Abstract
Despite the fact that more breast cancer survivors are currently enjoying longer lifespans, there remains limited knowledge about the factors and issues that are of greatest significance for these survivors, particularly from their perspectives. This review was based on the concept that the topics addressed should focus on the perspectives of current survivors and should be extended to future modalities, which physicians will be able to use to gain a better understanding of the hidden needs of these patients. We intended to choose and review dimensions other than the pathology and the disease process that could have been overlooked during treatment. The eight topics upon which we focused included: delay of treatment and survival outcome; sexual well-being; concerns about childbearing; tailored follow-up; presence of a family history of breast cancer; diet and physical activity for survivors and their families; qualitative approach toward understanding of breast cancer survivorship, and; mobile health care for breast cancer survivors. Through this review, we aimed to examine the present clinical basis of the central issues noted from the survivors' perspectives and suggest a direction for future survivorship-related research.
Keywords: Breast neoplasms, Quality of life, Survivors
INTRODUCTION
Although definitions of the term vary, a frequently cited definition of cancer survivor is the following: An individual is considered a cancer survivor from the time of diagnosis, through the balance of his or her life. Family members, friends, and caregivers are also impacted by the survivorship experience and are therefore included in this definition of cancer survivor [1,2]. Despite the dramatic improvements in cancer diagnostics and treatments, many cancer survivors continue to feel that they have no source to turn to when they need appropriate solutions or supports for a broad range of survivorship issues encountered throughout the period following the diagnosis. A better understanding of the unique needs of the growing population of cancer survivors can be promoted by patient-centered approaches and a new focus on downstream data collection for the identification of possible complications and late effects [3].
To understand dimensions other than the pathology and the disease process that physicians could have overlooked during treatment, we presented the following questions to breast cancer survivors: What was most difficult for you since the diagnosis of breast cancer? What did you feel was the most deficient in the current treatment and care process of breast cancer? As a survivor, what type of service would you like health care providers to offer? In terms of the value of a qualitative approach, which is discussed in detail in the section "Qualitative approach toward understanding of breast cancer survivorship," we believed this would be a pragmatic first step to choose focused topics from among a wide range of survivorship issues. The summarized transcript of the interview with survivors is shown in Appendix 1 and 2.
Six focused reviews about the survivorship issues upon which we concentrated, based on current survivors' perspectives of the patient experience from diagnosis through treatment to the stage of routine follow-ups, are presented in the following sections. In addition, the utility of qualitative approaches and the emerging potential of smart phones are addressed as complementary modalities for collection of the downstream data, which survivors should be encouraged to report.
Through this review, we aimed to examine the present clinical basis of the central issues noted from the survivors' perspectives and suggest a direction for future survivorship-related research.
DELAY OF TREATMENT AND SURVIVAL OUTCOME
In cancer care, initiation of definitive treatment is often delayed owing to a variety of patient, provider, and health system factors. The patient-related delay time is the time between the onset of the first symptoms and the first medical visit, the system-related delay time is the time between the first medical visit and the start of therapy, and the total delay time is considered the sum of the abovementioned delay times. Treatment delays following the diagnosis of breast cancer, specifically, cause significant psychosocial distress to patients, and in addition, breast cancer patients often associate time delay with adverse oncologic outcomes and survival. A recent retrospective study based on Korea Central Cancer Registry and National Health Insurance (NHI) data reported that 13.6% of 147,682 patients who underwent definitive surgery for any of six cancers in Korea waited >31 days from diagnosis to surgery [4]. In another report, also based on the NHI data, the median time from breast cancer diagnosis to surgery was 14 days, and the proportion of breast cancer patients who had undergone surgery within 4 weeks of the diagnosis of cancer was 74.1% [5]. In the United States, a study based on the National Cancer Data Base demonstrated that the time to treatment for breast cancer increased from 17 days (median) in the period from 1995-1997 to 23 days (median) in 2003-2005 [6].
The impact of treatment delay on survival is still uncertain, and the acceptable time interval from diagnosis of breast cancer to initiation of treatment remains controversial. In Korea, two retrospective studies demonstrated a negative impact of delay of surgical treatment on patients' survival outcomes. Yun et al. [4] and Shin et al. [5] reported that treatment delays of >1 month or 12 weeks, respectively, were associated with worse survival outcomes for breast cancer patients (adjusted hazard ratio [aHR], 1.59; 95% confidence interval [CI], 1.37-1.84 and aHR, 1.91; 95% CI, 1.06-3.49, respectively). Likewise, in the United States, a recent retrospective study on young breast cancer patients aged 15 to 39 years reported similar outcomes: the 5-year survival rate in women who were treated via surgery and had a treatment delay time >6 weeks was 80% compared with a rate of 90% among those with a treatment delay time of <2 weeks (p=0.005) [7]. Interestingly, Vujovic et al. [8] suggested that an interval of >12 weeks to breast surgery might be associated with decreased survival for mammographic presentation, but it appeared to have no effect on the survival of patients presenting with a palpable breast lump. This suggests that for patients with palpable lumps, if metastasis is to occur, it will have already taken place by the time a breast lump is detected. On the other hand, several other studies have suggested that there is no significant impact of surgical treatment time delay on patients' survival outcomes [9,10,11].
It is also uncertain whether treatment delay of postoperative adjuvant therapy, such as radiotherapy and chemotherapy, affects the survival outcomes of breast cancer patients. There are several retrospective studies on radiotherapy that assessed the time interval between breast-conserving surgery and the start of adjuvant radiotherapy, as well as its impact on survival and local recurrence. In Korea, early radiotherapy, within 6 weeks after breast-conserving surgery, was reported to be associated with increased local control [12]. However, other retrospective studies have reported contradictory findings on local recurrence and survival [13,14]. In chemotherapy, immediate reconstruction, re-excision, and use of the 21-gene assay have been identified as factors associated with chemotherapy delay, but, as with reports on adjuvant radiotherapy or surgery, the impact of a delay in chemotherapy has not been confirmed [15,16].
Since the current data available on treatment time delay are limited and retrospective, there is no definitive conclusion on the acceptable wait time and its impact on survival outcome. Treatment delay is not an issue that can be discussed prospectively; therefore, it is difficult to arrive at a consensus on this matter. Studies which supported a negative survival impact of surgical treatment delay suggested 12 weeks, 6 weeks, or 4 weeks as an acceptable wait time. It is difficult to generalize these retrospective findings to diverse clinical settings; however, considering that >70% of Korean breast cancer patients undergo initial treatment within 1 month, with a median wait time of 14 days, treatment delay may not be a major negative prognostic factor in the current clinical settings. Furthermore, it is crucial that clinicians interpret these findings carefully for breast cancer patients in order to further reduce psychosocial distress among patients.
SEXUAL WELL-BEING
Sexuality is a basic and important domain of quality of life (QoL) for humans. Sexual dysfunction has a significant impact on the physical, psychological, and social QoL of breast cancer survivors. The sexuality of breast cancer survivors is affected by physiological as well as psychological effects of oncologic treatment [17], and consequently, sexual dysfunction consists of a wide spectrum of issues including physiological, psychological, physical, and interrelational problems [18].
Sexual dysfunction may result from oncologic treatment for breast cancer such as surgery, radiation, chemotherapy, and antiestrogen therapy. In addition, the distress of breast cancer survivors or their partners can damage a person's healthy sexuality [19]. Loss of sexual self-image, loss of nipple sensitivity, and scarring can occur after breast cancer surgery. Although some problems gradually diminish over time, some breast cancer survivors still report problems several years after surgery. Radiation therapy can result in skin fibrosis, loss of sexual sensitivity of the skin, fatigue, and general malaise, thereby negatively impacting sexual desire and response. Chemotherapy is a major determinant of sexual dysfunction and affects all phases of the sexual response cycle [20]. Cytotoxic chemotherapy, besides inducing amenorrhea and ovarian failure, also causes alopecia, alterations in nail color, and weight changes, thereby affecting the survivors' sexual self-concept and consequently their sexual interactions. Various antiestrogen treatments have similar effects on sexual functions, such as vaginal dryness, subsequent dyspareunia, and decreased sexual desire. Many survivors experience a persistent depressed mood and sadness following the diagnosis of breast cancer, even after successful treatment, due to the fear of treatment, body image concerns, fear of recurrence, and fear related to changes in the relationships with their spouse and family [21]. Although sexual dysfunction can result directly from breast cancer and its treatment, issues that are unrelated to breast cancer, such as medical conditions, psychosocial status, and premorbid sexual dysfunction, which may exacerbate or attenuate sexual dysfunction, may also be important factors.
Because young breast cancer survivors are generally more sexually active, the risk of sexual dysfunction is of great importance to them [22]. In addition, young breast cancer survivors seem to have a worse QoL and are more vulnerable to the negative effects of the disease than the older survivors [23]. There are many therapeutic options for sexual dysfunction, including hormonal agents, dilator therapy, lubricants, medications for depression or anxiety, sex therapy, education on sexual intercourse, and counseling for the survivor or partner [18,24]. However, a comprehensive review of management of sexual dysfunction in breast cancer survivors shows that confirmatory evidence of the benefit of the available treatment options is lacking.
Recent advances in breast cancer screening and treatment have led to increased survival rates. Consequently, the number of breast cancer survivors who experience long-term sexual adverse effects and seek help for these issues may be expected to increase. Moreover, the sexuality of breast cancer survivors is complex with an inherent wide spectrum of problems. For the sexual well-being of breast cancer survivors, all members of the oncology team must employ approaches tailored to each individual breast cancer survivor. Hence, multidisciplinary team members should focus on research regarding the sexual well-being of breast cancer survivors.
CONCERNS ABOUT CHILDBEARING
Young breast cancer survivors frequently have concerns about childbearing issues including fertility and pregnancy. However, they do not obtain adequate information regarding these issues from their clinicians, and it remains controversial whether pregnancy is safe for breast cancer survivors [25,26]. Pregnancy has been considered harmful to breast cancer survivors, because they could be exposed to high levels of ovarian hormones during pregnancy [27]. However, several studies have shown that pregnancy does not increase breast cancer recurrence and even leads to a favorable prognosis [28,29]. A meta-analysis of 14 studies also demonstrated that pregnancy could decrease breast cancer-related death [28].
Regarding the appropriate timing of pregnancy, previous available studies reported that early pregnancy, within 2 years of diagnosis, did not affect breast cancer recurrence, although most breast oncologists have recommended that breast cancer survivors should wait for at least 2 years from diagnosis [30,31]. In addition, systemic treatments are also taken into consideration for the optimal timing of pregnancy. Young breast cancer survivors should delay their pregnancy for at least 6 months after chemotherapy, and for at least 2 months after antiestrogen treatment [32]. Chemotherapy-induced amenorrhea has been known to be a predictor of infertility, and this is affected by the chemotherapeutic regimen, number of chemotherapy cycles, cumulative dose (particularly the dose of cyclophosphamide), and the patient's age at treatment [33,34]. However, the impact of antiestrogen treatment and radiotherapy on infertility is still controversial [35,36].
Embryo and oocyte cryopreservation are established fertility preservation methods [37]. Because ovarian stimulation could result in a significant increase in estradiol levels and a significant delay of chemotherapy, breast oncologists should refer all potential patients to the appropriate reproductive endocrinologist to ensure that the patients receive sufficient information and to avoid treatment delays [38]. Other fertility preservation methods such as ovarian tissue cryopreservation and transplantation could be considered, but the effectiveness of these methods remains controversial [39,40,41].
As the numbers of young breast cancer survivors and their survival times have increased, it has become increasingly necessary to keep these issues of fertility and childbearing in mind in the treatment of breast cancer patients. In addition, individualized decision-making, with the assistance of a multidisciplinary team, should be recommended regarding the optimal timing of pregnancy and the available fertility preservation methods.
TAILORED FOLLOW-UP
Follow-up after primary treatment for breast cancer is an important component of the care of survivors. Routine follow-up aims at monitoring the adverse effects of primary treatment and providing psychosocial care. Another prominent goal is the early recognition and treatment of potentially curable disease recurrence. Early detection of second primary breast cancer or locoregional recurrence is beneficial for survival [42]. However, routine testing for distant metastasis provides no benefit for survival or health-related QoL [43]. Randomized controlled trials have found that reduced follow-up strategies did not negatively affect patient outcomes or early detection of recurrence, and more intensive follow-up was associated with higher costs without differences in early detection of relapses [44,45].
Since the American Society of Clinical Oncology published an evidence-based clinical practice guideline on breast cancer follow-up in 1997, multiple international guidelines have been published for the surveillance of breast cancer survivors [46]. These guidelines recommend a minimal clinical follow-up including routine history and physical examination and regularly scheduled mammography (MMG). However, these guidelines are not stratified on the basis of cancer stage or tumor biology, and there is no agreement on the optimal frequency or duration of follow-up modes. The Korean Breast Cancer Society (KBCS) guidelines recommend that history taking and physical examinations should be performed every 3 months for the first 2 years, every 6 months for years 3-5, and annually thereafter. MMG should be performed every 12 months. Assessment with complete blood counts, chemistry panels, and tumor markers is recommended every 6 months for 5 years. Further, annual chest radiography should be performed for 5 years. Gynecologic examinations are recommended for women receiving tamoxifen; regular bone mineral density examinations are recommended for women receiving aromatase inhibitors. Bone scintigraphy, liver ultrasonography, computed tomography, positron emission tomography, and magnetic resonance imaging are not recommended for routine follow-up in an otherwise asymptomatic patient with no specific findings on clinical examination.
Despite the lack of evidence supporting routine follow-up testing other than MMG for breast cancer survivors and the presence of recommendations against its use, follow-up testing is performed by many physicians under the assumption that detecting and treating recurrences early results in better outcomes [47]. Moreover, although routine follow-up visits are very stressful for patients attending them, many survivors may favor surveillance that is more intensive, and may overestimate the value of laboratory and imaging studies. Follow-up tests themselves may cause psychosocial and physical harm in healthy survivors owing to false-positive findings, unnecessary investigations, and overtreatment. Little is known about current actual practice patterns of physicians-do they adhere to or deviate from guideline recommendations? Therefore, we devised a plan to evaluate the current follow-up patterns of experienced physicians who provide care for breast cancer patients and monitor them after treatment. We created a survey instrument to accomplish this and chose KBCS members as survey participants, and we are aiming to announce the results by the end of 2014. Additionally, further research is needed to determine the comparative effectiveness of different modes of breast cancer surveillance and the ideal frequency and duration of follow-up.
PRESENCE OF A FAMILY HISTORY OF BREAST CANCER
Breast cancer survivors face problems regarding family members, including the fear of being cheated on by the husband, feeling sorry for what may be their decreased ability to spend time with or care for their children, and feeling guilty owing to their children's potential inheritance of their disease. Considering that the incidence of breast cancer peaks in the late 40s among the Korean population [48], many sexually active breast cancer survivors face sexual problems with their spouse, and this can be of great significance. In addition, relatively young breast cancer survivors may feel responsible as mothers for providing support such as education, caring, and companionship to their young children. However, above all, breast cancer survivors who are parents experience unbearable distress due to the concept that their children might develop the same disease someday.
Genetic predisposition is, of course, one of the most important risk factors for breast cancer and accounts for 5% to 10% of all breast cancers [49]. To date, five high-penetrance genes (BRCA1, BRCA2, TP53, PTEN, and LKB1), four intermediate-penetrance genes (ATM, BRIP1, CHEK2, and PALB2), and various low-penetrance loci (rs3803662, rs889312, rs3817198, and rs13281615) have been discovered [50]. Among those, approximately 50% to 70% of the hereditary breast cancers are caused by BRCA1/2 gene mutations [51]. BRCA1/2 mutations are present in 12.7% of the high-risk patients as compared with 2.8% of unselected patients. Not all carriers of BRCA1/2 mutations develop breast cancer, but the penetrance for breast cancer has been reported to be as high as approximately 70% in BRCA1 mutation carriers and 60% in BRCA2 mutation carriers in their lifetime [52].
The majority of breast cancer survivors suffer from misconceptions regarding the genetic implications of having a breast cancer patient in their family. More than 10% of the probability of harboring the BRCA1/2 gene mutation can be reasonably suspected, and genetic counseling should be provided for high-risk breast cancer survivors with the following: young age (<40 years) at diagnosis, bilateral breast cancer, multiple organ cancer, or male breast cancer [53]. According to the results from the Korean Hereditary Breast Cancer Study, although the overall prevalence of the BRCA mutation among familial breast cancer survivors was 21.7% (BRCA1, 9.3% and BRCA2, 12.4%), the prevalence of the BRCA mutations among subgroups that had two breast cancer survivors in a family, with both survivors aged >50 years at diagnosis, was only 4.1% [54]. Currently, genetic counseling is routinely recommended to all newly diagnosed women who have a family history of at least one relative with breast cancer at any age of diagnosis, but such counseling needs to be tailored considering the proband age at diagnosis.
The misunderstanding that children of mothers with breast cancer will inevitably develop the disease should be resolved to reduce unnecessary guilt among mothers and diminish the exaggerated possibility of inheritance.
DIET AND PHYSICAL ACTIVITY FOR SURVIVORS AND THEIR FAMILY
Breast cancer patients and their families tend to be particularly careful about their diets and their use of supplements; however, little is known about the association between dietary factors and breast cancer prognosis among breast cancer patients. Although breast cancer prevention and etiology studies have long provided information on dietary modification strategies for cancer prevention, research on diet for breast cancer survivors is relatively limited, partly because changes in diet and the use of supplements have been considered relative to therapeutics, stage/grade, hormone receptor status, and other prognostic factors.
Two large intervention trials [55,56] and a few prospective studies [57,58,59,60,61,62,63] analyzed the effect of diet on breast cancer prognosis, and the evidence from studies on diet and food choices for breast cancer patients is increasing, but is not yet conclusive. A healthy dietary pattern, including high consumption of fruits and vegetables, whole grain, poultry, and fish, has been examined in a few epidemiologic studies [57,58, 64,65] and was found to be associated with a lower risk of breast cancer recurrence or death. Recent prospective studies have reported that consumption of fruits and vegetables and dietary components that are abundant in fruits and vegetables, such as carotenoid and dietary fiber, improves breast cancer prognosis [59,66]. However, intensive counseling intervention promoting high consumption of vegetables, fruits, and fiber and low consumption of fat did not reduce the risk of breast cancer recurrence or mortality during a 7.3-year follow-up period among women with early breast cancer in the Women's Healthy Eating and Living Study [56]. Cancer patients were more likely to use dietary supplements than the general population in the United States [67], and a similar pattern was observed in Korea. However, results from prospective cohort studies are not conclusive [68,69] and warrant additional prospective studies to examine the effect of such supplements on breast cancer prognosis.
The Women's Intervention Nutrition Study found that a low-fat diet reduced the risk of recurrence among postmenopausal breast cancer survivors, especially women with estrogen receptor-negative tumors [55]. High intake of saturated fat or trans fats was found to increase the risk of death from any cause in the Collaborative Women's Longevity Study [60]. A recent review of five cohort studies examining soy products and breast cancer survival reported that soy product intake was associated with better survival and lower risk of recurrence [70]. The vitamin D status may be also important with regard to breast cancer risk and survival. It has been hypothesized that a low vitamin D status worsens breast cancer prognosis; however, the current studies provide contradictory evidence [71,72].
On the basis of the current findings from existing prospective or intervention studies, physical activity is the most well-established lifestyle factor associated with breast cancer survival among breast cancer patients. A recent large collaborative work of four cohort studies including 13,302 breast cancer patients, the After Breast Cancer Pooling Project, suggested that breast cancer survivors who met the physical activity guidelines from the U.S. Department of Health and Human Services of 10 metabolic equivalent-hours/week for 18 to 48 months postdiagnosis had a lower risk of death [73].
In the Asian population, including Korea, China, and Japan, an increase of >100% in breast cancer mortality has been observed from the 1970s to the present [74], clearly suggesting a relationship between lifestyle factors and breast cancer progression. Additionally, a progressive improvement in overall breast cancer survival during the past decades has led to increased interest in the effect of diet and exercise on breast cancer prognosis. Although the current evidence is insufficient to provide health professionals and patients with specific and detailed guidelines, a healthy diet high in fruits, vegetables, and soy products and low in fat seems to be important for breast cancer patients. However, it is still unclear whether any specific dietary component can influence breast cancer prognosis. In addition, current evidence largely arises from Western studies, where postmenopausal breast cancer is more common than premenopausal breast cancer and the proportion of overweight or obesity in breast cancer patients is greater than that among Korean breast cancer patients. Therefore, the lifestyle factors that improve breast cancer prognosis should be explored in the Korean population specifically. Regarding physical activity, considering the evidence accumulated over the past decades, breast cancer patients can be counseled to increase or maintain a moderate level of physical activity.
QUALITATIVE APPROACH TOWARD UNDERSTANDING OF BREAST CANCER SURVIVORSHIP
With the growing number of breast cancer survivors, ensuring the overall health of these individuals by providing the optimal health care services is proving to be a challenge for health care professionals. Breast cancer survivors have numerous medical and psychosocial concerns or needs that must be addressed in the posttreatment period [75]. Therefore, it is necessary to understand their experience from their point of view, and a qualitative method serves this purpose. Not surprisingly, qualitative research methods are gaining popularity in medicine and health care fields, and an increasing number of qualitative studies are being published in medical journals [76].
Qualitative methods aim to understand phenomena in a naturalistic environment and from the participant's perspective rather than an outside perspective [77]. Aimed at understanding how the survivorship shapes the experience of breast cancer, qualitative methods emphasize the meanings and views of all the participants [78]. Quantitative and qualitative methods are complementary but each has its own theoretical and methodological assumptions. The quantitative method is variable-oriented, whereas the qualitative method is case-oriented [79]. Their differences are well summarized by Camic, Rhodes, and Yardley in the following description: "Quantitative research as the process of producing a map of a place and qualitative research as the process of producing a video of that place." Although a map is unable to convey an understanding of what it is like to be at a place, a video conveys vivid and subjective experiences of being in that position [80].
Qualitative methods provide significant contributions to the understanding of breast cancer survivorship. These methods help us understand the needs of the under-represented or under-researched individuals and stimulate theory development, allowing unknown or novel phenomena to be later tested using quantitative methods. Qualitative methods also help to explain mechanisms underlying relationships among variables found in quantitative results [81]. Generally, qualitative methods are particularly suitable for research questions regarding experiences, thoughts, perceptions, expectations, motives, and attitudes [82]. For instance, breast cancer survivors' perceptions and attitudes about their healthcare utilization, screening, and information needs were previously explored via a qualitative approach [83]. Further, the experience of transitioning from a patient to a survivor was previously explored in a longitudinal qualitative 2-year follow-up study of survivors [84]. Delicate sequelae issues such as fertility [85] and sexual concerns [86], and breast cancer patients' perceptions of and attitudes toward the adverse effects of chemotherapy such as alopecia [87] have also been explored via qualitative means.
Qualitative research methods have been found to be a useful means for the development of QoL instruments [82] and complement the shortcomings of objective QoL instruments [88]. Owing to the subjective nature of the QoL, the impact of breast cancer and its treatment cannot be fully understood using predetermined scales, and important issues that patients experience are overlooked [89]. In fact, QoL issues and needs in a minority population have been popular topics of qualitative methods in the literature on breast cancer survivorship [90,91,92]. A prominent concern among cancer survivors is the fear of recurrence, and the approach that breast cancer survivors use to deal with this issue was reported on the basis of in-depth interviews [93]. Communication issues, such as the patients' view of how doctors should communicate with them, have also been addressed via qualitative approaches in breast cancer [94,95]. Qualitative research methods have additionally been applied to the understanding of health behaviors among survivors, because an understanding of why survivors behave as they do is crucial for any positive change [96]. For instance, in a large-scale qualitative study, identifying psychological, physical, and contextual and environmental barriers, Hefferon et al. [97] aimed to explore the perceived barriers to exercise implementation 5 years after breast cancer diagnosis. Similarly, Miedema and Easley [98] used qualitative methods to examine barriers to rehabilitative care for young breast cancer survivors.
To understand how a survivorship care plan created by oncologists could improve the quality of survivorship care, focus group interviews were conducted to assess the perspectives of survivors and health care professionals [75]. A qualitative method can be also useful for exploring the experiences of participants in clinical trials. For example, Nelson et al. [99] examined the experiences of participants in the National Cancer Research Institute ZICE clinical trial, a randomized trial assessing two types of bisphosphonate treatment in breast cancer patients with bone metastases.
Despite the potential of qualitative methods to record breast cancer survivors' experiences while allowing for individuality and subjectivity, these methods have issues with reliability and validity which must be improved [96]. Quantitative and qualitative approaches should be seen as complementary methods, and not as opposites. In fact, these two methods can be successfully combined into a mixed approach toward a systematic and objective, yet broader, deeper, and also subjective understanding of the issues of breast cancer survivorship. Qualitative methods can be preliminary to quantitative research, supplement it, and explore complex phenomena or issues that quantitative methods cannot resolve [78,82].
MOBILE HEALTH CARE FOR BREAST CANCER SURVIVORS
Electronic health (eHealth) can be defined as the practice of medicine and public health using information and communication technology (ICT) devices such as computers, mobile phones, and satellite communications [100]. The term mobile health (mHealth) refers to a subsegment of eHealth and is now used when the practice involves wireless communications, especially mobile or smart phones, the penetration of which amounts to over 70% (as of 2013) in the United Arab Emirates, South Korea, Saudi Arabia, and Singapore.
In recent years, the Cochrane Collaboration has provided substantial evidence from systematic reviews to advocate the effectiveness of mobile phone-based clinical applications among patients with chronic health problems including psychiatric disorders and human immunodeficiency virus (HIV) infection. Computer-based diabetes self-management interventions to manage type 2 diabetes mellitus had a small beneficial effect on blood glucose control, but the effect was larger in the mobile phone subgroup [101]. Under some conditions, short message service and multimedia message service have been reported to have a positive impact on the health status of patients with diabetes mellitus, hypertension, and asthma and on their ability to self-manage their conditions [102]. For short-term prescriptions for diverse medical problems, several simple interventions increased adherence to medication and improved outcomes; however, for long-term treatments, no simple intervention and only a few complex interventions led to improvements in health outcomes [103]. The use of telephone voice interventions may play a role in improving medication adherence, reducing risky sexual behavior, and reducing depressive and psychiatric symptoms in patients with HIV infection [104]. A meta-analysis that studied health behavior outcomes of healthy populations showed that strategies with mobile communications that aimed at smoking cessation increase the long-term quit rates compared with control programs (relative risk, 1.71; 95% CI, 1.47-1.99; over 9,000 participants) [105] and promote enrollment of smokers into cessation programs (participants enrolled: 0% in the control group; 1.3% in the postcard group; and 20.6% in the telephone call group) [106].
Currently, studies addressing the use of mobile technologies to promote a new era of healthcare, especially in the management of cancer survivors, are few. The noteworthy feature of mHealth is the feasibility of the use of mobile phones to assist in the collection of data on disease-related vital signs [107], treatment-related adverse effects [108], and a possibly comprehensive psychological status [109]. According to a recent randomized trial of interactive social networking sites, Facebook-based intervention may help cancer survivors receive health information and support that promotes physical activity and other health behaviors [110]. Since physical activity is the most well-established positive lifestyle factor among breast cancer survivors, and its beneficial effects are more pronounced with moderate or vigorous intensity compared to mild intensity [111], this mobile phone-based intervention may improve disease outcomes as well as related QoL among breast cancer survivors. Although there are important concerns about the use of mobile phones for health-related purposes, such as the risk of "driving while texting" or "brain tumors" [112], studies assessing the value of incorporating mobile phone-based health applications into breast cancer survivors' care are being conducted.
CONCLUSION: WHAT THE FUTURE HOLDS
Since cancer has the potential to affect every aspect of the survivor's life, including the physical, psychological, social, economic, and existential or spiritual aspects [113], a comprehensive and multidisciplinary approach should be considered for breast cancer survivorship research. Our cancer survivorship research focuses on the etiology and prevention of breast cancer, management of treatment-related adverse effects, lifestyle modification, and QoL issues to optimize the physiologic, psychosocial, and functional outcomes for breast cancer survivors. To achieve the ultimate goals of reducing the cancer burden and providing guidance for survivors, understanding the integration and interaction of multidisciplinary research domains is of prime importance. To date, however, most survivorship research has been performed in a fragmented fashion, and an evidence-based comprehensive framework for survivorship research has yet to be established.
Owing to the ongoing evolution of novel breast cancer therapies, it is essential for clinicians to understand both the acute and long-term effects of new treatment agents on breast cancer survivors' health and functioning. In addition, cancer survivorship research needs to evolve in parallel with global evaluation of trends including demographics, economics, and patterns of cancer-related and non-cancer-related morbidity and mortality. Moreover, the ICT sphere offers potential as a complementary element to the traditional healthcare system and it is rapidly changing in Korea and other developing countries; therefore, we particularly need to focus upon its improvement. Healthcare is not a product; it is a service that is coproduced between the providers and the users, and it has value only when survivors use it. Therefore, the service design could play a crucial role in innovating the healthcare delivery system to balance different perspectives [114].
To meet these demands for knowledge in a timely manner, efforts to identify specific research to clarify relevant issues and foster collaboration in diverse fields are important. The Korean Breast Cancer Survivorship Research Group was organized to meet the demands of breast cancer survivors. Various members including breast surgeons, surgical oncologists, and specialists in service design, food and nutrition, and psychology are actively participating to establish a scientific paradigm in survivorship research, which looks beyond treatment and represents a shift from a medical deficit-dysfunction model, toward a multi- and interdisciplinary focus.
Future research on breast cancer survivorship needs to provide management guidance for clinicians, personalize and enhance follow-up care, facilitate early detection and prevention of treatment-related adverse effects, provide timely intervention for long-term effects, enhance QoL and psychosocial functioning, and promote a healthy lifestyle among breast cancer survivors. Fundamental basic research is required to understand the mechanisms and etiology of breast cancer, treatment-related sequelae, and late effects. Currently, there are limited clinical data on breast cancer survivorship, and intervention studies to address the management of long-term effects, QoL issues, and lifestyle modification must be conducted. The next generation of survivorship research will need to use validated and reliable measures for surveillance and monitoring of both physiologic and psychosocial variables.
To incorporate this perspective, a framework could be established for survivorship research. Evidence-based knowledge should be achieved through fundamental research, intervention research, and surveillance and monitoring to promote clinical guidance (such as a survivorship care plan) for breast cancer survivors. With the appropriate provision of clinical guidance through health care systems and social policies, the burdens of breast cancer survivors can be reduced in the future.
ACKNOWLEDGMENTS
We thank all survivors to participate in the interviews.
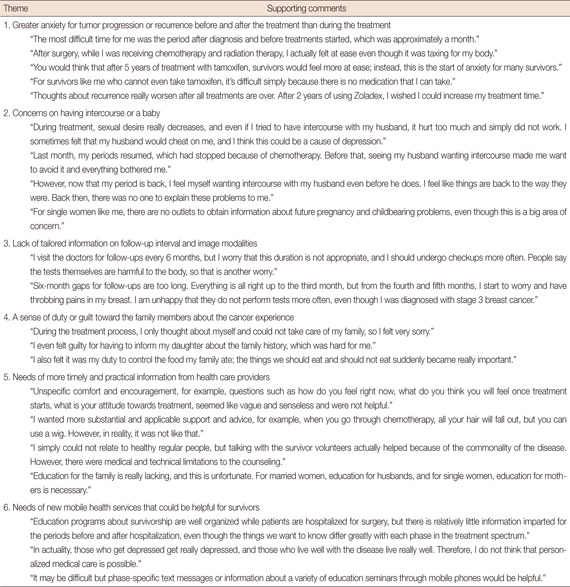
Appendix 1
Comments from breast cancer survivors supporting the themes identified in the interview
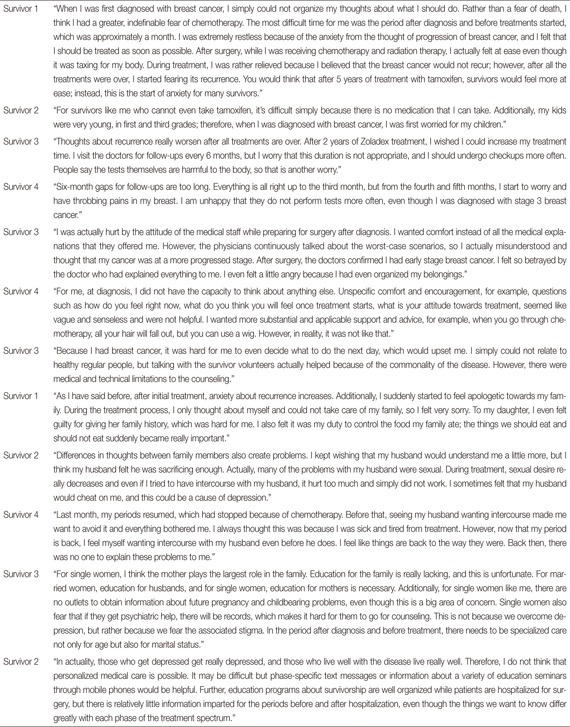
Appendix 2
The summarized transcription of the interviews of four survivors
Footnotes
This study was supported by a grant from Korea Breast Cancer Foundation and a grant from the National R&D Program for Cancer Control, Ministry for Health and Welfare, Republic of Korea (number: 1220170).
The authors declare that they have no competing interests.
References
- 1.Hewitt ME, Ganz P. From Cancer Patient to Cancer Survivor: Lost in Transition: an American Society of Clinical Oncology and Institute of Medicine Symposium. Washington, DC: National Academies Press; 2006. pp. 23–24. [Google Scholar]
- 2.Survivorship definitions. 2014. Office of Cancer Survivorship. 2014. [Accessed August 25th, 2014]. http://cancercontrol.cancer.gov/ocs/statistics/definitions.html.
- 3.Kappel ML. It's not the model that matters: still lost in transition. J Oncol Pract. 2013;9:128–129. doi: 10.1200/JOP.2013.001016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yun YH, Kim YA, Min YH, Park S, Won YJ, Kim DY, et al. The influence of hospital volume and surgical treatment delay on long-term survival after cancer surgery. Ann Oncol. 2012;23:2731–2737. doi: 10.1093/annonc/mds101. [DOI] [PubMed] [Google Scholar]
- 5.Shin DW, Cho J, Kim SY, Guallar E, Hwang SS, Cho B, et al. Delay to curative surgery greater than 12 weeks is associated with increased mortality in patients with colorectal and breast cancer but not lung or thyroid cancer. Ann Surg Oncol. 2013;20:2468–2476. doi: 10.1245/s10434-013-2957-y. [DOI] [PubMed] [Google Scholar]
- 6.Bilimoria KY, Ko CY, Tomlinson JS, Stewart AK, Talamonti MS, Hynes DL, et al. Wait times for cancer surgery in the United States: trends and predictors of delays. Ann Surg. 2011;253:779–785. doi: 10.1097/SLA.0b013e318211cc0f. [DOI] [PubMed] [Google Scholar]
- 7.Smith EC, Ziogas A, Anton-Culver H. Delay in surgical treatment and survival after breast cancer diagnosis in young women by race/ethnicity. JAMA Surg. 2013;148:516–523. doi: 10.1001/jamasurg.2013.1680. [DOI] [PubMed] [Google Scholar]
- 8.Vujovic O, Yu E, Cherian A, Perera F, Dar AR, Stitt L, et al. Effect of interval to definitive breast surgery on clinical presentation and survival in early-stage invasive breast cancer. Int J Radiat Oncol Biol Phys. 2009;75:771–774. doi: 10.1016/j.ijrobp.2008.11.049. [DOI] [PubMed] [Google Scholar]
- 9.Brazda A, Estroff J, Euhus D, Leitch AM, Huth J, Andrews V, et al. Delays in time to treatment and survival impact in breast cancer. Ann Surg Oncol. 2010;17(Suppl 3):291–296. doi: 10.1245/s10434-010-1250-6. [DOI] [PubMed] [Google Scholar]
- 10.Mujar M, Dahlui M, Yip CH, Taib NA. Delays in time to primary treatment after a diagnosis of breast cancer: does it impact survival? Prev Med. 2013;56:222–224. doi: 10.1016/j.ypmed.2012.12.001. [DOI] [PubMed] [Google Scholar]
- 11.Eastman A, Tammaro Y, Moldrem A, Andrews V, Huth J, Euhus D, et al. Outcomes of delays in time to treatment in triple negative breast cancer. Ann Surg Oncol. 2013;20:1880–1885. doi: 10.1245/s10434-012-2835-z. [DOI] [PubMed] [Google Scholar]
- 12.Kim K, Chie EK, Han W, Noh DY, Ha SW. Impact of delayed radiotherapy on local control in node-negative breast cancer patients treated with breast-conserving surgery and adjuvant radiotherapy without chemotherapy. Tumori. 2011;97:341–344. doi: 10.1177/030089161109700314. [DOI] [PubMed] [Google Scholar]
- 13.Barbieri V, Sanpaolo P, Genovesi D. Interval between breast-conserving surgery and start of radiation therapy in early-stage breast cancer is not predictive of local recurrence: a single-institution experience. Clin Breast Cancer. 2011;11:114–120. doi: 10.1016/j.clbc.2011.03.004. [DOI] [PubMed] [Google Scholar]
- 14.Karlsson P, Cole BF, Colleoni M, Roncadin M, Chua BH, Murray E, et al. Timing of radiotherapy and outcome in patients receiving adjuvant endocrine therapy. Int J Radiat Oncol Biol Phys. 2011;80:398–402. doi: 10.1016/j.ijrobp.2010.02.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barry PN, Riley EC, Pan J, Crew JB, Lee K, Jain D, et al. Delay of adjuvant chemotherapy after elective mastectomy and immediate reconstruction in breast-conservation candidates: a matched-pair analysis. Am J Clin Oncol. doi: 10.1097/COC.0b013e318280d79f. Epub 2013 Mar 4. http://dx.doi.org/10.1097/COC.0b013e318280d79f. [DOI] [PubMed] [Google Scholar]
- 16.Baena-Cañada JM, Rosado-Varela P, Estalella-Mendoza S, Expósito-Álvarez I, González-Guerrero M, Benítez-Rodríguez E. Influence of clinical and biographical factors on the delay in starting adjuvant chemotherapy treatment among breast cancer patients. Med Clin (Barc) 2013;140:444–448. doi: 10.1016/j.medcli.2012.03.007. [DOI] [PubMed] [Google Scholar]
- 17.Lamb MA. Effects of cancer on the sexuality and fertility of women. Semin Oncol Nurs. 1995;11:120–127. doi: 10.1016/s0749-2081(05)80019-1. [DOI] [PubMed] [Google Scholar]
- 18.Dizon DS. Quality of life after breast cancer: survivorship and sexuality. Breast J. 2009;15:500–504. doi: 10.1111/j.1524-4741.2009.00766.x. [DOI] [PubMed] [Google Scholar]
- 19.Krychman ML, Pereira L, Carter J, Amsterdam A. Sexual oncology: sexual health issues in women with cancer. Oncology. 2006;71:18–25. doi: 10.1159/000100521. [DOI] [PubMed] [Google Scholar]
- 20.Ochsenkühn R, Hermelink K, Clayton AH, von Schönfeldt V, Gallwas J, Ditsch N, et al. Menopausal status in breast cancer patients with past chemotherapy determines long-term hypoactive sexual desire disorder. J Sex Med. 2011;8:1486–1494. doi: 10.1111/j.1743-6109.2011.02220.x. [DOI] [PubMed] [Google Scholar]
- 21.Kornblith AB, Ligibel J. Psychosocial and sexual functioning of survivors of breast cancer. Semin Oncol. 2003;30:799–813. doi: 10.1053/j.seminoncol.2003.08.025. [DOI] [PubMed] [Google Scholar]
- 22.Krebs LU. Sexual health during cancer treatment. Adv Exp Med Biol. 2012;732:61–76. doi: 10.1007/978-94-007-2492-1_5. [DOI] [PubMed] [Google Scholar]
- 23.Kroenke CH, Rosner B, Chen WY, Kawachi I, Colditz GA, Holmes MD. Functional impact of breast cancer by age at diagnosis. J Clin Oncol. 2004;22:1849–1856. doi: 10.1200/JCO.2004.04.173. [DOI] [PubMed] [Google Scholar]
- 24.Gallo-Silver L. The sexual rehabilitation of persons with cancer. Cancer Pract. 2000;8:10–15. doi: 10.1046/j.1523-5394.2000.81005.x. [DOI] [PubMed] [Google Scholar]
- 25.Partridge AH, Gelber S, Peppercorn J, Sampson E, Knudsen K, Laufer M, et al. Web-based survey of fertility issues in young women with breast cancer. J Clin Oncol. 2004;22:4174–4183. doi: 10.1200/JCO.2004.01.159. [DOI] [PubMed] [Google Scholar]
- 26.Thewes B, Meiser B, Taylor A, Phillips KA, Pendlebury S, Capp A, et al. Fertility- and menopause-related information needs of younger women with a diagnosis of early breast cancer. J Clin Oncol. 2005;23:5155–5165. doi: 10.1200/JCO.2005.07.773. [DOI] [PubMed] [Google Scholar]
- 27.Holleb AI. Breast cancer and pregnancy. CA Cancer J Clin. 1965;15:182–183. doi: 10.3322/canjclin.15.4.182. [DOI] [PubMed] [Google Scholar]
- 28.Azim HA, Jr, Santoro L, Pavlidis N, Gelber S, Kroman N, Azim H, et al. Safety of pregnancy following breast cancer diagnosis: a meta-analysis of 14 studies. Eur J Cancer. 2011;47:74–83. doi: 10.1016/j.ejca.2010.09.007. [DOI] [PubMed] [Google Scholar]
- 29.de Bree E, Makrigiannakis A, Askoxylakis J, Melissas J, Tsiftsis DD. Pregnancy after breast cancer: a comprehensive review. J Surg Oncol. 2010;101:534–542. doi: 10.1002/jso.21514. [DOI] [PubMed] [Google Scholar]
- 30.Mueller BA, Simon MS, Deapen D, Kamineni A, Malone KE, Daling JR. Childbearing and survival after breast carcinoma in young women. Cancer. 2003;98:1131–1140. doi: 10.1002/cncr.11634. [DOI] [PubMed] [Google Scholar]
- 31.Ives A, Saunders C, Bulsara M, Semmens J. Pregnancy after breast cancer: population based study. BMJ. 2007;334:194. doi: 10.1136/bmj.39035.667176.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Azim HA, Jr, Peccatori FA, de Azambuja E, Piccart MJ. Motherhood after breast cancer: searching for la dolce vita. Expert Rev Anticancer Ther. 2011;11:287–298. doi: 10.1586/era.10.208. [DOI] [PubMed] [Google Scholar]
- 33.Partridge AH, Ruddy KJ. Fertility and adjuvant treatment in young women with breast cancer. Breast. 2007;16(Suppl 2):S175–S181. doi: 10.1016/j.breast.2007.07.029. [DOI] [PubMed] [Google Scholar]
- 34.Lee SJ, Schover LR, Partridge AH, Patrizio P, Wallace WH, Hagerty K, et al. American Society of Clinical Oncology recommendations on fertility preservation in cancer patients. J Clin Oncol. 2006;24:2917–2931. doi: 10.1200/JCO.2006.06.5888. [DOI] [PubMed] [Google Scholar]
- 35.Walshe JM, Denduluri N, Swain SM. Amenorrhea in premenopausal women after adjuvant chemotherapy for breast cancer. J Clin Oncol. 2006;24:5769–5779. doi: 10.1200/JCO.2006.07.2793. [DOI] [PubMed] [Google Scholar]
- 36.Partridge AH, Ruddy KJ, Gelber S, Schapira L, Abusief M, Meyer M, et al. Ovarian reserve in women who remain premenopausal after chemotherapy for early stage breast cancer. Fertil Steril. 2010;94:638–644. doi: 10.1016/j.fertnstert.2009.03.045. [DOI] [PubMed] [Google Scholar]
- 37.Loren AW, Mangu PB, Beck LN, Brennan L, Magdalinski AJ, Partridge AH, et al. Fertility preservation for patients with cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol. 2013;31:2500–2510. doi: 10.1200/JCO.2013.49.2678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lee S, Ozkavukcu S, Heytens E, Moy F, Oktay K. Value of early referral to fertility preservation in young women with breast cancer. J Clin Oncol. 2010;28:4683–4686. doi: 10.1200/JCO.2010.30.5748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Porcu E, Bazzocchi A, Notarangelo L, Paradisi R, Landolfo C, Venturoli S. Human oocyte cryopreservation in infertility and oncology. Curr Opin Endocrinol Diabetes Obes. 2008;15:529–535. doi: 10.1097/MED.0b013e3283199129. [DOI] [PubMed] [Google Scholar]
- 40.West ER, Shea LD, Woodruff TK. Engineering the follicle microenvironment. Semin Reprod Med. 2007;25:287–299. doi: 10.1055/s-2007-980222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Donaldson SS, Link MP, Weinstein HJ, Rai SN, Brain S, Billett AL, et al. Final results of a prospective clinical trial with VAMP and low-dose involved-field radiation for children with low-risk Hodgkin's disease. J Clin Oncol. 2007;25:332–337. doi: 10.1200/JCO.2006.08.4772. [DOI] [PubMed] [Google Scholar]
- 42.Dalberg K, Mattsson A, Sandelin K, Rutqvist LE. Outcome of treatment for ipsilateral breast tumor recurrence in early-stage breast cancer. Breast Cancer Res Treat. 1998;49:69–78. doi: 10.1023/a:1005934513072. [DOI] [PubMed] [Google Scholar]
- 43.Palli D, Russo A, Saieva C, Ciatto S, Rosselli Del Turco M, Distante V, et al. Intensive vs clinical follow-up after treatment of primary breast cancer: 10-year update of a randomized trial. National Research Council Project on Breast Cancer Follow-up. JAMA. 1999;281:1586. doi: 10.1001/jama.281.17.1586. [DOI] [PubMed] [Google Scholar]
- 44.Oltra A, Santaballa A, Munárriz B, Pastor M, Montalar J. Cost-benefit analysis of a follow-up program in patients with breast cancer: a randomized prospective study. Breast J. 2007;13:571–574. doi: 10.1111/j.1524-4741.2007.00506.x. [DOI] [PubMed] [Google Scholar]
- 45.Sheppard C, Higgins B, Wise M, Yiangou C, Dubois D, Kilburn S. Breast cancer follow up: a randomised controlled trial comparing point of need access versus routine 6-monthly clinical review. Eur J Oncol Nurs. 2009;13:2–8. doi: 10.1016/j.ejon.2008.11.005. [DOI] [PubMed] [Google Scholar]
- 46.American Society of Clinical Oncology. Recommended breast cancer surveillance guidelines. J Clin Oncol. 1997;15:2149–2156. doi: 10.1200/JCO.1997.15.5.2149. [DOI] [PubMed] [Google Scholar]
- 47.Elston Lafata J, Simpkins J, Schultz L, Chase GA, Johnson CC, Yood MU, et al. Routine surveillance care after cancer treatment with curative intent. Med Care. 2005;43:592–599. doi: 10.1097/01.mlr.0000163656.62562.c4. [DOI] [PubMed] [Google Scholar]
- 48.Jung YS, Na KY, Kim KS, Ahn SH, Lee SJ, Park HK, et al. Nation-wide Korean breast cancer data from 2008 using the breast cancer registration program. J Breast Cancer. 2011;14:229–236. doi: 10.4048/jbc.2011.14.3.229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Claus EB, Schildkraut JM, Thompson WD, Risch NJ. The genetic attributable risk of breast and ovarian cancer. Cancer. 1996;77:2318–2324. doi: 10.1002/(SICI)1097-0142(19960601)77:11<2318::AID-CNCR21>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- 50.Stratton MR, Rahman N. The emerging landscape of breast cancer susceptibility. Nat Genet. 2008;40:17–22. doi: 10.1038/ng.2007.53. [DOI] [PubMed] [Google Scholar]
- 51.Kang DH, Kim SW, Noh DY, Ahn YO, Ryu KY. Korean Breast Cancer Society, editor. The Breast. 2nd ed. Seoul: Ilchokak; 2005. Epidemiology of breast cancer; pp. 168–188. [Google Scholar]
- 52.Han SA, Park SK, Ahn SH, Son BH, Lee MH, Choi DH, et al. The breast and ovarian cancer risks in Korea due to inherited mutations in BRCA1 and BRCA2: a preliminary report. J Breast Cancer. 2009;12:92–99. [Google Scholar]
- 53.Son BH, Ahn SH, Kim SW, Kang E, Park SK, Lee MH, et al. Prevalence of BRCA1 and BRCA2 mutations in non-familial breast cancer patients with high risks in Korea: the Korean Hereditary Breast Cancer (KOHBRA) Study. Breast Cancer Res Treat. 2012;133:1143–1152. doi: 10.1007/s10549-012-2001-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Han SA, Kim SW, Kang E, Park SK, Ahn SH, Lee MH, et al. The prevalence of BRCA mutations among familial breast cancer patients in Korea: results of the Korean Hereditary Breast Cancer study. Fam Cancer. 2013;12:75–81. doi: 10.1007/s10689-012-9578-7. [DOI] [PubMed] [Google Scholar]
- 55.Chlebowski RT, Blackburn GL, Thomson CA, Nixon DW, Shapiro A, Hoy MK, et al. Dietary fat reduction and breast cancer outcome: interim efficacy results from the Women's Intervention Nutrition Study. J Natl Cancer Inst. 2006;98:1767–1776. doi: 10.1093/jnci/djj494. [DOI] [PubMed] [Google Scholar]
- 56.Pierce JP, Natarajan L, Caan BJ, Parker BA, Greenberg ER, Flatt SW, et al. Influence of a diet very high in vegetables, fruit, and fiber and low in fat on prognosis following treatment for breast cancer: the Women's Healthy Eating and Living (WHEL) randomized trial. JAMA. 2007;298:289–298. doi: 10.1001/jama.298.3.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kroenke CH, Fung TT, Hu FB, Holmes MD. Dietary patterns and survival after breast cancer diagnosis. J Clin Oncol. 2005;23:9295–9303. doi: 10.1200/JCO.2005.02.0198. [DOI] [PubMed] [Google Scholar]
- 58.Kwan ML, Weltzien E, Kushi LH, Castillo A, Slattery ML, Caan BJ. Dietary patterns and breast cancer recurrence and survival among women with early-stage breast cancer. J Clin Oncol. 2009;27:919–926. doi: 10.1200/JCO.2008.19.4035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Belle FN, Kampman E, McTiernan A, Bernstein L, Baumgartner K, Baumgartner R, et al. Dietary fiber, carbohydrates, glycemic index, and glycemic load in relation to breast cancer prognosis in the HEAL cohort. Cancer Epidemiol Biomarkers Prev. 2011;20:890–899. doi: 10.1158/1055-9965.EPI-10-1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Beasley JM, Newcomb PA, Trentham-Dietz A, Hampton JM, Bersch AJ, Passarelli MN, et al. Post-diagnosis dietary factors and survival after invasive breast cancer. Breast Cancer Res Treat. 2011;128:229–236. doi: 10.1007/s10549-010-1323-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Shu XO, Zheng Y, Cai H, Gu K, Chen Z, Zheng W, et al. Soy food intake and breast cancer survival. JAMA. 2009;302:2437–2443. doi: 10.1001/jama.2009.1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Vrieling A, Buck K, Seibold P, Heinz J, Obi N, Flesch-Janys D, et al. Dietary patterns and survival in German postmenopausal breast cancer survivors. Br J Cancer. 2013;108:188–192. doi: 10.1038/bjc.2012.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.McEligot AJ, Largent J, Ziogas A, Peel D, Anton-Culver H. Dietary fat, fiber, vegetable, and micronutrients are associated with overall survival in postmenopausal women diagnosed with breast cancer. Nutr Cancer. 2006;55:132–140. doi: 10.1207/s15327914nc5502_3. [DOI] [PubMed] [Google Scholar]
- 64.Nechuta S, Caan BJ, Chen WY, Kwan ML, Lu W, Cai H, et al. Postdiagnosis cruciferous vegetable consumption and breast cancer outcomes: a report from the After Breast Cancer Pooling Project. Cancer Epidemiol Biomarkers Prev. 2013;22:1451–1456. doi: 10.1158/1055-9965.EPI-13-0446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Thomson CA, Rock CL, Thompson PA, Caan BJ, Cussler E, Flatt SW, et al. Vegetable intake is associated with reduced breast cancer recurrence in tamoxifen users: a secondary analysis from the Women's Healthy Eating and Living Study. Breast Cancer Res Treat. 2011;125:519–527. doi: 10.1007/s10549-010-1014-9. [DOI] [PubMed] [Google Scholar]
- 66.Rock CL, Flatt SW, Natarajan L, Thomson CA, Bardwell WA, Newman VA, et al. Plasma carotenoids and recurrence-free survival in women with a history of breast cancer. J Clin Oncol. 2005;23:6631–6638. doi: 10.1200/JCO.2005.19.505. [DOI] [PubMed] [Google Scholar]
- 67.Velicer CM, Ulrich CM. Vitamin and mineral supplement use among US adults after cancer diagnosis: a systematic review. J Clin Oncol. 2008;26:665–673. doi: 10.1200/JCO.2007.13.5905. [DOI] [PubMed] [Google Scholar]
- 68.Poole EM, Shu X, Caan BJ, Flatt SW, Holmes MD, Lu W, et al. Postdiagnosis supplement use and breast cancer prognosis in the After Breast Cancer Pooling Project. Breast Cancer Res Treat. 2013;139:529–537. doi: 10.1007/s10549-013-2548-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Rock CL, Doyle C, Demark-Wahnefried W, Meyerhardt J, Courneya KS, Schwartz AL, et al. Nutrition and physical activity guidelines for cancer survivors. CA Cancer J Clin. 2012;62:243–274. doi: 10.3322/caac.21142. [DOI] [PubMed] [Google Scholar]
- 70.Chi F, Wu R, Zeng YC, Xing R, Liu Y, Xu ZG. Post-diagnosis soy food intake and breast cancer survival: a meta-analysis of cohort studies. Asian Pac J Cancer Prev. 2013;14:2407–2412. doi: 10.7314/apjcp.2013.14.4.2407. [DOI] [PubMed] [Google Scholar]
- 71.Jacobs ET, Thomson CA, Flatt SW, Al-Delaimy WK, Hibler EA, Jones LA, et al. Vitamin D and breast cancer recurrence in the Women's Healthy Eating and Living (WHEL) Study. Am J Clin Nutr. 2011;93:108–117. doi: 10.3945/ajcn.2010.30009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Vrieling A, Hein R, Abbas S, Schneeweiss A, Flesch-Janys D, Chang-Claude J. Serum 25-hydroxyvitamin D and postmenopausal breast cancer survival: a prospective patient cohort study. Breast Cancer Res. 2011;13:R74. doi: 10.1186/bcr2920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Beasley JM, Kwan ML, Chen WY, Weltzien EK, Kroenke CH, Lu W, et al. Meeting the physical activity guidelines and survival after breast cancer: findings from the after breast cancer pooling project. Breast Cancer Res Treat. 2012;131:637–643. doi: 10.1007/s10549-011-1770-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Shin HR, Boniol M, Joubert C, Hery C, Haukka J, Autier P, et al. Secular trends in breast cancer mortality in five East Asian populations: Hong Kong, Japan, Korea, Singapore and Taiwan. Cancer Sci. 2010;101:1241–1246. doi: 10.1111/j.1349-7006.2010.01519.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hewitt ME, Bamundo A, Day R, Harvey C. Perspectives on post-treatment cancer care: qualitative research with survivors, nurses, and physicians. J Clin Oncol. 2007;25:2270–2273. doi: 10.1200/JCO.2006.10.0826. [DOI] [PubMed] [Google Scholar]
- 76.Borreani C, Miccinesi G, Brunelli C, Lina M. An increasing number of qualitative research papers in oncology and palliative care: does it mean a thorough development of the methodology of research? Health Qual Life Outcomes. 2004;2:7. doi: 10.1186/1477-7525-2-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ragin CC. The Comparative Method: Moving beyond Qualitative and Quantitative Strategies. Berkeley: University of California Press; 1987. pp. 1–18. [Google Scholar]
- 78.Pope C, Mays N. Reaching the parts other methods cannot reach: an introduction to qualitative methods in health and health services research. BMJ. 1995;311:42–45. doi: 10.1136/bmj.311.6996.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ragin CC. Introduction to qualitative comparative analysis. In: Janoski T, Hicks AM, editors. The Comparative Political Economy of the Welfare State. Cambridge: Cambridge University Press; 1994. pp. 300–309. [Google Scholar]
- 80.Camic PM, Rhodes JE, Yardley L. Naming the stars: integrating qualitative methods into psychological research. In: Camic PM, Rhodes JE, Yardley L, editors. Qualitative Research in Psychology: Expanding Perspectives in Methodology and Design. Washington, DC: American Psychological Association; 2003. pp. 3–15. [Google Scholar]
- 81.Hays DG, Singh AA. Qualitative Inquiry in Clinical and Educational Settings. New York: Guilford Press; 2011. pp. 3–31. [Google Scholar]
- 82.Strang P. Qualitative research methods in palliative medicine and palliative oncology: an introduction. Acta Oncol. 2000;39:911–917. doi: 10.1080/02841860050215873. [DOI] [PubMed] [Google Scholar]
- 83.Roundtree AK, Giordano SH, Price A, Suarez-Almazor ME. Problems in transition and quality of care: perspectives of breast cancer survivors. Support Care Cancer. 2011;19:1921–1929. doi: 10.1007/s00520-010-1031-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Lally RM, Underhill ML. Transition to breast cancer survivorship: a longitudinal qualitative follow-up study of two-year survivors. J Psychosoc Oncol. 2012;30:97–127. doi: 10.1080/07347332.2011.633983. [DOI] [PubMed] [Google Scholar]
- 85.Kirkman M, Winship I, Stern C, Neil S, Mann GB, Fisher JR. Women's reflections on fertility and motherhood after breast cancer and its treatment. Eur J Cancer Care (Engl) 2014;23:502–513. doi: 10.1111/ecc.12163. [DOI] [PubMed] [Google Scholar]
- 86.Wang F, Chen F, Huo X, Xu R, Wu L, Wang J, et al. A neglected issue on sexual well-being following breast cancer diagnosis and treatment among Chinese women. PLoS One. 2013;8:e74473. doi: 10.1371/journal.pone.0074473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Kim IR, Cho J, Choi EK, Kwon IG, Sung YH, Lee JE, et al. Perception, attitudes, preparedness and experience of chemotherapy-induced alopecia among breast cancer patients: a qualitative study. Asian Pac J Cancer Prev. 2012;13:1383–1388. doi: 10.7314/apjcp.2012.13.4.1383. [DOI] [PubMed] [Google Scholar]
- 88.Milberg A, Strang P. Met and unmet needs in hospital-based home care: qualitative evaluation through open-ended questions. Palliat Med. 2000;14:533–534. doi: 10.1191/026921600701536282. [DOI] [PubMed] [Google Scholar]
- 89.Luoma ML, Hakamies-Blomqvist L. The meaning of quality of life in patients being treated for advanced breast cancer: a qualitative study. Psychooncology. 2004;13:729–739. doi: 10.1002/pon.788. [DOI] [PubMed] [Google Scholar]
- 90.Ashing-Giwa KT, Padilla G, Tejero J, Kraemer J, Wright K, Coscarelli A, et al. Understanding the breast cancer experience of women: a qualitative study of African American, Asian American, Latina and Caucasian cancer survivors. Psychooncology. 2004;13:408–428. doi: 10.1002/pon.750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Foley KL, Farmer DF, Petronis VM, Smith RG, McGraw S, Smith K, et al. A qualitative exploration of the cancer experience among long-term survivors: comparisons by cancer type, ethnicity, gender, and age. Psychooncology. 2006;15:248–258. doi: 10.1002/pon.942. [DOI] [PubMed] [Google Scholar]
- 92.Lee S, Chen L, Ma GX, Fang CY, Oh Y, Scully L. Challenges and needs of Chinese and Korean American breast cancer survivors: in-depth interviews. N Am J Med Sci (Boston) 2013;6:1–8. doi: 10.7156/najms.2013.0601001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.De Vries J, Den Oudsten BL, Jacobs PM, Roukema JA. How breast cancer survivors cope with fear of recurrence: a focus group study. Support Care Cancer. 2014;22:705–712. doi: 10.1007/s00520-013-2025-y. [DOI] [PubMed] [Google Scholar]
- 94.Thomsen DK, Pedersen AF, Johansen MB, Jensen AB, Zachariae R. Breast cancer patients' narratives about positive and negative communication experiences. Acta Oncol. 2007;46:900–908. doi: 10.1080/02841860701261550. [DOI] [PubMed] [Google Scholar]
- 95.Wright EB, Holcombe C, Salmon P. Doctors' communication of trust, care, and respect in breast cancer: qualitative study. BMJ. 2004;328:864. doi: 10.1136/bmj.38046.771308.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Green J, Thorogood N. Qualitative Methods for Health Research. 3rd ed. London: Sage; 2013. p. 20. [Google Scholar]
- 97.Hefferon K, Murphy H, McLeod J, Mutrie N, Campbell A. Understanding barriers to exercise implementation 5-year post-breast cancer diagnosis: a large-scale qualitative study. Health Educ Res. 2013;28:843–856. doi: 10.1093/her/cyt083. [DOI] [PubMed] [Google Scholar]
- 98.Miedema B, Easley J. Barriers to rehabilitative care for young breast cancer survivors: a qualitative understanding. Support Care Cancer. 2012;20:1193–1201. doi: 10.1007/s00520-011-1196-7. [DOI] [PubMed] [Google Scholar]
- 99.Nelson A, Fenlon D, Morris J, Sampson C, Harrop E, Murray N, et al. QUALZICE: a QUALitative exploration of the experiences of the participants from the ZICE clinical trial (metastatic breast cancer) receiving intravenous or oral bisphosphonates. Trials. 2013;14:325. doi: 10.1186/1745-6215-14-325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Consulting VW. mHealth for Development: the Opportunity of Mobile Technology for Healthcare in the Developing World. Washington, DC: UN Foundation-Vodafone Foundation Partnership; 2009. [Google Scholar]
- 101.Pal K, Eastwood SV, Michie S, Farmer AJ, Barnard ML, Peacock R, et al. Computer-based diabetes self-management interventions for adults with type 2 diabetes mellitus. Cochrane Database Syst Rev. 2013;3:CD008776. doi: 10.1002/14651858.CD008776.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.de Jongh T, Gurol-Urganci I, Vodopivec-Jamsek V, Car J, Atun R. Mobile phone messaging for facilitating self-management of long-term illnesses. Cochrane Database Syst Rev. 2012;12:CD007459. doi: 10.1002/14651858.CD007459.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Haynes RB, Ackloo E, Sahota N, McDonald HP, Yao X. Interventions for enhancing medication adherence. Cochrane Database Syst Rev. 2008;(2):CD000011. doi: 10.1002/14651858.CD000011.pub3. [DOI] [PubMed] [Google Scholar]
- 104.Gentry S, van-Velthoven MH, Tudor Car L, Car J. Telephone delivered interventions for reducing morbidity and mortality in people with HIV infection. Cochrane Database Syst Rev. 2013;5:CD009189. doi: 10.1002/14651858.CD009189.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Whittaker R, McRobbie H, Bullen C, Borland R, Rodgers A, Gu Y. Mobile phone-based interventions for smoking cessation. Cochrane Database Syst Rev. 2012;11:CD006611. doi: 10.1002/14651858.CD006611.pub3. [DOI] [PubMed] [Google Scholar]
- 106.Marcano Belisario JS, Bruggeling MN, Gunn LH, Brusamento S, Car J. Interventions for recruiting smokers into cessation programmes. Cochrane Database Syst Rev. 2012;12:CD009187. doi: 10.1002/14651858.CD009187.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Ryan D, Cobern W, Wheeler J, Price D, Tarassenko L. Mobile phone technology in the management of asthma. J Telemed Telecare. 2005;11(Suppl 1):43–46. doi: 10.1258/1357633054461714. [DOI] [PubMed] [Google Scholar]
- 108.Weaver A, Young AM, Rowntree J, Townsend N, Pearson S, Smith J, et al. Application of mobile phone technology for managing chemotherapy-associated side-effects. Ann Oncol. 2007;18:1887–1892. doi: 10.1093/annonc/mdm354. [DOI] [PubMed] [Google Scholar]
- 109.Killingsworth MA, Gilbert DT. A wandering mind is an unhappy mind. Science. 2010;330:932. doi: 10.1126/science.1192439. [DOI] [PubMed] [Google Scholar]
- 110.Valle CG, Tate DF, Mayer DK, Allicock M, Cai J. A randomized trial of a Facebook-based physical activity intervention for young adult cancer survivors. J Cancer Surviv. 2013;7:355–368. doi: 10.1007/s11764-013-0279-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Wu Y, Zhang D, Kang S. Physical activity and risk of breast cancer: a meta-analysis of prospective studies. Breast Cancer Res Treat. 2013;137:869–882. doi: 10.1007/s10549-012-2396-7. [DOI] [PubMed] [Google Scholar]
- 112.Patrick K, Griswold WG, Raab F, Intille SS. Health and the mobile phone. Am J Prev Med. 2008;35:177–181. doi: 10.1016/j.amepre.2008.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Ganz PA. Quality of life across the continuum of breast cancer care. Breast J. 2000;6:324–330. doi: 10.1046/j.1524-4741.2000.20042.x. [DOI] [PubMed] [Google Scholar]
- 114.Polaine A, Løvlie L, Reason B. Service Design: from Insight to Implementation. Brooklyn: Rosenfeld Media; 2012. [Google Scholar]


