Abstract
Objective
Effectiveness of a resuscitation strategy may vary across communities. We hypothesized that a strategy that prioritized initial Emergency Medical Services (EMS) rhythm analysis (Analyze Early) would be associated with survival advantage among EMS systems with lower baseline (pretrial) ventricular fibrillation (VF) survival, while a strategy that prioritized initial EMS CPR (Analyze Late) would be associated with survival advantage among systems with higher VF baseline survival.
Methods
We conducted a secondary, post-hoc study of a randomized trial of out-of-hospital cardiac arrest. Subjects were stratified according to randomization status (Analyze Early versus Analyze Late) and EMS agency baseline VF survival. We used a mixed-effects model to determine whether the association between favorable functional survival to hospital discharge and trial intervention (Analyze Late versus Analyze Early) differed according to EMS agency baseline VF survival (≤20% or >20%).
Results
Characteristics were similar among those randomized to Analyze Early (n=4964) versus Analyze Late (n=4426). For EMS agencies with baseline VF survival ≤20%, Analyze Late compared to Analyze Early was associated with a lower likelihood of favorable functional survival (3.8% versus 5.5%, OR=0.67 [0.50,0.90]). Conversely, among agencies with a VF survival >20%, Analyze Late compared to Analyze Early was associated with higher likelihood of favorable functional survival (7.5% versus 6.1%, OR=1.22 [0.98,1.52]). In the multivariable-adjusted model, for every 10% increase in baseline VF survival, Analyze Late versus Analyze Early was associated with a 34% increase in odds of favorable functional survival (OR=1.34 [1.07-1.66]).
Conclusion
The findings suggest that system-level characteristics may influence resuscitation outcomes.
Background and Importance
Out-of-hospital cardiac arrest is a common cause of death worldwide (1). Successful resuscitation is possible and requires a coordinated set of interdependent actions that include early identification, early CPR, early defibrillation, supportive advanced care, and expert post-resuscitation care (2). Despite a common understanding of these core tenets of resuscitation, survival varies substantially across communities, ranging more than 10-fold for bystander witnessed ventricular fibrillation (VF) arrest (1,3). This wide range of outcomes suggests that the effectiveness of some therapies may differ depending upon the community and the composition of resuscitation care. Thus an effective strategy of care in one community may be ineffective or even relatively harmful in another community.
We considered the potential for this type of differential therapeutic effect for CPR performed by emergency medical services (EMS). Animal and initial human studies indicated that a prolonged period of EMS CPR prior to rhythm analysis and shock - that could prime the heart prior to defibrillation - produced a better outcome than a strategy that prioritized early rhythm analysis and shock by EMS (4-8). These findings were the basis for a large multisite randomized trial comparing two strategies of EMS CPR, one where EMS prioritized initial rhythm analysis so provided CPR just long enough to prepare the patient for rhythm analysis and potential shock termed “Analyze Early” strategy, versus one where EMS provide 3 minutes of CPR initially prior to rhythm analysis and potential shock termed “Analyze Late” strategy (9).
Goals of This Investigation
The Analyze Early versus Analyze Late randomized trial conducted by the Resuscitation Outcomes Consortium found no difference in neurologically-favorable survival overall or among clinical subgroups defined by initial rhythm, response interval, or bystander CPR status (10). However, we hypothesized that the association of the EMS-based strategy may depend upon the resuscitation proficiency of an EMS system as gauged by VF survival. Specifically, we hypothesized that the Analyze Early strategy that prioritized initial EMS rhythm analysis would provide a survival advantage over Analyze Late among ROC EMS agencies with lower baseline VF survival. Conversely, we hypothesized that the Analyze Late strategy that prioritized 3 minutes of initial EMS CPR would provide a survival advantage over the Analyze Early strategy among ROC EMS agencies with a higher baseline VF survival. We undertook the investigation to evaluate the broader topic of how system factors might influence resuscitation outcomes.
METHODS
Study design, population, and setting
We conducted an ancillary, post-hoc study of Analyze Early versus Analyze Late randomized trial of the Resuscitation Outcomes Consortium (NCT00394706). The study was approved by the respective Review Boards. The original trial was conducted from June 2007 through November 2009 and was stopped prior to the planned full enrollment because ongoing recruitment was not likely to change the result of the study (9). The primary population for the current investigation was patients who suffered out-of-hospital cardiac arrest and were enrolled in the Analyze Early versus Analyze Late trial. Per the original trial design, the study excluded those arrest patients who were < 18 years of age or under the local age of consent, were pregnant, were a prisoner, had a do not resuscitate order, suffered a traumatic arrest, or experienced the arrest in the presence of EMS. Because the study hypothesized a differential association of the Analyze Early versus Analyze Late strategies as a consequence of baseline VF survival for each EMS agency, we also excluded those patients treated by EMS agencies that did not enroll patients in the ROC Epistry observational cohort prior to the randomized study, as we were unable to estimate a baseline (pretrial) EMS agency survival for bystander-witnessed VF not attributed to an obvious non-cardiac cause.
The Resuscitation Outcomes Consortium is comprised of 10 U.S and Canadian universities and their regional EMS systems, with the goal to evaluate promising clinical strategies to improve care for out-of-hospital cardiac arrest and life-threatening trauma. Collectively, the EMS systems serve a population of approximately 28 million persons. For the Analyze Early versus Analyze Late trial, a total of 139 EMS agencies participated across the 10 clinical sites.
Intervention
The primary intervention was the Analyze Early versus Analyze Late strategy for initial EMS CPR. The Analyze Early strategy consisted of less than 60 seconds of EMS CPR (sufficient time to place the defibrillator pads) before ECG rhythm analysis. The Analyze Late strategy consisted of 3 minutes of EMS CPR before the initial rhythm analysis. The trial used a cluster randomization design whereby EMS agencies were assigned either the Analyze Early or Analyze Late strategy for a period of 3-12 months and then crossed over to the alternate approach. All the clusters were assigned to cross over to the other strategy one or more times during the study at fixed intervals.
Methods and Measurements
Information was collected about patient, circumstance, and care characteristics using the Utstein data definitions from dispatch, EMS, and hospital records. CPR performance information was also collected from the electronic recordings of the defibrillator using a standard computerized data collection form. Specifically we used the defibrillator recording to determine the peri-shock pause. Peri-shock pause was defined as the pre-shock plus post-shock pauses. Pre-shock pause was the time interval between chest compression cessation and shock delivery. Post-shock pause was defined as the time between shock delivery and chest compression resumption. Chest compression cessation was detected using the impedance channel waveform (11). De-identified information was transmitted to a central coordinating center where computerized data checks evaluated for completeness and consistency of the data. Second reviewer abstraction was also performed in a small number of cases to assess the validity of the primary abstraction.
Outcomes
The primary outcome was survival with favorable functional status as defined by discharge from the hospital alive with a Modified Rankin Score of 3 or less. The function among those with a score of 3 or less ranges from no symptoms and no dependence to requiring moderate assistance such that they need help preparing meals or managing household chores but have mobility independence. Those in the lower-performing functional group require at least assistance for basic activities of daily living (e.g. eating, walking, and toileting).
Analysis
Baseline (pretrial) bystander-witnessed VF survival according to EMS agency
We used bystander-witnessed VF not attributed to an obvious non-cardiac cause – subsequently referred to as baseline VF survival - as the gauge for baseline EMS agency resuscitation performance because this clinical group is defined by the Utstein template as the standard for reporting outcomes (12). To determine the baseline EMS agency VF survival, we used the Resuscitation Outcomes Consortium Cardiac Arrest Epistry (13). The Epistry is a population based observational cohort of consecutive cases. We used data from December 2005 through March 2007. The data resource has been used to assist in study design as well as for a variety of observational investigations. The large majority of EMS agencies that participated in the Analyze Early versus Analyze Late trial had previously participated in the Epistry activity. Estimates for baseline VF survival were determined using a binomial family mixed effects model with a logistic link function. This model included random effects for site and agency and fixed effects for multiple Utstein covariates. We then estimated agency-specific survival for VF arrest. For subjects that were treated by multiple EMS agencies, we considered the first arriving agency as the treating agency. We subsequently stratified descriptive comparisons using a baseline VF survival of ≤ or > 20% as summary studies of community-based survival have reported a median VF survival of approximately 20% (14,15).
Primary Analyses
We used descriptive analyses to stratify characteristics and outcomes according to baseline VF survival (≤ 20% versus > 20%) and Analyze Early versus Analyze Late status. In the inferential analyses to assess whether the association of the trial intervention (Analyze Early versus Analyze Late) differed based on baseline agency VF survival rate, we again used a binomial family mixed effects model with a logistic link function (16). The primary exposures included the Analyze Early versus Analyze Late intention-to-treat assignment, agency-adjusted baseline VF survival rate, and an interaction term between these two variables. If the association of Analyze Early versus Analyze Late was significantly modified by baseline agency VF survival, the interaction term should statistically improve the fit of the data as assessed by the likelihood ratio test. We first modeled baseline VF survival as a dichotomous exposure (≤ or > 20%). In the primary inferential analysis, we modeled baseline VF survival as a continuous exposure. The multivariable model adjusted for age, sex, witness status, public location, bystander CPR, EMS response interval, and initial EMS rhythm and a random effects term for site. We included these covariates based on scientific understanding that these characteristics can influence resuscitation prognosis, and so may in turn have the potential to confound the relationships of interest. We plotted the results of the logistic model as well as a lowess smoothed curve (17). In an additional model, we also adjusted for peri-shock pause to help determine if this variable explained the potential relationship (11,18).
We also evaluated whether the relationship differed among subgroups defined by initial rhythm, witness status, and randomization compliance (efficacy) by using the Breslow-Day test. Randomization compliance was determined by whether a patient randomized to Analyze Early received their first rhythm analysis during the first minute of EMS care. Compliance with the Analyze Late assignment was determined by whether the patient received at least 2.5 minutes but less than 3.5 minutes of EMS CPR prior to the first rhythm analysis. Analyses were done using R version 2.14 or SAS version 9.3.
RESULTS
Enrollment and eligibility
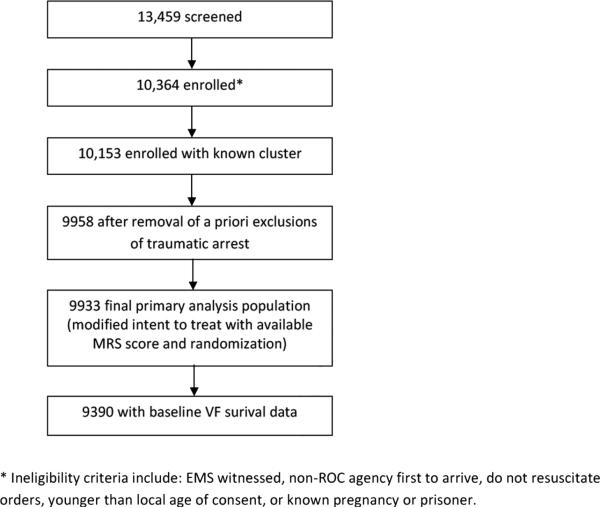
Figure 1 presents the flow diagram for patient inclusion in the current investigation. The original trial enrolled 9933 subjects; 5290 randomized to the Analyze Early strategy and 4693 randomized to the Analyze Late strategy. Of these 9933 patients, 543 from 12 EMS agencies were excluded because the treating EMS agency did not have sufficient information in the Epistry to estimate a baseline VF survival. The remaining 9390 patients were treated by 127 EMS agencies; 4964 randomized to Analyze Early and 4426 randomized to Analyze Late. The agency-specific, baseline bystander-witnessed VF survival rate was derived from a total of 7306 Epistry cases.
Figure 1.
Analyze Early versus Analyze Late Study Population
Characteristics
Table 1 presents the data stratified according to EMS agency specific baseline bystander- VF survival > or ≤ 20% and Analyze Early versus Analyze Late status. Characteristics were similar for those randomized to Analyze Early compared to those randomized to Analyze Late overall and when restricted to the particular baseline VF survival strata. Those patients treated by EMS systems with baseline VF survival ≥ 20% compared to those with survival < 20% were more likely to be younger, receive bystander CPR, receive EMS first response from BLS-level rather than ALS level providers, and achieve a shorter peri-shock pause regardless of the intervention strategy (Analyze Early or Analyze Late) (p<0.05 for all comparisons).
Table 1.
Characteristics according to baseline bystander-witnessed VF survival and Analyze Early versus Analyze Late status
| Characteristic | Baseline Survival ≤ 20% | Baseline Survival > 20% | ||
|---|---|---|---|---|
| Treatment Strategy | Analyze Early | Analyze Late | Analyze Early | Analyze Late |
| N=2291 | N=1903 | N=2673 | N=2523 | |
| EMS response interval (minutes), mean (sd) | 6.1 (2.7) | 6.0 (2.7) | 6.0 (2.8) | 6.0 (2.6) |
| Arrest witnessed, %* (n) | 45.9 (1030) | 45.8 (855) | 44.4 (1152) | 44.7 (1085) |
| Bystander CPR, %* (n) | 34.6 (799) | 35.0 (666) | 42.5 (1135) | 44.8 (1135) |
| Age (years), mean (sd) | 67.9 (16.3) | 68.0 (15.7) | 66.0 (16.8) | 66.1 (17.1) |
| Male, %* (n) | 65.4 (1499) | 64.7 (1232) | 64.1 (1713) | 63.5 (1601) |
| Public location, % (n) | 13.7 (315) | 14.3 (273) | 14.2 (381) | 14.5 (365) |
| Presumed cardiac cause, %* (n) | 97.9 (2242) | 98.0 (1864) | 97.9 (2616) | 97.6 (2462) |
| Service level of first vehicle to arrive | ||||
| BLS, %* (n) | 3.2 (74) | 74.1 (77) | 0.6 (16) | 0.1 (2) |
| BLS-D, %* (n) | 38.7 (886) | 39.9 (758) | 65.5 (1751) | 66.1 (1667) |
| BLS+, %* (n) | 15.6 (357) | 15.9 (302) | 11.0 (295) | 11.4 (288) |
| ALS, %* (n) | 42.5 (973) | 40.2 (765) | 22.9 (611) | 22.4 (566) |
| Peri-shock pause (seconds), mean (sd) | 30.6 (16.7) | 31.7 (15.9) | 21.7 (12.4) | 22.0 (12.8) |
| EMS initial rhythm | ||||
| VF, %* (n) | 26.0 (594) | 25.6 (484) | 23.3 (617) | 25.1 (627) |
| PEA, %* (n) | 19.1 (437) | 18.8 (355) | 19.5 (516) | 19.0 (474) |
| Asystole, %* (n) | 46.8 (1069) | 48.0 (908) | 46.4 (1226) | 45.3 (1131) |
| Perfusing, %* (n) | 0.1 (3) | 0.3 (5) | 0.1 (2) | 0.3 (7) |
| No shock and no strip, %* (n) | 8.0 (182) | 7.4 (140) | 10.7 (284) | 10.4 (259) |
EMS interval is the time from call receipt by emergency dispatch center to the time EMS arrives at the scene of the arrest. Baseline survival is for bystander-witnessed VF not attributed to an obvious non-cardiac cause. Basic life support is abbreviated BLS. Advanced life support is abbreviated ALS. Basic life support defibrillation is abbreviated BLS-D. BLS-D providers are equipped with defibrillation capability (AEDs). BLS+ are BLS providers with limited ALS scope of practice. For example, some BLS+ providers can place an intravenous access or supraglottic airways. Pulseless electrical activity is abbreviated PEA. Perfusing rhythm patients were noted to have a pulse upon the first EMS rhythm analysis.
% of known
Main results
Table 2 presents outcomes stratified according to EMS-agency specific baseline VF survival ≤ or > 20% and Analyze Early or Analyze Late status. Better baseline VF survival predicted better outcomes in the trial regardless of Analyze Early or Analyze Late Status. For EMS agencies with a baseline VF survival rate ≤20%, Analyze Late compared to Analyze Early was associated with a lower likelihood of favorable functional survival (3.8% versus 5.5%, OR=0.67 [0.50,0.90]). Conversely, among agencies with a baseline VF survival rate > 20%, Analyze Late compared to Analyze Early was associated with higher likelihood of favorable functional survival (7.5% versus 6.1%, OR=1.22 [0.98,1.52]), though the 95% confidence interval overlapped 1.0. In the model that included Analyze Early versus Analyze Late status, baseline VF survival modeled as a dichotomous exposure (≤ or > 20%), and the respective interaction term, the addition of an interaction term significantly improved the fit of the data according to the likelihood ratio test (p=0.006). The results were similar when restricted to the core Utstein comparator group of bystander-witnessed VF arrest. For those EMS agencies with a baseline VF survival ≤ 20%, Analyze Late compared to Analyze Early was associated with a lower likelihood of favorable neurological survival (15.8% versus 22.3%, OR=0.65 [0.45,0.95]). Conversely, for those EMS agencies with a baseline VF survival > 20%, Analyze Late compared to Analyze Early was associated with a higher likelihood of favorable neurological survival (28.5% versus 25.4%, OR=1.18 [0.98,1.52]). Similarly an interaction term significantly improved the fit of the model (p=0.02).
Table 2.
Outcomes according to baseline bystander-witnessed VF survival and Analyze Early versus Analyze Late status
| Baseline VF Survival ≤ 20% | Baseline VF Survival > 20% | |||
|---|---|---|---|---|
| Treatment Strategy | Analyze Early | Analyze Late | Analyze Early | Analyze Late |
| N=2291 | N=1903 | N=2673 | N=2523 | |
| ROSC at ED arrival, % (n) | 19.8 (453) | 19.8 (377) | 30.2 (806) | 31.1 (783) |
| Survived to hospital discharge, % (n) | 6.8 (155) | 5.1 (97) | 9.4 (251) | 10.1 (255) |
| Favorable functional survival % (n) | 5.5 (127) | 3.8 (72) | 6.2 (167) | 7.5 (189) |
| Odds ratio of favorable survival, (95%CI)* | 1 (reference) | 0.67 (0.50, 0.90) | 1.14 (0.90, 1.44) | 1.38 (1.09, 1.74) |
For the comparison of Analyze Late versus Analyze Early for the strata with baseline VF survival > 20%, the OR=1.22 (0.98,1.51)
Favorable neurological survival defined as survival to hospital discharge with a Modified Rankin Scale≤3. Ventricular fibrillation is abbreviated VF. Confidence interval is abbreviated CI.
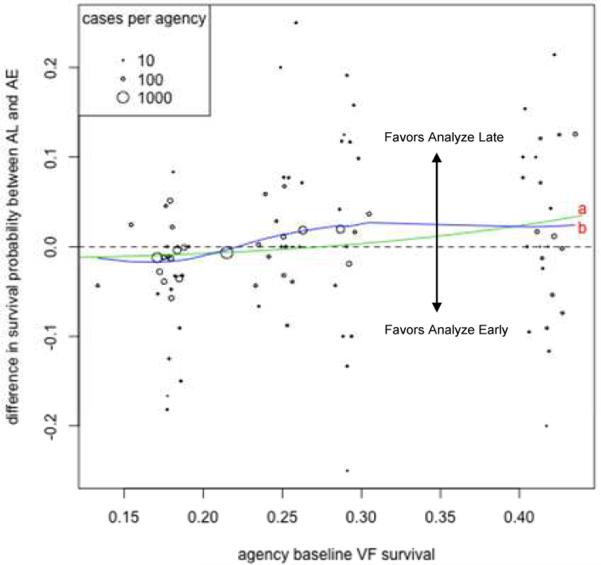
Table 3 presents the results of the primary inferential analysis. The addition of the interaction term between Analyze Early versus Analyze Late status and baseline VF survival was significant (p=0.009). For every 10% improvement in baseline VF survival, the Analyze Late as compared with the Analyze Early approach was associated with a 34% increase in the odds of survival with favorable neurological function after adjustment for potential confounders (OR=1.34 [1.07,1.66]). Figure 2 presents a scatter plot of agency's probability of favorable neurological survival for Analyze Late compared to Analyze Early versus EMS agency baseline VF survival and includes the logistic model and weighted lowess superimposed curves. For each of these curves, the slope was significantly different from 1.
Table 3.
Primary logistic regression model of odds of favorable functional survival
| Primary Model | Model with peri-shock pause* | |
|---|---|---|
| Predictor variable | OR (95% CI) | OR (95% CI) |
| Analyze Early | 1 (reference) | 1 (reference) |
| Analyze Late | 0.75 (0.59, 0.96) | 0.83 (0.59, 1.18) |
| Epistry survival rate for a +10% difference | 1.26 (1.05, 1.52) | 1.26 (1.03, 1.53) |
| Interaction between Analyze Late and baseline survival, For a +10% difference | 1.34 (1.07, 1.66) | 1.28 (0.97, 1.70) |
| Peri-shock pause, median from the first three shocks | ----- | |
| <20 seconds | ----- | 1 (reference) |
| ≥ 20 seconds, <40 seconds | ----- | 0.69 (0.51, 0.92) |
| ≥ 40 seconds | ----- | 0.64 (0.38, 1.10) |
| Covariates | ||
| Bystander CPR | 1.25 (1.02, 1.54) | 1.15 (0.86, 1.52) |
| Witnessed arrest | 2.49 (1.95, 3.19) | 2.89 (2.02, 4.14) |
| Age, for 1 year increase | 0.96 (0.95, 0.97) | 0.96 (0.96, 0.97) |
| Public location | 1.82 (1.47, 2.25) | 1.65 (1.24, 2.20) |
| EMS Arrival ≤ 10 minutes | 2.11 (1.23, 3.62) | 2.09 (0.99, 4.41) |
| No obvious cause | 1.35 (0.52, 3.54) | -- |
| Male | 1.01 (0.80, 1.28) | 0.96 (0.69, 1.35) |
| EMS Initial Rhythm | ||
| VF/VT | 1 (reference) | -- |
| PEA | 0.19 (0.14, 0.26) | -- |
| Asystole | 0.03 (0.02, 0.05) | -- |
| Perfusing | 5.17 (1.74, 15.34) | -- |
| AED, no-shock, no-strip | 0.14 (0.08, 0.23) | -- |
Pulseless electrical activity is abbreviated PEA. Model with peri-shock pause is restricted to those presenting with an initial shockable rhythm.
Restricted to those with an initial rhythm of ventricular fibrillation
Figure 2.
Plot of the difference in the probability of favorable survival for Analyze Late compared to Analyze Early according to baseline VF survival by agency. Line (a) is the model-fitted probability and line (b) is a weighted lowess smooth curve.
This overall relationship of Analyze Late benefit with increasing baseline VF survival was evident among subgroups defined by initial arrest rhythm, Analyze Early versus Analyze Late intervention compliance, and witness status. For example, for each 10% increase in baseline VF survival, the Analyze Late versus Analyze Early approach was associated with a 31% increase in the odds of survival with favorable neurological function among those with VF (n=2433, OR=1.31,[1.03,1.68]) and a 32% increase in odds of survival with favorable neurological function among witnessed arrests (n=4346, OR=1.32 [1.03,1.70]). Three quarters of cases (6998/9390) achieved randomization compliance as defined in the Methods. Among those cases compliant with the study intervention , the Analyze Late versus Analyze Early approach was associated with a 32% increase in odds of survival with favorable neurological function for each 10% increase in baseline VF survival (OR=1.32 [1.03,1.69]). Among the VF subset, additional adjustment for the peri-shock pause attenuated the interaction such that term was no longer statistically significant (OR = 1.28 [0.97, 1.70]).
LIMITATIONS
The study has limitations. The current study was not prospectively designed to test whether the survival effects of the Analyze Early versus Analyze Late strategy differed according to an EMS agency's baseline VF survival rate. Hence the results cannot be used to establish optimal clinical practice. To this point, the study is not able to determine an optimal survival cut-point for which an EMS agency would use one or the other CPR strategies. Moreover, we could not determine the specific mechanism responsible for the potential differential outcome association of the EMS CPR intervention. We did not have comprehensive information involving different CPR metrics. Moreover, characteristics such as provider experience may contribute to the observed relationships but such information was not available for this analysis. We classified care by the level of the first arriving EMS agency. We appreciate that an agency-based classification is likely not an optimal approach to categorizing a system's performance. Resuscitation ideally is a coordinated process that often involves multiple EMS agencies, multiple persons, and multiple interventions so that care is often integrated in a complex manner that comprises an “EMS system”. Finally, the study excluded about 6% of cases (543/9933) because the EMS agencies had not participated in Epistry and so we could not derive a baseline VF survival. These limitations should be considered in the context of the study's strengths: the study was conducted across a number of EMS agencies so enables the current hypothesis to be evaluated, the Analyze Early versus Analyze Late intervention was randomized, outcomes included functional status at hospital discharge and was comprehensively ascertained.
DISCUSSION
In this population-based ancillary study of a large randomized trial, the effectiveness of the EMS initial CPR strategy – either Analyze Early or Analyze Late – appeared to differ according to the EMS agency's resuscitation proficiency as gauged by the agency's baseline VF survival. Specifically, we observed a relationship whereby the Analyze Late strategy versus Analyze Early strategy was associated with increasing odds of neurologically-favorable survival as the EMS agency's baseline VF survival increased. Placed in clinical context, one interpretation is that an Analyze Early strategy was more beneficial among those EMS agencies with lower baseline survival while an Analyze Late strategy was more beneficial among those EMS agencies with a higher baseline survival. The findings may help explain prior conflicting study results and support the notion that the optimal initial EMS resuscitation strategy may differ depending upon a system's characteristics (4-8).
Survival following cardiac arrest varies substantially across communities. Only a modest portion of this variability can be attributed to system differences in the Utstein variables that measure patient demographics, early bystander CPR, and EMS response, suggesting that other therapeutic factors may have an important role in prognosis (19). To this end, some evidence indicates that EMS CPR performance can influence prognosis, as changes in EMS protocol or emphasis on CPR “quality” have been associated with improvements in outcome (20,21). Thus a strategy that varies the initial period of EMS CPR prior to rhythm assessment – such as Analyze Early versus Analyze Late - may affect survival. We hypothesized however that the fidelity of this CPR strategy would depend upon the EMS agency's overall resuscitation proficiency as determined by the agency's historical bystander-witnessed VF survival.
We observed that on average the Analyze Late strategy was associated with better outcome among EMS agencies with better baseline VF survival. One possible explanation is that the Analyze Late strategy – which emphasizes a prolonged period of initial EMS CPR – would favor EMS agencies that perform better CPR and in turn maximize the positive effect of the prolonged CPR. In contrast, an Analyze Early CPR strategy may favor EMS agencies that provide less effective CPR. We did observe that EMS agencies with better baseline survival had a shorter peri-shock interruption during the trial, a relationship that is consistent with the hypothesized mechanism. However adjustment for peri-shock pause, a metric associated with clinical outcome, attenuated the interaction term only modestly (the point estimate for the interaction term decreasing from 1.31 to 1.28). The result suggests that a CPR performance metric does not sufficiently explain the observed outcome relationships between trial intervention status and outcome. Another explanation is that “EMS CPR” is much more complex than peri-shock pause alone and includes other dynamic components of CPR such as compression depth, rate, release and how these components are integrated with airway management, ventilation strategy, medication treatments, and defibrillation – information not comprehensively available for this investigation (2).
What are the implications of the study's results? To date, most investigations have evaluated how individual case-specific characteristics are related to outcome. However there is an increasing appreciation that successful resuscitation following out-of-hospital cardiac arrest involves a system of care, an appreciation consistent with the links in the chain metaphor (22). The current investigation provides an instructive example of how “system” factors may influence the potential effectiveness of resuscitation therapies, and supports additional efforts to understand the prognostic interplay between case-specific and system characteristics.
In this ancillary investigation of a large trial evaluating an initial EMS CPR strategy, we observed a consistent statistical interaction indicating that the Analyze Early strategy was associated with greater likelihood of neurologically-favorable survival among EMS agencies with lower baseline VF survival while the Analyze Late strategy was associated with greater likelihood of neurologically-favorable survival among EMS agencies with a higher baseline VF survival. Although case-specific characteristics predict outcome, the findings from the current investigation suggest that system-level characteristics may influence the effectiveness of resuscitation treatments. These results emphasize the need for future development and validation of more nuanced survival models that potentially include multiple system-level factors. Such an understanding could enable more effective resuscitation care and in turn improve cardiac arrest outcomes.
Acknowledgments
Funding Support: The Resuscitation Outcomes Consortium is supported by a series of cooperative agreements to nine regional clinical centers and one Data Coordinating Center (5U01 HL077863-University of Washington Data Coordinating Center, HL077866-Medical College of Wisconsin, HL077867-University of Washington, HL077871-University of Pittsburgh, HL077872-St. Michael's Hospital, HL077873-Oregon Health and Science University, HL077881-University of Alabama at Birmingham, HL077885-Ottawa Hospital Research Institute, HL077887-University of Texas SW Medical Center/Dallas, HL077908-University of California San Diego) from the National Heart, Lung and Blood Institute in partnership with the National Institute of Neurological Disorders and Stroke, U.S. Army Medical Research & Material Command, The Canadian Institutes of Health Research - Institute of Circulatory and Respiratory Health, Defence Research and Development Canada and the Heart, Stroke Foundation of Canada and the American Heart Association. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung and Blood Institute or the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
To be presented at the American Heart Association Scientific Sessions, November 17, 2013
No conflicts of interest
TR conceived the study. All the authors had a role in conduct of the original randomized trial including implementation and data collection. DP provided statistical expertise and analyzed the data. TR drafted the manuscript, and all authors contributed substantially to its revision. TR and DP take responsibility for the paper as a whole.
Contributor Information
Thomas Rea, Department of Medicine, University of Washington, Seattle WA.
David Prince, Department of Biostatistics, University of Washington, Seattle WA.
Laurie Morrison, University of Toronto and St Michael's Hospital, Toronto, ON.
Clifton Callaway, Department of Emergency Medicine, University of Pittsburgh, Pittsburgh, PA.
Tom Aufderheide, Department of Emergency Medicine, Medical College of Wisconsin, Milwaukee, WI.
Mohamed Daya, Department of Emergency Medicine, Oregon Health Science University, Portland, OR.
Ian Stiell, Department of Emergency Medicine, University of Ottawa, Ottawa, ON.
Jim Christenson, Department of Emergency Medicine, University of British Columbia, Vancouver, BC.
Judy Powell, Department of Biostatistics, University of Washington, Seattle WA.
Craig Warden, Department of Emergency Medicine, Oregon Health Science University, Portland, OR.
Lois van Ottingham, Department of Biostatistics, University of Washington, Seattle WA.
Peter Kudenchuk, Department of Medicine, University of Washington, Seattle WA.
Myron Weisfeldt, Department of Medicine, Johns Hopkins University, Baltimore, MD.
References
- 1.Berdowski J, Berg RA, Tijssen JG, Koster RW. Global incidences of out-of-hospital cardiac arrest and survival rates: Systematic review of 67 prospective studies. Resuscitation. 2010;81(11):1479–87. doi: 10.1016/j.resuscitation.2010.08.006. [DOI] [PubMed] [Google Scholar]
- 2.Hazinski MF, Nolan JP, Billi JE, et al. Part 1: Executive summary: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation. 2010;122(16 Suppl 2):S250–75. doi: 10.1161/CIRCULATIONAHA.110.970897. [DOI] [PubMed] [Google Scholar]
- 3.Nichol G, Thomas E, Callaway CW, et al. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008;300(12):1423–31. doi: 10.1001/jama.300.12.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wik L, Hansen TB, Fylling F, et al. Delaying defibrillation to give basic cardiopulmonary resuscitation to patients with out-of-hospital VF: a randomized trial. JAMA. 2003;289(11):1389–95. doi: 10.1001/jama.289.11.1389. [DOI] [PubMed] [Google Scholar]
- 5.Cobb LA, Fahrenbruch CE, Walsh TR, et al. Influence of cardiopulmonary resuscitation prior to defibrillation in patients with out-of-hospital VF. JAMA. 1999;281(13):1182–8. doi: 10.1001/jama.281.13.1182. [DOI] [PubMed] [Google Scholar]
- 6.Jacobs IG, Finn JC, Jelinek GA, Oxer HF, Thompson PL. Effect of adrenaline on survival in out-of-hospital cardiac arrest: A randomised double-blind placebo-controlled trial. Resuscitation. 2011;82(9):1138–43. doi: 10.1016/j.resuscitation.2011.06.029. [DOI] [PubMed] [Google Scholar]
- 7.Baker PW, Conway J, Cotton C, et al. Defibrillation or cardiopulmonary resuscitation first for patients with out-of-hospital cardiac arrests found by paramedics to be in VF? A randomised control trial. Resuscitation. 2008;79(3):424–31. doi: 10.1016/j.resuscitation.2008.07.017. [DOI] [PubMed] [Google Scholar]
- 8.Niemann JT, Cairns CB, Sharma J, Lewis RJ. Treatment of prolonged VF. Immediate countershock versus high-dose epinephrine and CPR preceding countershock. Circulation. 1992;85:281–7. doi: 10.1161/01.cir.85.1.281. [DOI] [PubMed] [Google Scholar]
- 9.Stiell IG, Callaway C, Davis D, et al. Resuscitation Outcomes Consortium (ROC) PRIMED cardiac arrest trial methods part 2: rationale and methodology for “Analyze Later vs. Analyze Early” protocol. Resuscitation. 2008;78(2):186–95. doi: 10.1016/j.resuscitation.2008.01.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stiell IG, Nichol G, Leroux BG, et al. Early versus later rhythm analysis in patients with out-of-hospital cardiac arrest. N Engl J Med. 2011;365(9):787–97. doi: 10.1056/NEJMoa1010076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cheskes S, Schmicker RH, Christenson J, et al. Perishock pause: an independent predictor of survival from out-of-hospital shockable cardiac arrest. Circulation. 2011;124(1):58–66. doi: 10.1161/CIRCULATIONAHA.110.010736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jacobs I, Nadkarni V, Bahr J, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries. Circulation. 2004;110(21):3385–97. doi: 10.1161/01.CIR.0000147236.85306.15. [DOI] [PubMed] [Google Scholar]
- 13.Morrison LJ, Nichol G, Rea TD, et al. Rationale, development and implementation of the Resuscitation Outcomes Consortium Epistry-Cardiac Arrest. Resuscitation. 2008;78(2):161–9. doi: 10.1016/j.resuscitation.2008.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rea TD, Eisenberg MS, Sinibaldi G, White RD. Incidence of EMS-treated out-of-hospital cardiac arrest in the United States. Resuscitation. 2004;63(1):17–24. doi: 10.1016/j.resuscitation.2004.03.025. [DOI] [PubMed] [Google Scholar]
- 15.Atwood C, Eisenberg MS, Herlitz J, Rea TD. Incidence of EMS-treated out-of-hospital cardiac arrest in Europe. Resuscitation. 2005;67(1):75–80. doi: 10.1016/j.resuscitation.2005.03.021. [DOI] [PubMed] [Google Scholar]
- 16.Wakefield Jon. Bayesian and Frequentist Regression Methods. Springer; New York: 2013. General Regression Models. pp. 425–500. [Google Scholar]
- 17.Cleveland William S. Robust locally weighted regression and smoothing scatterplots. Journal of the American Statistical Association. 1979;74(368):829–836. [Google Scholar]
- 18.Cheskes S, Schmicker RH, Verbeek PR, et al. The impact of peri-shock pause on survival from out- of- hospital shockable cardiac arrest during the Resuscitation Outcomes Consortium PRIMED trial. Resuscitation. doi: 10.1016/j.resuscitation.2013.10.014. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rea TD, Cook AJ, Stiell IG, et al. Predicting survival after out-of-hospital cardiac arrest: role of the Utstein data elements. Ann Emerg Med. 2010;55(3):249–57. doi: 10.1016/j.annemergmed.2009.09.018. [DOI] [PubMed] [Google Scholar]
- 20.Rea TD, Helbock M, Perry S, et al. Increasing use of cardiopulmonary resuscitation during out-of- hospital VF arrest: survival implications of guideline changes. Circulation. 2006;114(25):2760–5. doi: 10.1161/CIRCULATIONAHA.106.654715. [DOI] [PubMed] [Google Scholar]
- 21.Bobrow BJ, Vadeboncoeur TF, Stolz U, et al. The Influence of Scenario-Based Training and Real-Time Audiovisual Feedback on Out-of-Hospital Cardiopulmonary Resuscitation Quality and Survival From Out of-Hospital Cardiac Arrest. Ann Emerg Med. 2013;62(1):47–56. doi: 10.1016/j.annemergmed.2012.12.020. 2013. [DOI] [PubMed] [Google Scholar]
- 22.Rea TD, Page RL. Community approaches to improve resuscitation after out-of-hospital sudden cardiac arrest. Circulation. 2010;121(9):1134–40. doi: 10.1161/CIRCULATIONAHA.109.899799. [DOI] [PubMed] [Google Scholar]