Abstract
Objective
It is imperative to study the clinical course of anxiety disorders among Latinos, given the implications for culturally-sensitive treatment in this population. The current study is the first prospective, observational, longitudinal study of anxiety disorders among Latinos.
Method
Data are reported on 139 adult Latinos (mean age 34.65, SD =10.98, 70.5% female) diagnosed with social anxiety disorder (SAD, n = 86), generalized anxiety disorder (GAD, n = 90) or panic disorder with agoraphobia (PDA, n = 62). The participants were interviewed with standardized clinical interviews at intake and annually over two years of follow-up. Probabilities of recovery were calculated using standard survival analysis methods.
Results
The two-year recovery rates in this study were 0.07 for SAD, 0.14 for GAD, 0.03 for PDA, and 0.50 for major depressive disorder (MDD). Overall functioning, social adjustment and life satisfaction in this sample were poor.
Conclusions
The recovery rates for anxiety disorders in this Latino sample were markedly low. Although caution must be used in comparing these data with prior longitudinal studies, these recovery rates seem to be much lower than in non-Latino White samples. However, the clinical course of MDD in this sample was similar to its course among non-Latino Whites, invoking the pressing question of whether there is something about the experience of anxiety disorders (but not MDD) among Latinos that makes them more impairing and persistent. The answer to that question should inform future treatment development for this population.
Keywords: anxiety disorders, longitudinal course, Latinos, recovery, social phobia, social anxiety disorder, generalized anxiety disorder, panic disorder, agoraphobia
Little is known about the clinical course of anxiety disorders among Latinos. In the only attempt to estimate the development of these disorders over time, Breslau et al. (2005) found that mood disorders, but not anxiety disorders, were more persistent in Latinos compared to Whites. However, that finding was based on a one-time assessment in which participants were asked to retrospectively report duration of illness. The Harvard/Brown Anxiety Research Project (HARP) was the first prospective, observational longitudinal study of anxiety disorders with the index disorders of generalized anxiety disorder (GAD), panic disorder with and without agoraphobia (PD/PDA) and social anxiety disorder (SAD). Prior to HARP, most longitudinal studies had either brief follow-up periods or long intervals between assessments, and they were often characterized by lack of systematic recovery and recurrence definitions. HARP extended previous studies by assessing clinical course with structured interviews, at relatively short intervals (12 months between assessments) for every week of the follow-up period (by using a change point method to anchor participant reports of symptom levels to relevant life events such as birthdays and holidays), with careful definitions of recovery and recurrence. Recovery was defined as having minimal or no symptoms for eight consecutive weeks, and recurrence was defined as meeting diagnostic criteria for at least two consecutive weeks following recovery (Bruce et al., 2005). The probability of recovery over a period of 2 years was 0.20 for SAD, 0.25 for GAD, and 0.23 for PDA (Bruce et al., 2005). In the Primary Care Anxiety Project (PCAP), a longitudinal study of anxiety disorders in primary care patients, which was modeled on HARP-I methodology, there was a 0.31 probability of recovery for SAD, a 0.39 probability of recovery from GAD, and a 0.16 probability of recovery for PDA over a period of two years (Beard, Moitra, Weisberg, & Keller, 2010; Francis et al., 2007; Rodriquez et al., 2006).
In summary, anxiety disorders are chronic. However, there was almost no minority representation in HARP (97% were white; Bruce et al., 2005) and PCAP (88% were White; Francis et al., 2007). It is imperative to study the experience of anxiety in Latino samples, since cultural variables such as acculturative stress (Hovey & Magaña, 2002), perceived discrimination (Flores, Tschann, Dimas, Pasch, & de Groat, 2010) and immigration status (Familiar, Borges, Orozco, & Medina-Mora, 2011) may contribute to worsening the course of illness in Latinos. The current report is the first prospective study of the clinical course of anxiety disorders among Latinos. Data are obtained from the second wave of the Harvard/Brown Anxiety Project (HARP-II) (Weisberg, Beard, Dyck, & Keller, 2012). HARP-II was designed to address the glaring lack of research available on minority populations. In the current study we report on demographic and clinical characteristics of a large sample of Latino individuals with anxiety disorders, and on the course of PDA, SAD, GAD and major depressive disorder (MDD; in order to evaluate whether mood disorders are more persistent than anxiety disorders among Latinos) in this population, and examine potential predictors of course.
Method
Data were obtained from a subset of HARP-II comprising Latino participants diagnosed with DSM-IV anxiety disorders (American Psychiatric Association, 2000).1 Participants were recruited from referrals from site collaborators and affiliated treatment providers, or were self-referred from postings in newspapers and on the Internet. The institutional review board of Brown University approved HARP-II, and participants provided written informed consent prior to enrollment in the study.
Participants and Procedure
Participants were 139 Latinos (age 18 or older) enrolled in HARP–II. Inclusion criteria for this study included being diagnosed with one or more of the following anxiety disorders, as assessed by the Structured Clinical Interview for DSM-IV (SCID-IV; First, Spitzer, Gibbon, & Williams, 1996): SAD, PD, PDA and GAD. Furthermore, participants needed to be at least 18 years of age and English speaking. Participants were excluded from the study if they were diagnosed with schizophrenia, suffering from active psychosis, or had an organic mental disorder, in order to increase the likelihood that participants would be able to complete the study interviews. Participants completed in-person assessments at baseline and in-person or telephone follow-up interviews at 6 months, 1 year, and 2 years post-intake, using the Longitudinal Interval Follow-Up Evaluation (LIFE; Keller et al., 1987). The current study presents data from 139 Latinos: 90 diagnosed with GAD, 86 with SAD, and 62 with PDA.
Measures
Structured Clinical Interview for DSM-IV Axis-I Disorders (SCID-IV; First et al., 1996)
The SCID is a semi-structured, clinician administered diagnostic interview employed at intake to assess current and lifetime history of Axis-I disorders. The interrater reliability of the SCID has been found to be excellent (Cohen’s kappa = .85) with very good diagnostic accuracy (Ventura, Liberman, Green, Shaner, & Mintz, 1998). The SCID has been evaluated in a Latino sample, with acceptable concordance rates with other diagnostic interviews (Alegria et al., 2009).
Longitudinal Interval Follow-Up Evaluation (LIFE; Keller et al., 1987)
The LIFE is an interviewer-administered assessment that collects detailed information on anxiety disorder symptoms during the follow-up period, psychosocial functioning, and treatment status, and is used at follow-up interviews to assess disorder course. The LIFE uses a 6-point psychiatric status rating (PSR) scale to indicate the severity of psychiatric symptoms, in which PSR of 1 indicates that the patient is asymptomatic, a PSR of 2 indicates that the patient has some mild symptoms, a PSR of 3 or 4 indicates that the participant does not meet full DSM-IV criteria for the disorder but still exhibits notable symptoms and impairment to a mild or moderate degree, respectively. A PSR of 5 or 6 indicates that the patient meets full DSM-IV criteria for the disorder with either moderate or severe functional impairment, respectively. The LIFE employs a change point method to anchor participant reports of symptom levels to relevant life events such as holidays and birthdays, resulting in weekly ratings of psychiatric symptom severity. Recovery in the present study was defined as at least a period of eight consecutive weeks at a PSR of 1 or 2. Recurrence was defined as meeting diagnostic criteria (PSR of 5 or 6) for at least two consecutive weeks (for GAD, for 6 consecutive months) following recovery. Interrater reliability and long-term test-retest reliability for the LIFE PSR ratings have been found to be good to excellent for all anxiety disorders and MDD (Warshaw, Keller, & Stout, 1994) in HARP-I. Interrater agreement on PSR values in HARP-II was found to be 65% for PD, 88% for GAD, 97% for SAD and 87% for MDD. The LIFE is also used to collect monthly information on functioning in a variety of areas including life satisfaction, global social adjustment, and global assessment of functioning (GAF), with good interrater reliability for these items with intraclass correlation coefficients ranging from .59 to .91 (Keller et al., 1987).
Demographics Questionnaire
This measure is used to obtain information on the participant’s self-reported race and ethnicity and variables such as age and employment.
Treatment History Questionnaire
This measure is used to assess participants’ psychiatric treatment history, including frequency and type of treatments received, and shows high interrater reliability (Keller et al., 1987). Reliability coefficients ranged from .91 to 1.00 for all treatment modalities except atypical antidepressants, which had kappas in the .66 to .86 range.
Rater Training and Supervision
Interviews were conducted by clinical interviewers with a bachelor’s or master’s degree in psychology or a related field. Interviewers complete a rigorous training program, which begins with studying instruments and watching training tapes. Interviewers then participate in a 1-2 day didactic session and review videotapes of interviews conducted by experienced interviewers. New interviewers then directly observe experienced interviewers and are themselves later directly observed by training supervisors. These interviews are also audio or video-recorded, for close review by training supervisors. Only after conducting at least three observed interviews, and being judged by training supervisors as competent, are new interviewers certified to collect data independently. After certification, all clinical interviewers remain closely supervised. HARP-II clinical staff review each diagnosis for each case enrolled in the study at a weekly meeting. The training supervisor monitors the ratings from each interviewer and provides feedback from periodic audio or video recordings.
Statistical Analyses
Data were analyzed using SPSS Version 16.0. Means, standard deviations, and frequencies were calculated. Standard survival analysis techniques and Kaplan-Meier life tables were used. Statistical comparisons of survival rates were conducted for each disorder examining the potential role of employment, education, income, receiving treatment at intake, being born in the U.S., and first language. Data for participants who were lost to follow-up were censored.
Results
Demographic Characteristics
Information on country of origin for the sample is presented in Table 1. The age range of the sample was 18-63 years (M = 34.65, SD = 10.98; see Table 2), with the majority female (70.5%) and about half single (52.5%). This was a relatively educated sample with most participants reporting at least some college education (63.3%). However, over half of them were unemployed (51.3%) and income in this sample was extremely low with 49.6% reporting an annual income of less than $20,000.
Table 1.
Country of Origin and Nativity Status of the Latino Sample at Intake
| Variable | Total Sample (N = 139) | Participants with SAD (N=86) | Participants with GAD (N=90) | Participants with PDA (N=62) | ||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| N | % | N | % | N | % | N | % | |
| Country of Origin | ||||||||
| United States | 72 | 51.8 | 43 | 50.0 | 44 | 48.9 | 34 | 54.8 |
| Puerto Rico | 30 | 21.6 | 19 | 22.1 | 15 | 16.7 | 15 | 24.2 |
| Mexico | 2 | 1.4 | 1 | 1.2 | 1 | 1.1 | 0 | 0 |
| Colombia | 2 | 1.4 | 2 | 2.3 | 2 | 2.2 | 0 | 0 |
| El Salvador | 1 | 0.7 | 1 | 1.2 | 1 | 1.1 | 0 | 0 |
| Guatemala | 3 | 2.2 | 1 | 1.2 | 3 | 3.3 | 2 | 3.2 |
| Dominican Republic | 8 | 5.8 | 8 | 9.3 | 6 | 6.7 | 3 | 4.8 |
| Cuba | 1 | 0.7 | 1 | 1.2 | 0 | 0 | 0 | 0 |
| Azores | 1 | 0.7 | 1 | 1.2 | 1 | 1.1 | 0 | 0 |
| Costa Rica | 2 | 1.4 | 0 | 0 | 2 | 2.2 | 1 | 1.6 |
| Ecuador | 3 | 2.2 | 1 | 1.2 | 2 | 2.2 | 2 | 3.2 |
| Honduras | 2 | 1.4 | 1 | 1.2 | 2 | 2.2 | 1 | 1.6 |
| Brazil | 4 | 2.9 | 2 | 2.3 | 4 | 4.4 | 1 | 1.6 |
| Peru | 1 | 0.7 | 1 | 1.2 | 1 | 1.1 | 1 | 1.6 |
| Canada | 1 | 0.7 | 1 | 1.2 | 1 | 1.1 | 0 | 0 |
| Argentina | 1 | 0.7 | 0 | 0 | 1 | 1.1 | 0 | 0 |
| Panama | 1 | 0.7 | 1 | 1.2 | 1 | 1.1 | 1 | 1.6 |
| Bolivia | 2 | 1.4 | 1 | 1.2 | 2 | 2.2 | 0 | 0 |
| Uruguay | 1 | 0.7 | 0 | 0 | 0 | 0 | 1 | 1.6 |
| Germany | 1 | 0.7 | 1 | 1.2 | 1 | 1.1 | 0 | 0 |
| Age Moved to USA | ||||||||
| Whole Sample (n = 67) | 14.14 (M) | 11.31 (SD) | ||||||
| SAD (n = 43) | 13.77 (M) | 11.93 (SD) | ||||||
| GAD (n = 46) | 14.76 (M) | 10.25 (SD) | ||||||
| PDA (n = 28) | 14.43 (M) | 11.88 (SD) | ||||||
Notes: M = Mean, SD = Standard Deviation, The number of participants who were born outside the US is shown in parentheses for the variable “Age Moved to USA”.
Table 2.
Demographic Characteristics of the Latino Sample at Intake
| Variable | Total Sample (N = 139) |
Participants with SAD (N=86) |
Participants with GAD (N=90) |
Participants with PDA (N=62) |
||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| N | % | N | % | N | % | N | % | |
| Age | 34.65 (M) | 10.98 (SD) | 32.93 (M) | 10.98 (SD) | 34.40 (M) | 11.12 (SD) | 36.89 (M) | 11.93 (SD) |
| Female | 98 | 70.5 | 56 | 65.1 | 66 | 73.3 | 45 | 72.6 |
| Marital Status | ||||||||
| Single | 73 | 52.5 | 44 | 51.2 | 48 | 53.3 | 33 | 53.2 |
| Married | 20 | 14.4 | 13 | 15.1 | 12 | 13.3 | 7 | 11.3 |
| Widowed/Separated/Divorced | 45 | 32.4 | 29 | 33.7 | 30 | 33.3 | 21 | 33.9 |
| Education (highest completed) | ||||||||
| High School or Less | 51 | 36.7 | 33 | 38.4 | 25 | 27.8 | 26 | 41.9 |
| At Least Some College | 88 | 63.3 | 53 | 61.6 | 65 | 72.2 | 36 | 58.1 |
| Economic Support | ||||||||
| Income from Job | 67 | 48.2 | 43 | 50.0 | 52 | 57.8 | 24 | 38.7 |
| Spouse | 15 | 10.8 | 8 | 9.3 | 10 | 11.1 | 8 | 12.9 |
| Partner | 16 | 11.5 | 12 | 14.0 | 10 | 11.1 | 5 | 8.1 |
| Family | 34 | 24.5 | 22 | 25.6 | 26 | 28.9 | 16 | 25.8 |
| Welfare | 35 | 25.2 | 16 | 18.6 | 19 | 21.1 | 14 | 22.6 |
| Pension/Social Security | 3 | 2.2 | 3 | 3.5 | 2 | 2.2 | 1 | 1.6 |
| Physical Disability | 17 | 12.2 | 8 | 9.3 | 10 | 11.1 | 9 | 14.5 |
| Psychiatric Disability | 30 | 21.6 | 19 | 22.1 | 14 | 15.6 | 21 | 33.9 |
| Physical AND Psych | 11 | 7.9 | 6 | 7.0 | 7 | 7.8 | 6 | 9.7 |
| Physical OR Psych | 36 | 25.9 | 21 | 24.4 | 17 | 18.9 | 24 | 38.7 |
| Employment | ||||||||
| Employed | 67 | 48.2 | 43 | 50.0 | 52 | 57.8 | 24 | 38.7 |
| Unemployed | 72 | 51.3 | 43 | 50.0 | 38 | 42.2 | 38 | 61.3 |
| Annual Income | ||||||||
| <$19,999/yr | 70 | 49.6 | 46 | 53.5 | 37 | 41.1 | 41 | 56.9 |
| $20,000 – 34,999 | 35 | 24.8 | 19 | 22.1 | 24 | 26.7 | 19 | 26.4 |
| $35,000 – 49,999 | 14 | 9.9 | 6 | 7.0 | 11 | 12.2 | 4 | 5.6 |
| $50,000 – 64,999 | 13 | 9.2 | 9 | 10.5 | 12 | 13.3 | 5 | 6.9 |
| $65,000 – 89,999 | 3 | 2.1 | 2 | 2.3 | 3 | 3.3 | 1 | 1.4 |
| $90,000 – 119,999 | 2 | 1.4 | 1 | 1.2 | 1 | 1.1 | 0 | 0.0 |
| $120,000 - $150,000 | 1 | 0.7 | 1 | 1.2 | 0 | 0.0 | 0 | 0.0 |
Notes: M = Mean, SD = Standard Deviation, Some numbers do not total to 100% due to missing data and some total to >100% due to endorsing more than 1.
Clinical Characteristics
Mean age of onset was 12.92 (SD = 5.51) for SAD, 20.52 (SD = 9.77) for GAD and 24.63 (SD = 12.23) for PDA (see Table 3). A high percentage of participants reported a history of trauma (41.7%). Comorbidity was high in this sample (mean number of current Axis-I disorders was 3.47, SD = 1.67), especially with anxiety and mood disorders. Overall functioning of this sample was low, with a mean GAF score of 52.09 (SD = 6.86) and overall social adjustment (mean GSA score of 3.87, SD = 0.84 on a scale of 1-5) and life satisfaction (M = 3.15, SD = 0.69, on a scale of 1-5) were poor. History of suicide attempts and suicidal gestures in this sample was alarmingly high (38.1%). Only 46% of the sample was undergoing individual therapy, and 53.2% were taking medications at the time of intake.
Table 3.
Clinical Characteristics of the Latino Sample at Intake
| Variable | Total Sample (N =139) | Participants with SAD (N=86) | Participants with GAD (N=90) | Participants with PDA (N=62) | ||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| N | % | N | % | N | % | N | % | |
| Age of Onset | - | - | 12.92 (M) | 5.51 (SD) | 20.52 (M) | 9.77 (SD) | 24.63 (M) | 12.23 (SD) |
| Duration (years) | - | - | 21.00 (M) | 12.96 (SD) | 13.88 (M) | 11.31 (SD) | 12.26 (M) | 12.55 (SD) |
| Severity of Current Episode | - | - | ||||||
| Mild | - | - | 33 | 38.4 | 28 | 31.1 | 20 | 32.3 |
| Moderate | - | - | 41 | 47.7 | 55 | 61.1 | 34 | 54.8 |
| Severe | - | - | 12 | 14.0 | 7 | 7.8 | 8 | 12.9 |
| Duration of first Episode Remains Current | - | - | 84 | 97.7 | 84 | 93.3 | 58 | 93.5 |
| Trauma History | 58 | 41.7 | 32 | 37.2 | 34 | 37.8 | 31 | 50.0 |
| Global Assessment of Functioning (GAF) at Intake | 52.09 | (6.86) | 51.85 | (6.86) | 52.67 | (6.82) | 49.87 | (6.89) |
| Global Social Adjustment (GSA) (1-5) | 3.67 | (0.84) | 3.68 | (0.86) | 3.62 | (0.84) | 3.87 | (0.80) |
| Very Good | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 |
| Good | 10 | 7.2 | 7 | 8.1 | 8 | 8.9 | 2 | 3.2 |
| Fair | 48 | 34.5 | 28 | 32.6 | 31 | 34.4 | 18 | 29.0 |
| Poor | 57 | 41.0 | 35 | 40.7 | 38 | 42.2 | 28 | 45.2 |
| Very Poor | 23 | 16.5 | 15 | 17.4 | 13 | 14.4 | 14 | 22.6 |
| Overall Life Satisfaction Rating (1-5) | 3.15 | (0.69) | 3.19 | (0.67) | 3.15 | (0.63) | 3.10 | (0.75) |
| Very Good | 2 | 1.4 | 0 | 0.0 | 0 | 0.0 | 2 | 3.2 |
| Good | 16 | 11.5 | 11 | 12.8 | 11 | 12.2 | 7 | 11.3 |
| Fair | 81 | 58.3 | 47 | 54.7 | 55 | 61.1 | 36 | 58.1 |
| Poor | 36 | 25.9 | 25 | 29.1 | 22 | 24.4 | 15 | 24.2 |
| Very Poor | 2 | 1.4 | 1 | 1.2 | 1 | 1.1 | 1 | 1.6 |
| Hx of Suicide Attempts & gestures | 53 | 38.1 | 33 | 38.4 | 29 | 32.2 | 24 | 38.7 |
| Psychosocial treatment | ||||||||
| Current Individual Therapy | 64 | 46.0 | 38 | 44.2 | 37 | 41.1 | 31 | 50.0 |
| Lifetime Individual Therapy | 120 | 86.3 | 72 | 83.7 | 76 | 84.4 | 55 | 88.7 |
| Psychotropic Medication | ||||||||
| Current | 74 | 53.2 | 48 | 55.8 | 42 | 46.7 | 38 | 61.3 |
| Lifetime | 108 | 77.7 | 67 | 77.9 | 67 | 74.4 | 49 | 79.0 |
| Comorbidity | ||||||||
| Number of Lifetime Axis-I Disorders | 5.19 (M) | 1.95 (SD) | 5.67 (M) | 1.88 (SD) | 5.26 (M) | 2.10 (SD) | 5.85 (M) | 2.12 (SD) |
| Number of Current Axis-I Disorders | 3.47 (M) | 1.67 (SD) | 3.93 (M) | 1.61 (SD) | 3.67 (M) | 1.73 (SD) | 3.98 (M) | 1.79 (SD) |
| Any Anxiety Disorder Current* | - | - | 84 | 97.7 | 79 | 87.8 | 57 | 91.9 |
| GAD Current | 90 | 64.7 | 51 | 59.3 | - | - | 35 | 56.5 |
| Panic w/Ag Current | 62 | 44.6 | 36 | 41.9 | 35 | 38.9 | - | - |
| Panic wo/Ag Current | 8 | 5.8 | 4 | 4.7 | 6 | 6.7 | 0 | 0.0 |
| Social Anxiety Dx Current | 86 | 61.9 | - | - | 51 | 56.7 | 36 | 58.1 |
| Specific Phobia Current | 56 | 40.3 | 41 | 47.7 | 34 | 37.8 | 27 | 43.5 |
| OCD Current | 31 | 22.3 | 21 | 24.4 | 21 | 23.3 | 19 | 30.6 |
| PTSD Current | 37 | 26.6 | 18 | 20.9 | 23 | 25.6 | 20 | 32.3 |
| Anxiety NOS Current | 9 | 6.5 | 8 | 9.3 | 3 | 3.3 | 2 | 3.2 |
| Any Mood Disorder Lifetime | 124 | 89.2 | 81 | 94.2 | 80 | 88.9 | 55 | 88.7 |
| Any Mood Disorder Current | 68 | 48.9 | 45 | 52.3 | 43 | 47.8 | 32 | 51.6 |
| MDD Current | 65 | 46.8 | 43 | 50.0 | 42 | 46.7 | 32 | 51.6 |
| Dysthymia Current | 2 | 1.4 | 2 | 2.3 | 0 | 0.0 | 0 | 0.0 |
| Bipolar Disorder current | 2 | 1.4 | 2 | 2.3 | 0 | 0.0 | 1 | 1.6 |
| Any Eating Disorder Lifetime | 24 | 17.3 | 17 | 19.8 | 17 | 18.9 | 16 | 25.8 |
| Any Eating Disorder Current | 10 | 7.2 | 8 | 9.3 | 7 | 7.8 | 4 | 6.5 |
| Alcohol Abuse Current | 1 | 0.7 | 1 | 1.2 | 1 | 1.1 | 0 | 0.0 |
| Alcohol Dependence Current | 5 | 3.6 | 3 | 3.5 | 4 | 4.4 | 2 | 3.2 |
| Drug Abuse Current | 2 | 1.4 | 2 | 2.3 | 2 | 2.2 | 1 | 1.6 |
| Drug Dependence Current | 4 | 2.9 | 3 | 3.5 | 2 | 2.2 | 1 | 1.6 |
Notes: M = Mean, SD = Standard Deviation
= Any Anxiety Disorder refers to any other anxiety disorder, excluding the column header disorder.
Clinical Course of Anxiety Disorders and MDD
Mean self-reported duration of SAD in the sample was 21.00 years (SD = 12.96) prior to intake, with 97.7% reporting that their first episode remained current (N = 84). Participants with SAD (N = 48 at two-year follow-up) had a 0.07 probability of achieving full recovery over two years of follow-up (N = 3). Of the 3 participants who experienced a recovery, none had a recurrence by the end of the follow-up period. No significant differences in survival rates were found for employment (employed at intake vs. not); χ2 (1) = 0.18, p = .67, education (at least high school vs. greater than high school); χ2 (1) = 0.05, p = .83, income (<$20,000 per year vs >$20,000 per year); χ2 (1) = 0.43, p = .51, receiving any treatment at intake; χ2 (1) = 0.004, p = .95, being born in the U.S. (vs. foreign born); χ2 (1) = 0.04, p = .84, or first language (English, Spanish or Bilingual); χ2 (2) = 0.93, p = .62.
Mean self-reported duration of GAD was 13.88 years (SD = 11.31) prior to intake. 93.3% (N = 84) reported that their first episode of GAD remained current to the time of intake. Participants with GAD (N = 56 at two-year follow-up) had a 0.14 probability of achieving full recovery over two years of follow-up (N = 8). Of the 8 participants who experienced recovery, 2 (25.0%) experienced a recurrence by the end of the follow-up period. No significant differences in survival rates were found for employment; χ2 (1) = 0.13, p = .72, education; χ2 (1) = 3.19, p = .07, income; χ2 (1) = 3.16, p = .08, receiving treatment at intake; χ2 (1) = 0.04, p = .85, being born in the U.S.; χ2 (1) = 1.13, p = .29, or first language; χ2 (2) = 2.13, p = .34.
Mean self-reported duration of PDA was 12.26 years (SD = 12.55) prior to intake, with 93.5% (N = 58) reporting that their first episode remained current to the time of intake. Participants with PDA (N = 48 at two-year follow-up) had a 0.03 probability of achieving full recovery over two years of follow-up (N = 1). The one participant who experienced a recovery did not have a recurrence by the end of the follow-up period. No significant differences in survival rates were found for employment; χ2 (1) = 1.84, p = .18, education; χ2 (1) = 2.49, p = .12, income; χ2 (1) = 0.02, p = .89, receiving any treatment at intake; χ2 (1) = 0.56, p = .46, being born in the U.S.; χ2 (1) = 0.06, p = .80, or first language; χ2 (2) = 1.75, p = .42.
At intake, 65 participants (46.1%) were also diagnosed with current MDD. Participants with MDD (N = 38 at two-year follow-up) had a 0.50 probability of achieving full recovery during the two years of follow-up (N = 18). Of the individuals that recovered, 4 participants (22.2%) had a recurrence by the end of the follow-up period. No significant differences in survival rates were found for employment; χ2 (1) = 0.04, p = .84, education; χ2 (1) = 0.56, p = .46, income; χ2 (1) = 1.73, p = .19, receiving any treatment at intake; χ2 (1) = 0.01, p = .92, being born in the U.S.; χ2 (1) = 0.25, p = .62, or first language; :χ2 (2) = 1.34, p = .51.
Discussion
HARP-II is the first prospective, observational study of the course of anxiety disorders among Latinos. This study revealed markedly low recovery rates for anxiety disorders in this sample. HARP-II was modeled on the same methodology as HARP-I and PCAP, which provide comparison data in mostly non-Latino White samples. Although such comparisons must be done with caution in light of different recruitment methods, cohort effects, and differences in measures, it is noteworthy that the two-year recovery rates for anxiety disorders is much lower in HARP-II compared to the HARP-I and PCAP samples (see Table 4). However, the recovery rates for major depressive disorder (MDD) over two years were similar in HARP-I and HARP-II (0.50 in HARP-II compared to approximately 0.48 in HARP-I for MDD; Bruce et al., 2005). These findings are the opposite of the pattern of results Breslau and colleagues (2005) reported, in which mood disorders (but not anxiety disorders) were found to be more persistent in Latinos than non-Latino Whites. However, as already noted, the validity of the Breslau finding is unclear due to it being based on a one-time retrospective assessment of the duration of illness. The current study invokes the pressing question of whether there is something about the experience of anxiety disorders (but not MDD) among Latinos that makes them more insidious.
Table 4.
2-Year Recovery Rates in HARP-I, PCAP and HARP-II (for Latinos) for Social Anxiety Disorder, Generalized Anxiety Disorder and Panic Disorder with Agoraphobia
| HARP-I | PCAP | HARP-II | |
|---|---|---|---|
| Social anxiety disorder | 0.20 | 0.31 | 0.07 |
| Generalized anxiety disorder | 0.25 | 0.39 | 0.14 |
| Panic disorder w. agoraphobia | 0.23 | 0.16 | 0.03 |
Notes: HARP-I = Harvard/Brown Anxiety Research Program – first wave, PCAP = Primary Care Anxiety Project, HARP-II = Harvard/Brown Anxiety Research Program - second wave.
The importance of this question is further revealed as other variables in this study are considered. This sample was fairly well educated, and yet levels of employment and poverty were extremely high. Severity of illness and comorbidity was high, and functioning and social adjustment markedly poor, and yet treatment was underutilized. It may be argued that these survival rates are a function of socio-economic variables, such as poverty, or variables such as receiving therapy, being born in the U.S. and whether English was the participants′ first language. However, the lack of significant differences in survival rates as a function of these variables points to a different direction. Cultural factors (such as acculturative stress, perceived discrimination and immigration status) that are well-known from research on mental health in Latinos may be a part of the explanation. In addition, although being in treatment at intake did not predict course, it is possible that the quality of the treatment received may have been less, in general, compared to non-Latino Whites. Future research should aim at teasing apart these causal mechanisms and important mediators and moderators of clinical course.
There are several strengths and weaknesses to this study. The observational design of this study precluded us being able to manipulate variables (e.g., treatment) which may contribute to the course of these disorders. On the other hand, HARP-II provides a view of what is taking place in the real world with respect to Latinos with anxiety disorders.This is not, however, an epidemiological study. This study uses a convenience sample of English-speaking Latinos and the results may not generalize to all Latinos, especially when considering levels of English proficiency and poverty. It is important to emphasize this point, since the experience of psychiatric disorders in various subgroups of the Latino population may be different (Alegría et al., 2007). Strengths of this study include the prospective design, careful training of assessors, comprehensive clinical interviews with excellent psychometric properties and widely acknowledged definitions of concepts such as recovery.
In summary, this first prospective, observational study of anxiety disorders among Latinos indicates that the course of anxiety disorders (but not MDD) may be more persistent and impairing among Latinos than non-Latino Whites. Furthermore, the experience of anxiety disorders in this sample was marked by severe symptoms, low levels of functioning, and high levels of comorbidity. Future studies should identify the mechanisms underlying the chronicity of anxiety disorders in this population, which will be critical in treatment development efforts for anxiety disorders among Latinos.
Figure 1.
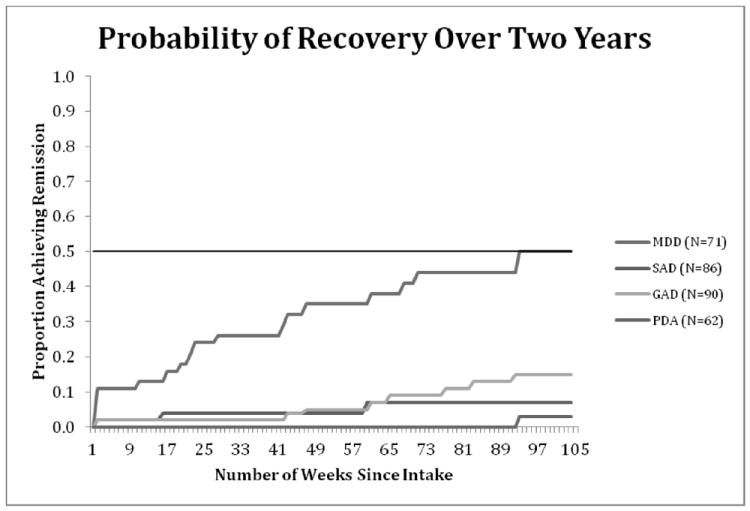
Cumulative Probability of Recovery in Latino-American Patients with GAD, SAD, PDA, and Comorbid MDD Over Two Years of Prospective Follow-up.
Acknowledgments
Martin B. Keller, Ethan Moitra and Risa B. Weisberg have received grant support from Pfizer, Inc. in the past year. Harvard/Brown Anxiety Research Project-Phase II (HARP-II) is funded by the National Institute of Mental Health (NIMH), Bethesda, MD (R01 MH51415). HARP was supported in the past by Upjohn Co, Wyeth-Ayerst Laboratories, Eli Lilly, and NIMH (MH-51415). Since 2008, HARP has been funded solely by NIMH.
This study was conducted with the current participation of the following collaborators: Martin B. Keller, M.D. (Chairperson); Risa B. Weisberg, Ph.D.; Robert L. Stout, Ph.D.; Ingrid R. Dyck, M.P.H.; Phillip Leduc; Benjamin F. Rodriguez, Ph.D.; Carlos Pérez Benítez, Ph.D.; Brooke A. Marcks; Ph.D; Holly J. Ramsawh, Ph.D.; Lisa A. Uebelacker, Ph.D.; Courtney Beard, Ph.D.; Andri S. Bjornsson, Ph.D.; Nicholas J. Sibrava, Ph.D.; Ethan Moitra, Ph.D.; and, Russell G. Vasile, M.D. This manuscript has been reviewed by the Publication Committee of HARP and has its endorsement. The original principal and co-investigators included Martin B. Keller, M.D. (Chairperson); Jane Eisen, M.D.; Eugene Fierman, M.D.; Robert M. Goisman, M.D.; Idell Goldenberg, Psy.D.; Gopi Mallya, M.D.; Ann Massion, M.D.; Timothy Mueller, M.D.; Kathleen Phillips, M.D.; Fernando Rodriguez-Villa, M.D.; Malcolm P. Rogers, M.D.; Carl Salzman, M.D.; M. Tracie Shea, Ph.D.; Gail Steketee, Ph.D.; Robert L. Stout, Ph.D.; Russell G. Vasile, M.D.; Meredith G. Warshaw, M.S.S., M.A.; Risa B. Weisberg, Ph.D.; Kimberly A. Yonkers, M.D.; and, Caron Zlotnick, Ph.D. Additional contributions from: Paul Alexander, M.D.; Jonathan Cole, M.D; James Ellison, M.D., M.P.H.; Alan Gordon, M.D.; Robert Hirschfeld Ph.D.; Philip Lavori, Ph.D.; John Christopher Perry, M.D.; Linda Peterson; Steven Rasmussen, M.D.; James Reich, M.D., M.P.H.; John Rice, Ph.D.; Harriet Samuelson, M.A.; David Shera, M.S.; Naomi Weinshenker, M.D.; Myrna Weissman, Ph.D.; and, Kerrin White, M.D.
The authors wish to thank Dr. Robert L. Stout for providing statistical consultation.
Footnotes
Weisberg et al. (2012) describe the methods for HARP-II in more detail.
References
- Alegría M, Mulvaney-Day N, Torres M, Polo A, Cao Z, Canino G. Prevalence of psychiatric disorders across Latino subgroups in the United States. American Journal of Public Health. 2007;97:68–75. doi: 10.2105/AJPH.2006.087205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría M, Shrout PE, Torres M, Lewis-Fernández RL, Abelson J, Powell M, Canino G, et al. Lessons learned from the Clinical Reappraisal Study of the Composite International Diagnostic Interview with Latinos. International Journal of Methods in Psychiatric Research. 2009;18:84–95. doi: 10.1002/mpr.280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Text-Revision. 4. Washington, DC: Author; 2000. [Google Scholar]
- Beard C, Moitra E, Weisberg RB, Keller MB. Characteristics and predictors of social phobia course in a longitudinal study of primary-care patients. Depression and Anxiety. 2010;27:839–845. doi: 10.1002/da.20676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau J, Kendler KS, Maxwell S, Gaxiola-Aguilar S, Kessler RC. Lifetime risk and persistence of psychiatric disorders across ethnic groups in the United States. Psychological Medicine. 2005;35:317–327. doi: 10.1017/s0033291704003514. doi: dx.doi.org/10.1017/S0033291704003514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruce SE, Yonkers KA, Otto MW, Eisen JL, Weisberg RB, Pagano M, Keller MK, et al. Influence of psychiatric comorbidity on recovery and recurrence in generalized anxiety disorder, social phobia, and panic disorder: A 12-year prospective study. American Journal of Psychiatry. 2005;162:1179–1187. doi: 10.1176/appi.ajp.162.6.1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Familiar I, Borges G, Orozco R, Medina-Mora M-E. Mexican migration experiences to the US and risk for anxiety and depressive symptoms. Journal of Affective Disorders. 2011;130:83–91. doi: 10.1016/J.JAD.2010.09.025. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis-I Disorders - Patient Edition (SCID-I/PI, Version 2.0) New York: Biometrics Research Department; 1996. [Google Scholar]
- Flores E, Tschann JM, Dimas JM, Pasch LA, de Groat CL. Perceived racial/ethnic discrimination, posttraumatic stress symptoms, and health risk behaviors among Mexican American adolescents. Journal of Counseling Psychology. 2010;57:264–273. doi: 10.1037/20020026. [DOI] [PubMed] [Google Scholar]
- Francis JL, Weisberg RB, Dyck IR, Culpepper L, Smith K, Orlando Edelen M, Keller ML, et al. Characteristics and course of panic disorder and panic disorder with agoraphobia in primary care patients. Primary Care Companion, Journal of Clinical Psychiatry. 2007;9:173–179. doi: 10.4088/pcc.v09n0301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hovey JD, Magaña CG. Cognitive, affective, and physiological expressions of anxiety symptomatology among Mexican migrant farmworkers: Predictors and generational differences. Community Mental Health Journal. 2002;38:223–237. doi: 10.1023/A:1015215723786. [DOI] [PubMed] [Google Scholar]
- Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott P, Andreasen NO, et al. The Longitudinal Interval Follow-up Evaluation: A comprehensive method for assessing outcome in prospective longitudinal studies. Archives of General Psychiatry. 1987;44:540–548. doi: 10.1001/archpsych.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- Rodriguez BF, Weisberg RB, Pagano ME, Bruce SE, Spencer MA, Culpepper L, Keller MB. Characteristics and predictors of full and partial recovery from generalized anxiety disorder in primary care patients. Journal of Nervous and Mental Disease. 2006;194:91–97. doi: 10.1097/01.nmd.0000198140.02154.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ventura J, Liberman RP, Green MF, Shaner A, Mintz J. Training and quality assurance with the Structured Clinical Interview for DSM-IV (SCID-I/P) Psychiatry Research. 1998;79:163–173. doi: 10.1016/S0165-1781(98)00038-9. [DOI] [PubMed] [Google Scholar]
- Warshaw MG, Keller MB, Stout RL. Reliability and validity of the longitudinal interval follow-up evaluation for assessing outcome of anxiety disorders. Journal of Psychiatric Research. 1994;28:531–545. doi: 10.1016/0022-3956(94)90043-4. [DOI] [PubMed] [Google Scholar]
- Weisberg R, Beard C, Dyck I, Keller MB. The Harvard/Brown Anxiety Research Project – Phase II (HARP-II): Rationale, methods, and features of the sample at intake. Journal of Anxiety Disorders. 2012;26:532–543. doi: 10.1016/j.janxdis.2012.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]


