Abstract
Background:
Active adults commonly present with lower extremity (LE) injuries from a variety of professional and amateur sports activities. Decreased LE function significantly alters daily life and subsequent injuries increase this impact. The purpose of this systematic review was to examine the association between previous injury and the risk of re‐injury, and to describe the changes in kinematics and motor programming that may contribute to this relationship.
Methods:
A preliminary search was conducted to determine the four most common LE injuries on PubMed, CINAHL and Web of Science. These injuries, in a healthy active adult population, were hamstring strain (HS), anterior cruciate ligament injury (ACL), achilles tendon pathology, and ankle sprain. After these injuries were established, the search for this systematic review found evidence relating these injuries to re‐injury. Articles related to degenerative changes were excluded. Twenty‐six articles were included in the systematic review detailing the risk of re‐injury from a previous injury and were graded for quality.
Results:
ACL injury was linked to a successive injury of the same ACL, and other injuries in the LE. HS was associated with subsequent ipsilateral HS and knee injuries. Previous achilles tendon rupture increased the risk of an analogous injury on the contralateral side. An ankle sprain was associated with a re‐injury of either the ipsilateral or the contralateral ankle. Post‐injury changes were present in strength, proprioception, and kinematics, which may have led to overall changes in motor control and function.
Conclusion:
This review provides insight into the changes occurring following common LE injuries, how these changes potentially affect risk for future injury, and address the needs of the active adult population in rehabilitation.
Clinical Relevance:
Current research on previous injury and re‐injury is of high quality, but scarce quantity. Deficits following an injury are known, but how these deficits correlate or lead to re‐injury requires further exploration.
Level of Evidence:
1
Keywords: Injury, motor programming, re‐injury
INTRODUCTION
Attempts at healthy living spur an increase in activity in the adult population and consequently, also in the risk for injury. Traumatic and atraumatic injuries are a common consequence of new or increased activity. Following injury, patients often experience decreased functional capacity. Several authors have described previous injury as the greatest risk factor for future injury secondary to changes along the kinematic chain, i.e. proprioceptive deficits, reduced range of motion, excessive flexibility, and scar tissue accumulation.1‐3 Knowledge of these intrinsic changes may benefit rehabilitation models for active adults with the potential of reducing re‐injury rates and improving quality of life, while also helping to lower overall medical costs.
A recent systematic review of the literature (SR) determined that the most common lower extremity injuries in a healthy active adult population were, in no specific order, hamstring strain (HS), anterior cruciate ligament (ACL) injury, achilles tendon pathology, and ankle sprain. Due to the intricate relationships between joints during movement of the lower extremity, changes often occur at sites other than the initial point of injury.4 Regional interdependence is an important key to understanding how anatomic variables occurring within the kinetic chain may contribute to re‐injury.5 Previously, researchers have examined these common injuries and the subsequent changes in kinematics and motor programming.2,6‐9 However, the connection of these changes to subsequent lower extremity injuries has not been examined.
The purpose of this systematic review is to establish the most common lower extremity injuries and the risk of re‐injury or subsequent injury as it relates to alterations in kinematics and motor programing. This review combines an analysis of established data on the risk of re‐injury following a lower extremity injury with a qualitative discussion on the factors that contribute to this relationship. By developing a greater understanding of the kinematic and motor programming changes following injury, the authors hope to illuminate how one injury to the lower extremity may increase the risk for re‐injury or subsequent injury. By integrating information on the relationship between injury and subsequent injury, rehabilitation could focus on not only the immediate injury, but also potentially reducing future injury.
METHODS
A five‐stage process was used to select studies. The first stage involved a search on PubMed, CINAHL, and Web of Science using the search terms “injuries AND lower extremity AND prevalence AND adults”. This search provided data that was utilized to select the four most common injuries that occur in the lower extremities. This search yielded 158 articles of which 17 were ruled in based on a title and abstract screen. From here the articles were read for full text and six articles were chosen for their specific research on injury prevalence according to these search terms. From the information presented in these articles, the four most common musculoskeletal injuries were determined to be ankle sprain, ACL injury, HS, and achilles injury.
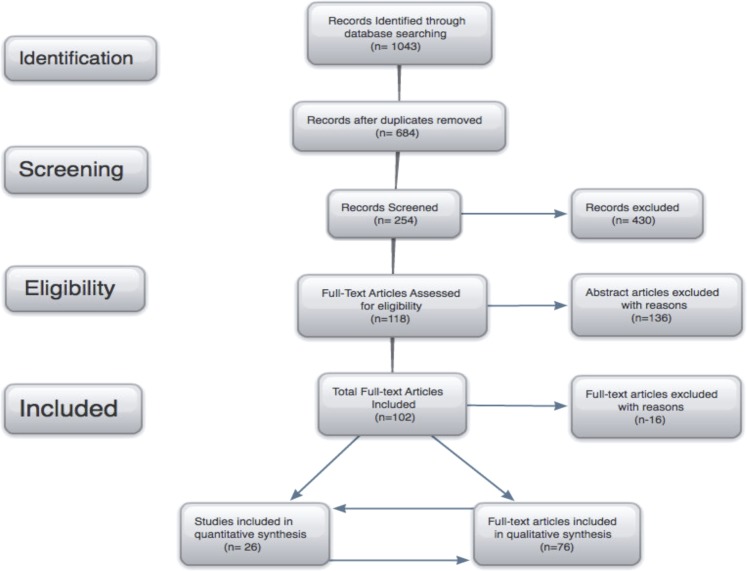
The second search for the topic of the current review utilized the terms “ankle sprain OR ACL injury OR Achilles injury OR hamstring strain AND previous injury” in PubMed and CINAHL (Figure 1). A filter of “ages 19‐44” was applied to this search. Next, two independent reviewers performed an initial assessment of the identified papers based on title. For all assessments, inclusion criteria included articles dealing with an active, healthy, athletic population (including military personnel); directly related to one of the four selected injuries; concerned with motor control or kinematics; as well as describing injury as a result of re‐injury. Articles dealing with osteoarthritis or degenerative injury were excluded. Articles written in languages other than English were excluded, unless a translated version was available. These criteria were chosen based on the immense return utilizing the selected search terms and the need to specify the population most likely at risk for re‐injury. Second, two independent reviewers performed an assessment based on the articles' abstract. For both the title and abstract assessments, all articles that received a “Yes” rating by one reviewer were kept. Finally, a full text review was performed, dividing articles equally among three teams of reviewers. Each team of two independent reviewers assessed each set. Any articles published before the year 2000 were excluded. Articles that received a split rating (one “Yes” and one “No”) were reviewed by another independent reviewer who made the final decision.
Figure 1.
Flow of literature search and review of studies
Four independent reviewers using the Quality Assessment of Diagnostic Accuracy Studies (QUADAS) tool completed grading of the articles regarding injury as a risk of re‐injury.10 The QUADAS is a 14‐question tool to determine the internal and external validity of a study. The questions are answered “yes, no, N/A or unclear”, for which one point is awarded for every “yes” answer. The QUADAS examines such biases as spectrum, selection, disease progression, and verification bias. Two reviewers graded articles related to ACL injuries and HS, while two other reviewers graded articles regarding Achilles and ankle injuries. After independently grading these articles, each pair came to a consensus on scoring criteria for each article. A score of 10 or more was considered “high quality, low risk of bias” and a score below 10 was considered “low quality, high risk of bias”.11 Cook states, “systematic reviews that use the QUADAS instrument provide a qualitative assessment of design with recognition that weaknesses in selected regions may alter some test findings more than others.”10(p. 98) Thus, with this grading system it can be stated that despite possible bias(es) existing within an article, overall quality could still be considered to be good. One of the articles, Friel et al,12 was not evaluated using the QUADAS due to the study design being Ex‐post Facto. Therefore, two independent reviewers individually graded this article as “poor”, “fair”, or “good” and came to a consensus on the grading of the article.
All five articles for ACL injury relating to subsequent injury were of high quality and low risk of bias, with scores ranging from 10 to 12 based on the QUADAS criteria. Of the seven HS related studies; only one was graded to be of low quality and high risk of bias, with a score of 8. The other articles ranged from a score of 10 to 13, indicating high quality and low risk of bias. Similarly, high quality and low risk of bias was evident in the three articles for the Achilles group, with scores ranging from 11 to 12, and the ankle injury group where the ten studies scores ranged from 11 to 13. With these findings and analyses, the authors concluded that appropriate designs have been formulated and implemented resulting in outcomes that could be used for evidence‐based practice.
RESULTS
Hamstring Strain
Five articles were found correlating HS with subsequent strains of the same muscle group (Appendix 1). In a study analyzing elite level Australian football players, the authors concluded that a HS strain within the previous 12 months was a strong predictor of future HS.3 The football players were 4.3 times more likely to incur another HS as opposed to players without history of previous HS.3 In a similar population of Australian football players and track and field athletes, 34% of HS were recurrences and previous strain was the most common reason for subsequent HS.13 In addition, 27% of all HS in the Australian Football League (AFL) were caused by previous HS, which increased the risk of recurrence by 11.6. It is unclear, however, if the cause of increased recurrence is due to accumulated microscopic muscle damage or the presence of a single injurious event.16 No matter the cause of HS, the research clearly indicates that previous HS is an important risk factor for future HS.14,15
Anterior Cruciate Ligament Injury
ACL injury has been linked to a successive injury of the same ACL and other impairments or injuries in the lower extremity (Appendix 2). In one study, ACL graft ruptures occurred in 6.4% of subjects and a contralateral ACL rupture followed at a frequency of 5.7%.17 In addition to a previous injury of the ACL, activity level after the injury was indicated to predict another injury of the same or contralateral ACL.17 In elite footballers, 70% of current ACL injuries occurred on the same leg as a previous ACL injury.2 Ten percent of subjects in another study reported traumatically reinjuring their knee, resulting in disruption of the graft, between four and twelve months after ACL reconstruction.18 Research indicates that re‐injury can occur to the same or contralateral ACL following an initial ACL injury, when that injury was treated conservatively or surgically. Inadequate landing force attenuation was identified as imposing abnormal forces after reconstruction on the musculoskeletal components, thus increasing the risk of re‐injury.19
Achilles Tendon Injury
There is little research exploring achilles tendon injury and its effect on re‐injury or subsequent injury (Appendix 3). However, one article discussed that following an Achilles tendon injury among the adult population, risk of re‐injury is greater in individuals 30 years or younger.20 Another study linked previous Achilles tendon rupture to a risk of an analogous injury on the contralateral side, stating that an individual is 176 times more likely to injure the opposite side approximately 3.1 years later compared to an individual without a previous Achilles tendon pathology. The authors proposed a multifactorial explanation to this connection suggesting an increased risk due to degenerative changes, a genetic predisposition for tendon ruptures, or disuse atrophy of the contralateral tendon from overall decreased physical activity due to immobilization of the injured leg.21
Ankle Sprain
In accordance with the research, a single ankle sprain is the most common injury resulting in a secondary sprain of the ipsilateral or contralateral ankle among the active adult population (Appendix 4). In a study investigating the effect of ankle sprain on recurrent ankle sprains in 202 elite Greek track athletes, there was a higher risk of re‐injury for low‐grade ankle sprains as opposed to high‐grade ankle sprains.22 The authors discovered that 17.8 percent of their athletes suffered a second lateral ankle sprain by the end of the follow‐up period.22 In another study involving 65 professional male football players, the recurrence of a secondary ankle sprain following the same initial injury was 50 percent higher than those without a previous ankle sprain. The authors also found that 75.38 percent of these athletes had sustained multiple ankle sprains (63.27 percent in bilateral ankles; 24.49 percent in the dominant ankle only) during their entire career up until the point at which the study was concluded.23 Pefanis et al found that a previous ankle sprain was the most important statistical factor leading to a subsequent ankle sprain, increasing the occurrence by 21 percent.24 Additional research in this area has suggested that leg dominance may be a factor leading to injury. Williams and colleagues reported that in college freshman physical education students 59 percent of recurrent ankle sprains occurred in the dominant foot among 44 of the 241 participants.25 In conclusion, the results of this SR indicate that an ankle sprain is linked to both re‐injury and subsequent injury to the contralateral side.
DISCUSSION
The results of this systematic review revealed a relationship between previous injury and re‐injury in each lower extremity injury that was studied. Overall, the vast majority of articles reviewed discussed this relationship in detail and suggested many possibilities for why this trend exists. Re‐injury was suggested to be associated with deficits in neuromuscular factors that are present following injuries.2,3,18,21,26 The goal of this discussion will be to qualitatively examine the changes that were identified in papers examined that occurred post‐injury and how they were proposed to link injury to re‐injury. Following injury, researchers have identified alterations occurring in strength, proprioception, and kinematics, which have led to overall changes in motor control and function.2,13,15,25,27‐35 This combination of insight may offer valuable information to clinicians for reduction of re‐injury.
Strength deficits between affected and unaffected limbs as well as imbalances between muscle groups have been documented post hamstring strain, post ACL rupture, and post Achilles tendon rupture.7,9,15,27‐29,33,36,37 Without recovering muscle strength of involved muscles following an initial injury, the stability of joints, biomechanics of motion, and the ability to safely participate in activity are likely compromised. Several authors suggested that incorporating strength training and standards for strength following injury is necessary in order to decrease long‐term muscular deficits that could go on to affect kinematics and motor control both proximal and distal to the injury, further increasing the risk of subsequent injury.7,9,15,27‐29,33,36,37
Proprioceptive deficits, altered muscular recruitment patterns, and changes in static and dynamic stability occur from altered neuronal firing and decreased sensory awareness within joint and muscle tissue following ACL rupture, Achilles tendon injury, and ankle sprains.9,19,31,38‐52 Authors of papers reviewed described variations in postural sway, gait mechanics, and decreased dynamic stability within functional activities that might place individuals at higher risk for re‐injury.39,40,42,48,50
Changes in strength and proprioception, which very likely occur together, contribute to the next factor to be addressed: changes in lower extremity biomechanics following injury. The observed biomechanical changes that have been documented are changes in peak torque, altered gait mechanics, and intra‐articular and intra‐muscular forces (including, compressive, tensile, and shear forces) in the hamstring, ACL, and ankle.13,30,47,48,53‐58 Comprehensive biomechanical evaluation of the patient is pertinent in order to correctly develop treatment strategies that positively affect vectors of force displacement within the body, with the aim of normalizing joint mechanics. Suboptimal mechanics during high‐level functional tasks have at times been associated with risk of future sports injuries.59‐61 The authors of this systematic review believe that by examining and addressing joint kinematics post injury, patients may have the potential to return to functional activity at a greater rate and avoid potential re‐injury.
This systematic review adequately describes the major risk of re‐injury post initial injury in the adult population. The high risk of re‐injury described, stresses the importance of comprehensive rehabilitation that uses the theory of regional interdependence to adequately mitigate local, proximal, and distal deficits in strength, proprioception, and lower extremity mechanics.5 Future research establishing standards for the aforementioned deficits and developing rehabilitation programming that addresses these limitations is important, and it may be possible to remove the previous injury risk factor component with regard to risk of future injury. In addition to the health benefits of preventing re‐injury, medical costs may also be reduced which would lower the economic burden of the initial injury.
Limitations to the study are typical of those attributed to systematic reviews. This paper focused on the four most common lower extremity injuries; however, the breadth of injuries incurred in the adult population extends beyond those examined in this research. Additionally, this research cannot be expanded beyond the active adult population. While the relationship between injury and re‐injury was described, the ability to generalize the qualitatively identified variables including kinematic alterations, motor control deficits, and musculoskeletal changes to other injuries requires further exploration. To maintain the focus of this SR, the authors did not attempt to discuss a standardized way to examine a patient for these changes, nor was it appropriate to discuss specific interventions to treat these impairments as these components were beyond the scope of this systematic review. Although there were standardized criteria for inclusion and exclusion of articles, the selection process has inherent inter‐rater reliability concerns, such that a third party reviewer was utilized if raters could not agree.
Future Studies
Future research should be performed in order to determine standardized outcome tools that could be used to objectively identify changes that occur following injury that relate to the risk for future injury. Based on the current research, it appears that it would be beneficial to include outcome tools that assess a patient's movement patterns following injury in order to optimize function from a regional interdependence approach prior to returning the patient to his/her previous level of activity. These tests may be beneficial in examining patients post‐treatment to assess for functional return to activity. Furthermore, research should be performed in order to identify the most beneficial interventions and strategies used to address changes following injury and to develop protocols to reduce risk of re‐injury.
CONCLUSION
In conclusion, this systematic review of the literature identified and reviewed 26 articles, which describe a relationship between injury and re‐injury for the four most common lower extremity injuries. Overall, the studies on re‐injury were of moderate to high quality, but the quantity of research was scarce. Evidence regarding the hamstring strain, ACL rupture, achilles tendon injury, and ankle sprain are of moderate to high quality in relation to this topic, aside from one article with a low quality rating.3 More analysis on the relationship between injury and re‐injury is needed. Motor control and kinematic deficits following injury have been suggested, but their direct relation to re‐injury requires further exploration.
Appendix 1.
Hamstring Strain Re‐injury Papers
| Title | Author | Population (age, gender, activity) | Main Findings | Type of study | QUADAS |
|---|---|---|---|---|---|
| Predictors of hamstring injury at the elite level of Australian football (2006) | Gabbe,B.J., et al. | 222 elite male Australian football players, between 17‐37 years old from 6 Melbourne AFL clubs during pre‐season of 2002 | "A positive hamstring injury history (sustained during the previous 12 months) was identified as the strongest predictor of subsequent hamstring injury and supports the findings of several studies.” | Cohort | 8 |
| Intrinsic risk factors of non‐contact quadriceps and hamstring strains in soccer: a prospective study of 100 professional players (2010) | Fousekis,K., et al. | 100 professional soccer players, between 19‐28 years old, free of injury for at least 6 months prior to testing | “For the development of hamstring strains in soccer players, two functional asymmetries of the lower limbs (isokinetic strength and leg length) are accountable, with previous history of strains in the same muscle group being rather reductive of the odds of this injury.” | Cohort | 13 |
| Predicting hamstring strain injury in elite athletes (2004) | Brockett,C.L, et al. | 27 athletes, 26 males & 1 female, 23 AFL players & 4 track‐and‐field athletes, between 19‐33 years old. | “If the optimum length for active tension is rather short, in terms of the muscle's working range, it follows that more of the descending limb will be included within the working range. That, in turn, increases the risk of damage." | Controlled Laboratory Study | 11 |
| Clinical risk factors for hamstring muscle strain (2001) | Verrall, et al. | 114 males from two professional Australian Football Leagues, mean age 21.6 years. | “There was a significantly increased risk of injury with older age, being of aboriginal descent, a past history of posterior thigh injury, a past history of knee injury, and a past history of osteitis pubis.” | Prospective Cohort | 12 |
| Clinical predictors of time to return to competition and of recurrence following hamstring strain in elite Australian footballers (2008) | Warren, et al. | 59 elite male Australian football players, mean age 24 years, who missed at least one game due to injury. | “Nine players (15%) experienced a recurrence of their hamstring injury within the first 3 weeks of returning to play” | Prospective Observational | 13 |
| The relationship between previous hamstring injury and the concentric isokinetic knee muscle strength of irish gaelic footballers (2008) | O'Sullivan, et al. | 44 male gaelic football players, mean age 21.2 years. | “Evidence of hamstring muscle weakness and muscle strength imbalance in gaelic footballers after previous hamstring injury” | Prospective Observational | 10 |
| Effects of Prior Hamstring Strain Injury on Strength, Flexibility, and Running Mechanics (2010) | Silder, et al. | 18 individuals involved in running‐related sports with a previous hamstring injury, between 18‐45 years old. | “Our results suggest that, while scar tissue may be present in subjects with a prior hamstring injury, these underlying morphological changes do not appear to be discernable in terms of functional strength measures, or musculotendon stretch and neuromuscular patterns during sprinting.” | Prospective Cohort | 11 |
Appendix 2:
ACL Re‐Injury Papers
| Title | Author | Population (age, gender, activity) | Main Findings | Type of study | QUADAS |
|---|---|---|---|---|---|
| High risk of new knee injury in elite footballers with previous anterior cruciate ligament injury (2006) | Waldén, M., et al. | 310 Male Swedish League players, mean age 25 years. 24 ACL injured, 286 ACL healthy. | “Total, 715 injuries were recorded, and 625 (87%) were located to the lower limbs. Of the injuries to the lower extremities in the ACL injured group, 70% (38/54) affected a limb with a previous ACL injury.” | Prospective Cohort | 12 |
| Factors affecting return to sports after anterior cruciate ligament reconstruction with patellar tendon and hamstring graft: a prospective clinical investigation (2006) | Gobbi,A., et al. | 100 athletes, 67 males & 33 females, mean age 28 years. Athletes playing in sports at regional/national levels/rec sports at least 3x/week, with normal contralateral knee, those w/ part. meniscectomies | “Two patients presented with persistent clicking and catching during the first year post‐ACL…In another case (HT graft), re‐injury to the operated knee was documented” | Longitudinal | 10 |
| Normalized motor function but impaired sensory function after unilateral non‐reconstructed ACL injury: patients compared with uninjured controls (2008) | Ageberg, et al. | 56 individuals, 36 males & 20 females, between 15‐45 years old who were ACL deficient with an uninjured contralateral extremity. | “The impact of these findings on the risk of sustaining re‐injuries requires further studies, and there may be a breakpoint at which the discrepancy between motor and sensory function becomes a risk factor during more strenuous activity.” | Cross‐sectional | 12 |
| Effects of early progressive eccentric exercise on muscle size and function after anterior cruciate ligament reconstruction: a 1‐year follow‐up study of a randomized clinical trial (2009) | Gerber,J.P., et al. | 40 patients with ACL‐R, between 18‐50 years old, who were moderately active prior to injury. Randomly assigned: Group 1 receiving early progressive eccentric exercise and Group 2 receiving standard rehab. | “Of those not returning for 1‐year follow‐up, 4 participants traumatically reinjured their involved knee between 4 and 12 months following initial ACL‐R, causing graft disruption.” | Randomized Control Trial | 11 |
| Closed kinetic chain alone compared to combined open and closed kinetic chain exercises for quadriceps strengthening after anterior cruciate ligament reconstruction with respect to return to sports: a prospective matched follow‐up study (2000) | Mikkelsen,C., et al. | 44 individuals, between 18–40 years old with a first‐ever unilateral ACL injury and a healthy contralateral leg. Randomly assigned: Group 1 trained with CKC and Group 2 trained with CKC for first 6 weeks, then OKC for quadriceps muscle. | Of the 22 patients in group 2, “12 returned to sport at the same level as before the injury, eight patients had reduced their activity level and/or changed to a less knee demanding sport due to impaired knee function in three patients, social and family reasons in three, and the fear of reinjuring the knee in two. One patient did not return to any type of sport due to a new knee injury of the contralateral leg. One patient was not physically active either before or after ACL reconstruction.” | Randomized Control Trial | 11 |
Appendix 3:
Achilles Tendon Re‐injury Papers
| Title | Author | Population (age, gender, activity) | Main findings | Type of study | QUADAS |
|---|---|---|---|---|---|
| Biomechanical Behavior of the Plantar Flexor Muscle‐Tendon Unit after an Achilles Tendon Rupture (2001) | Bressel, et al. | 40 individuals, 26 males & 14 females, mean age 51.4 years, volunteered for the study. All subjects were involved in at least light/ recreational activity and had ruptured their Achilles tendon more than 1 year before the study. | Stiffness and viscoelastic properties, such as torque relaxation, were similar between the involved and uninvolved limbs. However, other measurements, such as peak passive torque, calf circumference, and maximal isometric plantar flexor torque, were greater in the uninvolved limb. Increased values for stiffness may predispose the muscle‐tendon unit to further damage. | Experimental | 12 |
| Contralateral tendon rupture risk is increased in individuals with a previous Achilles tendon rupture (2004) | Aroen, et al. | 168 patients, 142 males & 26 females, median age 38.5 years at time of injury, who had Achilles rupture between 1990 and 1997 at a Norway hospital. | Greatly increased risk of rupture of contralateral Achilles tendon in those who had a previous rupture on one side. The authors proposed that this could be due to a genetic predisposition for tendon ruptures, that the injury is caused by degenerative changes, or that disuse atrophy of the contralateral tendon due to immobilization of the injured leg contributed to the injury. | Retrospective Self‐Report Questionnaire | 11 |
| Intrinsic Risk Factors for the Development of Achilles Tendon Overuse Injury (2006) | Mahieu, et al. | 69 male officer cadets at the Belgian Royal Military academy, mean age 18 years. | 10/69 had Achilles overuse injuries during the 6 weeks of basic training. Those with lower plantar flexor strength and increased dorsiflexion ROM were at greater risk of this injury. Authors hypothesized that stronger muscle strength produces stronger tendons that could better deal with excessive force. | Cohort (Prospective) | 11 |
Appendix 4:
Ankle Re‐injury Papers
| Title | Author | Population (age, gender, activity) | Main Findings | Type of study | QUADAS |
|---|---|---|---|---|---|
| Invertor and evertor strength in track and field athletes with functional ankle instability (2011) | Edouard, et al. | Track and field female athletes between 15‐40 years old with a history of lateral ankles sprains | The evertor muscle strength was higher than the invertor muscle strength in the dominant side for all groups, except for the group with a previous history of ankle sprain. An elevated ankle Evertor/Invertor Ratio (> 1.0) has been identified as an important indicator of ankle sprain susceptibility; otherwise, it could be an invertor strength weakness in subjects with FAI. | Cross‐Sectional | 12 |
| The Effect of Lateral Ankle Sprain on Dorsiflexion Range of Motion, Posterior Talar Glide, and Joint Laxity (2002) | Denegar, et al. | 12 athletes, 5 males & 7 females, between 18‐22 years old with a history of lateral ankle sprain within the last 6 months who had returned to sport participation | Residual ligamentous laxity was commonly found following lateral ankle sprain. Dorsiflexion range of motion was restored in the population studied despite evidence of restricted posterior glide of the talocrural joint. Although restoration of physiological range of motion was achieved, residual joint dysfunction persisted. | Retrospective Study | 12 |
| Examining Neuromuscular Control During Landings on a Supinating Platform in Persons With and Without Ankle Instability (2011) | Gutierrez, et al. | 45 active, healthy participants between 18‐30 years old were divided into 3 groups: ankle instability, lateral ankle sprain, and control | When landing on a device built to simulate the mechanism of a lateral ankle sprain (supination), the ankle instability group displayed significantly increased preparatory and reactive peroneal activation, while the Lateral Ankle Sprain group demonstrated increased preparatory tibialis anterior muscle activation. | Controlled Laboratory Study | 12 |
| Mechanical Instability After an Acute Lateral Ankle Sprain (2009) | Hubbard, et al. | 16 subjects with a first‐time acute unilateral ankle sprain, 7 males & 9 females, mean age 19.5 years. 16 healthy controls, 7 males & 9 females, mean age 20.4 years. | The lack of significant differences in mechanical laxity over an 8‐week period suggests that natural recovery of laxity takes longer than 8 weeks. | Cohort | 11 |
| Serial testing of postural control after acute lateral ankle sprain (2001) | Hertel, et al. | 17 young adults, 9 males & 8 females, mean age 21.8 years who sustained unilateral acute mild to moderate lateral ankle sprains | Individuals with postural control impairments are likely to have larger COP excursions and thus, larger sum of excursions throughout a trial. Elevated measures of postural control during static SLS have not been shown to predict recurrent ankle sprain with prolonged functional ankle instability. However, the lack of balance training after acute LAS appears to predispose ankle‐injured subjects to recurrent sprain | Longitudinal | 11 |
| Intrinsic Risk Factors of Noncontact Ankle Sprains in Soccer (2012) | Fousekis, et al. | 100 professional soccer players, mean age 23.6 years who had sustained no injury for the past 6 months were assessed for ankle joint asymmetries | The logistic regression analysis revealed 3 significant predictors of noncontact ankle sprains: (A) eccentric isokinetic strength asymmetries of ankle dorsal and plantar flexors; (B) increased BMI; and (C) increased body weight. This study found that there is not an increased risk for lateral ankle ligament injury after suffering a prior ankle injury. | Cohort | 12 |
| Ipsilateral Hip Abductor Weakness After Inversion Ankle Sprain (2006) | Friel, et al. | Convenience sample of 23 individuals, between 18‐52 years old with a history of at least 2 ankle sprains to the same side | Significant weakness in the hip abductor muscles on the involved side as compared with the uninvolved limb of subjects was found with chronic ankle sprain, which can contribute to increased risk for re‐injury. | Ex‐Post Facto Design | N/A |
| Reinjury After Acute Lateral Ankle Sprains in Elite Track and Field Athletes (2009) | Malliaropoulos, et al. | 202 elite male and female Greek track athletes with acute lateral ankle sprains | Low‐grade ankle sprains result in a higher risk of re‐injury than high‐grade ankle sprains at a 24‐month follow‐up. Grade II injuries showed a significantly higher rate of re‐injury than grades I and III A. There was no significant difference in time between original injury and re‐injury based on grade of injury. | Cohort (Prognosis) | 12 |
| Tibiofemoral angle and its relation to ankle sprain occurrence (2009) | Pefanis, et al. | 45 high‐level basketball, soccer, and volleyball male athletes, mean age 23 years. | The factors contributing more to an ankle sprain were previous similar injury, followed by BMI, and age. TFA was proven to be statistically non‐significant and does not seem to be a factor that could increase the probability of spraining an ankle. | Prospective | 11 |
| The effect of Q‐angle on ankle sprain occurrence (2009) | Pefanis, et al. | 45 high‐level basketball, soccer, and volleyball male athletes, mean age 23 years. | The factors contributing more to an ankle sprain were previous similar injury, followed by BMI and age. Q‐angle was shown to be statistically non‐significant and does not seem to be a factor that could increase the chances of spraining an ankle. | Prospective | 11 |
| Intrinsic risk factors for inversion ankle sprains in male subjects (2005) | Willems, et al. | 241 male Phys. Ed. students, mean age 18.3 years who were freshman at the Ghent University. | 44 of the 241 sustained an inversion sprain within the 1‐3 year follow‐up, 4 sprained both ankles. Those with slower running speed, less cardiorespiratory endurance, less balance, decreased dorsiflexion muscle strength, decreased dorsiflexion ROM, less coordination, and faster reaction of the tibialis anterior and gastrocnemius muscles are at a greater risk of ankle sprains. | Prospective Cohort Study | 13 |
References
- 1.Hagglund M Walden M Ekstrand J Previous injury as a risk factor for injury in elite football: A prospective study over two consecutive seasons. Br J Sports Med. 2006;40(9):767‐772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Walden M Hagglund M Ekstrand J High risk of new knee injury in elite footballers with previous anterior cruciate ligament injury. Br J Sports Med. 2006;40(2):158‐62; discussion 158‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gabbe BJ Bennell KL Finch CF Wajswelner H Orchard JW Predictors of hamstring injury at the elite level of australian football. Scand J Med Sci Sports. 2006;16(1):7‐13 [DOI] [PubMed] [Google Scholar]
- 4.Zazulak BT Hewett TE Reeves NP Goldberg B Cholewicki J Deficits in neuromuscular control of the trunk predict knee injury risk: A prospective biomechanical‐epidemiologic study. Am J Sports Med. 2007;35(7):1123‐1130 [DOI] [PubMed] [Google Scholar]
- 5.Wainner RS Whitman JM Cleland JA Flynn TW Regional interdependence: A musculoskeletal examination model whose time has come. J Orthop Sports Phys Ther. 2007;37(11):658‐660 [DOI] [PubMed] [Google Scholar]
- 6.Brown C, N. Padua D, A. Marshall S, W. Guskiewicz K, M. Gribble P, A [Commentary on] hip kinematics during a stop‐jump task in patients with chronic ankle instability. J Athletic Train. 2011;46(5):461‐470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ageberg E Pettersson A Fridén T 15‐year follow‐up of neuromuscular function in patients with unilateral nonreconstructed anterior cruciate ligament injury initially treated with rehabilitation and activity modification: A longitudinal prospective study. Am J Sports Med. 2007;35(12):2109‐2117 [DOI] [PubMed] [Google Scholar]
- 8.Silder A Thelen DG Heiderscheit BC Effects of prior hamstring strain injury on strength, flexibility, and running mechanics. Clin Biomech (Bristol, Avon). 2010;25(7):681‐686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bressel E Larsen BT McNair PJ Cronin J Ankle joint proprioception and passive mechanical properties of the calf muscles after an achilles tendon rupture: A comparison with matched controls. Clin Biomech (Bristol, Avon). 2004;19(3):284‐291 [DOI] [PubMed] [Google Scholar]
- 10.Cook C Cleland J Huijbregts P Creation and critique of studies of diagnostic accuracy: Use of the STARD and QUADAS methodological quality assessment tools. J Man Manip Ther. 2007;15(2):93‐102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reiman MP Goode AP Hegedus EJ Cook CE Wright AA Diagnostic accuracy of clinical tests of the hip: A systematic review with meta‐analysis. Br J Sports Med. 2013;47(14):893‐902 [DOI] [PubMed] [Google Scholar]
- 12.Friel K McLean N Myers C Caceres M Ipsilateral hip abductor weakness after inversion ankle sprain. J Athletic Train. 2006;41(1):74‐78 [PMC free article] [PubMed] [Google Scholar]
- 13.Brockett CL Morgan DL Proske U Predicting hamstring strain injury in elite athletes. Med Sci Sports Exerc. 2004;36(3):379‐387 [DOI] [PubMed] [Google Scholar]
- 14.Warren P Gabbe BJ Schneider‐Kolsky M Bennell KL Clinical predictors of time to return to competition and of recurrence following hamstring strain in elite australian footballers. Br J Sports Med. 2010;44(6):415‐419 d [DOI] [PubMed] [Google Scholar]
- 15.Fousekis K Tsepis E Poulmedis P Athanasopoulos S Vagenas G Intrinsic risk factors of non‐contact quadriceps and hamstring strains in soccer: A prospective study of 100 professional players. Br J Sports Med. 2011;45(9):709‐714 [DOI] [PubMed] [Google Scholar]
- 16.Opar DA Williams MD Shield AJ Hamstring strain injuries: Factors that lead to injury and re‐injury. Sports Med. 2012;42(3):209‐226 [DOI] [PubMed] [Google Scholar]
- 17.Salmon L Russell V Musgrove T Pinczewski L Refshauge K Incidence and risk factors for graft rupture and contralateral rupture after anterior cruciate ligament reconstruction. Arthroscopy. 2005;21(8):948‐957 [DOI] [PubMed] [Google Scholar]
- 18.Gerber JP Marcus RL Dibble LE Greis PE Burks RT LaStayo PC Effects of early progressive eccentric exercise on muscle size and function after anterior cruciate ligament reconstruction: A 1‐year follow‐up study of a randomized clinical trial. Phys Ther. 2009;89(1):51‐59 [DOI] [PubMed] [Google Scholar]
- 19.Ernst GP Saliba E Diduch DR Hurwitz SR Ball DW Lower‐extremity compensations following anterior cruciate ligament reconstruction. Phys Ther. 2000;80(3):251‐260 [PubMed] [Google Scholar]
- 20.Rettig AC Liotta FJ Klootwyk TE Porter DA Mieling P Potential risk of rerupture in primary achilles tendon repair in athletes younger than 30 years of age. Am J Sports Med. 2005;33(1):119‐123 [DOI] [PubMed] [Google Scholar]
- 21.Aroen A Helgo D Granlund OG Bahr R Contralateral tendon rupture risk is increased in individuals with a previous achilles tendon rupture. Scand J Med Sci Sports. 2004;14(1):30‐33 [DOI] [PubMed] [Google Scholar]
- 22.Malliaropoulos N Ntessalen M Papacostas E Longo UG Maffulli N Reinjury after acute lateral ankle sprains in elite track and field athletes. Am J Sports Med. 2009;37(9):1755‐1761 [DOI] [PubMed] [Google Scholar]
- 23.Baroni BM Generosi RA Junior E Incidence and factors related to ankle sprains in athletes of futsal national teams [portuguese]. FISIOTER MOVIMENTO. 2008;21(4):79‐88 [Google Scholar]
- 24.Pefanis N Karagounis P Tsiganos G Armenis E Baltopoulos P Tibiofemoral angle and its relation to ankle sprain occurrence. Foot Ankle Spec. 2009;2(6):271‐276 [DOI] [PubMed] [Google Scholar]
- 25.Willems TM Witvrouw E Delbaere K Mahieu N Bourdeaudhuij I De Clercq D Intrinsic risk factors for inversion ankle sprains in male subjects: A prospective study. Am J Sports Med. 2005;33(3):415‐423 [DOI] [PubMed] [Google Scholar]
- 26.Denegar CR Hertel J Fonseca J The effect of lateral ankle sprain on dorsiflexion range of motion, posterior talar glide, and joint laxity. J Orthop Sports Phys Ther. 2002;32(4):166‐173 [DOI] [PubMed] [Google Scholar]
- 27.O'Sullivan K O'Ceallaigh B O'Connell K Shafat A The relationship between previous hamstring injury and the concentric isokinetic knee muscle strength of irish gaelic footballers. BMC Musculoskelet Disord. 2008;9:30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ageberg E Fridén T Normalized motor function but impaired sensory function after unilateral non‐reconstructed ACL injury: Patients compared with uninjured controls. Knee Surg Sports Traumatol Arthrosc. 2008;16(5):449‐456 [DOI] [PubMed] [Google Scholar]
- 29.Andrade MS Cohen M Picarro IC Silva AC Knee performance after anterior cruciate ligament reconstruction. Isokinetics Exerc Sci. 2002;10(2):81‐86. [Google Scholar]
- 30.Button K van Deursen R Price P Recovery in functional non‐copers following anterior cruciate ligament rupture as detected by gait kinematics. PHYS THER SPORT. 2008;9(2):97‐104 [DOI] [PubMed] [Google Scholar]
- 31.St Clair Gibson A Lambert MI Durandt JJ Scales N Noakes TD Quadriceps and hamstrings peak torque ratio changes in persons with chronic anterior cruciate ligament deficiency. J Orthop Sports Phys Ther. 2000;30(7):418‐427 d [DOI] [PubMed] [Google Scholar]
- 32.Bressel E McNair PJ Biomechanical behavior of the plantar flexor muscle‐tendon unit after an achilles tendon rupture. Am J Sports Med. 2001;29(3):321‐326 [DOI] [PubMed] [Google Scholar]
- 33.Mahieu NN Witvrouw E Stevens V Van Tiggelen D Roget P Intrinsic risk factors for the development of achilles tendon overuse injury: A prospective study. Am J Sports Med. 2006;34(2):226‐235 [DOI] [PubMed] [Google Scholar]
- 34.Edouard P Chatard J Fourchet F, et al. Invertor and evertor strength in track and field athletes with functional ankle instability. Isokinetics Exerc Sci. 2011;19(2):91‐96 [Google Scholar]
- 35.Hertel J Buckley WE Denegar CR Serial testing of postural control after acute lateral ankle sprain. J Athletic Train. 2001;36(4):363‐368 [PMC free article] [PubMed] [Google Scholar]
- 36.Bonfim TR Paccola C Barela JA Proprioceptive and behavior impairments in individuals with anterior cruciate ligament reconstructed knees. Arch Phys Med Rehabil. 2003;84(8):1217‐1223 [DOI] [PubMed] [Google Scholar]
- 37.Benjuya N Plotqin D Melzer I Isokinetic profile of patient with anterior cruciate ligament tear. Isokinetics Exerc Sci. 2000;8(4):229‐232 [Google Scholar]
- 38.Roberts D Andersson G Friden T Knee joint proprioception in ACL‐deficient knees is related to cartilage injury, laxity and age: A retrospective study of 54 patients. Acta Orthop Scand. 2004;75(1):78‐83 [DOI] [PubMed] [Google Scholar]
- 39.Courtney C Rine RM Kroll P Central somatosensory changes and altered muscle synergies in subjects with anterior cruciate ligament deficiency. Gait Posture. 2005;22(1):69‐74 [DOI] [PubMed] [Google Scholar]
- 40.Fonseca ST Ócarino J Silva P Guimarães R Oliveira M Lage CA Proprioception in individuals with ACL‐deficient knee and good muscular and functional performance. Res Sports Med. 2005;13(1):47‐61 [DOI] [PubMed] [Google Scholar]
- 41.Heroux ME Tremblay F Corticomotor excitability associated with unilateral knee dysfunction secondary to anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc. 2006;14(9):823‐833 [DOI] [PubMed] [Google Scholar]
- 42.Williams GN Barrance PJ Snyder‐Mackler L Buchanan TS Altered quadriceps control in people with anterior cruciate ligament deficiency. Med Sci Sports Exerc. 2004;36(7):1089‐1097 [DOI] [PubMed] [Google Scholar]
- 43.Brown C Padua D Marshall SW Guskiewicz K Individuals with mechanical ankle instability exhibit different motion patterns than those with functional ankle instability and ankle sprain copers. Clin Biomech. 2008;23(6):822‐831 [DOI] [PubMed] [Google Scholar]
- 44.Palmieri‐Smith R McLean SG Ashton‐Miller J Wojtys EM Association of quadriceps and hamstrings cocontraction patterns with knee joint loading. J ATHLETIC TRAIN. 2009;44(3):256‐263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Palmieri‐Smith R Hopkins JT Brown TN Peroneal activation deficits in persons with functional ankle instability. Am J Sports Med. 2009;37(5):982‐988 [DOI] [PubMed] [Google Scholar]
- 46.Santilli V Frascarelli MA Paoloni M, et al. Peroneus longus muscle activation pattern during gait cycle in athletes affected by functional ankle instability: A surface electromyographic study. Am J Sports Med. 2005;33(8):1183‐1187 [DOI] [PubMed] [Google Scholar]
- 47.Mitchell A Dyson R Hale T Abraham C Biomechanics of ankle instability. part 1: Reaction time to simulated ankle sprain. Med Sci Sports Exerc. 2008;40(8):1515‐. [DOI] [PubMed] [Google Scholar]
- 48.Mitchell A Dyson R Hale T Abraham C Biomechanics of ankle instability. part 2: Postural sway‐reaction time relationship. Med Sci Sports Exerc. 2008;40(8):1522‐1528 [DOI] [PubMed] [Google Scholar]
- 49.Ross SE Guskiewicz KM Examination of static and dynamic postural stability in individuals with functionally stable and unstable ankles. Clin J Sport Med. 2004;14(6):332‐338 [DOI] [PubMed] [Google Scholar]
- 50.McKeon PO Hertel J Spatiotemporal postural control deficits are present in those with chronic ankle instability. BMC Musculoskelet Disord. 2008;9:76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Refshauge KM Kilbreath SL Raymond J Deficits in detection of inversion and eversion movements among subjects with recurrent ankle sprains... including commentary by vandervoort AA with authors' response. J Orthop Sports Phys Ther. 2003;33(4):166‐176 [DOI] [PubMed] [Google Scholar]
- 52.Sefton JM Hicks‐Little C Hubbard TJ, et al. Sensorimotor function as a predictor of chronic ankle instability. Clin Biomech. 2009;24(5):451‐458 [DOI] [PubMed] [Google Scholar]
- 53.DeVita P Hortobagyi T Functional knee brace alters predicted knee muscle and joint forces in people with ACL reconstruction during walking. J APPL BIOMECH. 2001;17(4):297‐311 [Google Scholar]
- 54.Tecco S Salini V Calvisi V, et al. Effects of anterior cruciate ligament (ACL) injury on postural control and muscle activity of head, neck and trunk muscles. J Oral Rehabil. 2006;33(8):576‐587 [DOI] [PubMed] [Google Scholar]
- 55.Binder‐Macleod B Buchanan TS Tibialis anterior volumes and areas in ACL‐injured limbs compared with unimpaired. Med Sci Sports Exerc. 2006;38(9):1553‐1557 [DOI] [PubMed] [Google Scholar]
- 56.Rudolph KS Axe MJ Snyder‐Mackler L Dynamic stability after ACL injury: Who can hop? Knee Surg Sports Traumatol Arthrosc. 2000;8(5):262‐269 [DOI] [PubMed] [Google Scholar]
- 57.Paterno MV Ford KR Myer GD Heyl R Hewett TE Limb asymmetries in landing and jumping 2 years following anterior cruciate ligament reconstruction. Clin J Sport Med. 2007;17(4):258‐262 [DOI] [PubMed] [Google Scholar]
- 58.Nakasa T Fukuhara K Adachi N Ochi M The deficit of joint position sense in the chronic unstable ankle as measured by inversion angle replication error. Arch Orthop Trauma Surg. 2008;128(5):445‐449 [DOI] [PubMed] [Google Scholar]
- 59.Hewett TE Torg JS Boden BP Video analysis of trunk and knee motion during non‐contact anterior cruciate ligament injury in female athletes: Lateral trunk and knee abduction motion are combined components of the injury mechanism. Br J Sports Med. 2009;43(6):417‐422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Boling MC Padua DA, Alexander Creighton R Concentric and eccentric torque of the hip musculature in individuals with and without patellofemoral pain. J Athl Train. 2009;44(1):7‐13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ferber R Noehren B Hamill J Davis IS Competitive female runners with a history of iliotibial band syndrome demonstrate atypical hip and knee kinematics. J Orthop Sports Phys Ther. 2010;40(2):52‐58 [DOI] [PubMed] [Google Scholar]
- 62.Kiesel KB Butler RJ Plisky PJ Prediction of injury by limited and asymmetrical fundamental movement patterns in american football players. J Sport Rehabil. 2014;23(2):88‐94. [DOI] [PubMed] [Google Scholar]
- 63.Plisky PJ Rauh MJ Kaminski TW Underwood FB Star excursion balance test as a predictor of lower extremity injury in high school basketball players. J Orthop Sports Phys Ther. 2006;36(12):911‐919 [DOI] [PubMed] [Google Scholar]
- 64.Plisky PJ Gorman PP Butler RJ Kiesel KB Underwood FB Elkins B The reliability of an instrumented device for measuring components of the star excursion balance test. N Am J Sports Phys Ther. 2009;4(2):92‐99 [PMC free article] [PubMed] [Google Scholar]