Abstract
Background
Adherence is a challenge in obesity treatment. Motivational interviewing (MI) may promote patient adherence. MI Values is a randomized controlled trial of MI implemented as an adjunct to an adolescent obesity treatment (T.E.E.N.S.).
Objective
Assess effects of MI Values on T.E.E.N.S. attrition and adherence.
Methods
Participants were randomized to MI (n=58) or control (n=41). At weeks 1 and 10, MI participants had brief MI sessions; controls viewed health education videos. All participants continued with T.E.E.N.S. (biweekly dietitian and behavioral support visits; 3x/week supervised physical activity). Assessments were repeated at baseline, 3 and 6-months. T-tests and chi-square analyses examined T.E.E.N.S. attrition and adherence by group.
Results
Adolescents (N=99) were primarily African American (73%) females (74%); age=13.8±1.8 years, body mass index percentile=98.0±1.2. Compared with controls, MI participants had greater 3-month adherence overall (89.2% vs. 81.0%, p=0.040), and to dietitian (91.3% vs. 84.0%; p=0.046) and behavioral support (92.9% vs. 85.2%; p=0.041) visits, and greater 6-month adherence overall (84.4% vs. 76.2%, p=0.026) and to behavioral support visits (87.5% vs. 78.8%, p=0.011).
Conclusions
MI enhanced adherence to this obesity intervention. MI Values is the first study to examine the impact of MI on treatment adherence among obese, primarily African American adolescents.
Keywords: motivational interviewing, pediatric obesity, treatment adherence
Introduction
Over one-third of U.S. children are overweight or obese, with higher rates among African Americans (AA) compared with Whites.1 Lifestyle intervention remains the mainstay of treatment.2,3 Poor treatment adherence and high attrition, however, are frequently encountered in obesity interventions, reducing their effectiveness.4–6 These issues are particularly pernicious within traditionally underserved populations.6 Innovative strategies to enhance retention and treatment adherence are needed, particularly among AA adolescents with obesity, who are at great risk for related health complications.6,7
Many strategies are recommended to address treatment adherence, including implementing a culturally sensitive intervention, using an easily accessible location, providing incentives, and making frequent participant contact.5 It is also likely that individual factors, including adolescent ambivalence about making behavioral changes, contribute to these challenges.8 Thus, targeted strategies addressing ambivalence about behavior change are needed. One innovative strategy demonstrated to increase adolescent treatment engagement in multiple behavioral domains is motivational interviewing (MI).9
MI is described as “a way of being with a patient,” that is patient-centered, non-judgmental and empathic, and seeks to reduce ambivalence and increase readiness to change via adherence to its spirit.8 Adolescence in particular is a developmental transition often accompanied by feelings of ambivalence as youth seek autonomy and reject authority. By rolling with (rather than confronting) resistance, eliciting adolescent-determined reasons for change, and treating adolescents as partners, MI might be particularly effective for this age group. Thus, implementing MI focused on behavior change as part of obesity treatment (targeting adolescents directly) might enhance treatment engagement via greater program attendance and adherence, ultimately leading to improved outcomes in this population.10–14
Despite its potential, few randomized controlled trials (RCTs) have evaluated MI with adolescents seeking obesity treatment.11,15–17 A meta-analysis investigating MI in adult obesity RCTs found that MI enhanced weight loss, with the greatest effects found when MI was an adjunct to behavioral weight loss treatment.18 Among adolescents, however, RCTs in this area are limited to a weight control program implemented in churches targeting overweight AA females,19 a Canadian study investigating MI in addition to a standard obesity program,17 and a small pilot comparing dietitian-delivered MI to an education control.16 Although none found group differences in body mass index (BMI) reduction, their results, combined with those investigating MI in other adolescent behavioral domains, provide guidance for future investigations. For example, studies demonstrated that adding MI early in treatment increases program adherence and improves outcomes.9 Further, while ultimate treatment goals are to effect BMI change, examining the effects of MI on proximal outcomes (e.g., adherence) can enhance understanding of mechanisms associated with treatment effects.16 Current recommendations state that health professionals integrate MI into pediatric obesity treatments.20 However, a clear need for rigorous investigations in this area remains, particularly among high-risk adolescents.9,11,16,20
The Current Study
MI Values was a RCT designed to investigate if brief (two session) MI can enhance treatment effects among adolescents with obesity enrolled in a multidisciplinary treatment (the T.E.E.N.S. [Teaching Encouragement Exercise Nutrition Support] Program).21 In the current report, we examine the impact of MI Values on T.E.E.N.S.’ treatment adherence (a proximal outcome), positing that participants in the MI treatment arm would manifest lower attrition and improved adherence to T.E.E.N.S. compared with those randomized to the education control. Thus the current report examines an indirect causal pathway between MI (targeting behavior change) and attendance and retention.
Methods
Participants
Adolescents ages 11–18 years with BMI ≥85th percentile for age and gender,22 with no underlying medical etiology of obesity (e.g., a genetic/congenital condition [e.g., Prader-Willi syndrome]), and with a participating parent/caregiver were eligible for T.E.E.N.S. and the adjunctive study, MI Values. Parents and adolescents provided written informed consent and assent, respectively. Study procedures were approved by the Institutional Review Board of Virginia Commonwealth University.
Design and Procedures
T.E.E.N.S
T.E.E.N.S. is a multidisciplinary treatment that includes physical activity, dietary intervention, and behavioral support.23–25 Parents attended bi-weekly groups (independent from adolescents). Participants met on alternating weeks with a dietitian and behavioral support specialist throughout T.E.E.N.S.’ initial six months. Adolescents performed supervised physical activity ≥3x/week at the T.E.E.N.S. gymnasium, and were encouraged to exercise on additional days (YMCA memberships provided).
MI Values
From 2009–2011, T.E.E.N.S. participants who also consented to MI Values were randomized to either a MI or education control treatment. All participants proceeded with T.E.E.N.S. treatment as usual. Detailed MI Values procedures have been reported,21 and are briefly described below.
Adolescents in the MI treatment participated in two 30 minute, individual MI sessions at weeks 1 and 10 of T.E.E.N.S., led by interventionists independent from T.E.E.N.S. Timing for session 1 was selected due to benefits of MI early in treatment, a common point of attrition across obesity trials;6,9 session 2 was implemented at week 10 due to patterns of increased attrition at month 3 of T.E.E.N.S. Interventionists followed a roadmap: Establish Rapport→Agenda Setting→Explore Target Behavior→Explore Values/Goals→Explore Ambivalence/Readiness to Change→Negotiate Change Plan→Summary. Participants selected target behaviors, and included T.E.E.N.S. participation, diet and/or exercise (in general or a specific dietary/exercise behavior). Session 1 included a values clarification exercise; participants selected their top 5 values and were prompted to explore the relation of these values to their target behavior.19,26 Clinicians helped participants develop discrepancy between values and current behaviors, intending to increase readiness to change to achieve congruency. In session 2, interventionists explored progress in T.E.E.N.S., re-examined value/behavior congruency, and elicited participant ideas for change. Throughout treatment, interventionists examined motivation and confidence to change, using open-ended questions and reflections to elicit change talk, resolve ambivalence, highlight autonomy and support self-efficacy. In control sessions, participants viewed 30 minute health education videos at identical time periods, proctored by interventionists, to match on attention without confounding content. Follow-up assessments were completed at 3- and 6-months.
Intervention Fidelity
Interventionists participated in a 2-day training conducted by a member of the Motivational Interviewing Network of Trainers and 30 hours of practice. Weekly supervision and feedback were provided throughout the study. MI sessions were audiotaped and coded by trained raters, blinded to study hypotheses, using the MI Treatment Integrity Code (MITI) 3.0.27 Interventionists demonstrated high fidelity: 77% complex reflections, 83% open questions, and average global spirit was 4.4 (of a possible 5.0), exceeding competency thresholds.21,27 Inter-rater reliabilities across domains were strong (intra-class correlations: 0.72–0.99).
Measures
Demographics
Age, gender, race, and parent education and income were reported at baseline.
Anthropometrics
Height was measured to the nearest 0.1 cm using a stadiometer (Holtain Limited by Crymmych Pembs, U.K.). Weight was measured in light clothing with shoes removed to the nearest 0.1 kg using an electric scale (“Health-o-meter” model 2500 KL, Serial #971ow2407). Data were used to calculate BMI (kg/m2). BMI z-scores and age and gender-specific BMI percentiles were determined using Epi Info software (CDC, Version 3.3).
Treatment Adherence and Attrition
Participants’ adherence to T.E.E.N.S. sessions (gym, dietitian, and behavioral support) was monitored throughout the study. Percentage of visits attended in each domain was calculated (visits attended/total possible visits) to reflect treatment adherence. A total adherence score was calculated, averaging the three subdomains. Weeks of T.E.E.N.S. participation was examined using date of enrollment and last date of attendance in any T.E.E.N.S. activity. Three and six month attrition from T.E.E.N.S. was examined using a dichotomous (1=yes; 0=no) variable delineating if a participant was still participating at the 3- and 6-month assessments, respectively (participants were included if they were still participating at the respective time point, regardless if they completed assessments). Participants who remained in T.E.E.N.S. longer than 3-months, but less than 6-months, were considered active only at 3-months.
Analyses
Primary outcomes for this investigation were retention and adherence to T.E.E.N.S. SPSS v.21.0 (Chicago, IL) was used in analyses. After descriptive analyses, chi squares and one-way ANOVAs examined baseline differences in study variables by treatment condition (MI or control). Independent samples t-tests explored group (MI vs. control) differences in adherence to: 1) dietitian, 2) behavior support, 3) gym, and 4) overall. Interventionist effects were examined with t-tests. Excluding participants (n=12) who did not receive the adjunctive treatment (MI or control), chi square analyses examined differential attrition at 3- and 6-months, and t-tests examined total weeks of T.E.E.N.S. participation by treatment condition and gender. Lastly, point-biserial (categorical variables) and Pearson’s (continuous variables) correlations examined associations among 3- and 6-month treatment adherence (total, dietitian, behavior support, and gym), demographics (race, gender, parental income and education), BMI percentile, and attrition. Post-hoc analyses examined within group correlations among 3-and 6-month total adherence and retention, demographics and BMI percentile, followed by multiple regression analyses examining if income moderated the relation between treatment group and overall adherence and retention at 3-months and 6-months. P<0.05 was used to determine significance.
Results
Participants and Recruitment
Consent rate was 82.1%, with 101/123 of T.E.E.N.S. participants consenting to MI Values. Participants who declined (17.9%) continued with TEENS as usual. There were no differences in consent rate by age, gender, race, or BMI percentile (p>0.05). Ninety-nine participants were randomized and completed baseline assessments (n=58 MI; n=41 control; Table 1). Notably, 20.6% of potential participants did not complete the T.E.E.N.S. enrollment process and were subsequently lost to follow-up after initially consenting (i.e., lost to follow-up after enrollment or did not obtain additional medical/psychological clearance required). Families with incomes <$40,000 were more likely to drop out prior to program initiation than families with incomes ≥$40,000 (χ2(1)=6.48, p=0.011).
Table 1.
Baseline Characteristics by Treatment Condition
| Variable | Total Sample M (SD) or % N = 99 |
MI M (SD) or % N = 58 |
Control M (SD) or % N = 41 |
p |
|---|---|---|---|---|
| Female (%) | 73.7% | 75.9% | 70.7% | 0.568 |
| Racea | 0.456 | |||
| Black | 72.4% | 75.4% | 68.3% | |
| White | 19.4% | 19.3% | 19.5% | |
| Other | 8.2% | 5.3% | 12.2% | |
| Age (years) | 13.8 (1.8) | 13.6 (1.8) | 14.1 (1.7) | 0.195 |
| BMI Percentile | 98.9 (1.2) | 98.9 (1.0) | 98.9 (1.3) | 0.929 |
| BMI z score | 2.4 (0.3) | 2.4 (0.3) | 2.4 (0.3) | 0.717 |
| Parent Educationb | 0.067 | |||
| High School Graduate or Less | 25.6% | 19.6% | 34.3% | |
| Some College | 33.7% | 43.1% | 20.0% | |
| College Degree or Beyond | 40.7% | 37.3% | 45.7% | |
| Family Incomec | 0.499 | |||
| <$40,000 | 52.9% | 56.0% | 48.6% | |
| ≥$40,000 | 47.1% | 44.0% | 51.4% |
Note: No group (intervention vs control) differences were found; n = 58 Intervention group, n = 41 Control group except where noted below.
n = 57 MI group
n = 35 control group; n = 51 MI group
n = 35 control group; n = 50 MI group
MI = Motivational Interviewing; BMI = Body mass index
Treatment Adherence
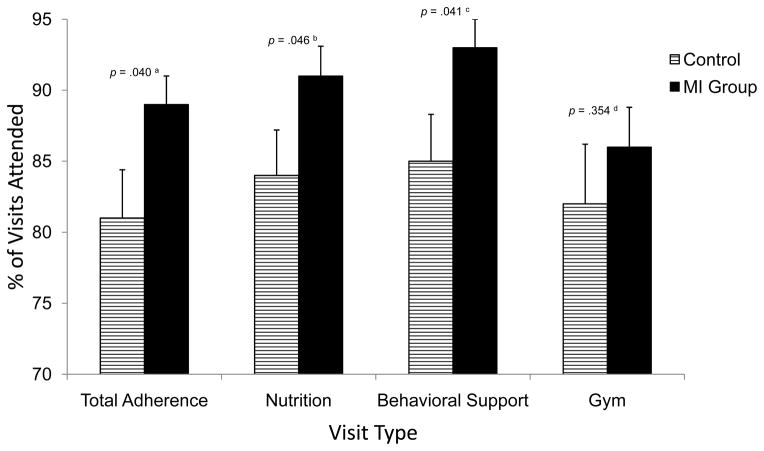
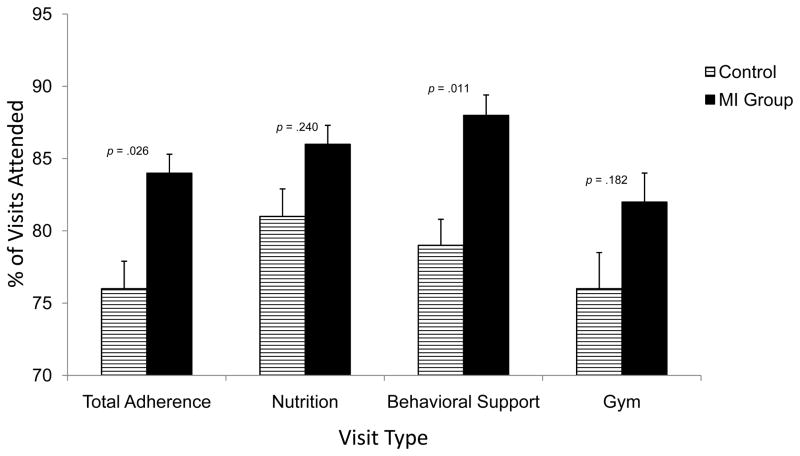
Figures 1 and 2 display adherence to T.E.E.N.S. (total, dietitian, behavior support, and gym) by treatment group. At 3-month follow-up, MI participants were more adherent than controls overall (p=0.040) and with dietitian (p=0.046) and behavior support (p=0.041) visits. At 6-months, MI participants were more adherent than controls overall (p=0.026) and with behavioral support (p=0.011) visits. Gender was not an effect moderator (p>0.05). There were no interventionist effects on adherence or retention (p>0.05).
Figure 1.
Three Month Adherence with T.E.E.N.S. Program Activities by Treatment Group
Note: Percentage of visits attended was calculated by dividing the number of visits attended by the participant by the total number of potential visits. At 3-months, the maximum number of sessions was: 6 nutrition, 6 behavior support, and 36 gym visits. P values represent results of independent samples t-tests. Effect sizes (Cohen’s d) are as follows: aTotal Adherence = 0.44; bNutrition = 0.41; cBehavioral Support = 0.43; dGym = 0.20.
Figure 2.
Six Month Adherence with T.E.E.N.S. Program Activities by Treatment Group
Note: Percentage of visits attended was calculated by dividing the number of visits attended by the participant by the total number of potential visits. At 6-months, the maximum number of session was: 12 nutrition, 12 behavior support, and 62 gym visits. P values represent results of independent samples t-tests. Effect sizes (Cohen’s d) are as follows: aTotal Adherence = 0.49; bNutrition = 0.29; cBehavioral Support = 0.55; dGym = 0.28.
Parent education was positively associated with overall adherence at 3 (r=0.24; p=0.014) and 6 months (r=0.27; p=0.004). BMI percentile and other demographics were not related to overall adherence (p>0.05). Among MI participants, lower family income was associated with better total 3- (r=−0.33, p=0.019) and 6-month (r=−0.34, p=0.017) adherence. Conversely, among controls, higher family income was associated with better 3- (r =0.51, p=0.002) and 6-month (r=0.57, p<0.001) total adherence and with better retention at 3- (r=0.74, p<0.001) and 6-months (r=0.51, p=0.002). Post-hoc regression analyses suggested that income moderated the relation between treatment group and overall adherence at both 3- (p<0.001) and 6-months (p<0.001), such that control participants with incomes <$40,000 had lower adherence at both 3-months and 6-months than those with incomes ≥$40,000. MI participants with incomes <$40,000 manifested better adherence at both time points. With respect to retention, there was again an interaction with income at 3- (p<0.001) and 6-months (p=0.049), with the same pattern of findings: control participants with lower incomes had poorer retention than those with higher incomes; in the MI group, participants with lower incomes had better retention than those with higher incomes.
Table 2 outlines MI Values dose and retention for adolescents who participated in at least one treatment session. There were no group or interventionist differences in retention. Although nonsignificant, MI participants remained in T.E.E.N.S. ~8 weeks longer than controls. Not shown in Table 2 is that, in the total sample, participants who were still engaged in T.E.E.N.S. at the 3-month follow-up had parents with higher educational attainment (r=0.23; p=0.015) and higher incomes (r=0.27, p=0.006) than those no longer enrolled. Higher parental education (r=0.35, p<0.001) and income (r=0.19, p=0.049) were also associated with 6-month retention. Lastly, higher parental education was associated with more weeks of T.E.E.N.S. participation (r=0.25, p=0.01).
Table 2.
Dose and Retention by Treatment Condition among Participants who Received ≥ 1 MI Values Session
| Variable | MI M (SD) or % N = 52 |
Control M (SD) or % N = 35 |
Cohen’s d | p |
|---|---|---|---|---|
| Dose (%) | 0.35 | 0.155a | ||
| 50% (1 session) | 23.1 | 37.1 | ||
| 100% (2 sessions) | 76.9 | 62.9 | ||
| Still participating at 3-months (%) | 73.1 (44.8) | 62.9 (49.0) | 0.22 | 0.312 |
| Still participating at 6-months (%) | 48.1 (50.5) | 34.2 (48.2) | 0.28 | 0.202 |
| Weeks of T.E.E.N.S. participation | 37.7 (31.8) | 29.9 (32.8) | 0.24 | 0.270 |
Note: MI = Motivational Interviewing; Adolescents (n = 12) who discontinued prior to Session 1 were excluded. 50% dose reflects percentage of participants who completed only 1 of 2 MI or Control sessions; 100% dose reflects percentage of participants who completed both MI or Control sessions. Weeks of T.E.E.N.S. participation reflects total number of weeks participant remained in the T.E.E.N.S. program. No group differences were found in independent samples t-tests or chi-square analyses.
p value indicates difference in dose between treatment groups.
Discussion
The MI Values study is one of only a handful of RCTs investigating MI as a component of pediatric obesity treatments. Adolescents in a multidisciplinary obesity treatment program who were randomized to a brief, two-session MI intervention showed greater treatment adherence than those randomized to an education control, particularly for behavioral support and dietitian visits. Additionally, adolescents in the MI group remained enrolled in T.E.E.N.S. for ~8 weeks longer than control participants. Although not statistically significant, this increase in length of stay might be clinically meaningful. We have previously demonstrated that T.E.E.N.S. participation is associated with significant improvements in BMI, dietary intake, cardiorespiratory fitness, and other health indicators.23–25
Despite these findings, T.E.E.N.S. attrition was still high, particularly at 6-months. At 3-months, 73% of MI participants remained in T.E.E.N.S. (compared with 63% of the control group). By 6-month follow-up, however, only 48% of MI participants and 34% of control participants remained. Although high, rates are comparable to (or better than) retention in obesity treatments targeting similar populations. For example, 4-month retention was 45% in an interdisciplinary obesity treatment targeting a similarly low income, ethnically diverse population.28 Although 6-month retention was not examined in this prior study, MI Values retention was higher in the MI treatment arm at both 3-months (73%) and 6-months (48%), suggesting potential benefits of MI among underserved, obese adolescents. A recent review of pediatric weight management programs found attrition to be as high as 73% in some programs; factors associated with attrition include higher BMI z-scores, AA race, and eligibility for Medicaid.6 Indeed, T.E.E.N.S. families were 75% AA and 46% received Medicaid. We found that lower income and education were associated with higher attrition, further highlighting the need to address socioeconomic treatment barriers. Moreover, income moderated the relation between treatment group and retention and adherence, such that in the MI group, families with lower incomes had better adherence and retention than those with higher incomes; conversely, control families with higher incomes had better adherence and retention than those with lower incomes. Thus, MI might be effective for lower income families, who also manifest high levels of treatment drop-out.6 Further investigation of characteristics associated with better MI responders might inform targeted interventions. Given the high cost of obesity treatment and similarly high cost of implementing a MI treatment with integrity, novel and parsimonious strategies for addressing attrition are paramount to inform resource allocation.
An additional related finding was the high attrition (20.6%) encountered immediately after enrollment, prior to the first MI session, representing a significant loss of potential participants and a common point of attrition across obesity treatments.6 (It should be noted that attrition at this point contributed to imbalanced sample sizes between groups). Thus, using MI at enrollment to explore ambivalence and readiness to participate might be an effective strategy to increase readiness to enter treatment, thereby reducing attrition. Indeed, MacDonnell and colleagues suggested that MI might be useful as a prelude to treatment to diffuse ambivalence about participation.16 Further, a single MI session was associated with very high retention (96%) when implemented as a “pre-treatment” in a nonrandomized adult behavioral weight loss trial.29 Future studies should examine whether findings are generalizable to adolescents and perhaps, parents of adolescents who are considering weight management treatment. In addition, booster MI sessions later during program participation might help address retention at later stages, as ambivalence may re-emerge due to treatment success or challenges.
Additional research on the appropriate target of MI intervention in this age group is also needed. While T.E.E.N.S. is a family-centered treatment, in MI Values, MI was conducted individually with adolescents. Family factors, including the influence of parents/caregivers, may play a significant role in adherence and retention, given the time-intensive nature of T.E.E.N.S. and reliance on parents/caregivers for instrumental (e.g., transportation) and emotional support. Indeed, while parent/caregiver ambivalence might be important to address, the positive relations between parent income and education with program retention suggests additional (and commonly reported)6 socioeconomic barriers, unlikely to be significantly modified with MI alone. Thus, multiple retention strategies are needed.
Among previous RCTs investigating MI in adolescent obesity, group differences in treatment adherence were reported only by Walpole et al., who investigated an RCT of MI compared with social skills training as an adjunct to a behavioral weight loss program.17 Overweight adolescents in the MI group attended more treatment sessions than those in a social skills training group.17 However, authors did not examine adherence to the weight loss program, only to the adjunctive treatment. Furthermore, participants were primarily White and from a higher socioeconomic status than MI Values participants; thus findings might not be generalizable. In a small clinic-based pilot, no differences in attendance were found among overweight adolescents who received four sessions of either MI or standard nutritional counseling; however, control participants were more likely to receive at least 50% of treatment dose.16 Importantly, this intervention differs dramatically from T.E.E.N.S., an intensive, interdisciplinary treatment. Because MI is hypothesized to effect changes via its impact on behaviors, continued examination of proximal outcomes (e.g., retention and adherence) are needed to identify mechanisms of change in obesity interventions.
Although not examined in the current report, we will also investigate the effects of MI Values on diet, physical activity, and BMI percentiles. MI Values was powered on BMI percentile, the primary trial outcome. There was also large variability in adherence and retention. Thus, Type II error likely contributes to some nonsignificant findings on these secondary study outcomes. We do not differentiate reasons for missed sessions; thus data reflect many influences on attrition and adherence encountered by this population. MI Values strengths are its RCT design and diverse sample. To our knowledge this is the only published report specifically investigating the effect of MI on treatment engagement and attrition among primarily AA adolescents enrolled in a tertiary care obesity treatment. Findings may only be generalizable to this underserved population, one that is at high risk for adult obesity and related morbidity and mortality. Future investigations should examine MI and other strategies to increase adherence and retention, to provide a more comprehensive understanding of pediatric obesity treatment efficacy and effectiveness.
What is already known about this subject
Poor treatment adherence is a notorious challenge in pediatric obesity treatments, particularly among underserved adolescents.
Motivational Interviewing (MI) might be an effective intervention strategy, yet few randomized controlled trials have investigated MI in pediatric obesity treatment.
What this study adds
We implemented MI Values, an adjunct to a multidisciplinary treatment program for obese, primarily African American adolescents, and examined if MI improved retention and adherence compared with an education control.
Adolescents randomized to MI demonstrated better adherence to an obesity program, compared with control participants.
Acknowledgments
This study was supported by a grants from the American Cancer Society to MK Bean [PFT-08-144-01-CPPB] and the National Institutes of Health [K23 HD (EPW) and CTSA award No. UL1TR000058 from the National Center for Advancing Translational Sciences]. These funding sources had no involvement with the conduct of the research or preparation of the manuscript. We are grateful to Alyssa Forcehimes, PhD for facilitating our motivational interviewing training, to Sonya Satterlund, BS, Robert Coltrain, BS, Lauren Almond, BS and April Hafer, BS for their work as coders, and to Jessye Cohen, PhD, for her assistance with the study.
Footnotes
Conflict of Interest Statement
The authors have no conflicts of interest to report.
Author contributions: MKB, SEM, EPW, and KI significantly contributed to study design. MKB, PP, and AQ were involved in data collection. MKB and PP conducted analyses and interpretation of data. All authors were involved with writing and editing the paper and had final approval of the submitted version.
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA. 2012;307(5):483–90. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Oude Luttikhuis H, Baur L, Jansen H, et al. Interventions for treating obesity in children. Cochrane Database Syst Rev. 2009;(1):CD001872. doi: 10.1002/14651858.CD001872.pub2. [DOI] [PubMed] [Google Scholar]
- 3.McGovern L, Johnson JN, Paulo R, et al. Clinical review: treatment of pediatric obesity: a systematic review and meta-analysis of randomized trials. J Clin Endocrinol Metab. 2008;93(12):4600–5. doi: 10.1210/jc.2006-2409. [DOI] [PubMed] [Google Scholar]
- 4.Jeffery RW, Drewnowski A, Epstein LH, et al. Long-term maintenance of weight loss: current status. Health Psychol. 2000;19(1 Suppl):5–16. doi: 10.1037/0278-6133.19.suppl1.5. [DOI] [PubMed] [Google Scholar]
- 5.Karlson CW, Rapoff MA. Attrition in Randomized Controlled Trials for Pediatric Chronic Conditions. Journal of Pediatric Psychology. 2009;34(7):782–793. doi: 10.1093/jpepsy/jsn122. [DOI] [PubMed] [Google Scholar]
- 6.Skelton JA, Beech BM. Attrition in paediatric weight management: a review of the literature and new directions. Obesity Reviews. 2010:e273–e281. doi: 10.1111/j.1467-789X.2010.00803.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.U.S. Department of Health and Human Services NIH. Strategic Plan for NIH Obesity Research. 2011 Mar; [Google Scholar]
- 8.Miller WR, Rollnick S. Motivational Interviewing: Preparing People for Change. Guilford Press; New York: 2002. [Google Scholar]
- 9.Hettema J, Steele J, Miller WR. Motivational Interviewing. Annual Review of Clinical Psychology. 2005;1(1):91–111. doi: 10.1146/annurev.clinpsy.1.102803.143833. [DOI] [PubMed] [Google Scholar]
- 10.Schwartz RP, Hamre R, Dietz WH, et al. Office-based motivational interviewing to prevent childhood obesity: a feasibility study. Arch Pediatr Adolesc Med. 2007;161(5):495–501. doi: 10.1001/archpedi.161.5.495. [DOI] [PubMed] [Google Scholar]
- 11.Resnicow K, Davis R, Rollnick S. Motivational interviewing for pediatric obesity: Conceptual issues and evidence review. J Am Diet Assoc. 2006;106(12):2024–33. doi: 10.1016/j.jada.2006.09.015. [DOI] [PubMed] [Google Scholar]
- 12.Suarez M, Mullins S. Motivational interviewing and pediatric health behavior interventions. J Dev Behav Pediatr. 2008;29(5):417–28. doi: 10.1097/DBP.0b013e31818888b4. [DOI] [PubMed] [Google Scholar]
- 13.VanWormer JJ, Boucher JL. Motivational interviewing and diet modification: a review of the evidence. Diabetes Educ. 2004;30(3):404–416. doi: 10.1177/014572170403000309. [DOI] [PubMed] [Google Scholar]
- 14.Taveras EM, Gortmaker SL, Hohman KH, et al. Randomized controlled trial to improve primary care to prevent and manage childhood obesity: The High Five for Kids Study. Archives of Pediatrics & Adolescent Medicine. 2011 doi: 10.1001/archpediatrics.2011.44.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Erickson SJ, Gerstle M, Feldstein SW. Brief interventions and motivational interviewing with children, adolescents, and their parents in pediatric health care settings: a review. Arch Pediatr Adolesc Med. 2005;159(12):1173–80. doi: 10.1001/archpedi.159.12.1173. [DOI] [PubMed] [Google Scholar]
- 16.MacDonell K, Brogan K, Naar-King S, Ellis D, Marshall S. A Pilot study of motivational interviewing targeting weight-related behaviors in overweight or obese African American adolescents. Journal of Adolescent Health. 2012;50(2):201–203. doi: 10.1016/j.jadohealth.2011.04.018. [DOI] [PubMed] [Google Scholar]
- 17.Walpole B, Dettmer E, Morrongiello BA, McCrindle BW, Hamilton J. Motivational Interviewing to Enhance Self-Efficacy and Promote Weight Loss in Overweight and Obese Adolescents: A Randomized Controlled Trial. Journal of pediatric psychology. 2013 doi: 10.1093/jpepsy/jst023. [DOI] [PubMed] [Google Scholar]
- 18.Armstrong MJ, Mottershead TA, Ronksley PE, Sigal RJ, Campbell TS, Hemmelgarn BR. Motivational interviewing to improve weight loss in overweight and/or obese patients: a systematic review and meta-analysis of randomized controlled trials. Obesity Reviews. 2011;12(9):709–723. doi: 10.1111/j.1467-789X.2011.00892.x. [DOI] [PubMed] [Google Scholar]
- 19.Resnicow K, Taylor R, Baskin M, McCarty F. Results of go girls: a weight control program for overweight African-American adolescent females. Obes Res. 2005;13(10):1739–48. doi: 10.1038/oby.2005.212. [DOI] [PubMed] [Google Scholar]
- 20.Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120 (Suppl 4):S164–92. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 21.Bean MK, Mazzeo SE, Stern M, Bowen D, Ingersoll K. A values-based Motivational Interviewing (MI) intervention for pediatric obesity: study design and methods for MI Values. Contemp Clin Trials. 2011;32(5):667–74. doi: 10.1016/j.cct.2011.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention. [Accessed January 17, 2006];National Center for Health Statistics. Clinical Growth Charts. 2000 Available at: http://www.cdc.gov/growthcharts/
- 23.Bean MK, Mazzeo SE, Stern M, et al. Six-Month Dietary Changes in Ethnically Diverse, Obese Adolescents Participating in a Multidisciplinary Weight Management Program. Clinical Pediatrics. 2011;50(5):408–416. doi: 10.1177/0009922810393497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Evans RK, Franco RL, Stern M, et al. Evaluation of a 6-month multi-disciplinary healthy weight management program targeting urban, overweight adolescents: effects on physical fitness, physical activity, and blood lipid profiles. Int J Pediatr Obes. 2009;4(3):130–3. doi: 10.1080/17477160802314997. [DOI] [PubMed] [Google Scholar]
- 25.Wickham EP, Stern M, Evans RK, et al. Prevalence of the metabolic syndrome among obese adolescents enrolled in a multidisciplinary weight management program: clinical correlates and response to treatment. Metab Syndr Relat Disord. 2009;7(3):179–86. doi: 10.1089/met.2008.0038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Miller WR, C’de Baca J. Quantum Change: When Epiphanies and Sudden Insights Transform Ordinary Lives. Guilford Press; New York: 2001. [Google Scholar]
- 27.Moyers TB, Martin T, Manuel JK, Miller WR, Ernst D. The Motivational Interviewing Treatment Intergrity (MITI) Code: Version 3.0. University of New Mexico, Center on Alcoholism, Substance Abuse, and Addictions; 2007. [Google Scholar]
- 28.Zeller M, Kirk S, Claytor R, et al. Predictors of attrition from a pediatric weight management program. The Journal of Pediatrics. 2004;144(4):466–470. doi: 10.1016/j.jpeds.2003.12.031. [DOI] [PubMed] [Google Scholar]
- 29.Goldberg JH, Kiernan M. Innovative techniques to address retention in a behavioral weight-loss trial. Health Educ Res. 2005;20(4):439–47. doi: 10.1093/her/cyg139. [DOI] [PubMed] [Google Scholar]