Abstract
Objectives
To assess the HIV care continuum among HIV-infected persons residing in Seattle & King County, Washington at the end of 2011 and compare estimates of viral suppression derived from different population-based data sources.
Methods
We derived estimates for the HIV care continuum using a combination of HIV case and laboratory surveillance data supplemented with individual investigation of cases that appeared to be unlinked to or not retained in HIV care, a jurisdiction-wide population-based retrospective chart review, and local data from the CDC's Medical Monitoring Project and National HIV Behavioral Surveillance.
Results
Adjusting for in- and out-migration of persons diagnosed with HIV, laboratory surveillance data supplemented with individual case investigation suggest that 67% of persons diagnosed with HIV and 57% of all HIV-infected persons living in King County at the end of 2011 were virally suppressed (plasma HIV RNA <200 copies/mL). The viral suppression estimates we derived from a population-based chart review and adjusted local Medical Monitoring Project data were similar to the surveillance-derived estimate and identical to each other (59% viral suppression among all HIV-infected persons).
Conclusions
The level of viral suppression in King County is more than twice the national estimate and exceeds estimates of control for other major chronic diseases in the U.S. Our findings suggest that national care continuum estimates may be substantially too pessimistic, and highlight the need to improve HIV surveillance data.
Keywords: HIV Care Cascade, HIV Care Continuum, Public Health Surveillance, Linkage to Care, Retention in Care, Viral Suppression
Introduction
The concept of the HIV care continuum has galvanized the international HIV research agenda and transformed HIV prevention programs in recent years.1-3 In June, 2013, U.S. President Barack Obama issued an executive order to focus HIV prevention efforts on improving outcomes at each step in the continuum, launching the U.S. HIV Care Continuum Initiative.4 The continuum, or cascade, captures the sequential steps from HIV infection to viral suppression, including diagnosis, linkage to care, retention in care, and antiretroviral therapy (ART). Early national estimates of the proportion of persons living with HIV/AIDS (PLWHA) who had reached each step in the continuum painted a bleak picture, with just 19-28% having achieved viral suppression.5-8 More recently, Centers for Disease Control and Prevention (CDC) investigators estimated that 82% of all HIV-infected persons in the U.S. have been diagnosed,9 and surveillance data from 19 U.S. states suggest that 43% of HIV-diagnosed persons10 were virally suppressed in 2010 (i.e. 36% viral suppression among all HIV-infected persons). Although these recent data are more encouraging that earlier reports, they continue to portray an inadequate HIV prevention and care system in the U.S., with levels of viral suppression more than 40% lower than those observed in the U.K.11 and France.12
The estimates for each step in the HIV care continuum are inherently uncertain. This is due in large part to the need to derive estimates from a combination of disparate data sources, each with important limitations.13 Published reports that appear asynchronous or use different methodology add to this uncertainty. For example, the CDC estimates that approximately 80% of persons with newly diagnosed HIV link to care within 3 months,9, 10, 14 but an analysis of Medicaid data suggested that only 21% of Medicaid recipients link to HIV care within one year.15 A widely referenced report16 interprets data from Massachusetts as demonstrating higher viral suppression than the national average, but the 72% viral suppression estimate referenced in that report was among patients who responded to a survey given to them by HIV providers,17 which by definition excluded persons who were undiagnosed or out of care. Even when HIV continuum estimates are derived with uniform methodology, profound differences on the local level10, 14, 18 raise questions about the degree to which variation reflects true differences in the successful provision of care versus heterogeneity in data quality.
We used multiple population-based data sources, including core and supplemental HIV/AIDS surveillance, individual case investigation, jurisdiction-wide population-based chart reviews, and local data from the CDC Medical Monitoring Project (MMP) and National HIV Behavioral Surveillance (NHBS) to derive and validate estimates of the HIV care continuum in King County, WA. Our findings suggest that the actual level of viral suppression among PLWHA in at least one area of the U.S. substantially exceeds national estimates, is similar to that observed in Europe, and likely represents a level of treatment success greater than that observed for other major chronic diseases in the U.S.
Methods
We sought to estimate viral suppression and each preceding step in the HIV care continuum among PLWHA in King County, WA in 2011. King County includes the city of Seattle.
Data Sources
HIV Case and Laboratory Surveillance with Supplementary Case Investigation
Procedures for HIV surveillance in King County are described in detail elsewhere.18, 19 Briefly, WA State implemented requirements that laboratories report all CD4 count and plasma HIV RNA [viral load (VL)] results to the health department in 2006. In addition to standard surveillance procedures,20, 21 our public health program staff investigates all CD4 and VL results reports that cannot be linked to a previously reported HIV/AIDS case. This captures in-migration of persons diagnosed with HIV outside of King County. Since 2007, we have investigated all HIV cases with no CD4 or VL results reported to the health department for ≥12 months to ascertain which PLWHA continue to reside in King County and the HIV care engagement status of persons for whom laboratories have reported no results.19
Public Health – Seattle & King County (Public Health) routinely attempts to contact all persons with newly diagnosed HIV infection in order to facilitate linkage to care and to ensure testing of sex and needle sharing partners. Linkage to care is an explicit, recorded outcome of these investigations and outreach efforts with persons diagnosed with HIV are continued until patients link to care, refuse further contact with the health department or Public Health determines that further linkage efforts would be futile. Health department staff successfully contacted 79% of all persons reported as newly diagnosed with HIV in 2011. In 2011, we began routinely investigating all cases with no CD4 or VL results reported within 3 months after HIV diagnosis to distinguish persons who failed to link to HIV care from those who completed an HIV medical visit but had no laboratory results reported to surveillance or relocated.
Medical Monitoring Project (MMP)
Washington State is one of 23 areas that participate in MMP, which is designed to gather nationally representative data about persons receiving HIV care.20, 22, 23 In conjunction with HIV case and laboratory surveillance, MMP is the primary data source that CDC uses to estimate retention in HIV care, ART prescription, and viral suppression among PLWHA in the US.9 MMP methods include facility-based sampling of persons who received HIV care in the first four months of a calendar year. We used MMP data as one data source to estimate the proportions of persons with HIV infection who were in care, prescribed ART, and virally suppressed (Table 1).
Table 1. Description of Data Sources.
| Population-Based Chart Review | National HIV Behavioral Surveillance | Medical Monitoring Project | HIV Case Surveillance | HIV Laboratory Surveillance | |
|---|---|---|---|---|---|
| Population Sampled | Persons included in the HIV case surveillance database | Populations at high risk for HIV infection (persons with known HIV infection are included) | Persons in HIV medical care | Persons diagnosed with HIV currently residing in King County | Persons diagnosed with HIV currently residing in King County who had a CD4 or viral load test in a reporting laboratory in King County |
| Sampling Method and Frame | Randomly selected cases from all persons not identified through routine surveillance procedures to have died. | Three stage weighted, population-based sampling:
|
Not applicable – Surveillance includes all mandatory name-based case reports. We included in-migrant, excluded out-migrants, and excluded persons who died prior to the end of 2011. | Mandatory laboratory reporting of all CD4 and VL results and actively collected results from individual case investigations | |
| Calendar Years | 2010 | 2008, 2011 (MSM)2012 (IDU) | 2010 | 2011 | 2011 |
| Sample Size | 266 | VDTS-based: 2008 MSM2: 3682011 MSM3: 371RDS-based:2012 IDU3: 686 | 313 | Not applicable | 6094 |
| Response Rate | 85% c | Participation rates d:MSM - 2008: 27%MSM - 2011: 20% | 57% c | >99% e | Completeness of laboratory reporting unknown |
Men who have sex with men
Injection drug users
Completeness of chart reviews
Participation rates cannot be calculated for IDU cycles due to RDS methodology
Estimate derived from matching records 3674 of 3679 cumulative MMP eligible participants with case surveillance in 2013
National HIV Behavioral Surveillance (NHBS)
We used NHBS data to estimate the proportion of PLWHA who have been diagnosed. NHBS is a CDC-funded research study in 20 urban areas, including Seattle. NHBS data have been used to estimate the proportion of HIV-infected persons who are undiagnosed among populations at high risk for HIV infection.24 NHBS methods include HIV testing of study participants. 25 26
Population-Based Chart Review
In order to generate additional local estimates of the proportion of PLWHA who are in care, prescribed ART, and virally suppressed, we conducted a chart review of cases randomly selected from all HIV cases recorded in the electronic HIV/AIDS Reporting System (eHARS); this population included persons diagnosed with HIV outside of King County. We attempted to review the medical record of each selected case to ascertain dates of HIV medical visits and CD4 count and VL results. The sampling frame for this effort was designed to be more inclusive than the MMP sample. Table 1 provides details of the populations sampled, sampling methods, and completion rates for each data source.
Definition and Calculation of Continuum Steps
Table 2 describes the calculations and associated data sources that we used to estimate each step in the continuum. The metrics we used are consistent with those that CDC authors used to estimate the national HIV care continuum.9, 10, 14 Our definition of the number of HIV-diagnosed persons living in the jurisdiction includes persons who moved to King County after HIV diagnosis elsewhere (in-migrants) and excludes cases determined through case investigation to have moved away from King County (out-migrants), as described in detail previously.18,19
Table 2. HIV Care Continuum Metric Definitions and Associated Data Sources.
| Metric | Definition | Numerator | Data Sources |
|---|---|---|---|
| HIV infected | All persons with HIV infection | Not applicable a |
|
| HIV diagnosed | Persons aware of their HIV infection | Number of persons diagnosed with HIV (in or out of King County) who were residing in King County as of 12/31/2011 |
|
| Linked to care | Persons who completed an HIV medical visit within 90 days after HIV diagnosis | Number of persons who had a CD4 count or viral load test result reported to HIV surveillanceb OR had a confirmed care visit with an HIV medical provider ≤ 90 days after HIV diagnosis, among persons diagnosed in 2011 |
|
| In care | Persons who had ≥ 1 HIV medical visit in 2011 | Number of persons with ≥ 1 CD4 or VL report in 2011 |
|
| Retained in continuous care | Persons who had ≥2 CD4 or VL reports ≥ 90 days apart in 2011 | Number of persons with ≥2 CD4 or VL reports ≥ 90 days apart in 2011 |
|
| Prescribed ART | Persons with an active ART prescription | Number of persons prescribed ART at the time of the last HIV medical visit in 2011 |
|
| Virally suppressed | Persons with a viral load <200 copies/mL | Number of persons with a viral load of <200 copies/mL at last test in 2011 |
|
The estimated number of HIV infected persons served as the denominator for all steps in the HIV care continuum.
Excludes results from laboratory tests ordered by PHSKC staff as part of a program designed to increase linkage to care
As shown in Table 1 and Figure1, we estimated the total number of HIV-infected persons by adjusting the number of HIV-diagnosed persons to include an undiagnosed fraction. CDC recommends that local jurisdictional surveillance efforts begin the continuum with the number of HIV-diagnosed persons in the area, but we estimated the undiagnosed fraction both to facilitate comparison with national estimates and because it is essential to the population-based framework of the continuum. We estimated the undiagnosed fraction by applying estimates of the undiagnosed percentage in each subgroup defined by HIV transmission risk factor to the number of HIV-infected persons in each subgroup. For men who have sex with men (MSM), injection drug users (IDU), and MSM-IDU, we used Seattle NHBS data on the proportion of HIV-infected persons who were unaware of their infection. Because non-IDU heterosexuals account for a small minority of HIV-infected persons in King County and the local NHBS estimates for this group are unstable, we used national estimates by sex and race that CDC produced through a back-calculation method.27 For persons with unknown risk factor, we assumed a distribution among risk groups equal to that seen in the population with known risk factors and used national estimates for the undiagnosed fraction among persons with “other” risk factors by sex and race. Race and ethnicity are ascertained on the HIV case report or at the time of a partner services interview.
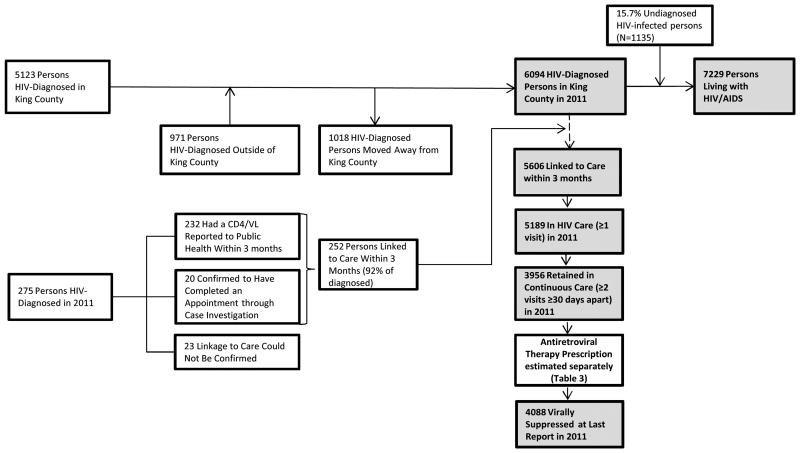
Figure 1.
HIV diagnosis, linkage to care, and retention in care in King County, 2011. Shaded boxes denote numbers used for HIV care continuum estimates shown in Table 3 and Figure 2.
We defined linkage to HIV care as a CD4 or VL test result reported to the health department or case investigation confirming a completed medical appointment ≤90 days after HIV diagnosis in 2011, excluding CD4 or VL test result ordered by Public Health at the time of HIV diagnosis. We defined retention in care using two definitions:14 “in care” denotes persons who had ≥1 CD4 or VL report in the calendar year, and “retained in continuous care” denotes the proportion with ≥2 CD4 or VL reports ≥90 days apart in a calendar year, the DHHS consensus metric for retention.28
We used two methods to calculate point estimates of ART use among all PLWHA. First, we defined the proportion of persons in the chart review sample who had an active prescription for ART as of the final medical visit in 2010. Second, we adjusted the proportion of persons prescribed ART in MMP by multiplying that proportion by the proportion of persons who were in-care in 2010. We did this to account for the MMP sampling frame, which is restricted to persons in care. To evaluate the robustness of our surveillance-derived point estimates, we separately calculated point estimates for care engagement and viral suppression using the population-based chart review and adjusted MMP data. Finally, we compared our estimates for each step to two national estimates from the CDC.9, 10 This analysis was exempt from Human Subjects review as a public health activity.
Results
HIV-Diagnosed
An estimated 6094 HIV-diagnosed persons were living in King County at the end of 2011. This population includes 971 (16%) persons who moved to King County after HIV diagnosis and excludes 1018 cases defined through case investigation as having left the area (Figure 1). The majority (89%) were male. Most persons were non-Hispanic White (64%), non-Hispanic Black (18%) or Hispanic (11%). The most common HIV transmission risk category was MSM (68%), followed by MSM-IDU (8%), heterosexual (11%) and IDU (5%). Including the estimated undiagnosed fraction of 15.7%, we estimated that 7,229 total HIV-infected persons were living in King County at the end of 2011.
Continuum Estimates Derived from Surveillance and Supplementary Case Investigation
Figure 1 shows the flow chart for derivation of continuum steps from surveillance data with supplemental case investigation. Of 275 persons newly diagnosed with HIV in 2011, 252 (92%) linked to care; 20 (8%) of these persons had no reported laboratory data in surveillance reflecting the linkage appointment that was confirmed by case investigation. Applying the 2011 linkage rate to the diagnosed population, we estimated that 5606 linked to care (78% of all HIV-infected persons). In 2011, 5189 persons were in HIV care, 3956 persons were retained in continuous care, and 4088 had viral suppression. Thus, 85% of HIV-diagnosed and 72% of HIV-infected persons were in care; 65% of HIV-diagnosed and 55% of HIV-infected persons were retained in continuous care; and 67% of HIV-diagnosed and 57% of HIV-infected persons were virally suppressed. Among suppressed persons, 3753 (92%) had VL <50 copies/mL.
Comparison of Estimates Derived from Different Data Sources
Table 3 shows multi-source estimates for all steps in the continuum after linkage to HIV care. The population-based chart review included 321 HIV cases; 55 were ineligible due to relocation (N=52) or death (N=3) prior to the end of 2010. Of 266 eligible cases, we completed medical records review for 227 (85%) cases. The remainder were incomplete because surveillance data did not include provider or facility data (N=13), the provider did not allow public health staff to access to medical records for review (N=16), or logistical difficulties prohibited surveillance staff from accessing records (N=10). CDC staff sampled 25 King County HIV medical care providers for MMP, of whom 13 (52%) agreed to participation, 10 (40%) were ineligible, and 2 (8%) refused. Of the 314 cases identified for MMP, chart reviews for 179 were completed (57%). Chart review and adjusted MMP data yielded similar estimates for retention in care and ART use, and both were slightly higher than surveillance-based estimates. However, estimates of viral suppression were similar from all three data sources: 59% from both chart review and adjusted MMP, and 57% from surveillance.
Table 3. Comparative Estimates of HIV Continuum Steps Derived from Different Data Sources.
| Population-Based Chart Review (N=227) | Unadjusted and AdjustedMedical Monitoring Project (N=179) | HIV Case & Laboratory Surveillance with Supplemental Case Investigation (N=6094) | |
|---|---|---|---|
| Reference population | HIV-diagnosed persons (N=6094) | Persons in HIV care (N=5189) | HIV-diagnosed persons (N=6094) |
| Percent of persons achieving each step of the continuum within reference population | |||
| In HIV care (%) | 89 | 100 | 85 |
| Retained in continuous care (%) | 79 | 94 | 65 |
| Taking ART (%) | 76 | 91 | NA |
| Viral suppression (%) | 70 | 82 | 67 |
| Number of persons achieving each step in the care continuum, with population standardized across data sources | |||
| Estimated number of persons in HIV care in reference population | 5424(0.89 × 6094) | 5189(1.00 × 5189) | 5189 |
| Estimated number of persons retained in continuous care in reference population | 4814(0.79 × 6094) | 4721(0.94 × 5189) | 3956 |
| Estimated number of persons on ART in reference population | 4631(0.76 × 6094) | 4721(0.91 × 5189) | NA |
| Estimated number of persons with viral suppression in reference population | 4266(0.70 × 6094) | 4255(0.82 × 5189) | 4088 |
| Size of total HIV-infected population, including undiagnosed fraction | 7229 | 7229 | 7229 |
| Percent of persons achieving each step in the care continuum, with population standardized across data sources | |||
| Estimated % in HIV care | 75 | NA | 72 |
| Estimated % retained in continuous care | 67 | 65 | 55 |
| Estimated % prescribed ART in total population | 64 | 65 | NA |
| Estimated % virally suppression in total population | 59 | 59 | 57 |
HIV Care Continuum in King County Compared to National Estimates
The estimates of the proportion of persons who reached each step in the HIV care continuum in King County in 2011 were higher than national estimates for 2009, which used MMP data, and for 2010, which used surveillance data from 19 jurisdictions (Figure 2).
Figure 2.
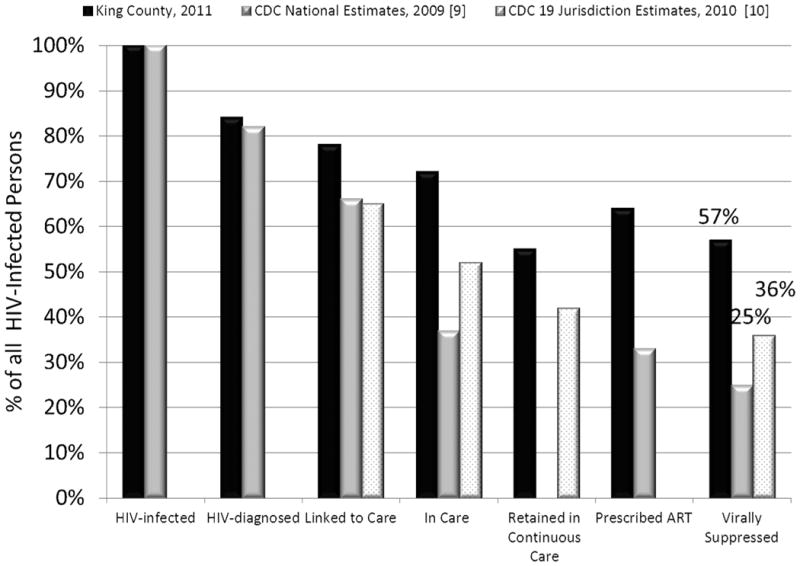
Comparison of the HIV care continuum in King County, 2011, and the United States, 2009 and 2010.
Discussion
We found that approximately 57% of all HIV-infected persons in King County, or 67% of HIV-diagnosed persons, were virally suppressed in 2011. The estimates we derived using different data sources yielded nearly identical results, suggesting that our findings are indeed accurate and our surveillance-derived estimates are valid. This estimate of population-level viral suppression is more than twice the U.S. national estimate, higher than estimates for British Columbia (35% of all HIV-infected persons),29 four other large U.S. cities (21-44% of HIV-infected persons),30 and all 19 jurisdictions included in a recent CDC report (14-56% of HIV-diagnosed persons).14 The level of viral suppression in King County is comparable to estimates from the U.K., France (53 and 52% of HIV-infected persons, respectively), and data from at least one U.S. state (61% of HIV-diagnosed persons in Minnesota).31 Although further improvements in the continuum are critical, our findings demonstrate that systems of HIV prevention and care in the U.S. are not universally failing. They also raise questions about the accuracy of existing national surveillance-based estimates of the HIV care continuum.
The marked difference between the level of viral suppression we observed compared to national estimates suggests a bifurcation either in the quality of HIV care, the quality of data used to estimate viral suppression in the U.S., or some combination of the two. Most estimates of the HIV care continuum based on laboratory surveillance data assume that missing data indicates non-retention in care. Failure to account for other causes of missing data, such as incomplete laboratory reporting, out-migration, and HIV care provision in settings exempt from reporting requirements (e.g. research settings) leads to misclassification of persons missing data and inflates the number of persons who appear to be out of care and viremic.18, 19, 32 Differences between local calculations and published national estimates of the same areas indicate that existing national estimates are likely too pessimistic and do not yet reflect rapid improvements in local surveillance data over the past few years. For example, the recent 19 jurisdiction CDC report indicated that 36% of HIV-diagnosed persons (N=2243) in Minnesota were virally suppressed in 2010, but Minnesota Department of Health reported that 61% (N=4394) were virally suppressed in 2012. The most recent update on the National HIV/AIDS Strategy from the Office of National AIDS Policy specifically noted that state and local level surveillance data can be used to augment national surveillance data for closer to ‘real-time’ monitoring of progress toward achieving the goals of the Strategy.33
Our results also suggest that virologic suppression probably is truly higher in King County than in some other parts of the U.S. Corroborating this, a previous study comparing engagement in HIV care in five U.S. states found that engagement was highest in Washington State34and in a recent eight-center study,35 viral suppression among patients at the largest HIV Clinic in Seattle was among the two highest. Washington State and King County devote substantial non-federal resources to HIV care and prevention and, although not all WA residents have health insurance, virtually all PLWHA in King County can access HIV medical care, including ART, as a result of funding through the Ryan White program and other sources. Our findings demonstrate that efforts to ensure that PLWHA have access to medical care and ART have, in at least some instances, been quite successful. They also highlight the fact that increased availability of health insurance under healthcare reform may not inevitably lead to further improvements in HIV care.
It is worth noting that our results suggest that current HIV treatment efforts in Seattle and surrounding areas have achieved a level of success higher than that observed for other treatable chronic health conditions in the U.S. Data from the U.S. National Health and Nutrition Survey (NHANES) suggest that, among adults age less than 65, 55% of persons diagnosed with diabetes mellitus, 47% of persons diagnosed with hypertension, and only 37% of persons diagnosed with elevated serum cholesterol have achieved the goals of clinical care.36, 37 In King County, an estimated 53% of persons with hypertension achieved blood pressure control in 2009 – a level higher than the national average, but still lower than our estimate of virologic control among PLWHA in King County.38 Indeed, the relative success of HIV care, at least in our area but likely also in others, could be a source of lessons for improving the treatment of other chronic diseases.
Our study has important strengths and limitations. Its primary strengths are that it was population-based (i.e., it was not restricted to a subset of PLWHA) and that we surmounted many of the limitations of using HIV surveillance data with individual case investigation, and validation with a population-based chart review and ancillary surveillance data sources. Nonetheless, substantial uncertainty still underlies some of our estimates, particularly the estimate of the undiagnosed fraction. Reliance on NHBS data could lead to overestimates of the undiagnosed fraction because NHBS methods rely on subjects to honestly disclose whether they have had a previous HIV diagnosis. Furthermore, our assumption that the distribution of HIV risk factors among the population with unknown risk factors was the same as that in the population with known risk factors could have affected our estimate of the undiagnosed fraction. Improved methods for estimating undiagnosed the undiagnosed fraction are critical for generating accurate estimates of the HIV care continuum at the local level. Recent results from a mathematical model of the undiagnosed fraction of HIV in MSM in King County39 suggest that we have overestimated the undiagnosed fraction in this analysis, meaning that we have underestimated the true proportion of PLWHA who are virally suppressed and preceding steps in the continuum. Similarly, our surveillance team's criteria for defining a case as having out-migrated is conservative and may have led to underestimation of retention in care and viral suppression.
In summary, we found that the majority of HIV-infected persons in King County have achieved viral suppression and our surveillance-based estimates of viral suppression are valid. Our findings demonstrate that the U.S. medical and public health system is not universally failing persons with HIV, suggest that national estimates of the HIV care continuum may be substantially too pessimistic and highlight the need to improve HIV surveillance data at the local, state and national level.
Acknowledgments
The authors appreciate the contributions of Michelle Perry, Lexa Moongrace, Allison Moore, Mark Fleming, Winnie Alston, and Cheryl Malinski for case investigation and chart abstractions; and James Kent, Elizabeth Barash and Julia Hood for data provision.
This work was supported by a grant to JCD from the National Institute of Mental Health (5K23MH090923); the University of Washington Center for AIDS Research (CFAR), an NIH funded program under award number P30AI027757 which is supported by the following NIH Institutes and Centers (NIAID, NCI, NIMH, NIDA, NICHD, NHLBI, NIA, NIGMS, NIDDK); and programmatic funding from the CDC, the Washington State Department of Health, and Public Health – Seattle and King County.
Footnotes
Note: This work was presented in part at the 20th Conference on Retroviruses and Opportunistic Infections (Abstract 1027)
Conflicts of Interest: JCD and MRG have received research support for STD studies unrelated to this work from Cempra pharmaceuticals and Genentech. All other authors had no potential conflicts of interest.
References
- 1.Kilmarx PH, Mermin J. Prevention with people with HIV in the United States: the nexus of HIV prevention and treatment. J Acquir Immune Defic Syndr. 2012;60(3):219–220. doi: 10.1097/QAI.0b013e3182531ba2. [DOI] [PubMed] [Google Scholar]
- 2.Fauci AS, Folkers GK, Dieffenbach CW. HIV-AIDS: much accomplished, much to do. Nat Immunol. 2013;14(11):1104–1107. doi: 10.1038/ni.2735. [DOI] [PubMed] [Google Scholar]
- 3.Mugavero MJ, Amico KR, Horn T, Thompson MA. The state of engagement in HIV care in the United States: from cascade to continuum to control. Clin Infect Dis. 2013;57(8):1164–1171. doi: 10.1093/cid/cit420. [DOI] [PubMed] [Google Scholar]
- 4.The White House. [Accessed October 28 2013];Executive Order -- HIV Care Continuum Initiative. http://www.whitehouse.gov/the-press-office/2013/07/15/executive-order-hiv-care-continuum-initiative.
- 5.Gardner EM, McLees MP, Steiner JF, Del Rio C, Burman WJ. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis. 2011;52(6):793–800. doi: 10.1093/cid/ciq243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marks G, Gardner LI, Craw J, Giordano TP, et al. The spectrum of engagement in HIV care: do more than 19% of HIV-infected persons in the US have undetectable viral load? Clin Infect Dis. 2011;53(11):1168–1169. doi: 10.1093/cid/cir678. [DOI] [PubMed] [Google Scholar]
- 7.Burns DN, Dieffenbach CW, Vermund SH. Rethinking prevention of HIV type 1 infection. Clin Infect Dis. 2010;51(6):725–731. doi: 10.1086/655889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Disease Prevention and Control. Vital signs: HIV prevention through care and treatment--United States. MMWR Morb Mortal Wkly Rep. 2011;60(47):1618–1623. [PubMed] [Google Scholar]
- 9.Hall HI, Frazier EL, Rhodes P, et al. Differences in human immunodeficiency virus care and treatment among subpopulations in the United States. JAMA Intern Med. 2013;173(14):1337–1344. doi: 10.1001/jamainternmed.2013.6841. [DOI] [PubMed] [Google Scholar]
- 10.Centers for Disease Prevention and Control. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data - United States and 6 dependent areas - 2011. [Accessed October 31 2013];HIV Surveillance Supplemental Report. 2013 18 http://www.cdc.gov/hiv/library/reports/surveillance/ [Google Scholar]
- 11.Delpech V. TasP PrEP Evidence Summit. London, UK: 2013. Health system concerns related to TasP and most at risk populations. [Google Scholar]
- 12.Supervie V, Costagliola D. 20th Conference on Retroviruses and Opportunistic Infections. Atlanta, GA: 2013. The spectrum of engagement in HIV care in France: strengths and gaps. [Google Scholar]
- 13.Institute of Medicine Monitoring HIV Care in the United States: Indicators and Data Systems. Washington, D.C.: The National Academies Press; 2012. [PubMed] [Google Scholar]
- 14.Gray KM, Cohen SM, Hu X, Li J, Mermin J, Hall HI. Jurisdiction level differences in HIV diagnosis, retention in care, and viral suppression in the United States. J Acquir Immune Defic Syndr. doi: 10.1097/QAI.0000000000000028. published online ahead of print, October 10 2013. [DOI] [PubMed] [Google Scholar]
- 15.Johnston SS, Juday T, Seekins D, et al. Patterns and correlates of linkage to appropriate HIV care after HIV diagnosis in the US Medicaid population. Sex Transm Dis. 2012;40(1):18–25. doi: 10.1097/OLQ.0b013e3182782014. [DOI] [PubMed] [Google Scholar]
- 16.Center for Health Law and Policy Innovation of Harvard Law School. Massachusetts case study: health reforms lead to improved individual and public health outcomes and cost savings. [Accessed October 31 2013]; http://www.law.harvard.edu/academics/clinical/lsc/documents/FACT_SHEET_%20MA_Case_Study_on_Health_Reforms6-27-12.pdf.
- 17.Holman J, Schneider K, Watson K, Mathur J, Flynn A. Massachusetts and Southern New Hampshire HIV/AIDS Consumer Study. JSI Research and Training Institute; 2011. [Google Scholar]
- 18.Dombrowski JC, Kent JB, Buskin SE, Stekler JD, Golden MR. Population-based metrics for the timing of HIV diagnosis, engagement in HIV care, and virologic suppression. AIDS. 2012;26(1):77–86. doi: 10.1097/QAD.0b013e32834dcee9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Buskin S, Kent JB, Dombrowski JC, Golden MR. Migration distorts surveillance estimates of engagement in care: results of public health investigations of persons who appear to be out of HIV care. Sex Transm Dis. 2014;41:35–40. doi: 10.1097/OLQ.0000000000000072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention. Surveillance Brief: Surveillance Systems Supported by the Division of HIV/AIDS Prevention. [Accessed April 14 2011]; http://www.cdc.gov/hiv/topics/surveillance/resources/factsheets/surveillance.htm.
- 21.Centers for Disease Control and Prevention. Technical Guidance for HIV/AIDS Surveillance Programs. [Accessed November 27 2013]; http://www.cdph.ca.gov/programs/aids/Documents/SOPCDCSurvTechGuidanceVol1.pdf.
- 22.Blair JM, McNaghten AD, Frazier EL, Skarbinski J, Huang P, Heffelfinger JD. Clinical and behavioral characteristics of adults receiving medical care for HIV infection --- Medical Monitoring Project, United States, 2007. MMWR Morb Mortal Wkly Rep. 2011;60(11):1–20. [PubMed] [Google Scholar]
- 23.Frankel MR, McNaghten A, Shapiro MF, et al. A probability sample for monitoring the HIV-infected population in care in the U.S. and in selected states. Open AIDS J. 2012;6:67–76. doi: 10.2174/1874613601206010067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention. Prevalence and awareness of HIV infection among men who have sex with men --- 21 cities, United States, 2008. MMWR Morb Mortal Wkly Rep. 2010;59(37):1201–1207. [PubMed] [Google Scholar]
- 25.MacKellar DA, Gallagher KM, Finlayson T, Sanchez T, Lansky A, Sullivan PS. Surveillance of HIV risk and prevention behaviors of men who have sex with men--a national application of venue-based, time-space sampling. Public Health Rep. 2007;122(Suppl 1):39–47. doi: 10.1177/00333549071220S107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gallagher KM, Sullivan PS, Lansky A, Onorato IM. Behavioral surveillance among people at risk for HIV infection in the U.S.: the National HIV Behavioral Surveillance System. Public Health Rep. 2007;122(Suppl 1):32–38. doi: 10.1177/00333549071220S106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chen M, Rhodes PH, Hall IH, Kilmarx PH, Branson BM, Valleroy LA. Prevalence of undiagnosed HIV infection among persons aged >/=13 years--National HIV Surveillance System, United States, 2005-2008. MMWR Morb Mortal Wkly Rep. Jun 15;61(Suppl):57–64. [PubMed] [Google Scholar]
- 28.Valdiserri RO, Forsyth AD, Yakovchenko V, Koh HK. Measuring what matters: development of standard HIV core indicators across the U.S. Department of Health and Human Services. Public Health Rep. 2013;128(5):354–359. doi: 10.1177/003335491312800504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nosyk B, Montaner JS, Colley G, et al. The cascade of HIV care in British Columbia, Canada, 1996-2011: a population-based retrospective cohort study. Lancet Infect Dis. doi: 10.1016/S1473-3099(13)70254-8. published online ahead of print September 26, 2013. doi:S1473-3099(13)70254-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Benbow N, Scheer S, Wohl AR, et al. Linkage, retention, ART use and viral suppression in four large cities in the United States XIX International AIDS Conference; Washington, D.C.. 2012. [Google Scholar]
- 31.Minnesota Department of Health. Minnesota's HIV Treatment Cascade. [Accessed February 7 2014];2013 Available at: http://www.health.state.mn.us/divs/idepc/diseases/hiv/hivtreatmentcascade.html.
- 32.Rowan S, Johnson S, Thrun M, Daniloff E, Reirden D, Burman W. Patient migration significantly impacts estimates of engagement inHIV care and attainment of viral suppression. XIX International AIDS Conference; Washington, D.C.. 2012. [Google Scholar]
- 33.The White House Office of National AIDS Policy. National HIV/AIDS Strategy: Improving outcomes: accelerating progress along the HIV care continuum. [Accessed February 10 2014];2013 Available at: http://www.whitehouse.gov/sites/default/files/onap_nhas_improving_outcomes_dec_2013.pdf.
- 34.Bertolli J, Shouse RL, Beer L, et al. Using HIV surveillance data to monitor missed opportunities for linkage and engagement in HIV medical care. Open AIDS J. 2012;6:131–141. doi: 10.2174/1874613601206010131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dombrowski JC, Kitahata MM, Van Rompaey SE, et al. High Levels of Antiretroviral Use and Viral Suppression among Persons in HIV Care in the United States, 2010. J Acquir Immune Defic Syndr. doi: 10.1097/QAI.0b013e3182945bc7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wilper AP, Woolhandler S, Lasser KE, McCormick D, Bor DH, Himmelstein DU. Hypertension, diabetes, and elevated cholesterol among insured and uninsured U.S. adults. Health Aff (Millwood) 2009;28(6):w1151–1159. doi: 10.1377/hlthaff.28.6.w1151. [DOI] [PubMed] [Google Scholar]
- 37.Yoon PW, Gillespie CD, George MG, Wall HK. Control of hypertension among adults--National Health and Nutrition Examination Survey, United States, 2005-2008. MMWR Morb Mortal Wkly Rep. 2012 Jun 15;61(Suppl):19–25. [PubMed] [Google Scholar]
- 38.Olives C, Myerson R, Mokdad AH, Murray CJ, Lim SS. Prevalence, awareness, treatment, and control of hypertension in United States counties, 2001-2009. PLoS One. 2013;8:e60308. doi: 10.1371/journal.pone.0060308. Companion Institute for Health Metrics and Evaluation Data Visualization Tool available at: http://vizhub.healthdata.org/us-health-map/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fellows I, Morris M, Dombrowski JC, et al. A new HIV testing history-based approach for estimating the undiagnosed fraction of persons with HIV infection: findings suggest that few HIV-infected men who have sex with men in King County, WA, U.S.A. are undiagnosed. Under Review. [Google Scholar]