Abstract
Background
The purpose of this study was to test whether lower socioeconomic status (SES) augments the effect of psychological distress on mortality from stroke or coronary heart disease (CHD).
Methods
We prospectively linked data from 66,500 participants 35 years or older in the Health Survey for England, selected using stratified random sampling from 1994 to 2004, and free of cardiovascular disease and cancer at baseline, with mortality records. The median follow-up time was 7.9 years. SES was indexed by occupational class, and psychological distress was assessed using the 12-item General Health Questionnaire (GHQ-12).
Results
After adjustment for demographic and clinical variables, both psychological distress and low SES were associated with increased mortality: the hazard ratios (HR) for one-category increase in low SES (three categories in total) were 1.15 for stroke-death (95% confidence interval [CI] = 1.00–1.31, p = .043) and 1.24 for CHD-death (95% CI = 1.09–1.41, p = .001); the HR for one-category increase in GHQ-12 (three categories in total) was 1.18 for stroke-death (95% CI = 1.07–1.30, p = .001) and 1.24 for CHD-death (95% CI = 1.13–1.36, p < .001). In stratified analyses, the strongest associations were found in the lowest SES categories: the HR for GHQ-12 toward stroke-death was 1.15 in high-SES participants (95% CI = 0.97–1.37, p = .107) and 1.31 in low-SES ones (95% CI = 1.13–1.51, p < .001); the HR for GHQ-12 toward CHD-death was 1.10 in high-SES participants (95% CI = 0.97–1.25, p = .129) and 1.33 in low-SES ones (95% CI = 1.19–1.48, p < .001).
Conclusions
People in low socioeconomic circumstances are more vulnerable to the adverse effect of psychological distress. This pattern should be taken into account when evaluating the association between psychosocial variables and health outcomes.
Key words: stroke, coronary heart disease, mortality, psychological distress, socioeconomic status
INTRODUCTION
Psychological distress is a term that incorporates a number of psychological risk factors including depressive symptoms, anxiety, and social dysfunction. These psychological constructs are becoming increasingly recognized as risk factors for mortality and cardiovascular disease (CVD) events (1–3). Socioeconomic status (SES) is also a known determinant of health status, with lower SES being associated with risk of cardiovascular and other health outcomes (4–6).
We recently hypothesized that when both risk factors are present (high levels of psychological distress and low levels of SES), the resulting effect on health outcomes is not additive, but that there is a multiplicative effect (7). This hypothesis was stimulated by concepts such as the reserve capacity model of Gallo and Matthews (8), which postulates that lower-SES individuals have fewer interpersonal and intrapersonal resources to manage stressful events than do more affluent individuals. In a recently published analysis of this study cohort, we showed that high levels of psychological distress were more strongly associated with all-cause mortality among individuals with lower-than-higher SES (7). Recent data (9) from the same subsample of the Health Survey for England (HSE) have demonstrated that the association between psychological distress and all-cause mortality is being strongly driven by CVD, which forms a strong rationale to examine the differential effect of psychological stress on specific CVD outcomes across SES groups rather than performing independent replications on subgroups of death causes. In addition, plausible mechanisms linking psychological distress with CVD have been well documented: factors such as vascular endothelial function, proinflammatory cytokines, C-reactive protein, and hemostatic variables have been recognized as potential mechanisms linking psychological distress and CVD (1,2,10,11). The differential effect of psychological stress on specific CVD outcomes across SES groups has not been directly investigated before in a large prospective observational study. Some smaller studies have shown additive effects of occupational stress and lower-SES position on CVD outcomes, including stroke and coronary heart disease (CHD) (12–17).
In the present article, we examined the association of psychological distress and SES on the incidence of specific CVD mortality end points (stroke and CHD), with an emphasis on the interaction between the two risk factors. We hypothesized that SES can operate as an amplifier of psychological distress, such that the effect of psychological distress on mortality from CHD and stroke would be greater in groups with lower-than-higher SES.
METHODS
This study is based on additional analyses on data that have previously been published (7). Previous analyses considered all-cause mortality as the primary outcome, whereas the present analyses are focused on mortality from stroke and CHD.
Study Design
We used data from the HSE, a program aimed at measuring the health status of the English population every year. The HSE is based on annual surveys, starting from 1991, in which the participants are representative (stratified random sampling) of the individuals living in private households in England. In every year, the HSE program is designed to collect information about general health, body mass index (BMI), health behaviors (smoking, alcohol consumption, and physical activity), biomarkers, SES, psychosocial parameters such as psychological distress and social relationships, and physician-diagnosed CVD and diabetes, during household visits. The trained interviewers collect the data using Computer-Assisted Personal Interviewing. Resting blood pressure is measured in a separate household visit by trained nurses who also collect blood samples (18).
We used HSE surveys from 1994 to 2004 and included all participants 35 years or older to form a baseline sample for a longitudinal study. We used Office of National Statistics death certificates to measure our outcomes, which provide information on the date and cause of death. The primary cause of death was recorded using the International Classification of Diseases, Ninth (ICD-9) and Tenth (ICD-10) Revisions. CVD codes were 390–459 for ICD-9 and I01–I99 for ICD-10, which were further categorized into CHD (410–414 [ICD-9] and I20–I25 [ICD-10]) and cerebrovascular diseases (430–438 [ICD-9] and I60–I69 [ICD-10]). The censoring date (the latest time of participants’ status ascertainment) was predetermined to be the 28th February 2008. Participants who reported a previous stroke or transitory ischemic attack or CHD (including angina) at the time of the baseline nurse visit were excluded. Patients with cancer were also excluded.
SES classification was derived from information about participants’ profession using the Registrar General’s Social class system. The categorization is based on work features such as career prospects, autonomy, method of payment, and period of notice (19). The system is based on data from the head of the household, and if at the time of the interview, this person was unemployed, the classification would be based on his/her most recent employment. In the HSE, participants were divided into six categories: managerial and professional positions, intermediate, small employers and own account workers, lower supervisory and technical, and semiroutine and routine occupations. In the primary analyses of interactions between SES and psychological distress, we further collapsed the six categories into three (1 = professional or managerial position; 2 = skilled manual or nonmanual workers; 3 = semiroutine or unskilled workers) (20).
We measured psychological distress using the General Health Questionnaire (GHQ-12) (21). The GHQ-12 is a unidimensional scale (22) and is composed of 12 questions relating to anxiety, depression, social dysfunction, and loss of confidence. Possible answers go from zero to four (symptom present: “not at all” = 0, “same as usual” = 0, “more than usual” = 1, and “much more than usual” = 1), and therefore, the total score can go from 0 to 12. Analytically, the GHQ-12 can be used either as an ordered categorical variable (0 = low distress; 1–3 = medium distress; 4+ = high distress) (21). The Cronbach α (internal consistency measure) for the GHQ-12 in this sample was .91.
All clinical variables were either directly measured (height, weight, blood pressure [cutoff, 140/90 mm Hg]) or reported to be diagnosed and treated through the National Health Service (diabetes, hypertension), or self-reported (smoking and physical activity, defined as the number of 30-minute sessions of moderate intensity walking or 15-min sessions of vigorous sports and exercises per week excluding domestic activity) (23,24).
Hypertension and physical activity were only recorded in survey years 1994, 1997 (physical activity only), 1998, 1999, 2003, and 2004, so the data for these variables are less complete than for other measures.
Study participants gave full informed consent, and ethical approval was obtained from the London Research Ethics Committee.
Data Analysis
An initial data cleaning procedure comprised checking for missing, duplicate and illogic values, as well as digit preferences, normality, and outliers of continuous variables.
We used Cox regression, with a follow-up time scale expressed in months. The main exposure variables were SES (profession) and psychological distress (GHQ-12). The outcomes were stroke-mortality and CHD-mortality. We modeled the association of SES, GHQ-12, age, sex, current smoking, BMI, and diabetes with each outcome separately. Assumptions such as proportional hazards and departure from linearity were satisfied.
The interaction between SES and GHQ-12 was evaluated using the likelihood ratio test (LRT) in three separate models, one with no adjustments, one with adjustment for age and sex, and one with further adjustment for all covariates. Our analysis strategy had a number of steps: first, we ran a model with SES, GHQ-12, and the other covariates; second, the model was repeated after adding in the interaction between the SES and GHQ-12; third, the estimates from the second model were compared with the estimates from the initial model using the LRT. This test is valid if the comparison is made on the same group of individuals, that is, missing values can distort the results, and this requirement has been respected.
A sensitivity analysis was conducted including hypertension and physical activity in the multivariable analyses because these variables were not recorded for the full sample.
The complete analysis was then repeated separately for men and women, people 35 to 54 years old and those 55 years and older, and people visited in years 1994 to 1999 and 2000 to 2004.
RESULTS
Of the initial sample of 96,605 adults, 10.4% (n = 10,065) did not consent to mortality follow-up and were therefore removed from the analysis. Individuals who did not agree to follow-up were older on average than those who consented (64.3 versus 56.1 years, p < .001). A proportion of participants (5864, or 6.8%) had histories of stroke or CHD or had another prevalent CVD or cancer at baseline and were therefore excluded from the analyses. Of the remaining 80,676 participants, 15.4% had missing values for psychological distress and 2.6% for SES. Individuals with missing GHQ-12 values were slightly older than those who completed the GHQ-12 (56.4 versus 55.1 years, p < .001), but did not differ from the remainder in sex distribution. Six individuals were lost to follow-up and 27 were excluded from the analysis because they experienced a cardiovascular event within 1 month of recruitment. The final analytic sample therefore consisted of 66,518 men and women. Around 40% of participants had missing data for hypertension and physical activity. The sample is described in Table 1.
TABLE 1.
Sample Description for 66,518 Participants 35 Years or Older From the Health Survey for England, Free From Cancer and Cardiovascular Disease at Baseline (1994–2004)
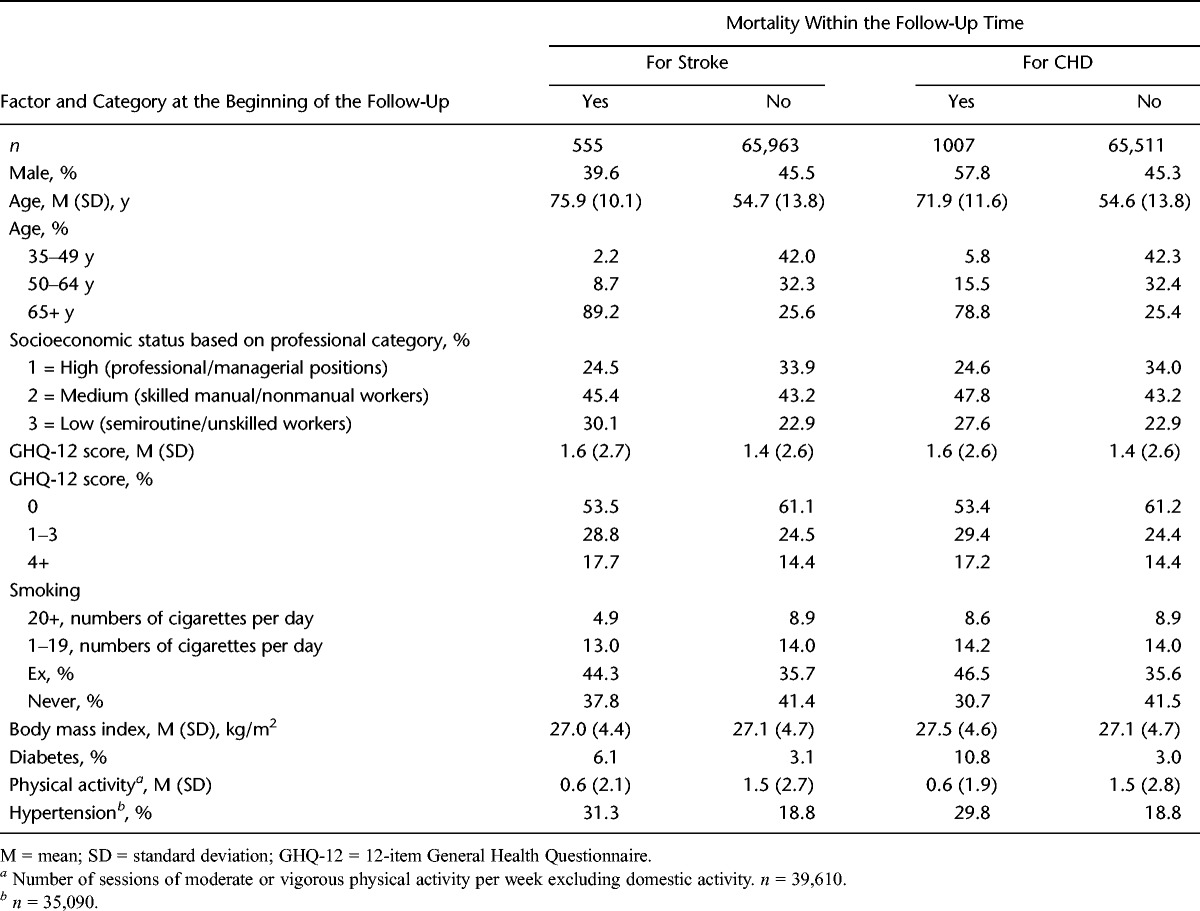
The cohort was followed up for a mean (standard deviation) of 8.2 (3.4) years (median = 7.9 years). Over this period, 7875 (11.8%) died of any cause, whereas 555 (0.8%) died of stroke and 1007 (1.5%) died of an CHD event. The crude mortality rates for stroke and CHD were 1.02 (95% confidence interval [CI] = 0.94–1.11) and 1.85 (95% CI = 1.74–1.97) per 1000 person-years.
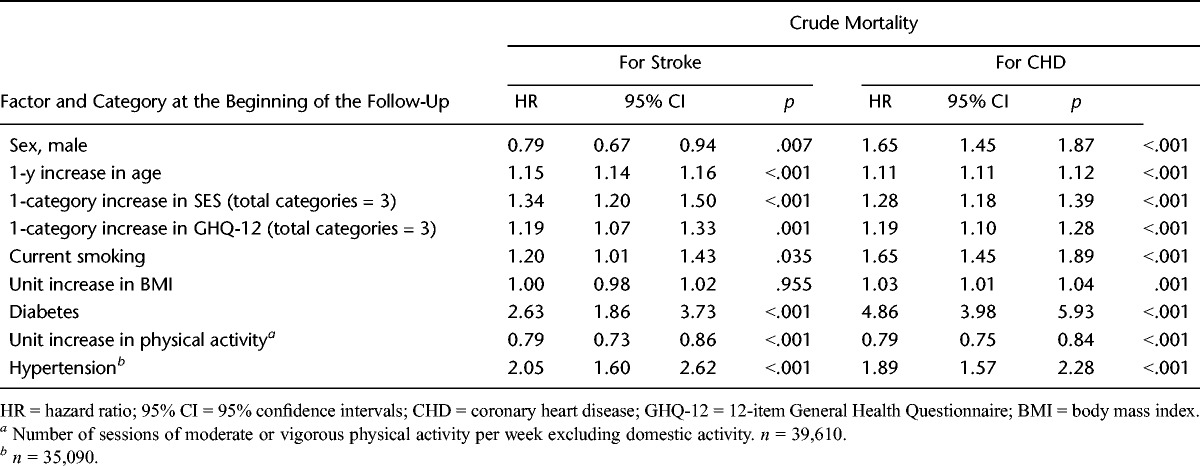
Across the complete study sample, 14.4% reported psychological distress based on the established cutoff point of GHQ-12 score of 4 or higher (21). Individuals in lower occupational classes were older, were more likely to be women, were more likely to be current smokers, and reported higher GHQ-12 score (the average GHQ-12 score was 1.40 for the whole sample [95% CI = 1.39–1.43], 1.30 for high-SES participants [95% CI = 1.27–1.33], 1.37 for the medium-SES ones [95% CI = 1.34–1.40], and 1.63 for the low-SES ones [95% CI = 1.59–1.68]). Psychological distress was associated with increased cardiovascular mortality rates, as was low SES. Mortality was also associated with diabetes, hypertension, and smoking, whereas physical activity was associated with lower risk. BMI was related to increased mortality for CHD but not for stroke (Table 2).
TABLE 2.
Crude HRs, 95% CIs, and p Values for Mortality From Stroke and CHD, Computed Using Unadjusted Cox Regression
After adjusting for psychological distress and the other covariates (age, sex, smoking, BMI, and diabetes) in multivariate models, lower SES was associated with higher mortality rates from CHD and stroke. Similarly, after adjusting for SES and the other covariates, greater psychological distress was associated with higher mortality rates (Table 3).
TABLE 3.
Multivariate Cox Regression Model Showing HRs, 95% CIs, and p Values for Mortality From Stroke and CHD
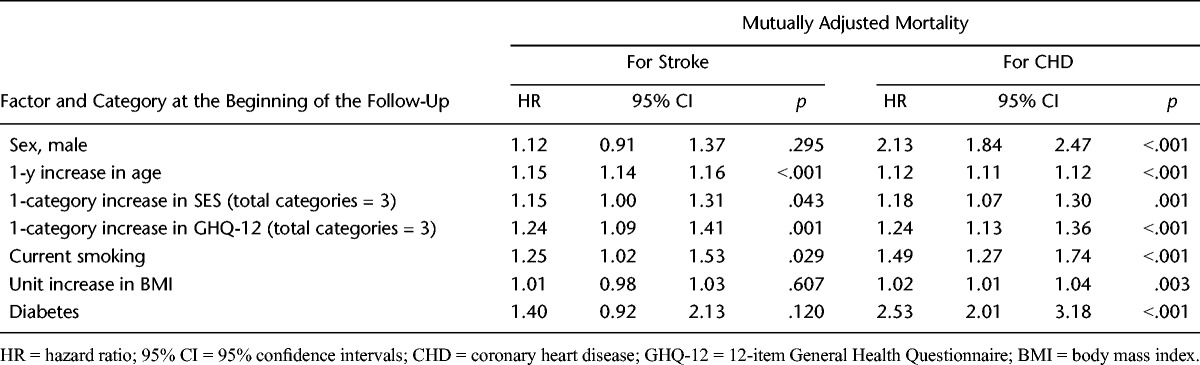
Table 4 presents the results of the analysis stratified by SES. After adjusting for age, sex, smoking, BMI, and diabetes, there was a significant interaction showing that psychological distress demonstrated stronger associations with both mortality outcomes in lower-SES participants (LRT, p < .05) and that there was a consistent risk gradient between low, medium, and high psychological distress within each category of SES. For example, the hazard ratio (HR) for death from CHD in lower-SES individuals was 1.39 (95% CI = 1.27–1.53, p < .001) for each one-category increase in psychological distress after adjusting for age and sex, and the HR for the fully adjusted model was 1.33 (95% CI = 1.19–1.48, p < .001); the HR for higher-SES individuals was 1.16 (95% CI = 1.04–1.29, p = .009) after adjusting for age and sex, and the HR for the fully adjusted model was 1.10 (95% CI = 0.97–1.25, p = .129).
TABLE 4.
Adjusted HRs and 95% CIs for Mortality From Stroke or CHD, as Function of Psychological Distress, Stratified by Socioeconomic Status
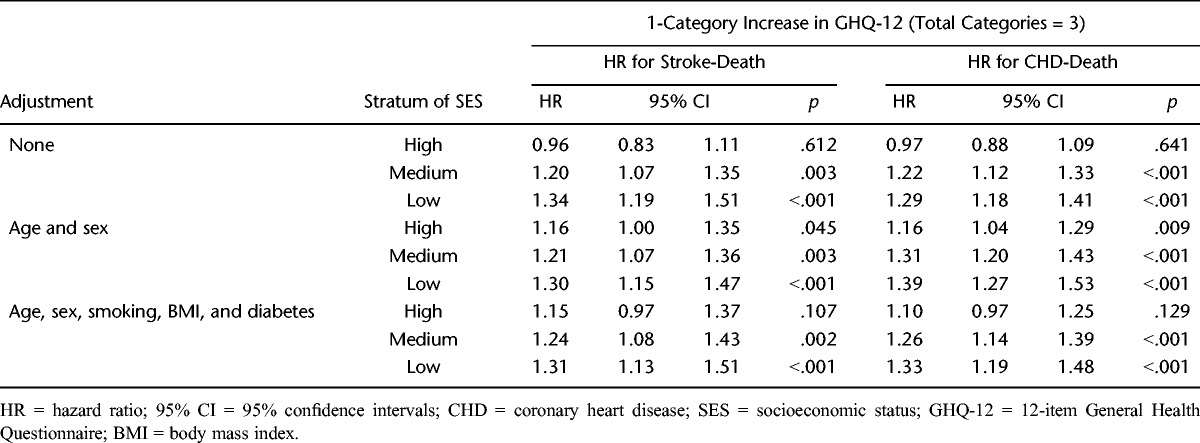
Figure 1 shows HRs for mortality from stroke and CHD adjusted for age and sex as functions of psychological distress, separately for each stratum of SES. The reference category is people with low psychological distress and high SES. The relationship between psychological distress and each mortality outcome differs by SES: it is stronger in lower-SES participants.
Figure 1.
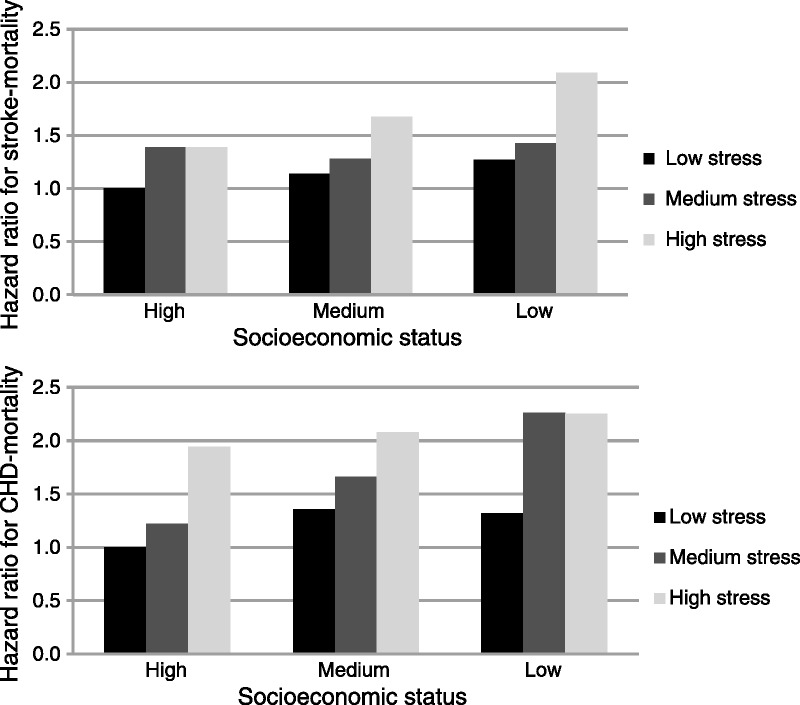
Hazard ratios for mortality from stroke or coronary heart disease (CHD) adjusted for age and sex, stratified by socioeconomic status and psychological distress.
Sensitivity analysis was conducted with inclusion of individuals with missing data for hypertension and physical activity levels and showed results similar to those in the main analyses: there were no differences in the key interactions between SES and psychological distress (data not shown). When the analyses were repeated after stratification by sex, older and younger age, and survey year, the results were similar to those in the main analyses (results not shown).
DISCUSSION
We recently hypothesized that when high levels of psychological distress and low levels of SES are present, the resulting effect on adverse health outcomes is not the mere sum of the two (additive effect) but that some extra risk may appear (multiplicative effect) (7). Our previous analysis demonstrated this pattern for all-cause mortality and the results of this study confirm that the association between psychological distress and mortality from CHD and stroke differs according to SES. Low SES operates as an amplifier of the noxious effect of psychological distress on mortality from CHD and stroke.
The effect of psychological distress on CHD or stroke outcomes after stratification by SES has never been studied directly, so this is the first study that has specifically set out to test this hypothesis. However, there have been some studies where a similar kind of interaction has been found. For example, a Swedish cohort study of nearly 3.5 million men and women showed that low job control was associated with stroke risk in women working in lower-status manual jobs but not in higher-status jobs (13). Another study of stroke in Japan found that job strain was correlated with higher chances of stroke in men from lower but not higher professional classes (12). Because lower SES categories are more likely to be exposed to greater adversity and stress, the question of whether work stress might account for the SES gradient in the risk of CHD or stroke has also been investigated (25–27). However, an analysis of Finnish public sector workers found that job demands either alone or in combination with job control accentuated rather than reduced socioeconomic differences in cerebrovascular disease (28). In the Whitehall study, effort-reward unbalance was found to be particularly deleterious with respect to CHD risk among those people with the lowest employment grades (29). A German cross-sectional study showed that stress at work was related to angina pectoris in the total study group, but the strongest associations were consistently observed in men and women with low educational level or low occupational position (30). In a Swedish study, researchers concluded that the heightened CHD risk of lower occupational class working women was accounted for, in part, by multiple sources of work and nonwork stress and their behavioral and biological correlates (31).
The pathways through which lower-SES individuals are more susceptible to stress than those from higher SES strata are not well understood. It has been argued that higher-SES individuals deploy more effective coping strategies and take advantage of larger support networks and greater material resources to deal with the potentially stressful circumstances (8). Biobehavioral differences may also be present, with more rapid recovery in cardiovascular responses after acute stress in higher SES categories (32,33); these may contribute to reduced progression in CVD pathology (34).
Psychological distress was only measured at the beginning of the study, and hence, we could not consider the effects of changes in distress over time. This may have caused exposure misclassification and thus may have diluted the results. The GHQ-12 has been validated as a measure of depression as assessed by Composite International Diagnostic Interview but is not designed to assess specific aspects of mental health such as anxiety (35). However, because the GHQ-12 assesses symptoms of anxiety, depression, and dysfunction in a combined measure of distress, it is particularly relevant in community-based samples because mental health problems in the community are often characterized by varying patterns of symptoms (36). The HSE does not unfortunately include measures of specific sources of life stress such as work stress, domestic strain, caregiver burden, or social isolation consistently over the different years. We do not therefore know whether the elevations in psychological distress were responses to adverse life conditions or enduring traits. We could have used other proxies of SES apart from occupational status, such as education or income. We preferred to use occupational class because it reflects socioeconomic circumstances and resources in midlife (37). We could not use household income because the HSE has a high missing values rate (approximately 50%) for this measure.
In conclusion, this study has demonstrated that the association between psychological distress and increased mortality from CHD and stroke is amplified in lower- compared with higher-SES individuals. Bolstering the psychological, social, and material capacity of lower-SES groups to manage life stress may be especially beneficial.
Acknowledgments
A.I.L. and M.H. had full access to the data and take responsibility for the integrity of the data and accuracy of the data analyses. A.I.L. and M.H. conducted the analyses. E.S. acquired the data set. All authors contributed to the concept and design of the study, drafting, and critical revision of the manuscript.
Source of Funding: This study was supported by grant RG/10/005/28296 from the British Heart Foundation.
Conflicts of Interest: The funder played no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript. The views expressed in this article are those of the authors and not necessarily of the funding bodies. The authors report no conflict of interest.
Abbreviations
- SES
socioeconomic status
- GHQ
General Health Questionnaire
- CVD
cardiovascular disease
- CHD
coronary heart disease
- HSE
Health Survey for England
- ICD
International Classification of Diseases
- LRT
likelihood ratio test
REFERENCES
- 1. Brotman DJ, Golden SH, Wittstein IS. The cardiovascular toll of stress. Lancet 2007; 370: 1089– 100 [DOI] [PubMed] [Google Scholar]
- 2. Steptoe A, Kivimaki M. Stress and cardiovascular disease. Nat Rev Cardiol 2012; 9: 360– 70 [DOI] [PubMed] [Google Scholar]
- 3. Surtees PG, Wainwright NW, Luben RN, Wareham NJ, Bingham SA, Khaw KT. Psychological distress, major depressive disorder, and risk of stroke. Neurology 2008; 70: 788– 94 [DOI] [PubMed] [Google Scholar]
- 4. Wilkinson R, Marmot MG. Social Determinants of Health: The Solid Facts. Copenhagen: World Health Organization, Regional Office for Europe; 2003 [Google Scholar]
- 5. Marmot M. Social determinants of health inequalities. Lancet 2005; 365: 1099– 104 [DOI] [PubMed] [Google Scholar]
- 6. Manrique-Garcia E, Sidorchuk A, Hallqvist J, Moradi T. Socioeconomic position and incidence of acute myocardial infarction: a meta-analysis. J Epidemiol Community Health 2011; 65: 301– 9 [DOI] [PubMed] [Google Scholar]
- 7. Lazzarino AI, Hamer M, Stamatakis E, Steptoe A. The combined association of psychological distress and socioeconomic status with all-cause mortality: a national cohort study. Arch Intern Med 2012; 3: 1– 6 [DOI] [PubMed] [Google Scholar]
- 8. Matthews KA, Gallo LC. Psychological perspectives on pathways linking socioeconomic status and physical health. Annu Rev Psychol 2011; 62: 501– 30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Russ TC, Stamatakis E, Hamer M, Starr JM, Kivimäki M, Batty GD. Association between psychological distress and mortality: individual participant pooled analysis of 10 prospective cohort studies. BMJ 2012; 345: e4933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Pitsavos C, Panagiotakos DB, Papageorgiou C, Tsetsekou E, Soldatos C, Stefanadis C. Anxiety in relation to inflammation and coagulation markers, among healthy adults: the ATTICA study. Atherosclerosis 2006; 185: 320– 6 [DOI] [PubMed] [Google Scholar]
- 11. Do DP, Dowd JB, Ranjit N, House JS, Kaplan GA. Hopelessness, depression, and early markers of endothelial dysfunction in U.S. adults. Psychosom Med 2010; 72: 613– 9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Tsutsumi A, Kayaba K, Ishikawa S. Impact of occupational stress on stroke across occupational classes and genders. Soc Sci Med 2011; 72: 1652– 58 [DOI] [PubMed] [Google Scholar]
- 13. Toivanen S, Hemström Ö. Is the impact of job control on stroke independent of socioeconomic status? A large-scale study of the Swedish working population. Stroke 2008; 39: 1321– 3 [DOI] [PubMed] [Google Scholar]
- 14. Kuper H, Marmot M. Job strain, job demands, decision latitude, and risk of coronary heart disease within the Whitehall II study. J Epidemiol Community Health 2003; 57: 147– 53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Bosma H, Stansfeld SA, Marmot MG. Job control, personal characteristics, and heart disease. J Occup Health Psychol 1998; 3: 402– 9 [DOI] [PubMed] [Google Scholar]
- 16. Toivanen S. Exploring the interplay between work stress and socioeconomic position in relation to common health complaints: the role of interaction. Am J Ind Med 2011; 54: 780– 90 [DOI] [PubMed] [Google Scholar]
- 17. Janszky I, Ahnve S, Lundberg I, Hemmingsson T. Early-onset depression, anxiety, and risk of subsequent coronary heart disease: 37-year follow-up of 49,321 young Swedish men. J Am Coll Cardiol 2010; 56: 31– 7 [DOI] [PubMed] [Google Scholar]
- 18.Department of Health. The Health Survey for England. Available at: http://www.dh.gov.uk/en/Publicationsandstatistics/PublishedSurvey/HealthSurveyForEngland/index.htm Accessed January 1, 2011.
- 19. Szreter SRS. The genesis of the Registrar-General’s social classification of occupations. Br J Sociol 1984; 35: 522– 46 [Google Scholar]
- 20.Official Documents. Available at: http://www.archive2.official-documents.co.uk/document/deps/doh/survey03/md/md-ap4.htm Accessed July 12, 2011.
- 21. Goldberg DP, Gater R, Sartorius N, Ustun TB, Piccinelli M, Gureje O, Rutter C. The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol Med 1997; 27: 191– 7 [DOI] [PubMed] [Google Scholar]
- 22. Hankins MCP. The factor structure of the twelve item General Health Questionnaire (GHQ-12): the result of negative phrasing? Clin Pract Epidemiol Ment Health 2008; 4: 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Stamatakis E, Hamer M, Lawlor DA. Physical activity, mortality, and cardiovascular disease: is domestic physical activity beneficial? The Scottish Health Survey—1995, 1998, and 2003. Am J Epidemiol 2009; 169: 1191– 200 [DOI] [PubMed] [Google Scholar]
- 24. Stamatakis E, Hillsdon M, Primatesta P. Domestic physical activity in relationship to multiple CVD risk factors. Am J Prev Med 2007; 32: 320– 7 [DOI] [PubMed] [Google Scholar]
- 25. Chandola T, Siegrist J, Marmot M. Do changes in effort-reward imbalance at work contribute to an explanation of the social gradient in angina? Occup Environ Med 2005; 62: 223– 30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Klabbers G, Bosma H, Van Lenthe FJ, Kempen GI, Van Eijk JT, Mackenbach JP. The relative contributions of hostility and depressive symptoms to the income gradient in hospital-based incidence of ischaemic heart disease: 12-year follow-up findings from the GLOBE study. Soc Sci Med 2009; 69: 1272– 80 [DOI] [PubMed] [Google Scholar]
- 27. Thurston RC, Kubzansky LD, Kawachi I, Berkman LF. Do depression and anxiety mediate the link between educational attainment and CHD? Psychosom Med 2006; 68: 25– 32 [DOI] [PubMed] [Google Scholar]
- 28. Kivimäki M, Gimeno D, Ferrie JE, Batty GD, Oksanen T, Jokela M, Virtanen M, Salo P, Akbaraly TN, Elovainio M, Pentti J, Vahtera J. Socioeconomic position, psychosocial work environment and cerebrovascular disease among women: the Finnish public sector study. Int J Epidemiol 2009; 38: 1265– 71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kuper H, Singh-Manoux A, Siegrist J, Marmot M. When reciprocity fails: effort-reward imbalance in relation to coronary heart disease and health functioning within the Whitehall II study. Occup Environ Med 2002; 59: 777– 84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Wege N, Dragano N, Erbel R, Jockel KH, Moebus S, Stang A, Siegrist J. When does work stress hurt? Testing the interaction with socioeconomic position in the Heinz Nixdorf Recall Study. J Epidemiol Community Health 2008; 62: 338– 41 [DOI] [PubMed] [Google Scholar]
- 31. Wamala SP, Mittleman MA, Horsten M, Schenck-Gustafsson K, Orth-Gomér K. Job stress and the occupational gradient in coronary heart disease risk in women. The Stockholm Female Coronary Risk Study. Soc Sci Med 2000; 51: 481– 9 [DOI] [PubMed] [Google Scholar]
- 32. Steptoe A, Feldman PM, Kunz S, Owen N, Willemsen G, Marmot M. Stress responsivity and socioeconomic status: a mechanism for increased cardiovascular disease risk? Eur Heart J 2002; 23: 1757– 63 [DOI] [PubMed] [Google Scholar]
- 33. Brydon L, Edwards S, Mohamed-Ali V, Steptoe A. Socioeconomic status and stress-induced increases in interleukin-6. Brain Behav Immun 2004; 18: 281– 90 [DOI] [PubMed] [Google Scholar]
- 34. Steptoe A, Marmot M. Impaired cardiovascular recovery following stress predicts 3-year increases in blood pressure. J Hypertens 2005; 23: 529– 36 [DOI] [PubMed] [Google Scholar]
- 35. Aalto AM, Elovainio M, Kivimäki M, Uutela A, Pirkola S. The Beck Depression Inventory and General Health Questionnaire as measures of depression in the general population: a validation study using the Composite International Diagnostic Interview as the gold standard. Psychiatry Res 2012; 197: 163– 71 [DOI] [PubMed] [Google Scholar]
- 36. Prince M, Patel V, Saxena S, Maj M, Maselko J, Phillips MR, Rahman A. No health without mental health. Lancet 2007; 370: 859– 77 [DOI] [PubMed] [Google Scholar]
- 37. Mirowsky J, Ross CE. Social Causes of Psychological Distress. New York: Aldine de Gruyter; 2003 [Google Scholar]


