences in alcohol consumption in caregivers compared with matched control subjects,47 whereas subjects in a second study reported limiting or avoiding the use of alcohol.44 Two other studies found excessive alcohol consumption to be a problem for more than a third of the caregivers42 and that a percentage of subjects used alcohol and drugs as a coping mechanism.48
The evidence regarding health responsibility behaviors (asymptomatic screening and routine healthcare) is somewhat more favorable. Four studies examined these behaviors in cancer caregivers. Cancer caregivers obtained cancer screenings at higher rates than matched control subjects,47 and the majority report having regular medical examinations44,46 and performing sun-safe practices.45 There were no studies discussing health detection or maintenance behaviors that address the attention to their own health relative to a perceived illness (eg, new illness or managing previously diagnosed illness) while serving as a caregiver.
Discussion
In response to the research questions posed in this review, there is a small body of relatively new research addressing the relationship between the stress of being a caregiver for a cancer patient and changes in health behaviors. Although these studies represent a good start in developing an evidence base regarding health behaviors in cancer caregivers, the evidence is inconclusive, and many gaps remain. These gaps must be addressed before confident conclusions can be made, and meaningful interventions can be designed.
First, some of the studies yielded conflicting information, with Beesley et al42 painting a relatively grim picture regarding the health behaviors of ovarian cancer caregivers, and others finding a “healthy” caregiver effect with the diagnosis of cancer providing a “wakeup call” to a healthier lifestyle44,45 or disease prevention.47 Some of these differences may well be a result of timing, as those studies focusing on active caregivers, those in the midst of the demands of caregiving, tended to have less favorable outcomes than did those studies involving caregivers of cancer survivors, most of whom were beyond the acute treatment phase. The HBM proposes that individuals may experience barriers that prevent them from engaging in healthy behaviors. It is possible that, particularly when the burden is greatest such as during an acute treatment, caregiving may be a perceived barrier, both psychological and practical, to maintaining healthy behaviors. For example, the time demands of active caregiving may prohibit the caregiver from exercising, eating properly, or participating in stress reduction activities; the stress of active caregiving may make individuals more susceptible to self-medicating with alcohol, drugs, and/or food. However, once the acute demands of active caregiving are over, cancer caregiving may be protective, particularly as it relates to obtaining cancer screening and routine medical care.
Most of the studies to date have relied on retrospective selfreports of health behaviors, which are subject to response and recall bias. Some utilized data from studies where health behaviors were not the primary outcome. The use of secondary data presents the problem of measures that were not designed specifically for the research questions being proposed. For example, examining current smoking status does not enable one to draw any conclusions about the impact of caregiving on smoking behaviors. Defining who precisely was a caregiver was an issue in some studies. For example, Son et al47 chose control subjects from a large national spousal health and nutrition study, with no way of excluding caregivers of other populations such as dementia or the elderly.
Because definitions and measures were not uniform across studies, it is difficult to compare results. For example, Son et al47 defined problem alcohol drinking as the consumption of 5 or more drinks for women and 7 or more drinks per occasion for men, whereas Beesley et al42 categorized individuals based on whether their alcohol consumption met guidelines for reducing health risk (≤2 drinks per occasion).
Almost all of the studies were descriptive in nature, with only 2 looking at the relationship between caregiving and any of the health outcomes.41,42 This is unfortunate in light of the fact that individuals who engaged in more healthy behaviors have reported significantly better total physical well-being and psychological well-being, as well as total quality of life.54 Conflicting results, lack of uniformity in terminology across studies, and the absence of prospective, controlled, longitudinal studies examining changes in health behaviors over time in cancer caregivers underscore the need for additional research in this area. According to the HBM, a critical factor in motivating individuals to make changes in health behaviors is whether they perceive the risks and benefits. The evidence elucidating the impact of cancer caregiving on health behaviors will help delineate the risks and benefits, and it will guide the development of appropriate interventions.
Implications for Research and Practice
Health behaviors, particularly those associated with cardiovascular risk and obesity, are currently a high priority in the United States.55 Caregivers of cancer patients, especially those receiving intense treatments, may be at risk for significant health effects including cardiovascular morbidity as a consequence of the caregiving experience.56 Although the evidence regarding the burden of cancer caregiving is clear, the relationship between caregiver burden and health behaviors is inconclusive and needs to be more clearly delineated to offer clear guidance to practice. Large-scale, longitudinal studies are needed to clarify whether cancer caregiving in general is damaging or protective to one’s health. Specifically, the relationship between cancer caregiving and specific health promotion, health risk, illness detection, and illness management behaviors needs to be examined in a systematic manner. Research regarding the development of unhealthy behaviors in caregivers across the cancer trajectory is needed, along with studies to identify what phenotypes place an individual at risk for unhealthy behaviors and what environmental factors contribute to the adoption of these unhealthy behaviors.
Because nearly every family will at some point in time be in the position of having to provide care for an ill loved one, this represents a very large and very real public health concern. The good news is that, should the morbidity and mortality associated with caregiving indeed be related to health behaviors, interventions may be implemented to improve outcomes. Interventions shown to improve one’s cardiovascular disease risk include improving diet/nutrition, attaining adequate activity/exercise, and limiting abuse of alcohol, as well as quitting smoking and managing stress.57
Although the findings of this review are inconclusive regarding the impact of the stress of cancer caregiving on health behaviors, the evidence that cancer caregiving can be stressful is irrefutable. At a minimum, health providers should encourage caregivers to take care of their own health. Caregivers should be given specific permission to care for themselves, as they tend to prioritize the cancer patient’s needs over their own.38 Because cancer caregiving is often more of a marathon than a sprint, caregivers should be reminded to pace themselves accordingly. Education should focus on the importance of maintaining a healthy diet and getting sufficient physical activity and rest. Caregivers should be encouraged to monitor their blood pressure and have regular health screenings. Current recommendations for a healthy heart are available from the American Heart Association at www.heart.org/numbersthatcount.
Primary care providers are often intensely and appropriately focused on the immediate needs of the cancer patient, and they may need to make a special effort to focus attention on the caregiver. Just as the caregiver may not be on the radar screen of the provider, their own health may not be on the screen of the caregiver as well.
ACKNOWLEDGMENT
The authors thank Stephen Klagholz, BS, for his support in the development of this article. This article is a product of official government work in the Intramural Research Program of the National Institutes of Health.
Footnotes
The authors have no funding or conflicts of interest to disclose.
References
- 1.Glanz K, Rimer BK, Lewis FM. The scope of health behavior and health education. In: Glanz K, Rimer BK, Lewis FM, editors. Health Behavior and Health Education: Theory, Research, and Practice. 3rd ed. San Francisco, CA: Jossey-Bass; 2002. pp. 3–21. [Google Scholar]
- 2.Cox BD, Whichelow MJ, Prevost AT. Seasonal consumption of salad vegetables and fresh fruit in relation to the development of cardiovascular disease and cancer. Public Health Nutr. 2000;3(1):19–29. doi: 10.1017/s1368980000000045. [DOI] [PubMed] [Google Scholar]
- 3.Heidemann C, Schulze MB, Franco OH, Van Dam RM, Mantzoros CS, Hu FB. Dietary patterns and risk of mortality from cardiovascular disease, cancer, and all causes in a prospective cohort of women. Circulation. 2008;118(3):230–237. doi: 10.1161/CIRCULATIONAHA.108.771881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Batty GD, Shipley MJ, Marmot M, Smith GD. Physical activity and cause-specific mortality in men: further evidence from the Whitehall study. Eur J Epidemiol. 2001;17(9):863–869. doi: 10.1023/a:1015609909969. [DOI] [PubMed] [Google Scholar]
- 5.Smith GD, Shipley MJ, Batty GD, Morris JN, Marmot M. Physical activity and cause-specific mortality in the Whitehall study. Public Health. 2000;114(5):308–315. doi: 10.1038/sj.ph.1900675. [DOI] [PubMed] [Google Scholar]
- 6.Batty GD, Kivimaki M, Gray L, Smith GD, Marmot MG, Shipley MJ. Cigarette smoking and site-specific cancer mortality: testing uncertain associations using extended follow-up of the original Whitehall study. Ann Oncol. 2008;19(5):996–1002. doi: 10.1093/annonc/mdm578. [DOI] [PubMed] [Google Scholar]
- 7.Teo KK, Ounpuu S, Hawken S, et al. Tobacco use and risk of myocardial infarction in 52 countries in the INTERHEART study: a case-control study. Lancet. 2006;368(9536):647–658. doi: 10.1016/S0140-6736(06)69249-0. [DOI] [PubMed] [Google Scholar]
- 8.Gmel G, Gutjahr E, Rehm J. How stable is the risk curve between alcohol and all-cause mortality and what factors influence the shape? A precision-weighted hierarchical meta-analysis. Eur J Epidemiol. 2003;18(7):631–642. doi: 10.1023/a:1024805021504. [DOI] [PubMed] [Google Scholar]
- 9.Mukamal KJ, Chen CM, Rao SR, Breslow RA. Alcohol consumption and cardiovascular mortality among U.S. adults, 1987 to 2002. J Am Coll Cardiol. 2010;55(13):1328–1335. doi: 10.1016/j.jacc.2009.10.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McEwen BS. Allostasis and allostatic load: implications for neuropsychopharmacology. Neuropsychopharmacology. 2000;22(2):108–124. doi: 10.1016/S0893-133X(99)00129-3. [DOI] [PubMed] [Google Scholar]
- 11.Ng DM, Jeffery RW. Relationships between perceived stress and health behaviors in a sample of working adults. Health Psychol. 2003;22(6):638–642. doi: 10.1037/0278-6133.22.6.638. [DOI] [PubMed] [Google Scholar]
- 12.Higley JD, Hasert MF, Suomi SJ, Linnoila M. Nonhuman primate model of alcohol abuse: effects of early experience, personality, and stress on alcohol consumption. Proc Natl Acad Sci U S A. 1991;88(16):7261–7265. doi: 10.1073/pnas.88.16.7261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Oliver G, Wardle J. Perceived effects of stress on food choice. Physiol Behav. 1999;66(3):511–515. doi: 10.1016/s0031-9384(98)00322-9. [DOI] [PubMed] [Google Scholar]
- 14.Schiffman SS, Graham BG, Sattely-Miller EA, Peterson-Dancy M. Elevated and sustained desire for sweet taste in African-Americans: a potential factor in the development of obesity. Nutrition. 2000;16(10):886–893. doi: 10.1016/s0899-9007(00)00403-2. [DOI] [PubMed] [Google Scholar]
- 15.Roohafza H, Sadeghi M, Sarraf-Zadegan N, et al. Short communication: relation between stress and other life style factors. Stress Health. 2007;23(1):23–29. [Google Scholar]
- 16.Salmon P. Effects of physical exercise on anxiety, depression, and sensitivity to stress: a unifying theory. Clin Psychol Rev. 2001;21(1):33–61. doi: 10.1016/s0272-7358(99)00032-x. [DOI] [PubMed] [Google Scholar]
- 17.Knoops KTB, De Groot LCPGM, Kromhout D, et al. Mediterranean diet, lifestyle factors, and 10-year mortality in elderly European men and women: the HALE project. JAMA. 2004;292(12):1433–1439. doi: 10.1001/jama.292.12.1433. [DOI] [PubMed] [Google Scholar]
- 18.Kvaavik E. Influence of individual and combined health behaviors on total and cause-specific mortality in men and women: the United Kingdom Health and Lifestyle Survey. Arch Intern Med. 2010;170(11):998. doi: 10.1001/archinternmed.2010.76. (Archives of Internal Medicine 2010; 170(8)711–718). [DOI] [PubMed] [Google Scholar]
- 19.Scrutinio D. The potential of lifestyle changes for improving the clinical outcome of patients with coronary heart disease: mechanisms of benefit and clinical results. Rev Recent Clin Trials. 2010;5(1):1–13. doi: 10.2174/157488710790820508. [DOI] [PubMed] [Google Scholar]
- 20.Van Dam RM, Li T, Spiegelman D, Franco OH, Hu FB. Combined impact of lifestyle factors on mortality: prospective cohort study in US women. BMJ. 2008;337(7672):742–745. doi: 10.1136/bmj.a1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Northouse L, Williams AL, Given B, McCorkle R. Psychosocial care for family caregivers of patients with cancer. J Clin Oncol. 2012;30(11):1227–1234. doi: 10.1200/JCO.2011.39.5798. [DOI] [PubMed] [Google Scholar]
- 22.Yabroff KR, Kim Y. Time costs associated with informal caregiving for cancer survivors. Cancer. 2009;115(Suppl 18):4362–4373. doi: 10.1002/cncr.24588. [DOI] [PubMed] [Google Scholar]
- 23.Schulz R, Beach SR. Caregiving as a risk factor for mortality: the Caregiver Health Effects Study. JAMA. 1999;282(23):2215–2219. doi: 10.1001/jama.282.23.2215. [DOI] [PubMed] [Google Scholar]
- 24.von Kanel R, Mausbach BT, Patterson TL, et al. Increased Framingham Coronary Heart Disease Risk Score in dementia caregivers relative to non-caregiving controls. Gerontology. 2008;54(3):131–137. doi: 10.1159/000113649. [DOI] [PubMed] [Google Scholar]
- 25.Hoffman GJ, Lee J, Mendez-Luck CA. Health behaviors among baby boomer informal caregivers. Gerontologist. 2012;52(2):219–230. doi: 10.1093/geront/gns003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gouin JP, Hantsoo L, Kiecolt-Glaser JK. Immune dysregulation and chronic stress among older adults: a review. Neuroimmunomodulation. 2008;15(4–6):251–259. doi: 10.1159/000156468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Roepke SK, Mausbach BT, Patterson TL, et al. Effects of Alzheimer caregiving on allostatic load. J Health Psychol. 2011;16(1):58–69. doi: 10.1177/1359105310369188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sörensen S, Conwell Y. Issues in dementia caregiving: effects on mental and physical health, intervention strategies, and research needs. Am J Geriatr Psychiatry. 2011;19(6):491–496. doi: 10.1097/JGP.0b013e31821c0e6e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kim Y, Schulz R. Family caregivers’ strains: comparative analysis of cancer caregiving with dementia, diabetes, and frail elderly caregiving. J Aging Health. 2008;20(5):483–503. doi: 10.1177/0898264308317533. [DOI] [PubMed] [Google Scholar]
- 30.Lucini D, Cannone V, Malacarne M, et al. Evidence of autonomic dysregulation in otherwise healthy cancer caregivers: a possible link with health hazard. Eur J Cancer. 2008;44(16):2437–2443. doi: 10.1016/j.ejca.2008.08.006. [DOI] [PubMed] [Google Scholar]
- 31.Rohleder N, Marin TJ, Ma R, Miller GE. Biologic cost of caring for a cancer patient: dysregulation of pro- and anti-inflammatory signaling pathways. J Clin Oncol. 2009;27(18):2909–2915. doi: 10.1200/JCO.2008.18.7435. [DOI] [PubMed] [Google Scholar]
- 32.Berger AM, Parker KP, Young-McCaughan S, et al. Sleep wake disturbances in people with cancer and their caregivers: state of the science. Oncol Nurs Forum. 2005;32(6):E98–E126. doi: 10.1188/05.ONF.E98-E126. [DOI] [PubMed] [Google Scholar]
- 33.Juster RP, McEwen BS, Lupien SJ. Allostatic load biomarkers of chronic stress and impact on health and cognition. Neurosci Biobehav Rev. 2010;35(1):2–16. doi: 10.1016/j.neubiorev.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 34.Capistrant BD, Moon JR, Berkman LF, Glymour MM. Current and long-term spousal caregiving and onset of cardiovascular disease. J Epidemiol Community Health. 2012;66(10):951–965. doi: 10.1136/jech-2011-200040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Haley WE, Roth DL, Howard G, Safford MM. Caregiving strain and estimated risk for stroke and coronary heart disease among spouse caregivers: differential effects by race and sex. Stroke. 2010;41(2):331–336. doi: 10.1161/STROKEAHA.109.568279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lee S, Colditz GA, Berkman LF, Kawachi I. Caregiving and risk of coronary heart disease in U.S. women: a prospective study. Am J Prev Med. 2003;24(2):113–119. doi: 10.1016/s0749-3797(02)00582-2. [DOI] [PubMed] [Google Scholar]
- 37.Stenberg U, Ruland CM, Miaskowski C. Review of the literature on the effects of caring for a patient with cancer. Psycho-oncology. 2010;19(10):1013–1025. doi: 10.1002/pon.1670. [DOI] [PubMed] [Google Scholar]
- 38.Williams LA. Whatever it takes: informal caregiving dynamics in blood and marrow transplantation. Oncol Nurs Forum. 2007;34(2):379–387. doi: 10.1188/07.ONF.379-387. [DOI] [PubMed] [Google Scholar]
- 39.Janz NK, Champion VL, Strecher VJ. The Health Belief Model. In: Glanz K, Rimer BK, Lewis FM, editors. Health Behavior and Health Education: Theory, Research, and Practice. Hoboken, NJ: Jossey-Bass; 2002. [Google Scholar]
- 40.O’Connor D, Green S, Higgins JPT, Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions. London, UK: The Cochrane Collaboration - John Wiley & Sons, Ltd; 2008. Chapter 5: defining the review question and developing criteria for including studies: the Cochrane Collaboration. No. 5.0.1. [Google Scholar]
- 41.Willette-Murphy K, Lee KA, Dodd M, et al. Relationship between sleep and physical activity in female family caregivers at the initiation of patients’ radiation therapy. J Obstet Gynecol Neonatal Nurs. 2009;38(3):367–374. doi: 10.1111/j.1552-6909.2009.01032.x. [DOI] [PubMed] [Google Scholar]
- 42.Beesley VL, Price MA, Webb PM. Loss of lifestyle: health behaviour and weight changes after becoming a caregiver of a family member diagnosed with ovarian cancer. Support Care Cancer. 2011;19(12):1949–1956. doi: 10.1007/s00520-010-1035-2. [DOI] [PubMed] [Google Scholar]
- 43.Weaver KE, Rowland JH, Augustson E, Atienza AA. Smoking concordance in lung and colorectal cancer patient–caregiver dyads and quality of life. Cancer Epidemiol Biomarkers Prev. 2011;20(2):239–248. doi: 10.1158/1055-9965.EPI-10-0666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bowman KF, Rose JH, Deimling GT. Families of long-term cancer survivors: health maintenance advocacy and practice. Psycho-oncology. 2005;14(12):1008–1017. doi: 10.1002/pon.911. [DOI] [PubMed] [Google Scholar]
- 45.Humpel N, Magee C, Jones SC. The impact of a cancer diagnosis on the health behaviors of cancer survivors and their family and friends. Support Care Cancer. 2007;15(6):621–630. doi: 10.1007/s00520-006-0207-6. [DOI] [PubMed] [Google Scholar]
- 46.Mazanec SR, Daly BJ, Douglas SL, Lipson AR. Work productivity and health of informal caregivers of persons with advanced cancer. Res Nurs Health. 2011;34(6):483–495. doi: 10.1002/nur.20461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Son KY, Park SM, Lee CH, et al. Behavioral risk factors and use of preventive screening services among spousal caregivers of cancer patients. Support Care Cancer. 2011;19(7):919–927. doi: 10.1007/s00520-010-0889-7. [DOI] [PubMed] [Google Scholar]
- 48.Kershaw T, Northouse L, Kritpracha C, Schafenacker A, Mood D. Coping strategies and quality of life in women with advanced breast cancer and their family caregivers. Psychol Health. 2004;19(2):139–155. [Google Scholar]
- 49.Kripke DF. Sleep and mortality. Psychosom Med. 2003;65(1):74. doi: 10.1097/01.psy.0000039752.23250.69. [DOI] [PubMed] [Google Scholar]
- 50.Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 51.Lee KA, DeJoseph JF. Sleep disturbances, vitality, and fatigue among a select group of employed childbearing women. Birth. 1992;19(4):208–213. doi: 10.1111/j.1523-536x.1992.tb00404.x. [DOI] [PubMed] [Google Scholar]
- 52.Northouse LL, Caffey M, Deichelbohrer L, et al. The quality of life of African American women with breast cancer. Res Nurs Health. 1999;22(6):449–460. doi: 10.1002/1098-240x(199912)22:6<449::aid-nur3>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 53.Carver CS. You want to measure coping but your protocol’s too long: consider the Brief COPE. Int J Behav Med. 1997;4(1):92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- 54.Matthews BA, Baker F, Spillers RL. Family caregivers’ quality of life: influence of health protective stance and emotional strain. Psychol Health. 2004;19(5):625–641. [Google Scholar]
- 55.US DHHS. The Surgeon General’s Vision for a Healthy and Fit Nation. Rockville, MD: U.S. Department of Health and Human Services, Office of the Surgeon General; 2010. [PubMed] [Google Scholar]
- 56.Bevans M, Sternberg EM. Caregiving burden, stress, and health effects among family caregivers of adult cancer patients. JAMA. 2012;307(4):398–403. doi: 10.1001/jama.2012.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.American Heart Association. Numbers That Count for a Healthy Heart. Dallas, TX: American Heart Association, Inc; 2011. [Google Scholar]