Abstract
Objectives
To determine the effects of Tai Chi training on functional performance and walking with and without performance of a cognitive task, in adults of advanced age living within supportive housing facilities.
Design
Secondary data analysis of a single-blind, randomized controlled trial of Tai Chi training versus an attention-matched educational control intervention with cross-over to Tai Chi.
Setting
Two supportive housing facilities.
Participants
Sixty-six men and women living in supportive housing facilities entered the study. Fifty-seven participants aged 87±7 years completed all study procedures.
Intervention
Interventions consisted of two, one-hour, instructor-led group sessions/week for 12 weeks. Tai Chi training consisted of movements based upon the Yang-style short form. Educational sessions consisted of lectures and discussions of age-related health topics.
Measurements
Subjects were tested for physical function (Short Physical Performance Battery, SPPB), balance (Berg Balance Scale, BBS), mobility (timed up-and-go, TUG), and walking speed under normal and cognitive dual task conditions.
Results
The Tai Chi group exhibited greater (p=0.005) improvement in SPPB scores (baseline=8.1±2.9, follow-up=9.0±2.6) compared to controls (baseline=8.2±2.6, follow-up=8.2±2.6). Tai Chi also increased normal and dual task walking speeds (p<0.001), yet did not affect BBS (p=0.02) or TUG (p=0.02) after accounting for multiple comparisons. The dual task cost (i.e., percent change) to walking speed was unaffected. Following the cross-over Tai Chi intervention, the control group improved performance in the SPPB, BBS, and TUG, and increased walking speed under normal and dual task conditions (p<0.008).
Conclusion
Tai Chi training may be a safe and effective therapy to help improve physical function and dual task walking in very old adults living within supportive housing facilities.
Keywords: Tai Chi, Frailty, Mobility, Gait, Randomized Controlled Trial
Introduction
Aging is often associated with multiple functional impairments that are characteristic of frailty and may diminish the ability to adapt to common stressors in daily life.1-2 Tai Chi is a Chinese martial arts form that engages multiple physiologic systems3,4 and thereby has the potential to overcome the impairments associated with frailty.5 Tai Chi's emphasis on the integration of mind and body may also make it particularly well-suited to improve one's ability to adapt walking to concurrent performance of cognitive “dual” tasks. Still, its effectiveness as a low-cost intervention to improve physical function and dual task capacity in very old adults living within supportive housing facilities is largely unknown. We therefore conducted a study comparing 12-weeks of Tai Chi training to an education attention-control intervention with cross-over to Tai Chi, for their effects on physical function and dual task walking in adults over the age of 70 and living within supportive housing facilities. We hypothesized that as compared to the control intervention, Tai Chi training would result in greater improvement in physical function, as well as the ability to maintain walking speed during a cognitive stressor.
Methods
Trial Design
A single-blinded RCT was conducted to determine the effects of Tai Chi exercise, as compared to an educational control intervention, on cardiovascular and balance system function in older people at risk of developing frailty (NCT01126723). Here, we report secondary study outcomes related to balance and physical function. Primary outcomes of frailty status and nonlinear dynamics will be reported elsewhere.
Eligible participants were assessed at baseline and randomly assigned to a Tai Chi or educational control group. Assessments were conducted by study personnel blinded to group assignment. Upon completion of follow-up testing, control group participants completed the Tai Chi intervention and a final “cross-over” assessment.
Participants
Men and women were recruited between 2010-2013 from two supportive housing facilities owned by Hebrew SeniorLife. Each site houses elderly residents >70 years old and in need of supportive services for instrumental activities of daily living. The study was advertised within each facility via flyers and a presentation by study personnel. Interested individuals were screened via phone interview. Potentially eligible individuals then completed an in-person evaluation. Written informed consent was obtained from all participants. The study was approved by the Hebrew SeniorLife Institutional Review Board.
Exclusion criteria included the inability to stand or ambulate unassisted, the presence of symptomatic cardiovascular or respiratory disease, history of myocardial infarction or stroke, self-reported painful arthritis, spinal stenosis, amputation, painful foot lesions, or neuropathy, systolic BP >160 or diastolic BP >100mmHg, known abnormal cardiac rhythm or presence of cardiac pacemaker, Parkinson's disease, metastatic cancer or immunosuppressive therapy.
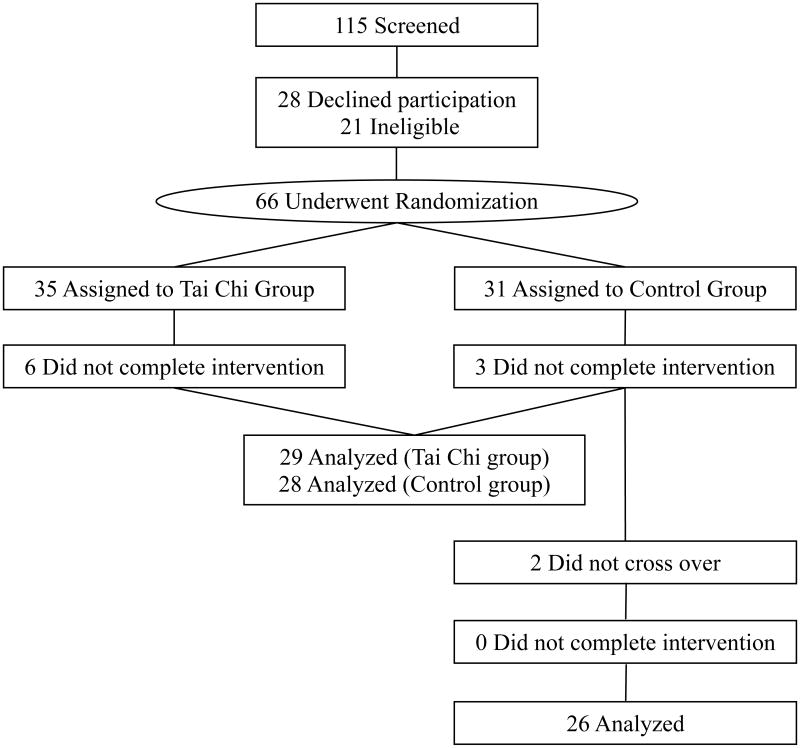
Thirty-five participants were assigned to the Tai Chi group and 31 to the control group. All participants completed the baseline assessment. Six withdrew from the Tai Chi group and three withdrew from the control group prior to follow-up. Reasons for withdrawal included injury unrelated to the study (n=1) and diminished interest in participation (n=8). Upon completion of follow-up, 26 of 28 remaining control group participants completed the cross-over Tai Chi intervention and assessment.
Interventions
Tai Chi Intervention
This12-week intervention was conducted within a common area of each facility. Two, one-hour group training sessions were taught per week by one of three instructors to a maximum of 12 participants per group. The certified instructors had >5 years of Tai Chi teaching experience with older health-impaired adults. Training was based upon a program initially developed for patients with heart disease and balance disorders.6-9 It focused upon traditional Tai Chi warm-up exercises and five core movements from the Cheng Man-Ch'ing's Yang-style short form: ‘raising the power,’ ‘withdraw and push,’ ‘grasp the sparrow's tail,’ ‘brush knee twist step,’ ‘wave hand like clouds.’ In addition, participants were provided with an instructional DVD of the entire protocol and instructed to practice at home for 20min at least 3 days per week. Home practice was tracked using participant diaries. Participants were instructed to report any adverse event to the Tai Chi instructor.
Educational Control Intervention
A time-matched attention control intervention was used in which participants attended one-hour group sessions twice weekly. Sessions were led by research personnel and included lectures, discussions, and Patient Education Handouts produced by the American Geriatric Society Public Education Committee (available at http://www.americangeriatrics.org).
Assessments
Participants were assessed for physical function, balance, mobility and walking with and without performance of a cognitive task.
The Short Physical Performance Battery (SPPB) is a valid and reliable test of physical function that includes measures of standing balance, 4-meter walking speed and the ability to rise from a chair 5 times.10,11 The Berg balance scale (BBS) assesses static and dynamic balance. Participant performance is graded on a 5-point ordinal scale in 14 separate tasks.12 A BBS score <45 has been linked with elevated fall risk.13 The Timed Up-and-Go (TUG) is a validated test of mobility14 in which the participant must rise from a chair, walk 3m and return to a seated position. Walking was assessed at preferred speed along a 30m course in a hallway of each facility. Two, 90sec trials were completed in random order: walking normally and walking while verbalizing serial-subtractions of 5 from a random 3-digit number. Walking speed was determined by dividing total distance by trial duration.
Frailty status was calculated based upon previously-reported cut-offs for unintentional weight loss, exhaustion, physical activity level, walking speed, and grip strength.15-17 Participants with ≥3 deficits were classified as frail, 1-2 deficits as pre-frail, and no deficits as non-frail.
Study Outcomes
Outcomes included SPPB and BBS scores, TUG time, and average walking speed during normal and dual task conditions. The “dual task cost” to walking speed was also calculated as the percent change in speed between normal and dual task conditions.
Statistical Analysis
Analyses were performed using JMP software (SAS Institute, Cary, NC). Descriptive statistics summarized group characteristics and study outcomes. An initial analysis examined the characteristics of the nine individuals who withdrew participation during the study. Their age, sex, height, body mass and baseline performance in each study outcome was similar to those who completed the study. We therefore based subsequent analyses on those who completed all study procedures.
Potential between-group differences in demographics and baseline characteristics were tested with one-way ANOVAs or chi-square tests.
The effects of intervention on study outcomes were first analyzed with data from the parallel-group RCT using two-way, repeated-measures ANCOVAs. Model effects were group, time and their interaction. Models were completed with and without adjustments for age, sex, BMI and attendance. Significance level was set at α=0.01 (Bonferroni adjusted) for each of the five outcomes. Tukey's post-hoc testing was used to compare factor means of significant models.
The effects of each intervention were also analyzed by examining the control-cross-over data. One-way, repeated-measures ANCOVAs were used to determine if performance in each outcome differed over time (i.e., baseline, follow-up, cross-over). Models were completed with and without adjustments for age, sex, BMI and attendance. Tukey's post-hoc testing compared factor means of significant models. Significance level was set to that described above.
As a secondary analysis, the influence of age on Tai Chi effectiveness was examined using linear regression. Data from both groups were included. Dependent variables were the percent change in each outcome following the original or cross-over Tai Chi intervention, as compared to the prior assessment. Model effects included age, group and their interaction. Each model was adjusted for Tai Chi attendance.
Results
Baseline Participant Characteristics (Table 1)
Table 1. Group characteristics and functional outcomes of the randomized controlled trial (means ± SD).
| Tai Chi Group | Control Group | ANCOVA* (p value) | |||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Baseline | Follow Up | Baseline | Follow Up | Group Effect | Time Effect | Interaction | |
| Sample (n) | 29 | - | 28 | - | |||
| Sex (M/F) | 5/24 | - | 7/21 | - | |||
| Age (years) | 87±5 | - | 86±6 | - | 0.21 | ||
| Age (range) | 75-95 | 71-98 | |||||
| Height (m) | 1.5±0.1 | - | 1.6±0.1 | - | 0.76 | ||
| Weight (kg) | 66±11 | 67±11 | 68±14 | 69±15 | 0.31 | 0.91 | 0.26 |
| Frailty Indexα | 9/16/4 | 7/16/6 | 6/20/2 | 5/21/2 | - | - | - |
| - Frail/Pre-frail/Non-frail (n) | |||||||
| SPPB (total score) | 8.1±2.9 | 9.0±2.6 | 8.2±2.6 | 8.2±2.6 | 0.60 | 0.32 | 0.005 |
| - 4m Gait Speed (m/s) | 1.02±0.26 | 1.11±0.28 | 0.94±0.30 | 0.93±0.28 | 0.08 | 0.67 | 0.009 |
| - Chair Stand Time (sec) | 14.5±4.7 | 12.6±2.9 | 14.2±3.6 | 14.3±2.9 | 0.46 | 0.30 | 0.01 |
| - Stand, Side-by-Side (sec) | 60.0±0.0 | 60.0±0.0 | 59.9±5.8 | 59.6±2.1 | 0.55 | 0.40 | 0.55 |
| - Stand, Semi-Tandem (sec) | 15.3±12.1 | 16.4±12.6 | 14.5±10.2 | 14.1±11.6 | 0.60 | 0.30 | 0.11 |
| - Stand, Tandem (sec) | 9.2±1.3 | 10.0±1.5 | 9.1±2.5 | 9.0±2.4 | 0.60 | 0.31 | 0.01 |
| Walking Speed, Normal (m/s) | 0.98±0.23 | 1.05±0.28 | 0.91±0.23 | 0.88±0.21 | 0.02 | 0.12 | <0.001 |
| Walking Speed, DT (m/s) | 0.87±0.22 | 0.94±0.24 | 0.80±0.25 | 0.76±0.21 | 0.02 | 0.08 | <0.001 |
| Dual task cost (% change) | -11.8±8.6 | -12.8±8.3 | -14.1±9.2 | -13.9±8.6 | 0.19 | 0.54 | 0.27 |
| BBS score | 45.6±6.8 | 47.3±6.4 | 44.4±6.5 | 44.0±6.7 | 0.23 | 0.08 | 0.02 |
| TUG (sec) | 12.0±4.2 | 11.2±3.8 | 13.9±5.6 | 14.4±6.5 | 0.09 | 0.60 | 0.02 |
Abbreviations: SPPB-Short Physical Performance Battery; BBS-Berg Balance Scale; TUG-Timed Up-and-Go, DT-Dual Task;
Adapted from Fried et al (REF);
Models were adjusted for age, sex, BMI and class attendance.
Fifteen participants were classified as frail, 36 as pre-frail and six as non-frail. Groups had similar gender distribution, age, height and body mass. The control group exhibited slower normal and dual task walking speeds (p=0.02). Baseline performance on other functional tests did not differ between groups.
Attendance and Adverse Events
Intervention attendance was similar between groups. Participants randomized to Tai Chi completed 20.9±2.6 of 24 classes and 20.1±6.4 hours of home practice. Participants randomized to the control intervention completed 21.0±2.6 of 24 educational classes. Following cross-over, this group completed 20.4±3.9 Tai Chi classes and 22.6±8.9 hours of home practice. No adverse events related to Tai Chi practice were reported.
Effects of Tai Chi on Walking and Physical Function
Parallel-Group Randomized Controlled Trial
Tai Chi had beneficial effects on physical function. A group by time interaction was observed for SPPB (F1,54=13.2, p=0.005), which remained significant after adjusting for covariates. Post-hoc testing revealed that control group performance did not change following the education intervention. The Tai Chi group, however, improved SPPB performance. Further analysis revealed that specific improvements were made within the 4m gait speed, chair stand time and tandem stance components of the test (see Table 1). Similar trends were observed for the TUG (F1,54=5.4, p=0.02) and BBS (F1,54=5.7, p=0.02), yet neither model reached significance after accounting for multiple comparisons.
Tai Chi training increased walking speeds. Group by time interactions were observed under normal (F1,54=12.0, p<0.001) and dual task conditions (F1,54=12.2, p<0.001). Each interaction remained significant after adjusting for covariates. At baseline, the control group walked slower in both conditions as compared to the Tai Chi group. Whereas the control group did not demonstrate a change in walking speed at follow-up, the Tai Chi group walked significantly faster—during both normal and cognitive dual task conditions.
At baseline, performing the cognitive task while walking resulted in a 14±8% (i.e., 0.13±0.81m/s) reduction in walking speed across all participants. This dual task “cost” was similar across groups. As Tai Chi training increased walking speeds under both normal and dual task conditions, it did not affect the dual task cost to this variable.
The effects of intervention on walking speed may have been confounded by baseline group differences (p<0.02) in these outcomes. Closer inspection of the data revealed that two control group participants walked significantly slower than average; i.e., 0.42 and 0.39m/s during normal conditions and 0.30 and 0.34m/s during dual task conditions. As each participant performed similarly at follow-up, and also exhibited lower than average performance in the other study outcomes, we did not deem these participants to be outliers. However, we repeated each ANCOVA with these two participants removed. In each case, baseline group differences were no longer present, yet similar interactions were observed; i.e., walking speed increased after Tai Chi training only.
Cross-Over Group
Upon completion of initial follow-up testing, 26 of 28 participants from the control group completed 12 weeks of Tai Chi training followed by a “cross-over” assessment. Significant effects of time were observed for the SPPB (F2,26=12.9, p<0.001), BBS (F2,26=6.6, p=0.004) and TUG (F2,26=5.6, p=0.008). In each case, post-hoc testing indicated that performance was improved following Tai Chi training as compared to the control period. As compared to their second assessment (following the control period), this group demonstrated a 21±16% increase in the SPPB score, an8±10% increase in the BBS score, and a 18±21% reduction in TUG time.
Significant effects of time were also observed for both normal (F2,26=8.0, p=0.001) and dual task (F2,26=8.1, p=0.001) walking speed. In each condition, walking speeds were greater following Tai Chi training as compared to either of the first two control assessments. Tai Chi training did not, however, reduce the dual task cost to walking speed.
It is of note that each of the two participants within this group that had relatively slow walking speeds at baseline (see previous subsection) demonstrated substantial improvements following the cross-over Tai Chi intervention. For the normal and cognitive task conditions, respectively, one participant walked 41 and 34% faster, and the other walked 20 and 26% faster after Tai Chi training.
Influence of Age on Tai Chi Effectiveness
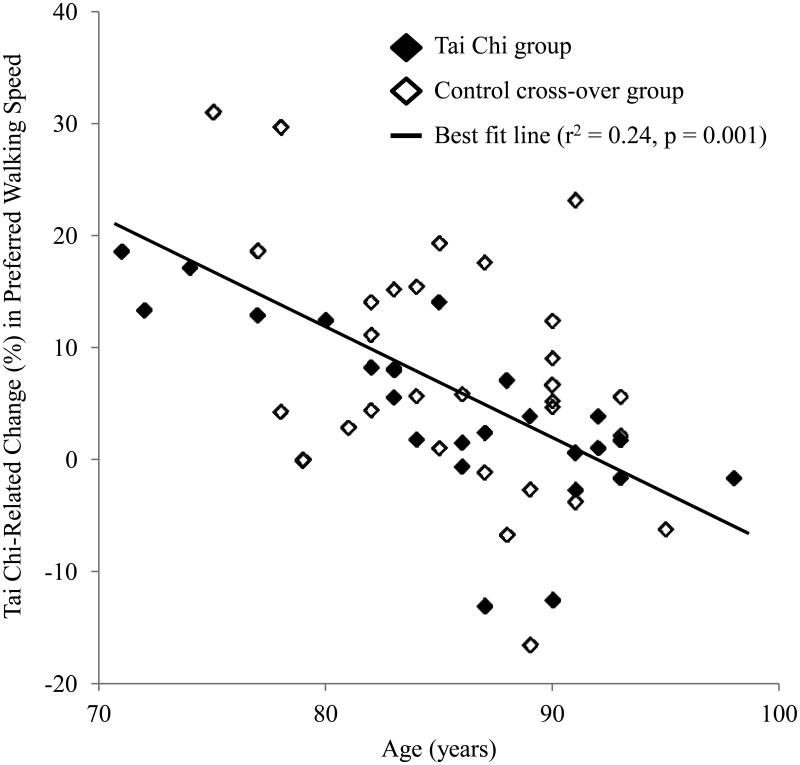
Cohort age ranged from 71-98 years. Secondary analyses revealed that younger participants made more improvement in the SPPB (R=0.36, p=0.02), TUG (R=-0.41, p=0.01) and normal walking speed (R=-0.48, p=0.001) (Figure 2). Regression analyses revealed that these relationships were similar between the original Tai Chi and cross-over groups, and independent of attendance. Age was not correlated with Tai Chi-related changes in BBS or dual task walking speed.
Figure 2. The relationship between participant age and Tai Chi-related improvement in walking speed.
Younger participants tended to exhibit larger percent changes in normal walking speed following their 12-week Tai Chi training intervention. A similar age effect was observed for performance in both the Timed Up-and-Go and Short Physical Performance Battery (not pictured). In each case, the relationship was similar between groups and independent of number of classes attended.
Discussion
As compared to an attention-matched educational intervention, 12 weeks of Tai Chi training improved physical function, balance and walking in very old adults living within supportive housing communities. Training sessions were well-attended and did not lead to adverse events. Tai Chi training may therefore be a safe, inexpensive and feasible therapeutic option to help maintain functional independence within vulnerable individuals of advanced age.
Tai Chi training improved performance in the SPPB, a test of physical function. Guralnik and colleagues10,11 reported that a summary score <9 predicted subsequent disability in adults aged >70 years. Here, average baseline SPPB scores were less than 9. Following both the original and cross-over Tai Chi training, average SPPB scores increased to above this 9-point threshold. Within the entire cohort, 17 participants with SPPB scores <9 at baseline exhibited scores ≥9 following Tai Chi training. These clinically-significant changes in physical function are supported by previous studies5,18-21 and warrant larger studies to determine the effectiveness of Tai Chi compared to other forms of exercise, and whether it reduces health care utilization within this costly population.
A common consequence of aging and frailty is a reduced capacity to adapt to the stressors of everyday life.1 Age-related decrements in walking, for example, are exacerbated when individuals are stressed by performing concurrent cognitive tasks.22 Slower walking speed when performing cognitive tasks is predictive of mobility decline and falls within older adults.23,24 In the present study, although Tai Chi training did not affect the dual task cost to walking speed, it did result in faster speeds within the dual task condition. Thus, while previous research has reported inconsistent results,25-26 our study suggests that 12-weeks of training may be sufficient to improve the capacity to adapt walking to a cognitive stressor within this population.
The present cohort was unique in that the average age was 87 years. Results indicated that for the TUG, SPPB and preferred walking speed, older participants made less improvement following Tai Chi (Figure 2). Few studies have examined the impact of age on exercise effectiveness. Kalapotharakos et al27 reported that 8 weeks of resistance training improved physical function in adults aged 80-88 years. Serra-Rexach et al,28 however, reported that a similar intervention improved strength, yet did not alter TUG performance in nonagenarians. The “oldest old” may thus be less responsive—in terms of mobility outcomes—to Tai Chi and other forms of exercise training. Still, the results of this relatively small, yet well-controlled trial indicate that Tai Chi may effectively improve functional performance in very old adults living within supportive housing facilities.
Figure 1. Participant Flow Diagram.
Acknowledgments
This work was supported by a Harvard Catalyst KL2 (1KL2RR025757-04) and grants from the NIA (R37-AG025037; T32AG023480; P01-AG004390). Dr. Lipsitz holds the Irving and Edyth S. Usen and Family Chair in Geriatric Medicine at Hebrew SeniorLife. The content is solely the responsibility of the authors and does not necessarily represent the official views of Harvard Catalyst, Harvard University and its affiliated academic health care centers.
Funding sources and related paper presentations: This work was supported by a KL2 Medical Research Investigator Training award (1KL2RR025757-04) from Harvard Catalyst, The Harvard Clinical and Translational Science Center (UL1RR025757) and grants from the National Institutes on Aging (R37-AG025037; T32AG023480; P01-AG004390).
Sponsor's Role: none
Footnotes
Author Contributions: LAL and PMW had the original idea for the study. All authors contributed to the design of the study and interpretation of the data. BM wrote the initial draft of the manuscript and all authors provided intellectual input to subsequent drafts. LAL is the study guarantor. BM and AC performed the statistical analyses of the data. All authors approved the final version of this manuscript.
An abstract from this study was presented at the 2012 Annual Meeting of The American Geriatrics Society.
| Elements of Financial/Personal Conflicts | *BM | ML | MMG | AC | PMW | LAL | |||||||||
| Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | ||||
| Employment or Affiliation | X | X | X | X | X | X | |||||||||
| Grants/Funds | X | X | X | X | X | X | |||||||||
| Honoraria | X | X | X | X | X | X | |||||||||
| Speaker Forum | X | X | X | X | X | X | |||||||||
| Consultant | X | X | X | X | X | X | |||||||||
| Stocks | X | X | X | X | X | X | |||||||||
| Royalties | X | X | X | X | X | X | |||||||||
| Expert Testimony | X | X | X | X | X | X | |||||||||
| Board Member | X | X | X | X | X | X | |||||||||
| Patents | X | X | X | X | X | X | |||||||||
| Personal Relationship | X | X | X | X | X | X | |||||||||
References
- 1.Lipsitz LA. Physiological complexity, aging, and the path to frailty. Sci Aging Knowledge Environ. 2004;2004:e16. doi: 10.1126/sageke.2004.16.pe16. [DOI] [PubMed] [Google Scholar]
- 2.Manor B, Costa MD, Hu K, et al. Physiological complexity and system adaptability: evidence from postural control dynamics of older adults. J Appl Physiol. 2010;109:1786–1791. doi: 10.1152/japplphysiol.00390.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wayne PM, Kaptchuk TJ. Challenges inherent to t'ai chi research: part II-defining the intervention and optimal study design. J Altern Complement Med. 2008;14:191–197. doi: 10.1089/acm.2007.7170b. [DOI] [PubMed] [Google Scholar]
- 4.Wayne PM, Kaptchuk TJ. Challenges inherent to t'ai chi research: part I—t'ai chi as a complex multicomponent intervention. J Altern Complement Med. 2008;14:95–102. doi: 10.1089/acm.2007.7170a. [DOI] [PubMed] [Google Scholar]
- 5.Wolf SL, Barnhart HX, Kutner NG, McNeely E, Coogler C, Xu T. Reducing frailty and falls in older persons: an investigation of Tai Chi and computerized balance training. Atlanta FICSIT Group. Frailty and Injuries: Cooperative Studies of Intervention Techniques. J Am Geriatr Soc. 1996;44:489–497. doi: 10.1111/j.1532-5415.1996.tb01432.x. [DOI] [PubMed] [Google Scholar]
- 6.McGibbon CA, Krebs DE, Wolf SL, Wayne PM, Scarborough DM, Parker SW. Tai Chi and vestibular rehabilitation effects on gaze and whole-body stability. J Vestib Res. 2004;14:467–478. [PubMed] [Google Scholar]
- 7.Yeh GY, Wood MJ, Lorell BH, et al. Effects of tai chi mind-body movement therapy on functional status and exercise capacity in patients with chronic heart failure: a randomized controlled trial. Am J Med. 2004;117:541–548. doi: 10.1016/j.amjmed.2004.04.016. [DOI] [PubMed] [Google Scholar]
- 8.Yeh GY, McCarthy EP, Wayne PM, et al. Tai chi exercise in patients with chronic heart failure: a randomized clinical trial. Arch Intern Med. 2011;171:750–757. doi: 10.1001/archinternmed.2011.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yeh GY, Wood MJ, Wayne PM, et al. Tai chi in patients with heart failure with preserved ejection fraction. Congest Heart Fail. 2013;19:77–84. doi: 10.1111/chf.12005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–M94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 11.Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med. 1995;332:556–561. doi: 10.1056/NEJM199503023320902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Berg KO, Wood-Dauphinee SL, Williams JI, Maki B. Measuring balance in the elderly: validation of an instrument. Can J Public Health. 1992;83:S7–11. [PubMed] [Google Scholar]
- 13.Muir SW, Berg K, Chesworth B, Speechley M. Use of the Berg Balance Scale for predicting multiple falls in community-dwelling elderly people: a prospective study. Phys Ther. 2008;88:449–459. doi: 10.2522/ptj.20070251. [DOI] [PubMed] [Google Scholar]
- 14.Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39:142–148. doi: 10.1111/j.1532-5415.1991.tb01616.x. [DOI] [PubMed] [Google Scholar]
- 15.Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: Evidence for a Phenotype. J Gerontol A Biol Sci Med Sci. 2001;56A:M146–M156. doi: 10.1093/gerona/56.3.m146. [DOI] [PubMed] [Google Scholar]
- 16.Theou O, Brothers TD, Mitnitski A, Rockwood K. Operationalization of frailty using eight commonly used scales and comparison of their ability to predict all-cause mortality. J Am Geriatr Soc. 2013;61:1537–1551. doi: 10.1111/jgs.12420. [DOI] [PubMed] [Google Scholar]
- 17.Rothman MD, Leo-Summers L, Gill TM. Prognostic significance of potential frailty criteria. J Am Geriatr Soc. 2008;56:2211–2216. doi: 10.1111/j.1532-5415.2008.02008.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wolf SL, O'Grady M, Easley KA, Guo Y, Kressig RW, Kutner M. The influence of intense Tai Chi training on physical performance and hemodynamic outcomes in transitionally frail, older adults. J Gerontol A Biol Sci Med Sci. 2006;61:184–189. doi: 10.1093/gerona/61.2.184. [DOI] [PubMed] [Google Scholar]
- 19.Li L, Manor B. Long term Tai Chi exercise improves physical performance among people with peripheral neuropathy. Am J Chinese Med. 2010;38:1–11. doi: 10.1142/S0192415X1000797X. [DOI] [PubMed] [Google Scholar]
- 20.Taggart HM. Effects of Tai Chi exercise on balance, functional mobility, and fear of falling among older women. Appl Nurs Res. 2002;15:235–242. doi: 10.1053/apnr.2002.35975. [DOI] [PubMed] [Google Scholar]
- 21.Tsang WW, Wong VS, Fu SN, Hui-Chan CW. Tai Chi improves standing balance control under reduced or conflicting sensory conditions. Arch Phys Med Rehabil. 2004;85:129–137. doi: 10.1016/j.apmr.2003.02.002. [DOI] [PubMed] [Google Scholar]
- 22.Hausdorff JM, Schweiger A, Herman T, Yogev-Seligmann G, Giladi N. Dual-task decrements in gait: Contributing factors among healthy older adults. J Gerontol A Biol Sci Med Sci. 2008;63:1335–1343. doi: 10.1093/gerona/63.12.1335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Herman T, Mirelman A, Giladi N, Schweiger A, Hausdorff JM. Executive control deficits as a prodrome to falls in healthy older adults: A prospective study linking thinking, walking, and falling. J Gerontol A Biol Sci Med Sci. 2010;65:1086–1092. doi: 10.1093/gerona/glq077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Springer S, Giladi N, Peretz C, Yogev G, Simon ES, Hausdorff JM. Dual tasking effects on gait variability: The role of aging, falls and executive function. Mov Disord. 2006;21:950–957. doi: 10.1002/mds.20848. [DOI] [PubMed] [Google Scholar]
- 25.Lu X, Siu KC, Fu SN, Hui-Chan CW, Tsang WW. Tai Chi practitioners have better postural control and selective attention in stepping down with and without a concurrent auditory response task. Eur J Appl Physiol. 2013;113:1939–1945. doi: 10.1007/s00421-013-2624-9. [DOI] [PubMed] [Google Scholar]
- 26.Hall CD, Miszko T, Wolf SL. Effects of Tai Chi intervention on dual-task ability in older adults: a pilot study. Arch Phys Med Rehabil. 2009;90:525–529. doi: 10.1016/j.apmr.2008.09.566. [DOI] [PubMed] [Google Scholar]
- 27.Kalapotharakos VI, Diamantopoulos K, Tokmakidis SP. Effects of resistance training and detraining on muscle strength and functional performance of older adults aged 80 to 88 years. Aging Clin Exp Res. 2010;22:134–140. doi: 10.1007/BF03324786. [DOI] [PubMed] [Google Scholar]
- 28.Serra-Rexach JA, Bustamante-Ara N, Hierro VM, et al. Short-term, light- to moderate-intensity exercise training improves leg muscle strength in the oldest old: a randomized controlled trial. J Am Geriatr Soc. 2011;59:594–6. doi: 10.1111/j.1532-5415.2011.03356.x. [DOI] [PubMed] [Google Scholar]