Summary
While the origins of child psychiatry in Britain can be traced to the interwar period, contemporary concepts and methodological approaches to pathological mental development in children were not created until the 1950s and 1960s. It was at this time that one of the most salient and lasting diagnoses in child psychiatry, autism, was established through a network of intellectual, institutional, and legal changes in Britain. This article argues that the work of child psychiatrists at the Maudsley Hospital was central in driving these changes and uses archival sources from this hospital, along with other legal and intellectual sources, to explore attempts to conceptualize pathological thought in infants in the 1950s and 1960s. When the first epidemiological study of autism was published in 1966, this finally established the autistic child as a scientific, demographic, and social reality in Britain.
Keywords: autism, psychosis, social science, Maudsley Hospital, Britain, mental deficiency, children, Mental Health Act 1959, institutional care
In 1953, Dr. Elwyn James Anthony and Dr. Kenneth Cameron founded a “psychotic clinic” for the intensive observation and study of children suffering from major psychosis or schizophrenia at the Maudsley Hospital, London, United Kingdom. The children who were observed at the clinic during the 1950s were usually aged between three and nine years and were referred from schools, hospitals, and child guidance clinics across Britain. The early 1950s also saw the establishment of several other similar centers in the United Kingdom.1 In June 1955, Mildred Creak, prior head of child psychiatry at the Maudsley, then based at Great Ormond Street Hospital, noted that there were “five centers up and down the country where psychotic children are accepted, mostly on a regional basis.”2 Many of these referred their patients to the Maudsley for intense observations.3 This article proposes that the establishment of the Maudsley psychotic clinic laid the theoretical and institutional foundations for the recognition and treatment of autism in Britain. Child psychiatrists such as Creak, Anthony, and Cameron sought to undermine and challenge government policy concerning the care, education, and institutionalization of children then classed under law as “defective” and “ineducable.” They encouraged educationalists, parents, and government officials to regard these children as mentally ill and treatable. The categories of schizophrenia and psychosis were initially used to diagnose these children, but the category of autism came to replace these diagnoses by the 1960s.
There has recently been a growth in literature on the history of the autism diagnosis. Adam Feinstein’s A History of Autism: Conversations with the Pioneers presents detailed theories on the causes and treatment of autism put forward since the 1930s but does not describe the legal, institutional, social, or theoretical context in which these theories arose.4 Chloe Silverman’s Understanding Autism explores the history of autism in the United States, focusing on the role that parent groups have played since the 1960s in demanding better care and treatment and forming their own organizations, schools, and even gene banks in order to challenge and contest what they regarded as psychological fallacies.5 She also described how parents reacted to psychologists and influential public figures such as Bruno Bettleheim, Leo Kanner, and Ivar Lovaas. As Silverman pointed out, autism is currently a highly contested and controversial diagnosis. A 2006 study in the Lancet posited a rate of 116.1 per 10,000 children in the United Kingdom, which translates to over 1 percent of the total U.K. child population.6 The increased public presence of autism has attracted the attention of psychiatrists, social scientists, and literary analysts.7 The sociologist Gil Eyal has pointed out that, in the United States and other Western countries, diagnoses of autism rose after institutions for the “mentally retarded” were closed down.8 This led to a blurring of boundaries between what was traditionally regarded as mental retardation and what was increasingly regarded as mental illness. This article claims that, prior to the closure of institutions for defective children described by Eyal and the growth of parental campaigns described by Silverman, child psychiatrists were already using the diagnoses of psychosis and autism to challenge conventional beliefs about mentally abnormal children and their care and treatment. By examining the historical relationship among the law, child psychiatry, and the origins of autism research in the 1950s, it becomes clear that child psychiatrists influenced legal changes concerning the care, education, and socialization of atypical children. It was via these changes that autistic children progressively came to be recognized and identified.
Several historians have examined the history of child health, child guidance, and child psychology in Britain, but few have focused on the history of child psychiatry and the study of severe mental pathology in children.9 As Harry Hendrick and Nikolas Rose have pointed out, the establishment of much twentieth-century U.K. child law was influenced by psychological theory. For example, psychologists John Bowlby and Donald Winnicott gave evidence to the Curtis Committee, established in 1946 to investigate the “care of children deprived of a normal home life.”10 Their recommendations that healthy bonds between parents and children led to better mental health influenced the resulting 1948 Children’s Act. However, very few people have explored the influence of child psychiatry and descriptive psychopathology on U.K. child law.
German Berrios has argued that the most important mental symptom to be ascertained and diagnosed as part of descriptive psychopathology in adults was hallucination.11 This influenced the foundation of the central psychiatric concepts of psychosis, dementia praecox, and schizophrenia, which have driven the development of psychiatric treatments for adults.12 However, even the sparse literature on the history of child psychiatry as a discipline in Britain has largely overlooked the significance of these concepts to the development of mental health services for children.13 This article explores this aspect of the history of child welfare in depth. It examines cases of children diagnosed and treated as “psychotic,” “schizophrenic,” and “autistic” in the 1950s and 1960s and explores the way that psychiatrists used these diagnoses to challenge the therapeutic nihilism that surrounded the treatment of mentally ill children and to develop better health and welfare services for these children. It focuses on the work of the Maudsley Hospital and uses this work to explain broader shifts in the conceptualization and treatment of children with psychiatric problems in the United Kingdom. It argues that the category of autism has become a lasting epithet of the historical struggles for the recognition and acceptance of severely atypical forms of mental development in children.
The Background
The origins of both child psychology and psychiatry are intimately linked to the identification and institutionalization of children who could not function within the state-funded education system. In 1913, the Mental Deficiency Act was passed in Britain; the legislation enforced certification and custodial care of “defective” children.14 In the same year, Cyril Burt was appointed by the London County Council (LCC) as the first official psychologist in the world, and part of his job was to ensure that “defectives” were identified.15 By 1915 there were already 14,626 “defective” children in residential institutions for defectives or special schools in England and Wales, and by 1927 there were 17,337.16 In the late 1920s, the Commonwealth Fund, an American philanthropic body, provided money to improve “child guidance” techniques in the United Kingdom and also established the Diploma in Mental Health course at the London School of Economics (LSE).17 In 1928 the first child guidance clinic was established in London.18 All of these factors helped to establish child psychology as a discipline.
In 1923, the Maudsley Hospital opened as the first state mental hospital in Britain to admit voluntary patients for the treatment of mental illness.19 The Maudsley Hospital’s services for children were quickly identified and exploited by London Care Committees and other welfare agencies. This was particularly the case after 1929 when the Poor Law was dismantled and increasing numbers of poor and needy children were referred to the Maudsley for assessments. In line with this transition, Maudsley child psychiatrists created new categories to distinguish children who required specialist psychiatric care from those who could be dealt with by other social agencies.20 In 1937, Mildred Creak, then heading the child department at the Maudsley, argued that the study of psychosis and schizophrenia in children offered a “tremendous field . . . for observation and research” which could help to clarify the type of psychiatric help that any individual child may require.21 She called for further divisions and distinctions to be made in child psychiatry. Diagnosis was particularly important when it came to the distinction between a mental illness and a mental defect because the latter required institutionalization by law. This distinction was notoriously difficult to make. The Maudsley often received referrals of children who were mute and/or extremely disturbed, and doctors did not know whether to refer them to mental deficiency institutions or whether to treat them as psychiatric cases. Creak claimed that a “no-man’s land . . . exists between the clear-cut picture of amentia and psychosis” in children. In other words, it was not easy to tell whether a child did not have a mind at all or whether the child had a mind that he or she had then lost.22 Further research into the causes and symptoms of childhood schizophrenia, a psychiatric disorder, would rectify this problem.
In the 1930s, several other child psychoanalysts and psychiatrists in both Britain and the United States began to use the terms “psychotic” and “schizophrenic” to describe children, such as Jacob Kasanin and Moses Kaufman at the Boston Psychopathic Hospital and Leo Kanner at Johns Hopkins University Hospital, Baltimore. Even as early as 1929, Melanie Klein in London argued that a child’s perception of reality could be disturbed to the extent that he or she could be described as experiencing a type of “psychosis.”23 Klein argued that child psychiatrists often misdiagnosed schizophrenia and psychosis as “arrested development,” “mental deficiency,” “psychopathic condition,” or “asocial tendency.”24 At child guidance clinics across Britain during the 1930s and 1940s, psychologists and social workers still used colloquial categories such as “backwards,” “difficult,” and “unmanageable.” Creak and a growing number of psychiatrists regarded schizophrenia research as the harbinger of reliable and accurate measures in child psychiatry. In 1937, Mildred Creak published a paper on the unusual form that psychoses took when they manifest themselves in infants and children.25
Kanner’s work has received much attention within the popular understanding of the history of autism. However, in Britain, it was the Maudsley and its offshoots that provided the foundations for the increase in diagnoses of childhood psychosis and autism in children and that also pioneered epidemiological studies internationally. Kanner’s definitions of autism were often critiqued.26 Furthermore, discussions about what constituted psychosis, schizophrenia, and autism in Britain were largely framed by previous British work on subnormality and mental deficiency and were influenced by wider international debates regarding the concepts of psychosis and schizophrenia (of which autism was a symptom).
British child psychiatrists’ claims to scientific legitimacy in diagnosis were important because they took place while the administration of social welfare for children in Britain was under reconstruction. In 1942, the Beveridge Report on Social Insurance and Allied Services presented plans for British postwar reconstruction and the reorganization of social services, providing a blueprint for the welfare state. After the war, the Family Allowances Act of 1945 and the National Insurance Act of 1946 led to the introduction of family allowances and comprehensive welfare assistance. The National Health Service (NHS) Act, which was passed in 1948, supported these acts with national medical assistance. The 1948 Children’s Act also ensured that all children were visible to government networks and eligible for assistance.
The postwar period witnessed a sustained campaign to improve the health of the general population, in particular children. Prior to the NHS Act, the routine medical inspection and treatment of children had largely taken place via the School’s Medical Service. As Bernard Harris has argued, postwar improvements in the general health of the child population led the school’s health services to shift their attention to psychological and speech therapies.27 The postwar period also witnessed a public recognition of the problems of child abuse, and strategies were created for dealing with this problem.28 Public child care practice was professionalized, and emphasis was placed on the rehabilitation of problem families and reduction of juvenile crime. Child health was recognized as a problem that could be tackled through social interventions, such as parental education, as well as medical interventions. Within this new organization of welfare, any psychological diagnosis that a child was given could greatly influence the support and/or coercion that the child received via government welfare agencies.
The 1945 Handicapped Pupils and School Health Regulations that supported the 1944 Education Act compelled authorities to provide special education to all children who could be classed under the following eleven labels: (1) blind, (2) partially sighted, (3) deaf, (4) partially hearing, (5) delicate, (6) diabetic, (7) educationally subnormal, (8) epileptic, (9) maladjusted, (10) physically handicapped, (11) those suffering from speech defects.29 Defective children were still catered for under Mental Deficiency Law, but “psychotic” children were not recognized under British law and technically received no special welfare entitlements or provisions. In 1948, the Ministry of Education (MoE) issued a circular that directly implicated medically trained psychiatrists in the diagnosis and treatment of “maladjusted” children. This prompted the employment of child psychiatrists in all child guidance clinics across the country, leading to a growth and dispersal of the profession.30 However, child psychiatrists still had their hands tied when it came to diagnosis and treatment. In 1950, the Underwood Committee began to investigate the treatment and prevention of “maladjustment” in children, and their 1955 report focused on the importance of keeping families together. “Maladjustment” was a broad term that described a child’s inability to control his or her instincts according to social requirements. As Rose has pointed out, the Underwood report was influential to the organization of general welfare services to children, in particular professionals associated with the Kleinian or Tavistock School.31 However, it was not well received among child psychiatrists, many of whom had been trained at the Maudsley.32 In 1955, Kenneth Cameron, head of child psychiatry at the Maudsley, criticized the entire concept of “maladjustment,” arguing that it was simply “a neutral word utilized to cover a group for whom special provision is required.” He was concerned that the concept was becoming reified as a clinical entity in a similar way to the legal term “insanity” and the social term “delinquency” and regarded this as a misunderstanding of medical science.33
Because the Mental Deficiency, Education, and NHS Acts made no mention of the concepts of childhood psychosis or schizophrenia, the children diagnosed with these conditions had no legal rights to long-term treatment or education. The Maudsley psychotic clinic was founded partly to get “childhood psychosis” recognized as a legal category and also to reinforce the role of medically trained child psychiatrists in determining the treatment that psychotic children received. On the other hand, because these children were neither theorized nor classified under law, Maudsley doctors were left with a considerable amount of creative freedom in their work, freedom that they would not have had in the treatment of children diagnosed with conditions listed in the 1945 regulations.
The Psychotic Clinic
My special purpose is the reinstatement of the psychotic within the theoretical framework of our normal practice. . . . Too often and for far too long we have stood outside and regarded him with increasing theoretical bewilderment as his behaviour continued to transgress the laws of orthodox psychopathology. . . . Getting inside the psychotic child is by no means an impossible phenomenological undertaking.
—Elwyn James Anthony, 195834
When Anthony and Cameron founded the “psychotic clinic” at the Maudsley in 1953, their goal was to use the concepts of schizophrenia and psychosis to understand the development of all forms of pathological thought in infants and children. In doing this, they aimed to give both scientific legitimacy and political clout to the discipline of child psychiatry. All children who attended the psychotic clinic were admitted as inpatients for “two weeks [of] observation and investigation” as part of the “psychotic survey programme” and were then referred elsewhere for residential placements.35 Many were kept on as outpatients. Anthony and Cameron’s clinic differed from others established at a similar time because the staff focused on generating observations for the purposes of research. It was because of this that “child psychotics” from other reception centers were often referred to the Maudsley for observation. For instance, Alan Cash-more sent many of his patients from Booth Hall Hospital, Manchester.36 The foundation of the psychotic clinic strengthened the reputation of the Maudsley as a reception center for the most severe cases of childhood psychiatric disorder.
During the interwar period the Maudsley children’s department had been inundated with requests to assess the needs of children suffering from malnutrition, neglect, or other indications of poverty, as well as serving as an evaluation center for schools. It thus took on the function of a sorting ground for human types, rather than a research center, and did not have the facilities to study or treat children over the long term.37 This situation altered radically in the postwar period when new administrative centers were set up to cater for the basic problems of malnutrition, child care, and family management. Child psychiatrists were then able to focus on severe psychopathology as they were able to retain severely ill children who would have previously been directed straight to deficiency institutions. In 1946, Aubrey Lewis required that all psychiatric trainees spend six months in the children’s department to ensure that they would receive a comprehensive education.38 When, in July 1948, the Maudsley Hospital was granted NHS funding, its position as the primary U.K. training center in psychiatry was confirmed.
Anthony was a British-born medical doctor who had trained under Aubrey Lewis, clinical director of the Maudsley, in the late 1940s.39 In 1951 he was granted a Nuffield fellowship to study with Jean Piaget at the Institute Jacques Rousseau in Geneva.40 On his return, the first academic post in child psychiatry was created for him as senior lecturer in child psychiatry at the Maudsley.41 By the mid-1950s, Anthony was also lecturing at the LSE and presenting at the British Psychological Society, the LCC Child Welfare Officers, and the Association for Workers of Maladjusted Children.42 Cameron had joined the Maudsley in 1939 after working with Leo Kanner and Adolf Meyer on a Rockefeller fellowship in Baltimore and took charge of the children’s department after the war. He had previously studied medicine in Edinburgh and specialized under David Henderson. He had a strong interest in the classification of disease entities in child psychiatry.43
The diagnosis of psychosis and schizophrenia in infants and children was not straightforward, as these categories had initially been used to classify adults. In addition, they already contained fixed assumptions about the nature of infantile thought. The word “psychosis” had been coined as an alternative to insanity by the Austrian doctor Ernst von Feuchtersleben in his 1845 textbook, translated into English two years later as the Principles of Medical Psychology.44 In 1901, Adolf Meyer noted that the term “psychosis” was being widely adopted in psychiatric literature to designate “an abnormal mental condition, specially [sic] inasmuch as it is correlated with a specific disease- process.”45 In 1894, Freud had defined psychosis as hallucinatory confusion and claimed that such lack of contact with reality was caused by the ego, or self, needing to break away from an idea that was irrevocably tied to real events.46 In 1905, he expanded on these ideas, adopting Havelock Ellis’s concept of autoerotism in order to explain the origins of what he termed “psychical reality” in infants. He argued that in autoerotic activity, satisfaction could be achieved through both self-stimulation and hallucination. This activity made infants independent of their external world and gave them a sense of control over a reality that they had not yet mastered. This type of hallucinatory thought could recur later in life.47
In 1911, Eugen Bleuler used Freud’s work on infantile hallucinations to describe the unconscious processes that characterized psychotic thought in his classic text Dementia Praecox or the Group of Schizophrenias. Bleuler had coined the term “schizophrenia” from the Greek meaning “split-mind,” drawing the concept of split consciousness from the French alienist Pierre Janet.48 He claimed that the “detachment from reality, together with the relative and absolute predominance of the inner life” that characterized the most severe cases of schizophrenia should be described as “autism.”49 When Bleuler coined the term “autism” in 1911, he claimed it was both an expansion of Freud’s concept of “autoerotism” and a refinement of what Janet had called perte de la fonction du réel.50
It was via the work of Freud, Bleuler, and Jean Piaget that Maudsley child psychiatrists first began to use the concepts of schizophrenia, psychosis, and autism to diagnose children. In 1922, Piaget gave a paper at the International Conference on Psychoanalysis in Berlin in which he developed Freud and Bleuler’s theories of infantile thought. Piaget argued that children’s thinking in general showed many analogies with unconscious symbolism as described in psychoanalytic theory.51 He later described autistic thought as the first stage in the development of normal intelligence. Autistic thought was not yet adapted to external reality or the processes of reasoning and was instead closely associated with dreams and affective wishes. It was only when a child developed other intellectual processes that he or she could move beyond autistic dream-like thought.52
Anthony and Cameron argued that the meaning of “psychosis” when applied to children needed clarification. Cameron argued that Klein had expanded the meaning of psychosis to describe common states of fear and anxiety that were part of normal child development, leading to “an almost indefinite extension of the term ‘psychotic’ to include cases which no clinician would regard as such.”53 In 1943, Leo Kanner used his own cases to construct a hypothesis concerning the existence of a unique psychological disorder characterized by “extreme autism, obsessiveness, stereotypy, and echolalia” in children. These symptoms brought “the total picture into relationship with some of the basic schizophrenic phenomena.”54 However, Anthony argued that Kanner had merely “come across constellations of symptoms recurring with a frequency suggesting some stable clinical entity.” He had not adequately described the etiology of that entity, thus making its legitimacy as a fixed clinical category somewhat dubious.55 Anthony and Cameron saw the psychotic clinic as a way to clear up this confusion and to establish a firm basis for child psychiatry.
Observing and Measuring the Psychotic Child
The architecture of the Maudsley Children’s Department enabled the close surveillance of children from virtually every standpoint. Children could be placed under constant observation by nurses in a centralized ward or in glass-fronted rooms. During playtimes, they remained easily observable in two bright and spacious recreation rooms.56 Although Anthony and Cameron provided the theoretical impetus for the psychotic clinic, the majority of the observational work was conducted by nurses. Every nurse was given the brief to closely observe the children whom she was also employed to care for. Doctors encouraged nurses to describe each child’s use of language and to illustrate his or her awareness of other people and objects. As one registrar put it, he was “interested in observations of [the child’s] autistic behaviour when absorbed in his play—arm movements, expressions, verbalisations.”57
Nurses’ reports were read by Anthony, Cameron, and other registrars, who would then correct their descriptions. For example, when one nurse began her observations in 1954, she initially portrayed her six-year-old male patient using language similar to that of social workers modeled on the Kleinian or Tavistock style of psychology. Her descriptions were infused with assumptions about the way that children should relate to one another.58 However, after further instruction and a request to focus on the boy’s “autistic behaviour,” she began to produce detailed accounts of the child’s individual behavior and speech. Each action that the child carried out, as well as everything that he said, was recorded. In particular, the nurse described all behavior that appeared to have some bearing on the child’s perceptual awareness and his ability to understand concepts. For example, one account read,
He dresses himself but is very slow needing constant verbal encouragement, “is this the vest?” he asks, “is this the right way up?,” etc. with every garment. He understands “upside down” and “the wrong way up” but is puzzled by “inside out.”59
The above observation is typical of those recorded in the 1950s because of the training that nurses received.
Central to these accounts were detailed descriptions of the child’s vocalizations. If children were unable to speak, then emphasis would be placed on the noises they made and whether these were imitative. It was thought that these accounts could demonstrate the child’s contact with reality by showing his or her ability to respond to external stimuli. If children were capable of using language, then nurses would record their words in full. Many repeated set idioms and phrases or exhibited echolalia or abnormal intonation. Others presented with more unusual speech abnormalities. For example, one patient was reported to “add the word ‘after’ wherever possible and doesn’t respond to correction.”60 Reports such as these highlighted speech abnormalities that signaled a lack of affective rapport. Nurses would pay attention to the children’s use of personal pronouns, which could indicate their capacity to distinguish themselves from others—the fundamental milestone in the psychoanalytic and Piagetian model of child development. Many of the children in the psychotic clinic referred to themselves in the third person or would confuse themselves with other people. In fact, Cameron considered that, in terms of diagnosis, any “inability to distinguish between first and third person . . . suggests psychosis.”61
For the doctors, the most treasured depiction of a child’s individual thoughts and fantasies came in the form of detailed accounts of that child’s speech when he or she was engrossed in thought. Nurses would record every single word that the child spoke when they observed these situations. The following extract is from a transcript of one child’s speech that covered scores of pages. Such accounts were common. They represented occasions where children described their own desires and emotions and were thus viewed as the only legitimate documentation of these phenomena:
The child speaks to herself continually. Her conversation:
“She wants to go out to tea, do you want to go out to tea, Friday, you ought to go. Your handies cold warm them up (puts them on radiator) dicky birds, little baby ones, do you want to sit on that (potty) sit on the potty, put her there. Little monkey get out of the way.”62
These words were thought to be a window onto psychotic states of mind. For Anthony and Cameron, who oversaw the production of this discourse, they could reveal the thinking processes that later led to adult schizophrenia.
All of the children in the psychotic clinic were given a battery of tests on arrival to determine their physiological functions and levels of intellectual and social development. These included X-rays, brain scans, tests on the nervous system, and standardized psychological tests. All children were tested using encephalography to measure the electrical charges in their brain. Wasserman and Kahn tests for syphilis were given, as were cardiolipine tests for thrombosis. Some of the children were also photographed or filmed.63 A standardized form covering aspects of the nervous system, circulatory system, respiratory system, alimentary system, and urinary system was completed in full. The child’s weight, height, and complexion were recorded, as were any “deformities or stigmata.” In measuring the child’s nervous system, “involuntary movements,” “tremors,” and “tics” would be noted, as would “deep reflexes,” “superficial reflexes,” and every twitch, reflex, or expression that would indicate the functioning of the cranial nerves (Figure 1). This information could assist Anthony and Cameron in their measurement of biological functioning at the sensory-motor level and its influence on the child’s psychological state.
Figure 1.
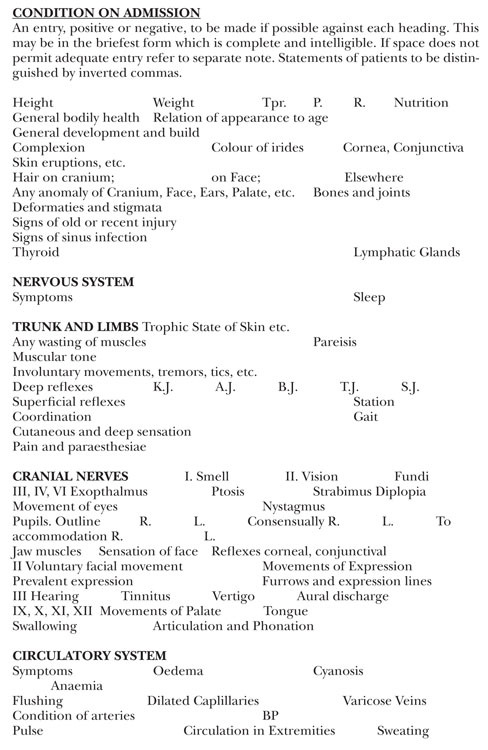
Typed copy of the first page of the “Condition on Admission” form used to collect information from children in the psychotic clinic in the 1950s. Source: Maudsley Hospital Autism Archive.
The most common form of intelligence test used on psychotic children in the 1950s was the Wechsler Intelligence Scale for Children. Other tests measured specific aspects of each child’s motor development and perceptual functions such as the Vineland Social Maturity Test, the Rorschach Test, and the Goodenough “Draw a Man” Test. The use of standard psychological tests alongside reflex and medical tests meant that a child’s conceptual development could be tallied with his or her functional abilities. The results formed the backbone of new theories of psychotic phenomena in children that divided “psychotic” children into types in an attempt to ascertain causes.
Anthony maintained that the causes of childhood psychosis were numerous and often took place simultaneously. He therefore postulated “an amalgam of forces that include constitutional, organic, genetic and psychogenic determinants and possibly some still unknown factor.”64 Anthony urged against any “monocausal” view of the condition, especially that which placed excessive emphasis on “schizophregenic” or “psychotogenic” parents. He noted that the role of disturbed parents in the etiology of the condition had been raised by Kanner as well as several other American doctors such as William Goldfarb from the Henry Ittleson Center for Child Research in New York.65 Goldfarb had described the mothers of autistic children as “wooden” and argued that these mothers added to the confusion of their children by lacking any form of direction.66 Anthony thought that this view was untenable if regarded as the sole cause of childhood psychosis. As he put it, “Not all ‘psychotogenic’ mothers produce psychotic children; nor are all the children of ‘psychotogenic’ mothers psychotic or the mothers of psychotic children ‘psychotogenic.’”67 On the other hand, he also criticized doctors and researchers who placed too
much emphasis on “organic” or “constitutional” factors in causation. He admitted that there were always cases in which organic factors may have played a part. For example, Lauretta Bender from Bellevue Hospital, New York, had identified neurological damage and evidence of encephalitis and encephalopathy in some of her cases of childhood schizophrenia.68 However, Anthony warned against making direct correlations between cause and effect. Taking the “multicausal” view, he drew up a “diagnostic schema” listing five different continua on which all cases of childhood psychosis could be placed. They could be placed on a “normal,” “deficiency,” “organic,” “neurotic,” or “psychopathic” continuum. Once identified on one of these continua, the severity of the child’s disturbance could also be measured “in terms of withdrawal, regression, rigidity, [and] the presence or absence of organic involvement.”69
In 1958, the European Journal of Child and Adolescent Psychiatry published Anthony’s article, “An Aetiological Approach to the Diagnosis of Psychosis in Childhood,” and this article was later quoted by virtually all Maudsley child psychiatrists.70 Anthony presented “the concept of psychosis . . . [in] relationship with other psychiatric disorders of childhood” in an attempt to merge psychoanalytic theory with the sciences of infant observation, symptomatology, and natural history in the Kraepelinian sense of tracking the development of an illness over time.71 Anthony argued that although all autistic and psychotic children displayed abnormalities in ego development, these disturbances followed different trajectories depending on the age of onset. In the case of primary autism, the infant’s constitutional barrier was “abnormally thick” and the infant developed “an unselective psychotic barrier with the result that he failed to emerge from his primary narcissism.” In cases of secondary autism, the constitutional barrier was “abnormally thin,” allowing an excessive amount of stimulation, which led the child to withdraw “behind a thick, unselective psychotic barrier which blankets the stimulation.” Anthony claimed that the “psychotic ego” failed to draw a distinction between “inner phantasy”and outer reality, resulting in an inability to relate to definable objects and identities. This engendered a state of defense manifest in stereotyped behavior and a withdrawal from sensory experiences. The psychotic child then formed “transitional relationships to inanimate objects” and engaged in “projection, introjection” and “denial.”72
Anthony worked hard to develop a theoretical model of childhood psychosis that would be taken seriously and used to challenge the bureaucracy in which he worked. He realized that clear criteria needed to be established, and he argued that within all cases of childhood psychosis and autism, there were “components of three basic conditions of malfunctioning.” These were, first, an inability to form a coherent and stable sense of self, second, an inability to “cathect” internal experiences accurately, leading to “difficulties in interpersonal relationships and displacement of affect onto things,” and, third, “a confusion of self and non-self and disturbances in the perception of the self.”73 Anthony named this last problem “a-dualism,” borrowing the term from Piaget.74 This triad of “malfunctions” would later form the basis for all autism research at the Maudsley.75
Treating the Psychotic Child
Prior to the establishment of the psychotic clinic, children diagnosed with schizophrenia or psychosis at the Maudsley in the late 1940s and early 1950s were often given very intensive and invasive treatments ranging from insulin shock and drug therapies to intensive psychoanalysis. For example, in 1955, Cameron reported the case of one psychotic girl who had begun to deteriorate at the age of three and who was treated at age eight “by insulin comas without benefit ‘and during the course of treatment died from subarachnoid haemorrhage.’”76 Another nine-year-old boy admitted in 1950 was given insulin shock treatment over a period of twenty-six weeks.77 Cameron later admitted that “[i]nsulin treatment has been disappointing in pre-pubertal cases.”78 No children were treated with insulin shock after the late 1950s.
In place of insulin shock and psychoanalysis, the establishment of the psychotic clinic saw the introduction of more sedate therapeutic measures, in particular “occupational therapy” or “school therapy.” Anthony and Cameron believed that if children’s psychological problems were acknowledged, then they could be educated and trained to their potential. “Occupational therapy” was usually conducted by nurses who socialized the children and taught them to live independently.79 Some children from the psychotic clinic were referred to special schools where they were given speech therapy. Many children were sent to one of several Rudolph Steiner Schools across Britain with headquarters on Harley Street. The superintendent, Karl König, acted as consultant for cases at the Larfield Hall School in Kent, the Salmon’s Cross School in Surrey, and the Murtle House School in Aberdeen, where former patients of the Maudsley psychotic clinic were sent. Cameron and König often corresponded on the diagnosis of children and their progression.80 The Maudsley kept in contact with Steiner Schools and other similar institutions and formed strong institutional, intellectual, and administrative bonds with them. They worked together to see how “psychotic” children developed as they grew, finding that their symptoms sometimes improved. Anthony and Cameron were interested in diagnoses in order to enable cure, but they had no long-term treatment facilities and had to observe children’s development from afar.
Referral to a defective institution was a last resort but often considered necessary, as the following extract about a six-year-old boy from a 1958 letter from Cameron reveals:
By now it is clear that this boy developed a psychotic illness at the very end of 1955, of which you must have seen the initial phase of withdrawal, muteness, loss of toilet habits, etc. . . . The prognosis is not good and he may have to be dealt with ultimately under the mental deficiency acts.81
In the cases where a psychotic child was deemed to be mentally defective, there was sometimes an appeal by the parents. Correspondence and discussions pending the appeal could take place over months or even years as the parents sought to postpone decisions, and these would continue if the appeal was upheld. Maudsley doctors corresponded with county medical officers and representatives of local education authorities in these cases. For example, in 1954, the principal school medical officer of West Sussex County Council, J. S. Bradshaw, claimed that one child who was attending the Maudsley clinic was, in the words of the 1944 Education Act, “suffering from a disability of mind of such a nature or to such an extent as to make him incapable of receiving education at school.” The child’s parents claimed that their child should be sent to a special school rather than a defective institution, where he would be “doomed for life.” Anthony commiserated with the parents. He told Bradshaw that “it is difficult to explain to parents that there is nothing wrong with the child’s brain and yet the child is not normal.”82 However, parental appeals were not usually successful in the 1950s, and Anthony and other Maudsley psychiatrists knew that the only way to fully challenge bureaucratic inertia was to develop new models of child psychosis as a treatable condition.
The Law Concerning Psychotic and Autistic Children in the 1960s
In the 1950s, Maudsley researchers began to publish studies that claimed that “mentally defective” children were able to progress given the correct diagnoses and training. After the NHS Act was passed in 1948, Mental Defective Institutions became the responsibility of Regional Hospital Boards under the Ministry of Health (MoH). The practices of care used within them were suddenly opened up to new scrutiny by institutions supported by the Medical Research Council (MRC), in particular the Unit for Research in Occupational Adaptation, which was an adjunct to the Maudsley Hospital and also headed by Aubrey Lewis.83 In 1951, Jack Tizard and Neil O’Connor from the Maudsley’s MRC Unit argued that the motor skills, performance, intelligence, and personality of defectives could be improved so that they might be capable of even employment and life outside an institution.84 The idea that defective children of “imbecile” level could be educated challenged the view that institutional care was the only option. In line with work emanating from the psychotic clinic, such studies encouraged new conceptualizations of the treatment of mentally abnormal children.
Many who worked in deficiency institutions pointed out the difficulties of supervising large groups of child “defectives” in institutions (Figure 2). Statistics obtained from the Board of Control for the year 1955 revealed a total of 141,164 “defectives” certified under the Mental Deficiency Act.85 Although this figure included adults, the majority of all defective cases were certified and institutionalized during childhood. From the total of 6,386 “defectives” ascertained in 1954, 73 percent had been referred by Local Education Authorities.86 In conjunction with that of researchers at the MRC Unit, Anthony and Cameron’s work challenged the laws that were preventing psychotic children from developing to their full potential. By maintaining contact with Steiner schools and others, they argued that psychotic children could develop beyond their psychotic state. They called for more research and less institutional care.
Figure 2.
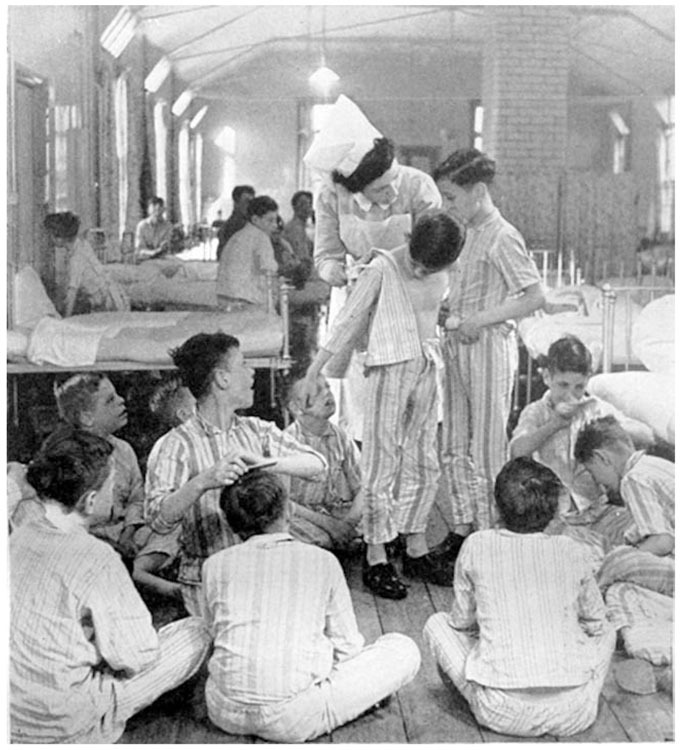
“A Ward for Imbeciles in a Mental Deficiency Hospital,” ca. 1956. First printed in Leslie Hilliard and Brian Kirman, Mental Deficiency (London: Churchill, 1957).
In 1954, the British government established the Royal Commission on the Law relating to Mental Illness and Mental Deficiency.87 The commission was established following growing dissent concerning the civil liberties of the mentally ill, in particular following a 1953 report by the Third Expert Committee on Mental Health of the World Health Organization. The resulting Percy Report (1957) argued that any individuals with “mental” or “personality” problems and illnesses should be treated under the law “with no more restriction of liberty or legal formality than is applied to people who need care because of other types of illness, disability or social or economic difficulty.”88 It discredited most legal powers that had been employed to compel the mentally defective and insane to institutional treatment.89 However, the rights and liberties of psychotic and schizophrenic children were not clear in the resulting legislation.
In 1959, the Mental Health Act was passed; the act brought the recommendations of the Percy Report into force.90 Following this, the terms “defective,” “idiot,” “imbecile,” and “feeble-minded” were all abandoned as legal terms and replaced with the terms “subnormal,” “severely subnormal,” and “psychopathic disorder.”91 The Percy Report had argued that the term “psychopathic” should replace the earlier terms “feeble-minded” and “moral defective,” and other “pathologically mentally abnormal” persons who would not previously have been classed as “mentally defective.”92 A number of debates then ensued in parliament regarding this definition of “psychopath,” which many regarded as too broad.93 In the act, psychopathy was eventually defined as “a persistent disorder or disability of mind (whether or not including subnormality of intelligence) which results in abnormally aggressive or seriously irresponsible conduct on the part of the patient, and requires or is susceptible to medical treatment.”94 Subnormality was defined in relation to intelligence, but, similarly to psychopathy, it had to be “susceptible to medical treatment or other special care and training of the patient.”95 In both cases, a type of child was created in law who was “mentally disordered” yet susceptible to treatment, and this type of child entirely replaced the “defective” child who was legally incapable of social transformation. However, what was to be done with this new social entity was not clear.
It was still the duty of the medical officer to determine whether or not a child was educable. However, now the legal status of children who were ineducable included both children who would have previously been termed “defective” and those who were increasingly coming to be called “psychotic.” It therefore conflated these conditions in the eyes of the law. Most important, section 8 of the Children Act, 1948, and subsection 6 of section 5 of the Matrimonial Proceedings (Children) Act, 1958, which had given powers to medical officers to remove children from the care of local authorities and place them in hospitals and defective institutions, then ceased to have any effect.96 Local Authority Children’s Departments then assumed responsibility for all children, whether educable or not, unless they were thought to require specific short-term hospital treatment for mental disorder.
The concepts of childhood psychosis and autism were first raised in parliament in May 1960. William Compton Carr, Conservative member of Parliament (1959–64), questioned the parliamentary secretary to the MoH, Edith Pitt, on why responsibility for “mentally handicapped” children did not come under the MoE. The prospect of improving the mental capacity of such children, or “upgrading” them, was steadily growing, and he argued that the government should be at the forefront of this:
The most exciting thing, which is still a frontier to be crossed, is the work on causes and treatment of so-called autistic—sometimes called schizoid, sometimes psychotic—children, which is almost unknown territory. These children are apparently schizoids who live in a dream world. They seem intelligent, but it is impossible to touch them even with treatment that is nowadays giving success in 75 per cent of normal adult schizoids. We must pay attention to that factor.97
Prior to 1959, the developing subjectivity of children with severe mental health problems was not of interest to many people other than Anthony, Cameron, Creak, and other child psychiatrists working at psychotic clinics. However, after the Mental Health Act was passed, the subject became an issue that was relevant to everyone involved in the NHS and Local Authority administration.
In 1961, the MoH began to collect information on “the nature and extent of the hospital inpatient accommodation which is needed for mentally ill and maladjusted children and adolescents.” All existing children’s units, including the Maudsley clinic, were enquired as to how many beds they had for children younger than twelve classed as either suffering from “behaviour problems requiring short-term treatment” or as “psychotic and others requiring long-term treatment.”98 There were sixteen inpatient units containing a total of 340 beds, mainly for short-term treatment. The draft paper for the Standing Mental Health Advisory Committee (SMHAC) stated that provision was immediately required for children who needed long-term hospital treatment and that the Maudsley Hospital had stated this case most strongly. The committee suggested that around twenty-five beds per region would be required for long-term psychiatric treatment of children. However, the committee was still unclear as to how many children actually had psychosis and thus would require special treatment. They had no clear information on numbers and, as a government department, found this frustrating.99
In 1961, Mildred Creak and Kenneth Cameron joined together with several others to draw up a definitive list of diagnostic points that could identify psychotic children. By this time, Anthony had moved to the United States. There was no clear consensus on the terminology that should be used to describe the problem that the committee was identifying. While some members had wanted to call the phenomenon “psychosis in childhood,” others had preferred the “more specific” term “childhood schizophrenia.” In the end, the committee reached a compromise with the awkward term “schizophrenic syndrome in childhood.” The committee agreed on nine diagnostic points that they claimed were crucial to a diagnosis: (1) gross and sustained impairment of emotional relationships with people; (2) apparent unawareness of his own personal identity; (3) pathological preoccupation with particular objects; (4) sustained resistance to change in the environment; (5) abnormal perceptual experience; (6) acute, excessive and seemingly illogical anxiety; (7) speech may have been lost or never acquired; (8) distortion in motility patterns; (9) a background of serious retardation in which islets of normal, near normal, or exceptional intellectual function or skill may appear.100
Creak’s team shelved Anthony’s aim to discover etiology until they could reach consensus with other researchers and government departments. Creak argued that if all psychiatrists could agree on the same diagnostic features then this “would clear the way towards a common understanding and recognition of the phenomenological composition of the syndrome” and toward better treatment options. These nine diagnostic points came to be well known by all those working in the field of childhood psychosis and autism research and care.101
In 1958, the Maudsley’s MRC Unit was renamed the Social Psychiatry Research Unit and the focus shifted to prevalence-rate and epidemiological studies of psychiatric disorder to assist government administration. For example, in 1960, Jack Tizard began a major study on the administrative prevalence of “subnormal” children, finding a rate of 3.45 per 1,000 in Middlesex.102 Many Maudsley researchers were becoming interested in this aspect of autism and psychosis research, in particular Tizard, John and Lorna Wing, and Michael Rutter. At the time, Rutter was gaining ground as a leading child psychiatry researcher particularly interested in psychiatric epidemiology as a means to identify causation. He had studied under both Aubrey Lewis and Hans Eysenck at the Maudsley and also under the psychiatric epidemiologist Ben Pasamanick in New York.103 In May 1965 Rutter was appointed as senior lecturer in child psychiatry, thereby filling the post that had been left vacant since Anthony’s departure in 1958.104 In the early 1960s, Rutter had estimated the rate of autism in Aberdeen after analyzing a sample of 120 children who had already been referred to special agencies. He proposed a rate of 3.3 per 10,000 population, although he acknowledged that more research was needed.
In 1963, the Wings, then at the MRC Unit, wrote a memorandum to the SMHAC that aimed to clarify the educational and hospital services that autistic children required. The Wings pointed out that a review of seventy-four cases seen by Anthony and Cameron (whom the Wings now classed as autistic) had found that 37 percent had a “nuclear” form that did not affect their intelligence and were thus educable.105 They then used Rutter’s work to provide a figure on which they should base service provision. The Wing’s memorandum was sent to the SMHAC by the Society for Autistic Children (SAC), a parent-led organization which had been established in January 1962 as the Autistic Children’s Aid Society of North London. Their aim was to provide long-term residential care “for the treatment and education of autistic or psychotic children” as well as to improve scientific research and public understanding.106 Three years later, Bernard Rimland and other parents formed a similar society in the United States. As Chloe Silverman has pointed out, parent groups were significant as they advocated strongly for children diagnosed with psychosis and autism. In the United Kingdom, SAC campaigned directly to the MoE and the MoH and pushed through reforms to ensure that children diagnosed with these conditions received education. However, it is important to recognize that they did this by working closely with doctors and researchers at the Maudsley to inform government departments and the public. The Wing memorandum was taken seriously by the MoH and MoE and led to further studies funded by the MRC Unit.
The first ever epidemiological study of autism was supervised by J. K. Wing and Neil O’Connor from the MRC Unit and conducted by Victor Lotter. Lotter surveyed all children in Middlesex aged between eight and ten years to generate a percentage figure for the rate of autism in the U.K. population. Lotter drew directly from the 1961 working party’s nine diagnostic points, although he discarded the point “apparent unawareness of his own personal identity.” This was in order to “avoid unnecessary assumptions about what is going on in the child’s mind.”107 Creak had claimed that it was “impossible” to use purely behavioral criteria to indicate “the presence of an impaired capacity for human relationships.”108 However, the Wings and Lotter considered that clear-cut purely behavioristic criteria were paramount to the development of reliable research on “autism” regardless of the fact that the psychological state of autism concerned the capacity to relate to others. The Wings argued that “autism” was preferable to schizophrenia as a diagnostic label “because of its neutrality and lack of implications about aetiology and prognosis.”109 Using these criteria, along with information collected through the education and social welfare systems, Lotter argued that the prevalence rate for autism was 4.5 per 10,000 population.110
Lotter’s epidemiological study offered new possibilities for the analysis of children’s developmental and psychological problems using social-psychiatric methods. Drawing from childhood psychosis research, it established autism, the major symptom of childhood psychosis, as a label that could be used in the rapidly changing landscape of mental health care for children. This label has stuck precisely because it provided security and certainty to parents, bureaucrats, psychiatrists, social scientists, and others who witnessed the changes ushered in by the 1959 Mental Health Act. The fact that autism was then recognized as an administrative and medical category was a major milestone for child psychiatrists as well as all those affected by the diagnosis. Following publicity campaigns by SAC, Lotter’s epidemiological study was reported in ten national newspapers, and this increased public awareness of the condition.111
Following the 1959 Mental Health Act, many parents began to use section 57 of the 1944 Education Act to appeal against decisions that their child was “ineducable.” In 1963, SAC had made a deputation to the Ministers of Education and Health calling for all autistic children to become the responsibility of the Education rather than the Health authorities. SAC also argued that the ministry must give grants to teach autistic children in independent schools if Local Authority Schools could not provide proper education for them.112 However it was not until Lotter’s epidemiological study that the government began to act. A debate in the House of Commons in February 1966 on “mentally handicapped children” had highlighted the fact more information was needed on the precise number of children with “autism” and other “mental handicaps.”113 In March 1966, a meeting was held with HM school inspectors and the MoE to discuss the educational needs of psychotic children, and the question of “exactly how many children there were in England and Wales who were psychotic or autistic” was again raised.114 When Lotter’s study was finally published, it provided a figure for government to work with. Once this figure was available, the possibility of treating and educating these children became a reality. Tizard was consulted directly as to how many teachers would be required to teach autistic children (400–500 were proposed) and where they would be trained.115 The planning and organization of services for psychotic and autistic children in the mid-1960s was thus driven directly by research conducted at the MRC’s Social Psychiatry Research Unit.
In January 1966, a report was published by the British Psychological Society (BPS), “Children in Hospitals for the Subnormal.” This quoted widely from work by the MRC’s Social Psychiatry Unit such as Tizard’s famous Brookland’s experiment.116 All of these studies recommended small-scale well-funded family-style educational units employing behavioral and speech therapies rather than large institutions that thwarted the child’s social, intellectual, and verbal development. The BPS report claimed that “children who show autistic or psychotic symptoms—at least 10 percent of the admissions in the present survey—tend to become even more withdrawn if left to their own devices.”117 O’Connor later used psychological tests to investigate which behavioral techniques would be most effective for teaching “autistic” children by measuring their “sensory dominance.”118
These studies were extremely important in guiding the future of hospital and social services for children. When the Seebohm Committee reported on Local Authority and Allied Services in 1968, they recommended that Local Authority Social Services Departments should be established and children with mental health problems should be managed via these departments rather than Health Departments.119 In 1966 Rutter requested £2,000 from the newly renamed Department of Education and Science (DES) to conduct a study on the special educational treatment of autistic children at a school in Ealing set up by SAC.120 The DES, along with the Gulbenkian Foundation, funded this study, and the findings showed, among other things, that children who received individual tuition improved greatly. This evidence helped to create reform.
Although in 1968 the DES still refused to recognize autism as a specific handicap, they suggested that small educational units and parental guidance should be provided to all children with “severe learning and developmental problems.”121 Rutter’s work, which built on Anthony and Cameron’s foundations to build new theories of psychosis and autism, established a theory of child development that satisfied the hiatus left following the closure of mental deficiency institutions. In conjunction with the epidemiological work conducted by Lotter and others at the MRC Unit, the Maudsley group pushed through radical changes in health and educational reform for children diagnosed with subnormality, psychosis, and autism, and these changes had lasting effects.
The Establishment of Autism as a Legal Category
The Chronically Sick and Disabled Person’s Bill, 1970, enshrined the category of autism in law by listing it as a disability that ensured special education.122 This ensured that professional organizations such as schools and social work agencies paid attention to children so categorized. This was another major turning point that would not have been possible without a growing acceptance that children could suffer from major psychiatric disorder. Between 1960 and 1970, there had been a steady rise in numbers of children defined as both “maladjusted” and “educationally subnormal” attending specialist schools, and this was a direct result of the 1959 act, which removed the category of “mentally deficient” from legal terminology. In 1960, 1,742 children were classified as “maladjusted” and 32,815 were classed as educationally subnormal. In 1970, these figures had risen to 6,293 and 51,768, respectively.123
Following the Education (Handicapped Children) Act 1970, there was an increase in the numbers of children with psychosis and autism diagnoses attending special schools and special classes. The reason for this was the final closure of schools for all children with subnormality, which led to the need for additional specialist schooling facilities. Many children with autism, schizophrenia, and psychosis diagnoses were sent to language units such as the language unit attached to the Forest Oak special school in Solihull,124 the Charles Burns Unit for children with language and communication problems in Warwickshire,125 or the Brent Knoll Unit in Lewisham.126 Other children were sent to mixed special schools such as Court Meadow Special School in Sussex,127 the Dysart Special School in Surrey,128 or the J. F. Kennedy Special School in Newham.129 Some children were sent to Steiner Schools as in the 1950s, and many of these Steiner Schools reclassified themselves as schools for children with “severe learning difficulties,” such as Sunfield School in Worcestershire.130 Each of these schools had its own unique approach to the education of children, and each claimed to specialize in a particular type of child. Following the Helen Allison School and other schools of the Autistic Society, some special schools such as Doucecroft School in Essex were classified as schools specifically “for autistic children.”131
Between 1970 and 1975, the number of “maladjusted” children registered at the DES increased from 6,293 to 13,527, the number of physically handicapped pupils increased from 8,830 to a total of 12,224, the number of epileptic children rose from 1,015 to 2,205, and the number of children with a speech defect increased dramatically from 828 to 6,893. The number of “educationally subnormal” children shot up from 51,768 to 72,636, of whom 19,892 were given the new category of “severely educationally subnormal.” In addition, 542 children were registered under the new category “autistic.”132 In total, this showed an increase of 39,293 newly categorized children, a number comparable with 34,177 who were transferred from the Health Authority to the DES and then integrated into the education system through various classificatory routes after 1970. The discrepancy in figures can be accounted for by population increases, the growth of specialist education services generally, and the elimination of the category “delicate,” which had previously classified 1,729 children.133 It is clear from these figures that when “subnormal” or “defective” children were integrated into the general education system, they entered along many different routes and in doing so assumed many different classifications, such as “speech disorder,” “maladjusted,” and “autistic.” These figures also show the beginnings of a legal recognition of the fact that children could be “autistic.”
Although the category of autism was used to classify a few children only in 1970, its appeal would gradually expand as children’s psychiatric needs were increasingly recognized in an educational setting. In 1973, Margaret Thatcher, then minister of education, proposed a committee “to review educational provision in England, Scotland and Wales for children and young people handicapped by disabilities of body or mind.”134 Rutter had previously met with Thatcher and had discussed his research with her.135 The resulting Warnock Committee based many of their plans for special educational provision on Rutter’s work. In 1964, Rutter, Tizard, and Kingsley Whitmore, senior medical officer from the DES, embarked upon a series of surveys on the Isle of Wight, claiming that 6.8 percent suffered from “psychiatric disorder.” This study sparked a number of comparative surveys generating further statistics.136
The Warnock Committee based service provision on these prevalence-rate studies. However, they argued that responses should always be tailored to the individual child.137 The committee proposed that the term “learning difficulties” should be applied to all children with any kind of special educational need and that all previous categories such as “maladjusted” and “educationally subnormal” should be abolished. This abolition of central concepts that had previously assisted with the administration of children with psychological problems left another large gap in the descriptive terminology used by the educational bureaucracy. This gap came to be filled with the autism category. In 1979, Lorna Wing and Judith Gould used Anthony’s work on classification to define what they termed a triad of “impairments” rather than malfunctions. They also claimed that their triad could be found in children within a broader phenotype of “autism,” claiming that 20 in 10,000 children had this condition.138
The 1981 Education Act, which became law on April 1, 1983, stated that all Local Education Authorities must draw up statements, which were legally binding contracts between the authority and the child’s parents.139 In 1983, The DES and the Department of Health and Social security issued a joint statement to all LEAs stating that each child’s “special educational needs” should be regarded as specific to him or her and that each child must be given individual support to overcome these problems. This approach was diametrically opposite to that which had institutionalized children as “defective,” and this new model fitted much more neatly with a descriptive model of child development pioneered by Maudsley researchers.
Maudsley psychiatric studies were fundamental to reframing the legal status of children with psychological diagnoses within the education system. It was through the operation of the “statementing” system that educational psychologists, parents, parent-led organizations, teachers, bureaucrats, administrators, and psychiatrists began to work together to propagate and disseminate categories that had been developed by child psychiatrists of the 1950s and 1960s. Autism had become the most salient of those categories because it referred to an individual state of mind that could be measured using psychiatric definitions and altered using educational means. Today the number of children on the “autistic spectrum” in Britain is thought to be over 1 in every 100 children, and this is an artifact of these historical foundations.140
Conclusion
Maudsley child psychiatrists and psychological researchers of the 1950s and 1960s railed against institutional solutions to psychological problems and argued that severe psychopathology in children needed to be studied in detail before therapeutic, educational, and political decisions were made on behalf of mentally ill children. In doing this, they created new categories for the classification of children’s developmental problems and argued that these were scientifically grounded in the study of severe psychopathology. When laws concerning the institutionalization of defectives were relaxed in 1959, it was the psychiatric categories of childhood psychosis and autism to which social-scientific researchers turned rather than concepts used by the previous generation of psychological researchers.
Many epidemiological studies of autism have been conducted since Lotter’s first study. They have all employed this category, which became established through the psychotic clinics established in Britain in the 1950s and which became an administrative and epidemiological category in the 1960s. This article has explored the work of the psychotic clinic at the Maudsley Hospital, the leading training institute for child psychiatrists since the 1940s. This clinic had been established to create a scientific basis to the study of psychological disturbance in infants and children. Psychiatrists such as Creak, Anthony, and Cameron argued that psychotic children formed a significant subsection of the population who, if studied in detail, provided the key to understanding the development of infantile thought in general. They worked in depth with individual cases in order to understand child psychotics’ inner thoughts, their formation of concepts, and how they understood their relationship to others.
After 1959, psychotic children came to be recognized under law, and their inability to relate to others was thought of as a symptom that could be broken down into behavioral units and measured. It was via this measurement that “autism” became established as a social-scientific entity and later as a legal category that ensured special educational provision. Creak and Cameron were the first to construct a list of diagnostic points for the “schizophrenic syndrome in childhood” that could be used in statistical studies. Lotter’s study of autism, which drew from these diagnostic points, was part of a wider expansion of the epidemiological method in child psychiatry and developmental psychology. Psychiatrists of the 1950s presented this category to epidemiologists, social scientists, and policy makers as a legitimate focus of research and administration. This category has since proved influential to child psychiatry, psychology, and general theories of child development. It has also become extremely influential to the classification of children with special educational needs.
Chloe Silverman is correct in arguing that parents have played a major role in driving increases in diagnoses of autism. However, in Britain, parental groups such as SAC, later renamed the National Autistic Society, would have had no foundations and would have not moved forward in their efforts were it not for the existence of the Maudsley Hospital, the Institute of Psychiatry, and the MRC’s Social Psychiatry Research Unit. These interconnected institutions laid the groundwork for parents to campaign by providing new ways to consider abnormal child development and by using their studies to challenge government policy toward the health and education of children classed as “psychotic” and “autistic.” The work of researchers such as Creak, Anthony, Rutter, Tizard, Lotter, and the Wings continues to influence government policy, parental interventions, and even self-advocacy work in the United Kingdom. Internationally, it has enabled autism to be regarded as an epidemiological entity, and this has had repercussions through subsequent epidemiological studies conducted worldwide. In short, Maudsley research of the 1950s and 1960s set the foundations for major legal changes concerning the care and education of autistic children that continue to influence perceptions of what autism is and how it can be treated.
Acknowledgments
The author wishes to thank Professor John Forrester and Edgar Jones. Many thanks also go to Professor Sir Michael Rutter, Professor Patrick Bolton, and all the staff at the MRC Social, Genetic and Developmental Psychiatry Centre for their assistance with the project. Thanks are also due to the staff of the U.K. National Archives. Finally, the author wishes to thank the Wellcome Trust for supporting this research under grant numbers 077889 and 086071.
Biography
Bonnie Evans is a Wellcome Trust Postdoctoral Fellow at Queen Mary, University of London. She is conducting a project entitled “Neuroscience, Psychology and Education: Autism in the UK 1959-2014.” She is interested in the development of psychology, psychoanalysis, psychiatry, and related neurosciences in the twentieth and twenty-first centuries. She completed her Ph.D. at the Department of History and Philosophy of Science, Cambridge University, in 2010 on the origins of child psychiatry and childhood schizophrenia research and its influence on contemporary theories of autism. Her thesis was awarded the International Society for the History of the Neurosciences 2012 award for Outstanding Student Essay in the History of the Neurosciences. After completing her Ph.D., she worked as a postdoctoral researcher at King’s College, London’s Centre for Medical Humanities. Her first monograph, The Origins of Autism, is contracted with Manchester University Press and is due out later this year. She can be contacted at b.evans@qmul.ac.uk.
Footnotes
Letter—Cameron to Cashmore, 10/28/58, Maudsley Hospital Autism Archive (MHAA) 573500 (all numbers anonymized).
Letter—Creak to Elliot, County Medical Officer, Maidstone, 6/24/55, MHAA: 926185.
Letter—Cashmore to Anthony, 10/30/57, MHAA: 573500.
Feinstein Adam. A History of Autism: Conversations with the Pioneers (West Sussex, UK: Wiley-Blackwell; 2010
Silverman Chloe. Understanding Autism (Princeton: Princeton University Press; 2011
Baird Gillian, Simonoff Emily, Pickles Andrew, Chandler Susie, Loucas Tom, Meldrum David, Charman Tony. “Prevalence of Disorders of the Autism Spectrum in a Population Cohort of Children in South Thames,” Lancet 368 9531 (2006): 210–15.
Murray Stuart. Representing Autism (Liverpool: Liverpool University Press; 2008. 175–76. Nadesan Majia Holmer. Constructing Autism (London: Routledge
Eyal Gil, Hart Brendan, Oncular Emine, Oren Neta, Rossi Natasha. The Autism Matrix (Cambridge: Polity; 2010
Levene A. “Family Breakdown and the ‘Welfare Child’ in 19th and 20th Century Britain,” Hist. Fam. 11 2 (2006 67 79 Stewart John. “U.S. Influences on the Development of Child Guidance and Psychiatric Social Work,” in Public Health and Preventive Medicine 1800–2000 Andresen Astri. (Bergen: Stein Rokkan; 85–95, Thom Deborah. “Wishes, Anxieties, Play, and Gestures,” in In the Name of the Child, ed. Cooter Roger. (London: Routledge; 1992): 200–19.
Rose Nikolas. Governing the Soul (London: Free Association; 1999): 170–73. Hendrick Harry. Child Welfare (London: Routledge; 1994): 196–99.
Berrios German E. The History of Mental Symptoms (Cambridge: Cambridge University Press; 1996
Beer M. Dominic. “Psychosis,” Hist. Psychiatry 6 no. 22 (1995): 177 200
Hersov L. “Child Psychiatry in Britain,” J. Child Psychology Psychiatry 27 no. 6 (1986): 781–801. Wardle C. J. “Twentieth-Century Influences on the Development in Britain of Services for Child and Adolescent Psychiatry,” Brit. J. Psychiatry 159 (1991): 53–68, Warren W. “You Can Never Plan the Future by the Past,” J. Child Psychology Psychiatry 11 (1971): 241–57.
Thomson Mathew. The Problem of Mental Deficiency. Oxford: Clarendon; 1998. p. 33.
Sutherland Gillian, Sharp Stephen. Ability, Merit and Measurement. Oxford: Clarendon; 1984. p. 55.
Ibid., 297.
Stewart “U.S. Influences”. (9)
Thom “Wishes, Anxieties, Play, and Gestures”. (9):207.
Allderidge Patricia. “The Foundation of the Maudsley Hospital,” in 150 Years of British Psychiatry 1841–1991, ed. Berrios German E., Freeman Hugh. (London: Gaskell; 1991. 79–88. Jones Edgar, Rahman S., Woolven R. “The Maudsley Hospital,” Med. Hist. 51 no. 3 (2007): 358,, 363
Evans Bonnie, Rahman Shahina, Jones Edgar. “Managing the ‘Unmanageable’: Interwar Child Psychiatry at the Maudsley Hospital, London,” Hist. Psychiatry 19 no. 4 (2008): 454–75.
Creak Mildred. “Psychoses in Children,” Proc. Roy. Soc. Med. 31 (1938): 519–28., quotation on 528.
Ibid., 525.
Klein Melanie. “Personification in the Play of Children,” Int. J. Psychoanal. 10 (1929): 193–204., esp. 195.
Klein Melanie. “The Importance of Symbol Formation in the Development of the Ego,” Int. J. Psychoanal. 11 (1930): 24–39., quotations on 36–37.
Creak “Psychoses in Children” (n. 21 520–21.
Anthony Elwyn James. “An Aetiological Approach to the Diagnosis of Psychosis in Childhood,” Acta Paedopsychiatrica: The European Journal of Child and Adolescent Psychiatry 25 (1958): 90; Creak Mildred. “Schizophrenic Syndrome in Childhood,” Brit. Med. J. 2 (1961): 889–90.
Harris Bernard. The Health of the Schoolchild (Buckingham: Oxford University Press; 1995
Hendrick Harry. Child Welfare (London: Routledge; 1994. 11
Phtiaka Helen. Special Kids for Special Treatment? (London: Falmer; 1997. 9
Wardle “Twentieth-Century Influences” (n. 13 58, Warren “You Can Never Plan” (n. 13 244–45.
Rose N. S. Governing the Soul, 2nd ed. (London: Free Association Books; 1999. 176–77.
Hersov “Child Psychiatry” (n. 13 785
Cameron Kenneth. “Diagnostic Categories in Child Psychiatry,” Brit. J. Med. Psychology 28 (1955): 67–71.
Anthony Elwyn James. “An Experimental Approach to the Psychopathology of Childhood: Autism,” Brit. J. Med. Psychology 31 (1958): 211–25., quotation on 211–12.
Letter—Cameron to Frederic De Havas, Salmon’s Cross School, 7/21/54, MHAA: 448773; Letter from L. Wilson (Maudsley Registrar) 6/20/55, MHAA: 979317.
Letter—Cashmore to Anthony, 10/30/57, MHAA: 573500.
Evans Rahman, Jones “Managing the ‘Unmanageable’” (n. 20
Hersov “Child Psychiatry” (n. 13 784
Shepherd Michael. Conceptual Issues in Psychological Medicine (London: Routledge; 1990. 134
Institute of Psychiatry, Annual Report 1950–1951, 13
Institute of Psychiatry, Annual Report 1951–1952, 15; Hersov “Child Psychiatry” (n. 13 793
Elwyn James Anthony, “Group Therapeutic Techniques for Residential Units,” Case Conference 4 no. 6 (1957); Anthony Elwyn James. “Other People’s Children,” Case Conference 5 no. 2 (1958); Anthony Elwyn James. “The Significance of Jean Piaget for Child Psychiatry,” Brit. J. Med. Psychology 29 (1956): 20–34.
“Kenneth Cameron: Obituary,” Lancet 281 no. 7284 (1963): 782–83. Cameron Kenneth. “Symptom Classification in Child Psychiatry,” Acta Paedopsychiatrica 25 no. 6 (1958
Beer “Psychosis” (n. 12); Berrios German E. “Historical Aspects of Psychoses: 19th Century Issues,” Brit. Med. Bull. 43 no. 3 (1987): 484–98.
Meyer 1901, quoted in Berrios, “Historical Aspects of Psychoses” (n. 44 489`
Freud Sigmund. Standard Edition (London: Vintage; 2001 3:58
Ellis Havelock. Studies in the Psychology of Sex (London, 1899. 1:130–243. Freud Standard Edition, 7: 181–83.
Berrios History of Mental Symptoms (n. 11 188–89. Shorter Edward. A History of Psychiatry (New York: John Wiley; 1997. 107–9.
Bleuler Eugen. Dementia Praecox or the Group of Schizophrenias, trans. Zinkin Joseph. (1911; repr., New York: International Universities Press; 1950. 63
Ibid., 373–74; Ellenberger Henri F. The Discovery of the Unconscious (London: Penguin; 1970. 287–88., 406–7. Moskowitz A. “Pierre Janet’s Influence on Bleuler’s Concept of Schizophrenia,” Janetian Stud., no. 2 (November 2005
Chapman Michael. Constructive Evolution (Cambridge: Cambridge University Press; 1988. 121
Piaget Jean. The Language and Thought of the Child (1923; repr., London: Routledge; 2002. 44
Cameron Kenneth. “Psychosis in Infancy and Early Childhood,” Med. Press (1955): 280–83., quotation on 283.
Kanner Leo. “Autistic Disturbances of Affective Contact,” Nervous Child 2 (1943): 217–50., quotations on 248.
Anthony “Aetiological Approach” (n. 25 90
Creak Mildred. “Child Psychiatry at the Maudsley Hospital,” Amer. J. Psychiatry 97 no. 2 (1940): 395–400.
“Record for Nursing Staff,” 10/26/1954, MHAA: 874753.
Nurses’ notes, 10/19/54–10/26/54, MHAA: 874753.
Nurses’ notes 10/30/54, MHAA: 874753.
Nurses’ notes, 2/27/58, MHAA: 772931.
Case summary ca. 1954, MHAA: 874753.
Nurses’ notes, 10/29/53, MHAA: 893951.
Anthony Elwyn James. Clinical Aspects of Childhood Psychosis. 2nd Icp Zurich (Film, 1957
Anthony “Aetiological Approach” (n. 25 93
Meyers Donald. “Obituary: William Goldfarb,” Int. J. Psychoanal. 78 (1997): 391–92.
Goldfarb quoted in Anthony, “Aetiological Approach” (n. 25 92
Ibid., 92.
Bender L. “Clinical Study of One Hundred Schizophrenic Children,” Amer. J. Orthopsychiatry 17 (1947): 40–56., quotations on 53.
Anthony “Aetiological Approach” (n. 25 95
E.g., Rutter Michael. “Behavioural and Cognitive Characteristics,” 51–81., quotation on 55; and Wing J. K. “Diagnosis, Epidemiology, Aetiology,” 16, both in Early Childhood Autism: Clinical, Educational and Social Aspects, ed. Wing J. K. (London: Pergamon; 1966
Anthony “Aetiological Approach” (n. 26 94
Anthony “Experimental Approach” (n. 34 212
Anthony“Aetiological Approach” (n. 26
Anthony “Experimental Approach” (n. 34 222
Happé Francesca, Ronald Angelica. “The ‘Fractionable Autism Triad,’” Neuropsychology Rev. 18 no. 4 (2008): 287–304. Wing Lorna, Gould Judith. “Severe Impairments of Social Interaction and Associated Abnormalities in Children: Epidemiology and Classification,” J. Autism Dev. Disorders 9 no. 1 (1979): 11–29.
Cameron “Psychosis in Infancy and Early Childhood” (n. 53 280
Insulin treatment chart 8/3/1950–1/11/1951, MHCP/A: 887704.
Cameron “Psychosis in Infancy and Early Childhood” (n. 53 283
E.g., OT report—12/20/54, MHCP/A: 338427.
Letter—König to Cameron, 6/19/52, MHCP/A: 948758.
Letter 10/29/58, MHCP/A: 573500.
Letter—Anthony to Bradshaw, 9/22/54, MHCP/A: 874753.
Thomson Problem (n. 14 285
O’Connor Neil. “Neuroticism and Emotional Instability in High-Grade Male Defectives,” J. Neurol. Neurosurg. Psychiatry 14 no. 3 (1951): 226–30. O’Connor Neil, Tizard Jack. The Social Problem of Mental Deficiency (London: Pergamon; 1956).
Hilliard Leslie, Kirman Brian. Mental Deficiency (London: Churchill; 1957: ), 8
Ibid., 24.
Jones Kathleen. A History of the Mental Health Services (London: Routledge; 1972. 306
Percy Report, 1957, paras. 17–19, in Brian Watkin, Documents on Health and Social Services 1834 to the Present Day (London: Methuen; 1975. 387
Ibid., 387.
Ibid., 392–93.
Mental Health Act 1959, pt. 1, sec. 4, pp. 2–3.
Percy Report, 1957, paras. 17–19, in Watkin, Documents (n. 87), 389.
E.g., HC Deb, May 6, 1959, Hansard, vol. 605, cc403–83.
Mental Health Act of 1959, pt. 1, sec. 4, p. 3.
Ibid., pt. 1, sec. 3, p. 3.
Ibid., pt. 2, sec. 10, p. 6.
William Compton Carr, Houses of Parliament, May 1960, Hansard, May 18, 1960.
Special Educational Treatment Psychotic Autistic Children 1961–1965 and Letter from P. Benner (MoH) to H. E. Clinkard (MoE), August 27, 1961, National Archives, London, ED50/994.
Draft report of the SMHAC sent from Benner to Clinkard, September 6, 1962, National Archives, London, ED50/994.
Creak Mildred. “Schizophrenic Syndrome in Childhood,” Brit. Med. J. 2 (1961): 889–90. quotations on 889.
Allison Helen. “Perspectives on a Puzzle Piece,” Communication 22 no. 1 (1988): 6–9.
Tizard Jack. “Community Services for the Mentally Subnormal,” Proc. Roy. Soc. Med. 58 no. 5 (1965): 373–74.
Rutter Michael. “The Emergence of Developmental Psychopathology,” in Psychology in Britain, ed. Bunn G. C., Lovie A. D., Richards G. D. (Leicester: BPS Books; 2001. 422–32.
IOP, Report 1964–1965.
Wings’ Memorandum, 8, National Archives, London, ED50/994.
Ibid.
Ibid.
Creak “Schizophrenic Syndrome in Childhood” (n. 100 889–90.
Wings’ Memorandum (n. 104).
Lotter Victor. “Epidemiology of Autistic Conditions in Young Children,” Soc. Psychiatry 1 no. 3 (1966): 124–37.
Newsletter, SAC, March 1965, National Archives, London, ED50/969.
Letter—Compton Carr to Priestley, April 13, 1964, National Archives, London, ED50/969.
Mentally handicapped children, HC, February 18, 1966, Hansard.
Branch meeting with HM inspectors, March 30, 1966, National Archives, London, ED50/994.
Ibid.
Tizard Jack. “Results and Summary of the Brooklands Experiment,” in Child Development and Social Policy, ed. Clarke A. D. B., Tizard Barbara. (Leicester: British Psychological Society; 1983. 37–44.
Draft BPS report, 1966, National Archives, London, ED50/994.
Hermelin Beate, O’Connor Neil. “The Response and Self-Generated Behaviour of Severely Disturbed Children and Severely Subnormal Controls,” Brit. J. Soc. Clin. Psychology 2 (1963): 37–43.
Great Britain, Government Document: Committee on Local Authority and Allied Personal Services, Report of the Committee on Local Authority and Allied Personal Social Services 1968: 25; Jones, A History (n. 87), 332.
Branch meeting with HM inspectors (n. 114), 7–8.
Minute Sheet concerning SAC 1968, National Archives, London, ED50/969.
HC Deb, February 10, 1971, Hansard, vol. 811, c203W; CSDPA1970(1971).
Ford Julienne, Mongon Denis, Whelan Maurice. Special Education and Social Control (London: Routledge & Kegan Paul; 1982. 24
Letter—Director of Education, Solihull, to Dr. Skuse November 1978, MHCP/A: 514794.
MHCP/A: 514794.
Letter from Patricia Howlin April 1982, MHCP/A: 741149.
MHCP/A: 901137.
MHCP/A: 723269.
MHCP/A: 281589.
MHCP/A: 761794.
MHCP/A: 307194.
DES figures quoted in Ford, Mongon, and Whelan, Special Education and Social Control (n. 123), 24.
Ibid., 24.
Great Britain, Government Document: Department of Education and Science. Special Educational Needs. Report of the Committee of Enquiry into the Education of Handicapped Children and Young People 1978 (WARNOCK), 1–3.
Michael Rutter Interview with Bonnie Evans, December 7, 2006, Department of History and Philosophy of Science, Cambridge University.
Rutter Michael, Cox Anthony, Tupling Celia, Berger Michael, Yule William. “Attainment and Adjustment in Two Geographical Areas: The Prevalence of Psychiatric Disorder,” Brit. J. Psychiatry 126 (1975): 493–509.
WARNOCK 1978 (n. 134), para. 3.21.
Wing, Gould “Severe Impairments” (n. 75
King’s College London Archives, Fiona Subotsky Papers: Brixton Child Guidance Clinic Annual Report 1983.
Baird et al., “Prevalence of Disorders” (n. 6).


