Abstract
Mayer-Rokitanski-Kuster-Hauser (MRKH) syndrome is a rare disease. A 27-year-old woman was admitted for primary amenorrhea and cyclic pelvic pain. Magnetic resonance imaging (MRI) revealed bilateral Müllerian remnants with functioning endometrium and a pelvic mass considered to be an endometriotic cyst. Bilateral Müllerian remnants were removed, and right ovarian cystectomy was performed at laparoscopic surgery. Accurate evaluation before the operation and informed consent are necessary to treat patients with MRKH syndrome.
Keywords: Mayer-Rokitanski-Kuster-Hauser syndrome, vaginal agenesis, endometriosis
Introduction
Mayer-Rokitanski-Kuster-Hauser (MRKH) patients do not always have agenesis of the vagina; sometimes the lower vagina is normal and only the upper two-thirds is missing. Müllerian remnants have reportedly been often observed. It has been reported that a small uterine corpus with functioning endometrium was present.1,2 It had been recognized that endometriosis is a disease that affects 6% to 10% of women of reproductive age.3
We present the case of a woman who was diagnosed with MRKH syndrome with a unilateral endometriotic cyst who had been in cyclic pain. Hence, preoperative continuous combined oral contraceptives (OC) were administrated to control symptoms of the endometriosis and amenorrhea. The patient has given her consent for publication of this case report.
Case Report
A 27-year-old woman, gravida 0, was admitted to our hospital complaining of primary amenorrhea and lower abdominal pain. She had been described previously because a laparoscopic examination had been performed when she was 17 years old. The patient was Tanner stage 3 for pubic hair and Tanner stage 4 for breast development. Physical examination revealed external genitalia with a 1 cm vaginal dimple.
Pelvic magnetic resonance imaging showed 2 structures of Müllerian remnants and a cystic mass about 7.0 cm in diameter (Fig. 1) in the right side of the pelvic cavity. It was a heterogeneous, nonenhancing simple cystic mass with fluid-fluid levels likely representing blood products. Magnetic resonance imaging (MRI) also confirmed the absence of a normal uterus and vagina. However, bilateral Müllerian remnants with a small endometrium were inferred. The patient’s history was unremarkable except for amenorrhea. Bilateral kidneys were detected by pyelography. After that, low-dose oral contraceptives did not give the patient relief from the pain, as she chronically suffered from cyclic lower abdominal pain. She hoped to have the Müllerian remnants and the endometriotic cyst resected and firmly desired vaginoplasty. Other physical examinations showed normal findings, and the parameters from blood chemistry studies were within normal limits.
Figure 1.

Pelvic MRI images are shown (sagittal view).
Abbreviations: P, pubic symphysis; R, rectum.
Laparoscopic surgery to remove the abnormal structures was planned. After the patients gave written informed consent, vaginoplasty with a vaginal dilator (Protese, Atom Medical Co Ltd, Tokyo, Japan) was performed. The patient also underwent laparoscopic cystectomy of the right ovarian endometriotic cyst and resection of the Müllerian remnants. Bilateral fibrous bands with uterine horns were also removed, whereas the left ovary and fallopian tube were left in situ (Fig. 2). The findings of the operative specimen revealed a non-canalized bilateral uterine horn with functional small endometrium, thinning smooth muscle, fibrotic right ovary, and, under histopathologic examination an endometriotic cyst (Fig. 3).
Figure 2.
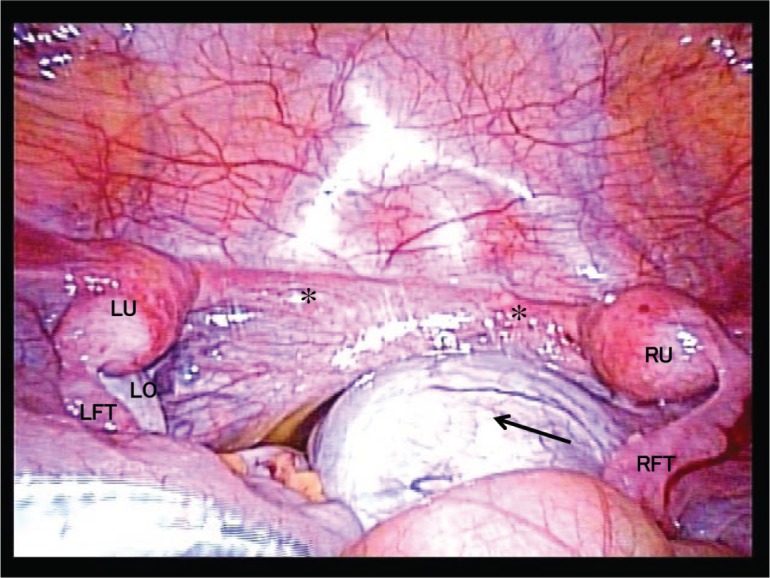
Laparoscopic images are shown. Bilateral uterine remnant with fibrous band and endometriotic cyst complex are detected. Normal left ovary and fallopian tube. Bilateral fibrotic bands ending in small uterine horns on the pelvic side walls are shown. Asterisk (*) indicates bilateral fibrotic bands; long arrow indicates endometriotic cyst (right ovary).
Abbreviations: RU, right fibrotic uterine horn; LU, left fibrotic uterine horn; RFT, right fallopian tube; LFT, right fallopian tube; LO, left ovary.
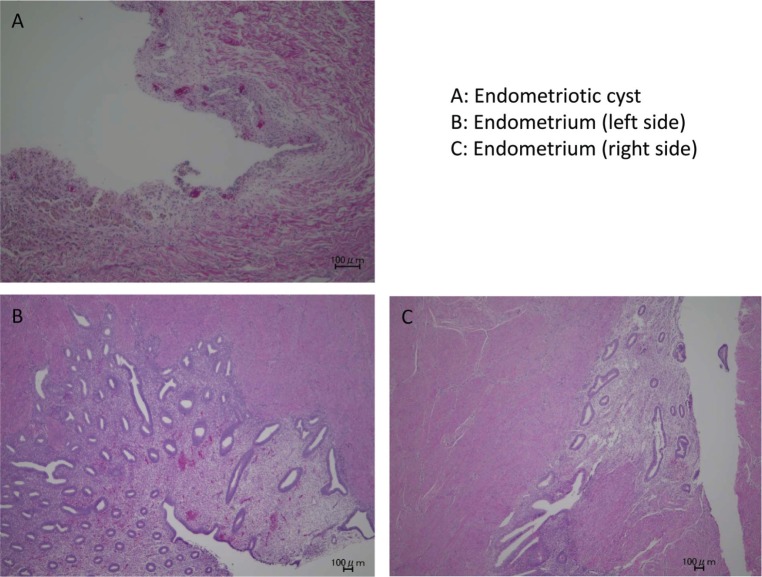
Figure 3.
Pathological analysis of the endometriotic lesion in the right ovary (A: hemosiderin deposit site, H&E, ×10) and endometrial tissues in bilateral uterine horns (B,C: H&E, ×10).
The uterine cervix did not exist. The pathological finding of the right ovarian cyst was that it was an endometriotic cyst. The postoperative recovery of the patient was uneventful. She was discharged on the 10th postoperative day. With continuous treatment with a dilator, the patient’s vagina showed no stenosis. Her pelvic pain resolved without further medical therapy. Three months after the surgery, sexual intercourse was allowed.
Discussion
Patients with MRKH syndrome have exhibited vaginal agenesis, streak Müllerian remnants, and normally developed ovaries and fallopian tubes. They usually complain primarily of amenorrhea without other symptoms; however, it is believed that pelvic pathology can be encountered in MRKH syndrome in patients who complain of chronic or cyclic pelvic pain.
In patients who have functional endometrium in Müllerian remnants, the accumulation of menstrual blood in the Müllerian structures or reverse flow to the pelvic cavity may allow a result in hematometra or endometriosis. In order to prevent morbidity, medical intervention should be performed to resolve the cyclic pelvic pain and distorted anomalies.4
The theory of the menstrual reflex is widely recognized and was first reported by Sampson.5 This theory proposes that the ectopic transplantation of endometrial tissue is brought about through menstrual flow. This phenomenon is commonly seen in women of reproductive age with endometriosis.
In our patient, MRI confirmed the absence of the vagina, cervix, and midline uterus. Moreover, a right endometrioma was identified with the presence of functional endometrium in the Müllerian remnants.
This case report supports Sampson’s theory of retrograde menstruation. On the other hand, a case of endometriosis in a patient with MRKH syndrome with a complete absence of the uterus, cervix, and vagina, which supports the theory of coelomic mataplasia, was also reported.6 Thus, the pathogenesis of endometriosis may be multifactorial, and a single theory may never be adequate to explain all cases of the disease. The presence of endometrium is very rare in MRKH syndrome. So, a curative approach was needed to improve the cyclic pain in this case.
A case was reported in which a Müllerian remnant was used to replace the uterus in a patient affected by MRKH syndrome, allowing the recovery of regular menstrual activity.7 In our patient, we created a neovagina; however, the uterine corpus was very small, so we could not replace the uterus and allow the recovery of regular menstruation, unfortunately.
In conclusion, we report a rare case of MRKH syndrome with functioning endometrium. Accurate evaluation before the operation and informed consent are necessary to treat Müllerian congenital anomalies such as MRKH syndrome. Further clinical follow-up and biological investigation are mandatory for a better understanding of this rare disease.
Footnotes
ACADEMIC EDITOR: Hiro Koshiyama, former Editor in Chief
FUNDING: Authors disclose no funding sources.
COMPETING INTERESTS: Authors disclose no potential conflicts of interest.
Paper subject to independent expert blind peer review by minimum of two reviewers. All editorial decisions made by independent academic editor. Prior to publication all authors have given signed confirmation of agreement to article publication and compliance with all applicable ethical and legal requirements, including the accuracy of author and contributor information, disclosure of competing interests and funding sources, compliance with ethical requirements relating to human and animal study participants, and compliance with any copyright requirements of third parties.
Author Contributions
Conceived and designed the experiments: YK. Analyzed the data: YK, TH, and MN. Wrote the first draft of the manuscript: YK. Contributed to the writing of the manuscript: KN and HN. Agree with manuscript results and conclusions: YK, TH, MN, AY, MY, KN, and HN. All authors reviewed and approved of the final manuscript.
REFERENCES
- 1.Fedele L, Bianchi S, Zanconato G, Raffaelli R. Laparoscopic creation of a neovagina in patients with Rokitansky syndrome: analysis of 52 cases. Fertil Steril. 2000;74:384–389. doi: 10.1016/s0015-0282(00)00620-8. [DOI] [PubMed] [Google Scholar]
- 2.Deligeoroglou E, Christopoulos P, Creatsas G. A unique case of descending salpingitis and functioning endometrium in a müllerian remnant in a woman with Mayer-Rokitansky-Küster-Hauser syndrome. Fertil Steril. 2005;83:1547.e5–e6. doi: 10.1016/j.fertnstert.2004.11.071. [DOI] [PubMed] [Google Scholar]
- 3.Giudice LC. Clinical practice. Endometriosis. N Engl J Med. 2010;362:2389–2398. doi: 10.1056/NEJMcp1000274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Elliott JE, Abduljabar H, Morris M. Presurgical management of dysmenorrhea and endometriosis in a patient with Mayer-Rokitansky-Kuster-Hauser syndrome. Fertil Steril. 2011;96:e86–e89. doi: 10.1016/j.fertnstert.2011.06.006. [DOI] [PubMed] [Google Scholar]
- 5.Sampson JA. Peritoneal endometriosis due to the menstrual dissemination of endometrial tissue into the peritoneal cavity. Am J Obstet Gynecol. 1927;14:422–469. [Google Scholar]
- 6.Mok-Lin EY, Wolfberg A, Hollinquist H, Laufer MR. Endometriosis in a patient with Mayer-Rokitansky-Kuster-Hauser syndrome and complete uterine agenesis: evidence to support the theory of coelomic metaplasia. J Pediatr Adolesc Gynecol. 2010;23:e35–e37. doi: 10.1016/j.jpag.2009.02.010. [DOI] [PubMed] [Google Scholar]
- 7.Fedele L, Bianchi S, Berlanda N, Bulfoni A, Fontana E. Laparoscopic creation of a neovagina and recovery of menstrual function in a patient with Rokitansky syndrome: a case report. Hum Reprod. 2006;21:3287–3289. doi: 10.1093/humrep/del315. [DOI] [PubMed] [Google Scholar]