It is being gradually recognized that portal vein thrombosis (PVT) is negatively associated with the prognosis of cirrhosis.[1,2] But the standard treatment algorithm remains lacking.[3] Anticoagulation, which is a widely available treatment option for venous thromboembolism, is also employed for the management of PVT in cirrhotic patients.[4] Retrospective case series demonstrated a relatively low risk of anticoagulation-related bleeding and a high rate of portal vein recanalization after anticoagulation,[3,4] which provided the preliminary support for the use of anticoagulation in cirrhosis with PVT. However, the clinicians are very cautious of the potential bleeding secondary to anticoagulation, because cirrhosis itself has a bleeding tendency.
In the dilemma of whether or not anticoagulation therapy should be employed, the investigators would rather pay more attention to the natural history of PVT in cirrhosis in the absence of any interventions. To our knowledge, spontaneous portal vein recanalization in cirrhosis has been evaluated by at least three previous case series.[5,6,7] The incidence of spontaneous recanalization varies from 30% to 50% in cirrhotic patients with PVT.
In this issue of The Saudi Journal of Gastroenterology, the concept of spontaneous portal vein recanalization has been further reinforced.[8] The investigators found that partial PVT could be spontaneously recanalized or unchanged in 72.7% (16/22) of patients, and worsened in only 27.3% (6/22) of patients.[8] More importantly, in spite of a small sample size (n = 22), the study showed a significantly higher incidence of hepatic decompensation and mortality in the cirrhotic patients with worsened PVT than in those with recanalized or unchanged PVT.[8] In line with the previous studies,[5] these impressive findings suggested that anticoagulation therapy should be selectively performed in patients who would develop the thrombus extension, thereby improving survival; by contrast, it is unnecessary in those who would develop the spontaneous thrombus resolution. However, the accurate predictors of spontaneous recanalization remain poorly recognized in this study. Therefore, the behavior to stop any interventions for partial PVT in all cirrhotic patients might be radical.
In accordance with previous studies,[5] the investigators also found that the severity of liver function (i.e. MELD score) was the only independent predictor for the survival and hepatic decompensation in the multivariate Cox regression analysis. In the absence of any detailed information, we fail to clearly understand whether or not the progression of PVT had been incorporated as a variable into the multivariate analysis. But it appeared to be rational that the worsened PVT and deteriorated liver function jointly increased the mortality. This consideration could be potentially supported by the accumulated evidence regarding a vicious cycle between the development of PVT and deterioration of liver function [Figure 1]. First, the portal vein flow velocity decreases with worsening liver fibrosis and liver function.[9,10] Subsequently, a decreased portal vein flow velocity predicts a higher risk of developing PVT.[11] portal vein flow velocity decreases with worsening liver fibrosis and liver function.[9,10] Subsequently, a decreased portal vein flow velocity predicts a higher risk improved liver function, thereby producing the scouring effect and spontaneously resolving the thrombus within the portal vein.[12]
Figure 1.
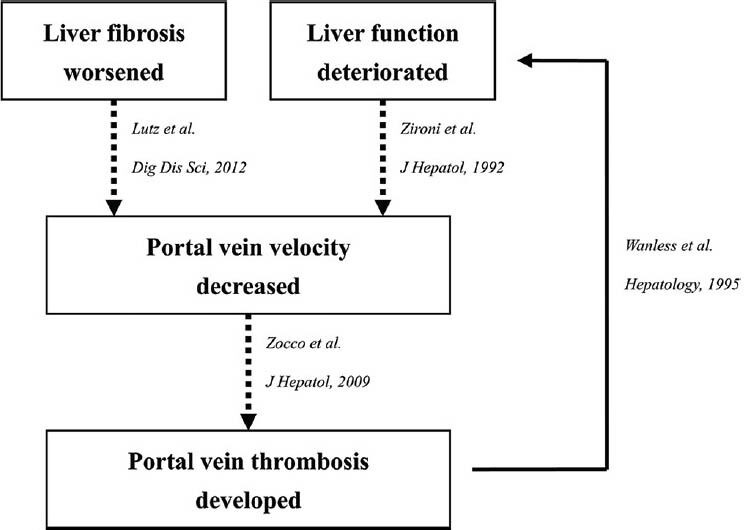
A scheme regarding the association between the severity of liver function and development of portal vein thrombosis
Collectively, spontaneous portal vein recanalization can be frequently observed in patients with partial PVT. This phenomenon may be attributed to the improvement of liver function. In addition, further work should focus on identifying the candidates who will develop the thrombus extension or is suitable for anticoagulation therapy.
REFERENCES
- 1.D’Amico G, de Franchis R Cooperative Study Group. Upper digestive bleeding in cirrhosis. Post- therapeutic outcome and prognostic indicators. Hepatology. 2003;38:599–612. doi: 10.1053/jhep.2003.50385. [DOI] [PubMed] [Google Scholar]
- 2.Qi X, Bai M, Yang Z, Yuan S, Zhang C, Han G, et al. Occlusive portal vein thrombosis as a new marker of decompensated cirrhosis. Med Hypotheses. 2011;76:522–6. doi: 10.1016/j.mehy.2010.12.007. [DOI] [PubMed] [Google Scholar]
- 3.Qi X, Han G, Fan D. Management of portal vein thrombosis in cirrhosis. Nat Rev Gastroenterol Hepatol. 2014;11:435–46. doi: 10.1038/nrgastro.2014.36. [DOI] [PubMed] [Google Scholar]
- 4.Qi X, Han G, Wu K, Fan D. Anticoagulation for portal vein thrombosis in cirrhosis. Am J Med. 2010;123:E19–20. doi: 10.1016/j.amjmed.2010.03.019. [DOI] [PubMed] [Google Scholar]
- 5.Luca A, Caruso S, Milazzo M, Marrone G, Mamone G, Crino F, et al. Natural course of extrahepatic nonmalignant partial portal vein thrombosis in patients with cirrhosis. Radiology. 2012;265:124–32. doi: 10.1148/radiol.12112236. [DOI] [PubMed] [Google Scholar]
- 6.Maruyama H, Okugawa H, Takahashi M, Yokosuka O. De novo portal vein thrombosis in virus-related cirrhosis: Predictive factors and long-term outcomes. Am J Gastroenterol. 2013;108:568–74. doi: 10.1038/ajg.2012.452. [DOI] [PubMed] [Google Scholar]
- 7.John BV, Konjeti R, Aggarwal A, Lopez R, Atreja A, Miller C, et al. Impact of untreated portal vein thrombosis on pre and post liver transplant outcomes in cirrhosis. Ann Hepatol. 2013;12:952–8. [PubMed] [Google Scholar]
- 8.Girleanu I, Stanciu C, Cojocariu C, Boiculese L, Singeap A, Trifan A. Natural course of non malignant partial portal vein thrombosis in cirrhotic patients. Saudi J Gastroenterol. 2014;20 doi: 10.4103/1319-3767.141687. In this issue. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lutz HH, Gassler N, Tischendorf FW, Trautwein C, Tischendorf JJ. Doppler ultrasound of hepatic blood flow for noninvasive evaluation of liver fibrosis compared with liver biopsy and transient elastography. Dig Dis Sci. 2012;57:2222–30. doi: 10.1007/s10620-012-2153-0. [DOI] [PubMed] [Google Scholar]
- 10.Zironi G, Gaiani S, Fenyves D, Rigamonti A, Bolondi L, Barbara L. Value of measurement of mean portal flow velocity by Doppler flowmetry in the diagnosis of portal hypertension. J Hepatol. 1992;16:298–303. doi: 10.1016/s0168-8278(05)80660-9. [DOI] [PubMed] [Google Scholar]
- 11.Zocco MA, Di Stasio E, De Cristofaro R, Novi M, Ainora ME, Ponziani F, et al. Thrombotic risk factors in patients with liver cirrhosis: Correlation with MELD scoring system and portal vein thrombosis development. J Hepatol. 2009;51:682–9. doi: 10.1016/j.jhep.2009.03.013. [DOI] [PubMed] [Google Scholar]
- 12.Wanless IR, Wong F, Blendis LM, Greig P, Heathcote EJ, Levy G. Hepatic and portal vein thrombosis in cirrhosis: Possible role in development of parenchymal extinction and portal hypertension. Hepatology. 1995;21:1238–47. [PubMed] [Google Scholar]


