Abstract
Objective
There is evidence supporting the efficacy of cognitive-behavioral therapy (CBT) for treatment of anxiety in youth with Autism Spectrum Disorders (ASD), but long-term course of anxiety after treatment and individual predictors of treatment response are unknown. To meet the demands for personalized mental health care, information on the fit between patient and treatment as well as treatment durability is needed.
Method
We evaluated change in anxiety symptoms during intervention and one year after completion of the treatment, and evaluated predictors of response using an advanced analytical design, with follow-up data from a randomized controlled trial (RCT) of 22 adolescents (12–17 yrs) with ASD and one or more anxiety disorders.
Results
Reduction in anxiety was partially maintained during the year following treatment; greater ASD severity predicted better treatment response.
Conclusions
Our finding that brief treatment is associated with sustained gains is promising, given the pervasive and chronic nature of ASD. Implications for the treatment of anxiety in higher functioning adolescents with ASD are considered.
Keywords: autism, anxiety, intervention research, pervasive developmental disorders
Clinically impairing anxiety affects approximately 44% of children and adolescents with ASD (e.g., Van Steensel, Bogels, & Perrin, 2011). Cognitive-behavioral therapy (CBT) has demonstrated efficacy for the treatment of anxiety in typically developing children and adolescents (Seligman & Ollendick, 2011) and there is growing evidence for its efficacy in treating anxiety in youth with ASD (e.g., Reaven, Blakeley-Smith, Culhane-Shelburne, & Hepburn, 2012; White et al., 2013). At present, the longest reported follow-up period on treatment of anxiety in ASD is six months (Reaven et al., 2012; White, Ollendick, Scahill, Oswald, & Albano, 2009); little is known about sustained effects or course of anxiety in ASD.
There is also demand for personalized intervention approaches that consider what works for whom (NIMH 2011 Strategic Plan), which requires the identification of intra-individual predictors of treatment response (Kraemer, Kiernan, Essex, & Kupfer, 2008). Although CBT shows considerable promise with children and adolescents with ASD (Lickel, MacLean, Blakeley-Smith, & Hepburn, 2012), treatment response is variable. It is possible that some youth with ASD lack requisite cognitive or verbal skills to participate in CBT, resulting in limited benefit. These and other predictors of treatment response to CBT for anxiety remain to be investigated (e.g., Lord et al., 2005).
Research on predictors of long-term outcomes for individuals with ASD has shown that the strongest predictors of better outcomes in adulthood are higher cognitive function (IQ; e.g., Gabriels, Hill, Pierce, Rogers, & Wehner, 2001), higher language or verbal ability (e.g., Eaves & Ho, 2008), and less severe ASD symptoms (e.g., Howlin, Mawhood, & Rutter, 2000). Although variables that predict better outcome longitudinally may also predict response to CBT, some protective factors (i.e., higher cognitive ability and expressive language) may actually increase risk for developing problems with anxiety or depression in adolescence or adulthood. For example, there is some evidence that youth with less severe symptoms, greater insight, and unimpaired cognitive ability are more prone to anxiety and depression (Hallett et al., 2013; Kuusikko et al., 2008; Sterling, Dawson, Estes, & Greenson, 2008). Because impairment among higher functioning people is less overt, they face unique challenges and unmet service needs. Indeed, more able individuals with milder forms of ASD tend to have limited access to many resources and community services afforded to more impaired people with ASD (Mazefsky & White, in press; Taylor & Seltzer, 2010).
In addition to intra-individual factors, family and parent variables may influence treatment response and symptom course. Parental trait anxiety has been associated with higher levels of anxiety in offspring (Hirshfeld-Becker, Micco, Simoes, & Henin, 2008). Elevated parental anxiety has also been associated with poorer treatment outcome in children with anxiety disorders uncomplicated by ASD (Bodden et al., 2008). Although this relationship has not yet been studied in anxious adolescents with ASD, high parental anxiety has been associated with psychiatric symptoms in children with ASD (Conner, Maddox, & White, 2012).
Given improved identification of ASD among individuals without intellectual impairment and the frequency of anxiety symptoms in this population, careful evaluation of the long-term course following CBT is warranted. Furthermore, the heterogeneous clinical presentation of youth with ASD prompts examination of individual factors that predict treatment response. The primary purpose of this report is to examine the course of anxiety and long-term stability of reductions in anxiety, in adolescents with ASD who received CBT for anxiety. We also examine the predictors of short-term treatment response and post-treatment outcomes one-year later in study participants. Analyses of individual predictors of treatment response and maintenance are exploratory.
Methods
Participants
Data for the present study were drawn from an IRB-approved, randomized controlled trial (RCT) of a novel CBT program (White et al., 2010). Eligible participants were between 12 and 17 years, had an ASD diagnosis determined by clinical assessment and supported by the Autism Diagnostic Interview - Revised (ADI-R; Lord, Rutter, & Le Couteur, 1994) or the Autism Diagnostic Observation Schedule (ADOS; Lord, Rutter, DiLavore, & Risi, 2002), met diagnostic criteria for at least one of the following anxiety disorders: Social Phobia (SoP), Generalized Anxiety Disorder (GAD), Specific Phobia (SP), or Separation Anxiety Disorder (SAD), as determined by the Anxiety Disorders Interview Schedule for Children/Parents (ADIS-C/P; Silverman & Albano, 1996), and had a verbal IQ of 70 or above (Table 1).
Table 1.
Sample Demographics
| n (%) | M (SD) | |
|---|---|---|
| Male | 16 (72.7) | |
| Race | ||
| Caucasian | 18 (81.8) | |
| Asian | 1 (4.5) | |
| Black | 2 (9.1) | |
| Other | 1 (4.5) | |
| Primary Anxiety Disorder Diagnosis | ||
| Social Phobia | 15 (68.2) | |
| GAD | 5 (22.7) | |
| Specific Phobia | 2 (9.1) | |
| Age (in months) | 174.05 (18.66) | |
| VIQ | 98.36 (16.10) | |
Note. GAD = Generalized Anxiety Disorder
Participants were randomly assigned to begin treatment immediately or to a waiting period of 14 to 15 weeks. Treatment comprised individual CBT (~12 sessions), seven group-delivered social skills practice sessions, and parent coaching concurrent with the individual and group sessions. Participants in the treatment group completed assessments at pre-treatment, midpoint, immediately post-treatment, three months post-treatment, and one year post-treatment. Participants in the wait-list condition completed an assessment at the baseline, mid-point, and at the end of the waiting period, at which time they were offered the treatment program. The endpoint of the wait-list period was used as the new baseline [prior to starting active treatment; hereafter referred to as “pre-treatment”]. These participants were re-evaluated immediately post-treatment, three months post-treatment, and one year post-treatment.
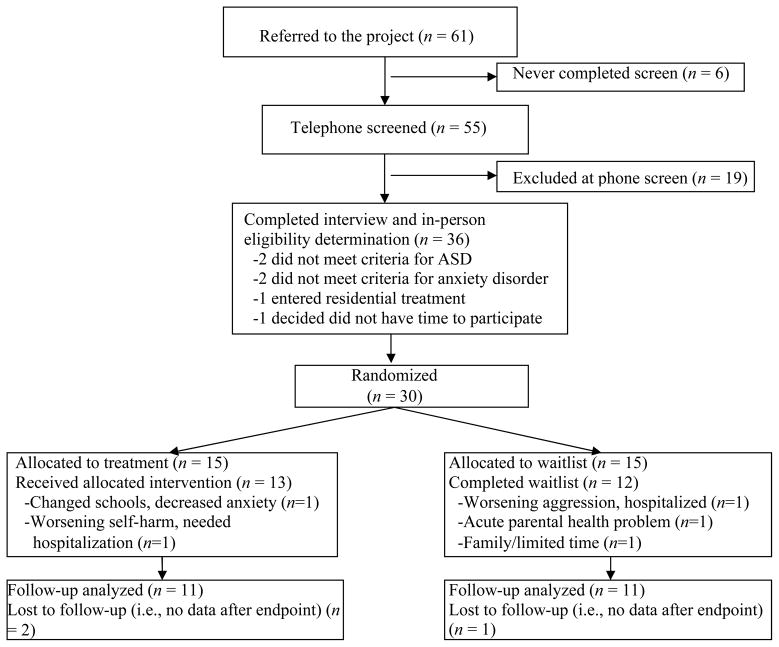
Of the 30 participants randomized in the initial trial, eight were excluded from the present analyses (Figure 1): three participants in the waitlist group never began treatment, nor did they complete follow-up assessments; two in the treatment group did not complete the full treatment (i.e., less than 12 individual sessions), nor did they complete follow-up assessments; three participants (two from treatment group, one from waitlist) did not complete endpoint or follow-up assessments. Given the primary purpose of this study was to assess long-term course following treatment completion and individual predictors of change, these eight individuals were dropped from the analysis. Efficacy results using the full sample of 30 participants, with last observation carried forward (LOCF) showed a medium between-group effect (d = .30), which was not statistically significant (see White et al., 2013). The present study combined data from the 22 participants who completed treatment to assess change during and following active intervention to maximize sample size.
Figure 1.
CONSORT Flow chart of participants through follow-up.
Measures
Child and Adolescent Symptom Inventory-4 ASD Anxiety Scale (CASI-Anx; Sukhodolsky et al., 2008)
The 20 items comprising the measure were drawn from the Child and Adolescent Symptom Inventories-4 (Gadow & Sprafkin, 1997, 1998). Parents (primary caregiver) are asked to rate each item on a 0 to 3 scale (0 = never, 1 = sometimes, 2 = often, and 3 = very often). The CASI-Anx has high internal consistency and little or no overlap with symptoms of ASD (Hallett et al., 2013). In this sample, alpha was .85 at baseline.
Social Responsiveness Scale (SRS; Constantino & Gruber, 2005)
This is a 65-item, parent-rated, dimensional measure of ASD-related symptoms. In light of evidence for a bidirectional relationship between anxiety and social impairment in ASD (e.g., Kleinhans et al., 2010), the 22-item Social Communication (SRS-SC) subscale of the SRS was selected as the primary index of ASD social disability. Internal consistency in the present sample at baseline was high for the SC subscale (alpha = .87).
State-Trait Anxiety Inventory (STAI; Spielberger, Gorssuch, Lushene, Vagg, & Jacobs, 1983)
A 40-item self-report questionnaire that assesses both stable traits of anxiety and current anxiety symptoms, parents completed the STAI at the pre-treatment visit. Only the trait scale (STAI-T), which assesses how the individual generally feels, was used in the current study. The scale’s 20 items are rated on a 4-point scale ranging from almost never to almost always. Derived internal consistency for this scale in this sample was excellent (alpha = .91).
Statistical Analyses
Paired samples t-tests were used to examine change in anxiety symptoms from pre-treatment to post-treatment and follow-up. Growth curve analysis, which has recognized advantages compared to analytic approaches such as ANCOVA with LOCF (e.g., Hamer & Simpson, 2009; Kraemer & Thiemann, 1989), was used to explore change over time. The influence of verbal ability (VIQ), ASD severity (SRS-SC), and parental anxiety (STAI-T) on trajectories of parent-rated anxiety symptoms during treatment and the one-year follow-up period was assessed using hierarchical linear modeling (HLM; Raudenbush & Bryk, 2002). Because data from the waitlist period were not used in these analyses, only data from pre-treatment forward were included. Time (indexed from entry to treatment) was entered as the level-1 predictor. Predictors of the growth parameters were entered as level-2 variables to explain the variation in growth trajectories (Raudenbush & Bryk, 2002).
HLM allows the level-1 regression coefficients to vary by participant (Hox, 2010), thus making it especially useful in treatment outcome research due to statistical power (Hox, 2010). HLM has been used previously for evaluating change in small samples (i.e., n < 50; e.g., Olatunji, Ciesielski, Wolitzky-Taylor, Wentworth, & Viar, 2012). Analyses were conducted using HLM 7.01 (Raudenbush, Bryk, & Congdon, 2012) using full maximum likelihood estimation method. A piecewise model, in which separate slopes are estimated for separate time periods, was used to estimate slopes for the treatment and follow-ups periods. The Time 1 variable reflected the time during the treatment period (approximately 15 weeks). The average number of days between pre-treatment and midpoint (64.00 days) was divided by average number of days between pre-treatment and post-treatment (107.36 days). Coding of the follow-up time points was calculated by dividing average number of days between post-treatment and the follow-up time point (3-month follow-up: 104.27 days; 1-year follow-up: 370.57 days) by the average number of days between pre-treatment and post-treatment. Coding Time 2 in this way retained the length of the treatment period as 1 unit of time (see Table 2).
Table 2.
Coding of Time Variables and Expected Value of the Outcome Variable
| Time Point | Pre-treatment | Midpoint | Post-treatment | 3-month follow-up | 1-year follow-up |
|---|---|---|---|---|---|
| Time 1 | 0 | .596 | 1 | 1 | 1 |
| Time 2 | 0 | 0 | 0 | 0.971 | 3.451 |
| Expected Value | π0i | π0i + 0.596π1i | π0i + π1i | π0i + π1i + 0.971π2i | π0i + π1i + 3.451π2i |
Note. π0i = expected anxiety level for subject i at the beginning of the treatment; π1i = expected change in anxiety level for subject i at the end of the treatment; π2i = expected change in anxiety level for subject i for the unit change in time (about 3 months) during the post-treatment period
The unconditional growth model with no level-2 predictors was used to examine the level of variability in the intercept and slopes (i.e., during treatment and slope during follow-up), before adding all level-2 predictors. Backward elimination was used to choose the final model, with non-significant level-2 predictors sequentially deleted (with the predictor with the largest p-value deleted first). Deviance tests were used to compare models in order to ensure that removing the predictor did not cause the model to fit significantly worse. In the final model, variables were retained as predictors of the intercept if they were statistically significant for either the Time 1 slope or the Time 2 slope. In addition to summarizing the coding of Time 1 and Time 2 variables, Table 2 includes the expected value of the dependent variable for participant i at each time point.
Results
All participants had data for all level-2 variables (SRS: M = 82.77, SD = 15.44; VIQ: M = 98.36, SD = 16.10; STAI-T: M = 35.68, SD = 9.28). Table 3 shows anxiety decreased during the treatment period and increased somewhat during the following year. Compared to baseline, paired t-tests indicated that CASI-Anx scores were significantly lower at post-treatment (t(21) = 2.88, p = .009), 3-month follow-up (t(18) = 5.15, p < .001), and 1-year follow-up (t(13) = 2.51, p = .026; Table 3).1
Table 3.
CASI-Anx Descriptive Statistics
| CASI-Anx | |||
|---|---|---|---|
|
| |||
| Timepoint | n | M | SD |
| Pre-treatment | 22 | 17.05 | 9.64 |
| Midpoint | 12 | 15.25 | 10.37 |
| Post-treatment | 22 | 10.77 | 5.76 |
| 3-month follow-up | 19 | 9.47 | 5.35 |
| 1-year follow-up | 14 | 14.43 | 9.36 |
To check the assumption that data were missing at random, we compared baseline characteristics as well as pre-post change scores on the CASI-Anx and all level-2 variables on the 14 participants with 1-year follow-up data to those who did not provide 1-year follow-up data (n = 8). The two groups did not differ on any of these variables (all ps > .39). In the unconditional model, there was a significant amount of variability in the intercept, π0i (estimated variance = 88.50, χ2(19) = 184.79, p < .001), and the Time 1 slope, π1i (estimated variance = 76.00, χ2(19) = 81.03, p < .001), but not the Time 2 slope, π2i (estimated variance = 1.66, χ2(19) = 24.80, p = .167). However, when the Time 2 slope was fixed (i.e., held at the sample average for all participants rather than allowed to vary between participants), model fit was significantly worse (χ2(3) = 12.49, p = .006); therefore, the Time 2 slope was allowed to vary between participants and level-2 predictors were examined.
The full model included VIQ, SRS, and STAI-T as predictors (all grand mean centered). In the final model for these analyses, intercept, Time 1 slope, and Time 2 slope were significant. CASI-Anx scores decreased significantly over the course of treatment. Additionally, SRS predicted the intercept and Time 1 slope; VIQ predicted the Time 1 slope. Adolescents with higher SRS scores had higher pre-treatment CASI-Anx scores. The effects of SRS and VIQ on the Time 1 slope were negative, suggesting that adolescents with higher SRS and VIQ scores improved more during treatment (i.e., their slope was larger in the negative direction). The Time 2 slope was also significant, indicating that anxiety increased during the post-treatment follow up period. In order to examine whether the rebound of anxiety symptoms was strong enough to cancel out the effect of treatment, a Wald test was used to compare the magnitude of the Time 1 slope to the magnitude of the Time 2 slope. For this test, the null hypothesis that anxiety returned to the original level one year after completing the treatment was rejected (estimate of the difference = 4.25, χ2(1) = 10.25, p = .002).
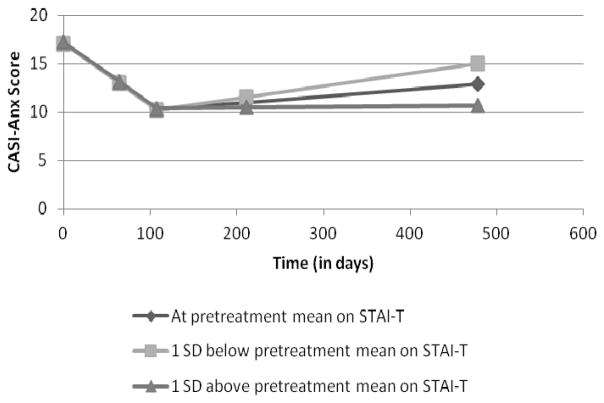
Parental self-report on the STAI-T score was a significant predictor of Time 2 slope. The direction of the effect indicates that adolescents whose parents had higher trait anxiety had less of an increase in anxiety following treatment (i.e., their slope was smaller in the positive direction). The effect of STAI-T score is shown in Figure 2.
Figure 2.
Effect of STAI-T on CASI-Anx scores.
Note: Pre-treatment STAI-T M = 35.68, SD = 9.28
Discussion
Results indicate that targeted CBT can produce sustained reduction in anxiety symptoms in adolescents with ASD. Although there was some increase in anxiety symptoms after treatment ended, anxiety did not return to pre-treatment severity a full year post-treatment. In this high-functioning sample, verbal ability predicted more improvement during treatment. Somewhat unexpectedly, ASD severity, predicted more severe anxiety pre-treatment and greater improvement following treatment. The only significant predictor of change during the follow-up period was higher parental trait anxiety at baseline. The offspring of more anxious parents experienced less of an increase in anxiety after treatment ended.
It may be that those with more severe ASD impairment displayed more anxiety pre-treatment because of pathological synergy (e.g., social disability contributing to anxiety) and were also more receptive to treatment, possibly because of heightened distress. It is also possible that they reaped greater benefit because of the integrated treatment focus on social skills and anxiety in this treatment program, or that there is a shared pathogenesis between the anxiety and ASD. In addition to examining why ASD severity appears to predict course of anxiety in young people with ASD, we need to understand the influence of parental anxiety. The apparent augmenting and sustaining effect of higher parental trait anxiety on treatment effect seen in this sample is contrary to what would be expected based on treatment outcome research in non-ASD youth (e.g., Bodden et al., 2008). Perhaps anxious parents were more invested in the treatment, or were more astute reporters of subtle changes in their children’s behaviors (cf, Conner et al., 2013).
Small sample size and reliance on parent-report outcome measures are the primary limitations. Results from this small, highly selected clinical sample may not generalize to a wider population of youth with ASD and anxiety symptoms. Attrition to the one-year datapoint was considerable, with a final sample size of only 14. Despite the small sample, post-hoc power analyses using G*Power 3.1.3 (Faul, Erdfelder, Lang, & Buchner, 2007) indicated that the power to detect a treatment effect was .87 for a one-tailed paired samples t-test based on the obtained effect size (.61). Power was slightly lower for detecting a significant effect during the post-treatment follow-up period (.56, effect size = .51). Power to detect significant level-2 predictors was lower. Results should be replicated in larger samples. These limitations notwithstanding, results suggest sustained anxiety reduction following CBT in youth with ASD, and intra-individual moderators of treatment response. Identification of factors that predict response to CBT is a step toward establishing individualized, mental health treatments that are not only effective but cost-efficient.
Table 4.
HLM Models
| Variable | Coefficient | T | df | p |
|---|---|---|---|---|
| Unconditional Model | ||||
| Intercept | 17.20 | 8.10 | 21 | <.001 |
| Time 1 Slope | −6.92 | −3.31 | 21 | .003 |
| Time 2 Slope | .77 | 2.10 | 21 | .048 |
|
| ||||
| Full Model | ||||
| Intercept | 17.17 | 10.55 | 18 | <.001 |
| VIQ | .16 | 1.42 | 18 | .173 |
| SRS | .40 | 3.45 | 18 | .003 |
| STAI-T | −.03 | −.15 | 18 | .885 |
| Time 1 Slope | −6.90 | −3.72 | 18 | .002 |
| VIQ | −.20 | −1.84 | 18 | .083 |
| SRS | −.24 | −2.54 | 18 | .020 |
| STAI-T | .04 | .19 | 18 | .853 |
| Time 2 Slope | .73 | 2.33 | 18 | .032 |
| VIQ | .02 | .99 | 18 | .334 |
| SRS | .02 | 1.16 | 18 | .262 |
| STAI-T | −.07 | −1.75 | 18 | .098 |
|
| ||||
| Final Model | ||||
| Intercept | 17.17 | 10.48 | 18 | <.001 |
| VIQ | .11 | 1.94 | 18 | .069 |
| SRS | .36 | 4.39 | 18 | <.001 |
| STAI-T | .00 | .04 | 18 | .966 |
| Time 1 Slope | −6.90 | −3.69 | 19 | .002 |
| VIQ | −.13 | −2.43 | 19 | .025 |
| SRS | −.18 | −2.92 | 19 | .009 |
| Time 2 Slope | .74 | 2.28 | 20 | .034 |
| STAI-T | −.05 | −4.13 | 20 | <.001 |
Footnotes
Paired samples t-tests to examine change during treatment and follow-up were conducted with the fullest available sample (n = 25), including those who received between 5 and 10 individual therapy sessions. Results were similar to those for the n = 22, and indicated that CASI-Anx were significantly lower at post-treatment compared to pre-treatment, t(24) = 3.16, p = .004; at 3-month follow-up, t(18) = 5.15, p < .001; and at 1-year follow-up, t(14) = 2.77, p = .015.
Contributor Information
Susan W. White, Email: sww@vt.edu, Virginia Tech, 109 Williams Hall (0436), Blacksburg, VA 24060
Amie R. Schry, Email: aschry@vt.edu, Virginia Tech, 109 Williams Hall (0436), Blacksburg, VA 24060
Yasuo Miyazaki, Email: yasuom@vt.edu, Virginia Tech, 109 Williams Hall (0436), Blacksburg, VA 24060.
Thomas H. Ollendick, Email: tho@vt.edu, Virginia Tech, 109 Williams Hall (0436), Blacksburg, VA 24060
Lawrence Scahill, Email: lawrence.scahill@emory.edu, Emory University, Atlanta, GA.
References
- Bodden D, Bogels S, Nauta MH, Haan ED, Ringrose J, Appelboom C, Appelboom-Geerts K. Child versus family cognitive-behavioral therapy in clinically anxious youth: An efficacy and partial effectiveness study. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47(12):1384–1394. doi: 10.1097/CHI.0b013e318189148e. [DOI] [PubMed] [Google Scholar]
- Conner CM, Maddox BB, White SW. Parents’ state and trait anxiety: Relationships with anxiety and treatment response in adolescents with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2012 doi: 10.1007/s10803-012-1728-0. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Constantino JN, Gruber CP. Social Responsiveness Scale (SRS) Los Angeles, CA: Western Psychological Services; 2005. [Google Scholar]
- Eaves LC, Ho HH. Young adult outcome of autism spectrum disorders. Journal of Autism and Developmental Disorders. 2008;38:739–747. doi: 10.1007/s10803-007-0441-x. [DOI] [PubMed] [Google Scholar]
- Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: A flexible statistical power analysis for the social, behavioral, and biomedical sciences. Behavior Research Methods. 2007;39:175–191. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- Gabriels RL, Hill DE, Pierce RA, Rogers SJ, Wehner B. Predictors of treatment outcome in young children with autism: A retrospective study. Autism. 2001;5:407–429. doi: 10.1177/1362361301005004006. [DOI] [PubMed] [Google Scholar]
- Gadow KD, Sprafkin J. Adolescent symptom inventory-4 screening manual. Stony Brook, NY: Checkmate Plus; 1997. [Google Scholar]
- Gadow KD, Sprafkin J. Adolescent symptom inventory-4 norms manual. Stony Brook, NY: Checkmate Plus; 1998. [Google Scholar]
- Hallett V, Lecavalier L, Sukhodolsky DG, Cipriano N, Aman MG, McCracken JT, Scahill L. Exploring the manifestations of anxiety in children with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2013 doi: 10.1007/s10803-013-1775-1. Early online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamer RM, Simpson PM. Last observation carried forward versus mixed models in the analysis of psychiatric clinical trials. American Journal of Psychiatry. 2009;166(6):639–641. doi: 10.1176/appi.ajp.2009.09040458. [DOI] [PubMed] [Google Scholar]
- Hirshfeld-Becker DR, Micco JA, Simoes NA, Henin A. High risk studies and developmental antecedents of anxiety disorders. American Journal of Medical Genetics, Part C (Seminars in Medical Genetics) 2008;148C:99–117. doi: 10.1002/ajmg.c.30170. [DOI] [PubMed] [Google Scholar]
- Howlin P, Mawhood L, Rutter M. Autism and developmental receptive language disorder – a follow-up comparison in early adult life. II: Social, behavioural, and psychiatric outcomes. Journal of Child Psychology and Psychiatry. 2000;41(5):561–578. doi: 10.1111/1469-7610.00643. [DOI] [PubMed] [Google Scholar]
- Hox JJ. Multilevel analysis: Techniques and applications. 2. New York, NY: Routledge; 2010. [Google Scholar]
- Kleinhans NM, Richards T, Weaver K, Johnson LC, Greenson J, Dawson G, Aylward E. Association between amygdala response to emotional faces and social anxiety in autism spectrum disorders. Neuropsychologia. 2010;48(12):3665–70. doi: 10.1016/j.neuropsychologia.2010.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraemer HC, Kiernan M, Essex M, Kupfer DJ. How and why criteria defining moderators and mediators differ between the Baron & Kenny and MacArthur approaches. Health Psychology. 2008;27(2) doi: 10.1037/0278-6133.27.2(Suppl.).S101. S101-D1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraemer HC, Thiemann S. A strategy to use soft data effectively in randomized controlled clinical trials. Journal of Consulting and Clinical Psychology. 1989;57(1):148–154. doi: 10.1037//0022-006x.57.1.148. [DOI] [PubMed] [Google Scholar]
- Lickel A, MacLean WE, Blakeley-Smith A, Hepburn S. Assessment of the prerequisite skills for cognitive behavioral therapy in children with and without autism spectrum disorders. Journal of Autism and Developmental Disorders. 2012;42:992–1000. doi: 10.1007/s10803-011-1330-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord C, Rutter M, DiLavore PC, Risi S. Autism Diagnostic Observation Schedule. Los Angeles: Western Psychological Services; 2002. [Google Scholar]
- Lord C, Rutter M, Le Couteur A. Autism Diagnostic Interview—Revised: A revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. Journal of Autism and Developmental Disorders. 1994;24(5):659–685. doi: 10.1007/BF02172145. [DOI] [PubMed] [Google Scholar]
- Lord C, Wagner A, Rogers S, Szatmari P, Aman M, Charman T, Yoder P. Challenges in evaluating psychosocial interventions for autistic spectrum disorders. Journal of Autism and Developmental Disorders. 2005;35:695–708. doi: 10.1007/s10803-005-0017-6. [DOI] [PubMed] [Google Scholar]
- Mazefsky CA, White SW. Adults with autism. In: Rogers SJ, editor. Handbook of Autism Spectrum Disorders. 4. Hoboken, NJ: Wiley and Sons; (in press) [Google Scholar]
- Olatunji BO, Ciesielski BG, Wolitzky-Taylor KB, Wentworth BJ, Viar MA. Effects of experienced disgust on habituation during repeated exposure to threat-relevant stimuli in blood-injection-injury phobia. Behavior Therapy. 2012;43:132–141. doi: 10.1016/j.beth.2011.04.002. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and data analysis methods. 2. Thousand Oaks, CA: SAGE Publications; 2002. [Google Scholar]
- Raudenbush S, Bryk A, Congdon R. HLM for Windows (Version 7.01) [Computer software] Skokie, IL: Scientific Software International, Inc; 2012. [Google Scholar]
- Reaven J, Blakeley-Smith A, Culhane-Shelburne K, Hepburn S. Group cognitive behavior therapy for children with high-functioning autism spectrum disorders and anxiety: A randomized trial. The Journal of Child Psychology and Psychiatry. 2012;53(4):410–419. doi: 10.1111/j.1469-7610.2011.02486.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seligman LD, Ollendick TH. Cognitive Behavior Therapy for anxiety disorders in children and adolescents. Psychiatric Clinics of North America. 2011;20:217–238. doi: 10.1016/j.chc.2011.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman WK, Albano AM. Anxiety Disorders Interview Schedule for DSM-IV. San Antonio, TX: The Psychological Corporation; 1996. [Google Scholar]
- Silverman WK, Saavedra LM, Pina AA. Test-retest reliability of anxiety symptoms and diagnoses with anxiety disorders interview schedule for DSM-IV: Child and parent versions. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40(8):937–944. doi: 10.1097/00004583-200108000-00016. [DOI] [PubMed] [Google Scholar]
- Spielberger CD, Gorssuch RL, Lushene PR, Vagg PR, Jacobs G. Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press, Inc; 1983. [Google Scholar]
- Sterling L, Dawson G, Estes A, Greenson J. Characteristics associated with presence of depressive symptoms in adults with autism spectrum disorder. Journal of Autism and Developmental Disorders. 2008;38:1011–1018. doi: 10.1007/s10803-007-0477-y. [DOI] [PubMed] [Google Scholar]
- Sukhodolsky DG, Scahill L, Gadow KD, Arnold E, Aman MG, McDougle CJ, Vitiello B. Parent-rated anxiety symptoms in children with pervasive developmental disorders: Frequency and association with core autism symptoms and cognitive functioning. Journal of Abnormal Child Psychology. 2008;36:117–128. doi: 10.1007/s10802-007-9165-9. [DOI] [PubMed] [Google Scholar]
- Taylor JL, Seltzer MM. Changes in the autism behavioral phenotype during the transition to adulthood. Journal of Autism and Developmental Disorders. 2010;40:1431–1446. doi: 10.1007/s10803-010-1005-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Steensel FJA, Bogels SM, Perrin S. Anxiety disorders in children and adolescents with autistic spectrum disorders: A meta-analysis. Clinical Child and Family Psychology Review. 2011;14:302–317. doi: 10.1007/s10567-011-0097-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White SW, Albano A, Johnson C, Kasari C, Ollendick T, Klin A, et al. Development of a cognitive-behavioral intervention program to treat anxiety and social deficits in teens with high-functioning autism. Clinical Child and Family Psychology Review. 2010;13(1):77–90. doi: 10.1007/s10567-009-0062-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White SW, Ollendick T, Albano A, Oswald D, Johnson C, Southam-Gerow MA, Scahill L. Randomized controlled trial: Multimodal anxiety and social skill intervention for adolescents with autism spectrum disorder. Journal of Autism and Developmental Disorders. 2013;43(2):382–394. doi: 10.1007/s10803-012-1577-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White SW, Ollendick T, Scahill L, Oswald D, Albano A. Preliminary efficacy of a cognitive-behavioral treatment program for anxious youth with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2009;39:1652–1662. doi: 10.1007/s10803-009-0801-9. [DOI] [PMC free article] [PubMed] [Google Scholar]