Abstract
Late cancellations of scheduled elective surgery limit the ability of the surgical care service to achieve its goals. Attributes of these cancellations differ between hospitals and regions. The rate of late cancellations of elective surgery conducted in Hamad General Hospital, Doha, Qatar was found to be 13.14% which is similar to rates reported in hospitals elsewhere in the world; although elective surgery is performed six days a week from 7:00 am to 10:00 pm in our hospital. Simple and systematic analysis of these attributes typically provides limited solutions to the cancellation problem. Alternatively, the application of the theory of constraints with its five focusing steps, which analyze the system in its totality, is more likely to provide a better solution to the cancellation problem. To find the constraint, as a first focusing step, we carried out a retrospective and descriptive study using a quantitative approach combined with the Pareto Principle to find the main causes of cancellations, followed by a qualitative approach to find the main and ultimate underlying cause which pointed to the bed crisis. The remaining four focusing steps provided workable and effective solutions to reduce the cancellation rate of elective surgery.
Introduction
Booking elective surgery is considered a contract between the patient and healthcare institution. From the perspective of healthcare providers, booking determines the day of service delivery when appropriate resources become available and surgeon's schedules permit. In essence, the process of scheduling elective surgery consists of allocating operating time to various surgical services, assigning blocks of operating time to designated surgeons and anesthesiologists, and finally, booking patients into the operating room slots available with the respective surgeons. Any cancellation of the booking without prior notice or arrangements from either the patient or the healthcare provider, have far-reaching implications for both. (1)
The classical and simplistic approach to solving the problem of late cancellations focuses on finding the causes of these cancellations, and then to provide a solution for each cause individually, or collectively for all identified causes. (2–8,10–19) As the rates and causes of cancellations are diverse and differ from one hospital to another, (9) this classic and simplistic approach is likely to provide only limited solutions to the problem. (10,18) Statistical methods to compare rates of cancellations have been suggested. Some of them are valid to compare and to evaluate the different cancellation rates but they are not able to identify indirect causes of cancellation. (20)
An alternative approach to assess and provide solutions to the problem of elective surgery late cancellations is to apply a strong management tool, one of which is the theory of constraints as published by Eliyahu Goldratt in 1984 in his book “The Goal”. (21) According to this theory, the solution of any problem needs systemic thinking. In this context, the different steps of the surgical care pathway must be considered as a chain and its weakest step must be considered as the weakest link within this chain. This weakest link is also described as the bottleneck or the constraint, which is always invisible but usually expressed as having many undesirable effects found through good analysis of the existing surgical care chain. Direct elevation of the different undesirable effects needs time and energy and its results are either short-lived or useless; whereas the elevation of the core problem, the constraint, provides better results and eliminates all its undesirable effects simultaneously. (22)
According to the theory of constraints, late cancellations of surgical care are just undesirable effects of underlying causes. In our case, the core problem will be studied at Hamad General Hospital. This paper shows our approach to implement that theory.
Methods
The study of late elective surgical case cancellations in Hamad General Hospital was conducted following approval from the Hamad Medical Corporation Research Committee.
The problem was studied by applying the theory of constraints, which is based on five focusing steps which are simply described in Table 1.
Table 1.
The five focusing steps of the theory of constraints.
| Step 1: Identification of the constraint |
|
|
| A good understanding of the workflow helps to establish the chain of surgical care. The weakest link of the chain is the constraint. There is at least one constraint and we might find many but only the main one is considered the weakest link of the chain. It can be physical, human or a form of policy. It can also be internal or external. It is always invisible and can be found as a result a number of undesirable effects. |
|
|
| Step 2: Exploitation of the constraint |
|
|
| Any improvement of the system must start with the improvement of the weakest link. If the concerned link is no longer the weakest after its exploitation, Step 3 and 4 should be skipped directly to Step 5. |
|
|
| Step 3: Subordination of all other processes to the above decision |
|
|
| The strength of a chain is not the sum of strengths of its links and the strengthening of any link other than the weakest is of no value. Therefore, efforts should focus on the weakest link. If the concerned link is no longer the weakest after subordination of the other processes, the next step should be skipped directly to Step 5. |
|
|
| Step 4: Elimination of the constraint |
|
|
| If Step 2 and 3 are not sufficient to eliminate the constraint, this might require major changes to an actual system. The elimination of policy constraints allows for a quick and large improvement; however, they are more difficult to identify than physical constraints. |
|
|
| Step 5: Avoidance of inertia |
|
|
| Once the constraint is eliminated and improvement is obtained, another cycle should start again to look for the newest weak link of the chain. Should no further action be taken, inertia itself will then considered the newest constraint. In such event, the new link is considered as completely unknown and not among the constraints of the previous cycle. |
|
|
To implement the first step of the theory, we conducted a retrospective chart review analysis of the elective surgical cases recorded during an eight month period, from January 1st to August 31st in Hamad General Hospital, which is the central and largest governmental hospital in Qatar. It has more than 600 beds, five intensive care units and eight operating theatres. Those theatres are assigned for eight surgical sub-specialties, which are cardio-thoracic, maxillo-facial, neurosurgery, pediatric, vascular, orthopedic, general, and urology surgeries. However, ear-nose-throat surgical cases are not always performed in Hamad General Hospital operating theatres due to the critical nature of patients requiring this surgery and the risky transfer should they already be admitted to intensive care units in other hospitals.
During the mentioned eight-month study period, we recorded 4458 bookings for elective surgery. Among them only 3872 cases were serviced. The remaining 586 cases were either cancelled or postponed. Data on serviced or cancelled surgical cases were obtained from the daily operating theatre's lists where the cancelled cases are usually notified with the cause of cancellation. A debriefing was necessary to identify the real cause of cancellations that would allow us an accurate analysis and easy grouping of causes. Following this, data analysis was conducted according to different approaches. The first approach was mainly quantitative. It allowed us to calculate many statistical parameters followed by the implementation of Pareto's Principle to select the main causes of cancellation. In 1950, Joseph Juran's The Quality Control Handbook first recognized the applicability of the Pareto Principle from the name of the economist Vilfredo Pareto. The principle is also known as the law of “the vital few and the useful many” or the “80–20 rule”. It states that the majority of effects are due to a minority of the causes.
The second approach used was purely qualitative and focused only on the main causes of cancellations identified by the implementation of Pareto's law. It uses the thinking process of theory of constraints and allows one to find the underlying or indirect causes, even those which are behind human behavior. The main underlying cause was considered the constraint.
To implement the remaining steps of the theory, we reviewed literature to search for the most practical and effective solutions tried elsewhere in the word. These solutions were our suggestions to solve the problem of late elective surgical cancellations in our hospital.
Results
In our study, the average age of patients of cancelled scheduled elective surgical cases was 39.6 ± 17.67 years, with no significant difference found in cancellation rates between genders. Among the cancelled cases, 440 were males (75.09%) and 146 females (24.91%). The male/female ratio was 1.2 among Qatari citizens and 5 among expatriate residents. This is attributed to the larger proportion of migrant workers who are predominantly single males.
During the study, 586 elective cases were cancelled among 4458 booked cases. The overall rate of cancellations was 13.14%, which is similar to the rates reported elsewhere in the world. Our analytic calculations indicated a slightly higher rate of cancellation in outpatients (Table 2).
Table 2.
Cancellation by status of patients.
| Booked | Performed | Cancelled | Cancellations % | |
|
| ||||
| Inpatient | 3458 | 3025 | 433 | 12.52 |
|
| ||||
| Outpatient | 1000 | 847 | 153 | 15.30 |
|
| ||||
| 4458 | 3872 | 586 | 13.14 | |
|
| ||||
We observed that the rate of cancellation varied greatly depending on the type of surgery. We found different rates of cancellation fluctuating between the lowest rate (5.66%) for maxillofacial surgery and the highest (42.5%) for ear-nose-throat surgery (Table 3). These differences are due to many reasons, either patients' health conditions or sometimes to the causes of cancellations themselves.
Table 3.
Types of surgery and rates of cancellations.
| Type of surgery | Cancelled cases | Performed cases | Total | % of Cancellations | 95% CI | Standard error | ||
|
| ||||||||
| ENTS | 17 | 23 | 40 | 42.50 | 27.18 | - | 57.82 | 2.4223 |
|
| ||||||||
| CTS | 41 | 137 | 178 | 23.03 | 16.85 | - | 29.22 | 0.4636 |
|
| ||||||||
| OS | 189 | 870 | 1059 | 17.85 | 15.54 | - | 20.15 | 0.0709 |
|
| ||||||||
| US | 126 | 616 | 742 | 16.98 | 14.28 | - | 19.68 | 0.0992 |
|
| ||||||||
| NS | 23 | 205 | 228 | 10.09 | 6.18 | - | 14.00 | 0.2589 |
|
| ||||||||
| PS | 21 | 210 | 231 | 9.09 | 5.38 | - | 12.80 | 0.2439 |
|
| ||||||||
| GS | 134 | 1356 | 1490 | 8.99 | 7.54 | - | 10.45 | 0.0376 |
|
| ||||||||
| VS | 29 | 355 | 384 | 7.55 | 4.91 | - | 10.19 | 0.1349 |
|
| ||||||||
| MFS | 6 | 100 | 106 | 5.66 | 1.26 | - | 10.06 | 0.4273 |
|
| ||||||||
| Total | 586 | 3872 | 4458 | 13.14 | 12.15 | - | 14.14 | 0.0149 |
|
| ||||||||
CTS: cardio-thoracic surgery, ENTS: ear-nose-throat surgery, GS: general surgery, MFS: saxillo-facial surgery, NS: neurosurgery, OS: orthopedic surgery, PS: pediatric surgery, US: urologic surgery, VS: vascular surgery.
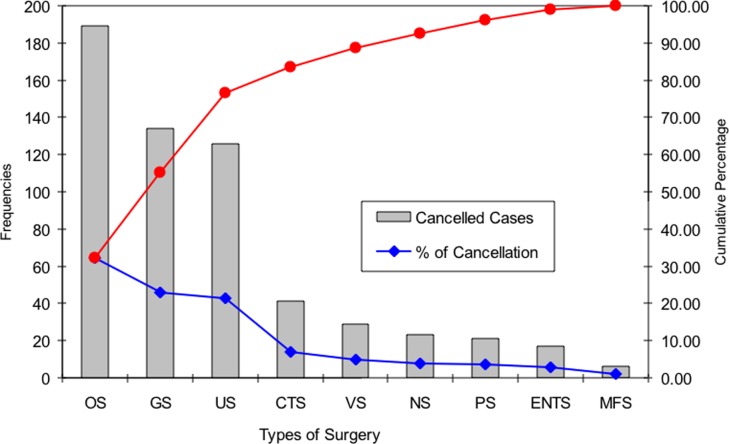
The cumulative proportion of general surgery with orthopedic surgery and urologic surgery was 76.62% among cancellations. They are well presented by the breakpoint of the Pareto chart (Figure 1), although the order of those three types of surgeries were not the same between inpatients and outpatients. While most of the cancelled inpatients were for orthopedic surgery, most of the cancelled outpatients were for urology surgery (Table 4).
Figure 1.
Proportion of types of surgery among cancelled cases.
Table 4.
Proportion of types of surgery among cancelled cases.
| Types of surgery | Inpatient | Outpatient | Cancelled cases | % of Cancellation | Cumulative percentage | Standard error |
|
| ||||||
| OS | 161 | 28 | 189 | 32.25 | 32.25 | 0.1563 |
|
| ||||||
| GS | 83 | 51 | 134 | 22.87 | 55.12 | 0.1404 |
|
| ||||||
| US | 65 | 61 | 126 | 21.50 | 76.62 | 0.1374 |
|
| ||||||
| CTS | 41 | 0 | 41 | 7.00 | 83.62 | 0.0853 |
|
| ||||||
| VS | 23 | 6 | 29 | 4.95 | 88.57 | 0.0725 |
|
| ||||||
| NS | 21 | 2 | 23 | 3.92 | 92.49 | 0.0649 |
|
| ||||||
| PS | 16 | 5 | 21 | 3.58 | 96.08 | 0.0621 |
|
| ||||||
| ENTS | 17 | 0 | 17 | 2.90 | 98.98 | 0.0561 |
|
| ||||||
| MFS | 6 | 0 | 6 | 1.02 | 100.00 | 0.0336 |
|
| ||||||
| Total | 433 | 153 | 586 | 100 | ||
|
| ||||||
| Percentage | 73.89% | 26.11% | 100% | |||
|
| ||||||
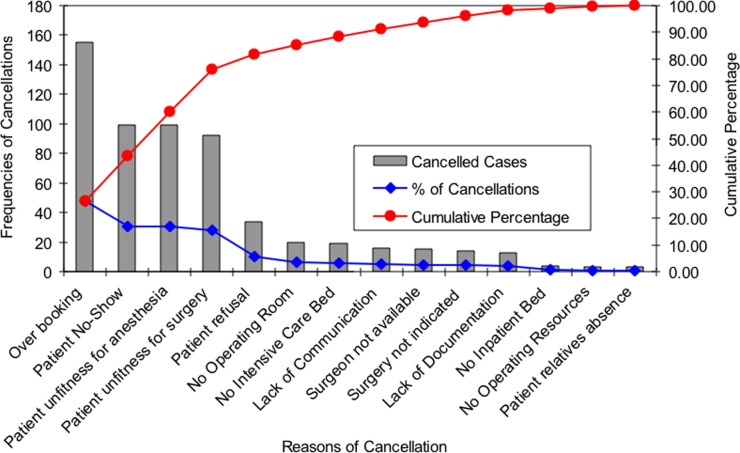
Some of the most common causes of cancellation were: over-booking, patient no-show, unfit for anesthesia, and unfit for surgery. Those results represented the most frequent causes of late cancellation (Table 5) as represented by the breakpoint of the Pareto chart (Figure 2). Our causative approach demonstrated that patients were the source of cancellations in 55.8% of cases followed by the surgeon 31.4% and the hospital 12.8%.
Table 5.
Reasons for cancellation.
| Reasons of cancellation | Cancelled cases | % of Cancellations | Cumulative percentage | Standard error |
|
| ||||
| Over booking | 155 | 26.45 | 26.45 | 0.1475 |
|
| ||||
| Patient no-show | 99 | 16.89 | 43.34 | 0.1253 |
|
| ||||
| Unfitness for anesthesia | 99 | 16.89 | 60.24 | 0.1253 |
|
| ||||
| Unfitness for surgery | 92 | 15.70 | 75.94 | 0.1217 |
|
| ||||
| Patient refusal | 34 | 5.80 | 81.74 | 0.0782 |
|
| ||||
| No operating room | 20 | 3.41 | 85.15 | 0.0607 |
|
| ||||
| No intensive care bed | 19 | 3.24 | 88.40 | 0.0592 |
|
| ||||
| Lack of communication | 16 | 2.73 | 91.13 | 0.0545 |
|
| ||||
| Surgeon not available | 15 | 2.56 | 93.69 | 0.0528 |
|
| ||||
| Surgery not indicated | 14 | 2.39 | 96.08 | 0.0511 |
|
| ||||
| Lack of documentation | 13 | 2.22 | 98.29 | 0.0493 |
|
| ||||
| No inpatient bed | 4 | 0.68 | 98.98 | 0.0275 |
|
| ||||
| No operating resources | 3 | 0.51 | 99.49 | 0.0239 |
|
| ||||
| Patient relatives absence | 3 | 0.51 | 100.00 | 0.0239 |
|
| ||||
| Total | 586 | 100.00 | ||
|
| ||||
Figure 2.
Reasons of cancellation.
The aim of the study was not compare the percentages of cancellation between the different types of surgery and therefore, we didn't apply the t-test and chi-squared test.
The qualitative study performed only for the first four causes of cancellation responsible for the majority of cancellations, revealed many underlying causes behind each apparent cause of cancellation. It was also found that the same underlying cause was mostly behind many of the apparent causes (Table 6). Our results of the qualitative approach found this main underlying cause of cancellations to point to the bed crisis.
Table 6.
Underlying causes of cancellation.
| Apparent reasons | Underlying reasons | Examples |
|
| ||
| Over booking | Bed crisis | Irregular number of weekly admissions per session and per surgeon |
|
| ||
| Bed crisis | Bypass of admission office through the emergency department | |
|
| ||
| Bed crisis | Forced admission through the Day Care Unit | |
|
| ||
| Bed crisis | Daily waiting list for replacement in case of cancellation | |
|
| ||
| Lack of communication | No coordination between the surgeons who share the same session | |
|
| ||
| No restrictive rules | No limitation for the booked cases | |
|
| ||
| No restrictive rules | Surgeon over estimation | |
|
| ||
| Limited operating time | Shortage of operating sessions per surgical team | |
|
| ||
| Ethical pressure on the surgeon | Discovery of a cancer: not emergent but cannot wait | |
|
| ||
| Social pressure on the surgeon | School holidays | |
|
| ||
| No-show | Bed crisis | Booking is not at a convenient time for the patient |
|
| ||
| Bed crisis | Omission due to long waiting time | |
|
| ||
| Bed crisis | Reorientation to another hospital if urgent surgery | |
|
| ||
| Bed crisis | No private room for the patients who want privacy | |
|
| ||
| Incomplete information | Language barrier without a check for understanding | |
|
| ||
| Unfit for anesthesia | Bed crisis | Expiry of anesthesia sheet and consent due to the delayed admission |
|
| ||
| Bed crisis | Change of health conditions due to the long waiting time | |
|
| ||
| Bed crisis | Incomplete preparation not to miss the admission date | |
|
| ||
| Lack of communication | Recent inevitable illness such as flu not communicated to the hospital | |
|
| ||
| No admission rules | Bypass of anesthesia consultation not to miss the bed availability | |
|
| ||
| Wrong decision | Involvement of junior doctors | |
|
| ||
| Incomplete information | Language barrier without check for understanding | |
|
| ||
| Unfit for surgery | Bed crisis | Change of indication due to the delayed admission |
|
| ||
| Bed crisis | Incomplete preparation not to delay the admission | |
|
| ||
| Wrong decision | Involvement of junior doctors | |
|
| ||
| Incomplete information | Language barrier without check for understanding | |
|
| ||
Discussion
To follow the theory of constraints analytic process, as described earlier, we will discuss the five focusing steps, step-by-step.
Step 1: Identification of the constraint
The current study of the elective surgical care chain helped us to analyze and understand the real causes of late cancellations. After surgical consultation in the outpatient department, patients are sent for pre-anaesthesia consultation in the same department for the first assessment. Once considered fit for anaesthesia, patients are sent either to the outpatient surgery office or inpatient surgery office to book a bed. Some patients are sent without anesthesia assessment for bed booking if their health conditions do not accept any delay for instance, a positive fine needle biopsy of a breast nodule. Other patients are admitted for observation or for clinical investigation due to lack of evident surgical indication, lack of operating time or due to the critical state that needs intensive care prior to any surgical care. Their booking forms are sent a few days later to the operating theatre reception as elective cases however, they are initially admitted as emergent cases.
The list of outpatients is sent automatically to the operating theatre reception by 3:00 pm the day before surgery and anesthetists assigned for outpatients, see their patients for the second assessment on the day of surgery, between 7:00–8:00 am. The list of inpatients is usually sent to the operating theatre reception before 3:00 pm or later, only if the patient is admitted and has a bed. “No inpatient bad” refers to a few patients scheduled as outpatients and who need admission. This happens due to two main reasons:
-
(1)
the patients' health conditions change and they cannot be discharged after surgery without risk or,
-
(2)
when the surgeon wants to do an urgent surgery that needs admission, he schedules the patient as a day care case and indicates the admission once the surgery is done. This will give the patient full priority and pushes the admission office to provide a bed.
Regarding ICU beds, their availability is not checked before admission and the bed is booked once the patient is admitted. Even booked early, the bed can be taken by another critical case. Hence, booking for admission does not ensure the admission due to the bed crisis. The anesthetists assigned for inpatients pre-anesthesia assessment will see their patients for the second assessment after 3:00 pm, the same day, or on the day of surgery, before 7:00 am, if the patient is admitted late in the evening. Sometimes, it will be the first assessment if the patient was not previously seen in the outpatient anesthesia clinic.
Once the booking form reaches the operating theatre, either before 3:00 pm or later, the case is considered booked and is added to the operating list without delay. Any removal from this list is considered a cancellation. In our hospital, elective surgery is performed six days a week, from 7:00 am to 10:00 pm. Over-booking therefore isn't only an issue of OR time, it is due mainly to the following three reasons:
-
(3)
completion of a program that needs more than fifteen hours;
-
(4)
surgeons' exhaustion when someone else cannot perform the surgery;
-
(5)
overlap when the same session is shared between surgeons of the same team.
The quantitative approach
Our rate of elective surgery cancellations is comparable to the rates reported in studies of other hospitals such as 13.2% at a major Australian tertiary hospital, (3) 13.2% and 13.3% at a United States Californian Hospital, (16) 9% and 13% at United States Chicago Hospital (13) and 12.4% in a German University Hospital. (23) In our study, there was no significant difference between inpatient (12.52%) and outpatient cancellation rates (15.3%) however, the proportions of their causes are different. We categorized the types of surgery according to their rates of cancellations. Cardio-thoracic surgery and ear-nose-throat surgery were associated with higher cancellation rates. Cardio-thoracic surgery is usually associated with a lot of complications that prolong the time of surgery and consume a lot of time and energy from a surgical team, while ear-nose-throat surgery cases are mainly tracheotomies and their cancellations are secondary to the patients unstable health condition. Orthopedic, general and urologic surgeries were found to have the highest absolute number of cancellations however, there was a difference between inpatients and outpatients regarding the rank of the types of surgery.
According to Pareto's Principle, the minority of causes is always responsible for the majority of effects. (24) In our study, we used the number of cancellations as an indicator. Comparing the rates of cancellations of each surgery, we found the highest rates for ear-nose-throat surgery and cardio-thoracic surgery cases (Table 3). The reduction of their rates of cancellations will not have a significant effect on the overall number of cancellations due to their small proportion among other types of surgery.
Contrariwise, applying Pareto's Principle on the types of surgery, we found that for both outpatients or inpatients, three types of surgery were responsible for 76.62% of the cancellations (Table 4) which is well represented by the breakpoint of the Pareto's chart (Figure 1). However, their respective rates of cancellations are neither the highest nor the lowest. Following the same principle, any reduction in the rates of cancellations for those types of surgery will significantly affect the overall number of cancellations including their financial and social costs. In our opinion, any effort to reduce the cancellations should be directed at orthopaedic, urologic and general surgery.
Applying Pareto's Principle on the causes of cancellations, we found that four causes are responsible for 75.94% of cancellations (Table 5). These causes are over-booking, patient no-show, unfitness for anesthesia and unfitness for surgery. Any reductions for the causes of those cancellations will significantly affect the overall rate of cancellations.
The qualitative approach
From a classical point of view, efforts must focus on all causes of cancellation and all types of surgery starting with the most important causes and surgeries. A problem with this approach however, is that the causes of cancellations identified in this study are actually categories, and trying to evaluate each elementary cause will lead to a very long list of causes that practically would be difficult to manage.
Following the theory of constraints, late cancellation is not a problem but just an undesirable effect. The first step aims to identify the main underlying cause. It is interesting to note that according to Pareto's Principle, the four major causes of cancellation in this study, which are over-booking, patient no-show, unfitness for anesthesia and unfitness for surgery, are also the major determinants of cancellations. In addition, the analysis of each of those four apparent major causes uncovers many underlying causes. Some of the most common underlying causes are presented in Table 6. The most common and most frequent underlying cause is evidently, the bed crisis. Hence, it is the core problem and the weakest link in the surgical care chain. The bed crisis restricts the whole system output. This is confirmed by the huge pre-admission waiting list. Bed crisis is also reflected in many surgeons' behaviors, patient behaviors and clinical conditions (Table 6). Table 6 includes the main apparent causes of cancellation with their respective underlying causes. Each underlying cause is followed by an example illustrating how it leads to the apparent effect.
In our opinion, there is no doubt that our actual constraint is the bed crisis but nevertheless, it remains a probable core problem and can only be confirmed by the dramatic improvement obtained by the following steps of the theory of constraints cycle.
Step 2: Exploitation of the constraint
The output of the constraint (bed availability) restricts the output of the whole system. Improvement of bed availability is the easiest and most effective way to improve the output when taking everything into consideration. It aims to maximize the utilization and productivity of the beds. The following solutions were exploited:
-
•
Avoidance of preoperative admission, (25)
-
•
Reallocation of inpatient to outpatient beds everytime the type of surgery allows, (26–28)
-
•
Reduction of patient no-show by good communication, (29–35)
-
•
Adequate preparation of the patient by providing sufficient information, (36–39)
-
•
Pre-admission reassessment of the patient by the nurse, the surgeon and the anesthetist, (40–42)
-
•
Revision of admission policies to provide priority care for emergent and urgent admissions and to reduce the risk of service disturbance. (43–46)
Consideration of non-constraint activity rather than the effective solutions provided, would drain resources and would have no proven gains.
Once bed availability is no longer a constraint, we can go directly to Step 5, starting a new cycle of investigation and suggesting improvement. Otherwise, the next step, the subordination of the other processes, might be an option.
Step 3: Subordination of all other processes to above decision
The bed crisis was identified as the constraint in our study and therefore we should subordinate activities upstream such as recruitment at the OPD (outpatient department) or downstream like scheduling at the OT (operating theatre) to get the best synchronization.
The first subordination should be to limit the recruitment at the OPD according to the capacity of admission and not to recruit patients unless well investigated. (47) This would result in an immediate decrease in the pre-admission waiting list.
The second subordination should involve not putting any patient on OR lists unless they are admitted as an inpatient or after having paid fees and confirmed their availability by phone call the day before surgery for outpatients. This would avoid any preoperative waiting time for patients already admitted. Priority of scheduling would then be given to those patients already admitted for investigations or treatment such as trauma patients and those admitted due to their medical conditions.
The third subordination for the optimization of the operating theater performance by innovative and creative management, should involve the important role of the operating theater manager or coordinator. (48) A slight extension beyond the allocated fifteen hours of surgery time wherever possible, might be beneficial when comparing its effect to the harmful effect of a cancellation. (49)
Once bed availability is no longer a constraint, we can go directly to Step 5, starting a new cycle of investigation and suggesting improvement. Otherwise, the next steps, the elimination of the constraint, will be the ultimate solution.
Step 4: Elimination of the constraint
If Step 2 and 3 are not sufficiently implemented, the elimination of the constraint is still a must. This may require major changes to the actual system, in our case either by reallocation of the medical beds to surgical beds or by posting some types of surgery outside the hospital itself. These solutions are the ultimate steps to improvement.
Step 5: Avoidance of inertia
Once the bed crisis is no longer identified as a constraint, another cycle must start to look for new constraints limiting the workflow of the surgical care service. Only this cyclic and dynamic process of investigation for the constraints can ensure continual improvement.
Conclusion
Employing a managerial approach using the theory of constraints, we demonstrated that late cancellations of scheduled elective surgery in Hamad General Hospital are not more than an undesirable effect of the bed crisis. Workable and effective solutions to reduce cancellation rate are provided in this study. Confirmation of the finding will be obtained by a net improvement following the different steps of implementation. If no improvement is observed, a new cycle has to start looking for another core problem. This continuous and cyclic process of the theory of constraints when applied to the surgical care service is what will ensure its ongoing improvement.
Acknowledgements
We thank Ms. Amal Jobrane, Dr. Magadi Pramod and Dr. Zakaria El Rasheid for their help.
References
- 1.Perroca MG, Jericó MC, Facundin SD. Surgery cancelling at a teaching hospital: implications for cost management. Rev Latino-am Enfermagem. 2007;15(5):1018–1024. doi: 10.1590/s0104-11692007000500021. [DOI] [PubMed] [Google Scholar]
- 2.Jonnalagadda R, Walrond ER, Hariharan S, Walrond M, Prasad C. Evaluation of the reasons for cancellations and delays of surgical procedures in a developing country. Int J Clin Pract. 2005;59(6):716–720. doi: 10.1111/j.1742-1241.2004.00354.x. [DOI] [PubMed] [Google Scholar]
- 3.Schofield WN, Rubin GL, Piza M, Lai YY, Sindhusake D, Fearnside MR, Klineberg PL. Cancellation of operations on the day of intended surgery at a major Australian referral hospital. Med J Aust. 2005;182(12):612–615. doi: 10.5694/j.1326-5377.2005.tb06846.x. [DOI] [PubMed] [Google Scholar]
- 4.Dexter F, Wachtel RE. Analysing day-of-surgery cancellation rates. Anaesth Intensive Care. 2009;37(5):858. author reply 58-9. [PubMed] [Google Scholar]
- 5.Gonzalez-Arevalo A, Gomez-Arnau JI, delaCruz FJ, Marzal JM, Ramirez S, Corral EM, García-del-Valle S. Causes for cancellation of elective surgical procedures in a Spanish general hospital. Anaesthesia. 2009;64(5):487–493. doi: 10.1111/j.1365-2044.2008.05852.x. [DOI] [PubMed] [Google Scholar]
- 6.Haana V, Sethuraman K, Stephens L, Rosen H, Meara JG. Case cancellations on the day of surgery: an investigation in an Australian paediatric hospital. ANZ J Surg. 2009;79(9):636–640. doi: 10.1111/j.1445-2197.2009.05019.x. [DOI] [PubMed] [Google Scholar]
- 7.Ahmed T, Khan M, Khan FA. Cancellation of surgery in patients attending the preoperative anaesthesia assessment clinic: a prospective audit. J Pak Med Assoc. 2009;59(8):547–550. [PubMed] [Google Scholar]
- 8.Hand R, Levin P, Stanziola A. The causes of cancelled elective surgery. Qual Assur Util Rev. 1990;5:2–6. doi: 10.1177/0885713x9000500102. [DOI] [PubMed] [Google Scholar]
- 9.Seim AR, Fagerhaug T, Ryen SM, Curran P, Saether OD, Myhre HO, Sandberg WS. Causes of cancellations on the day of surgery at two major university hospitals. Surg Innov. 2009;16(2):173–180. doi: 10.1177/1553350609335035. [DOI] [PubMed] [Google Scholar]
- 10.Yoon SZ, Lee SI, Lee HW, Lim HJ, Yoon SM, Chang SH. The effect of increasing operating room capacity on day-of-surgery cancellation. Anaesth Intensive Care. 2009;37(2):261–266. doi: 10.1177/0310057X0903700203. [DOI] [PubMed] [Google Scholar]
- 11.Knox M, Myers E, Hurley M. The impact of pre-operative assessment clinics on elective surgical case cancellations. Surgeon. 2009;7(2):76–78. doi: 10.1016/s1479-666x(09)80019-x. [DOI] [PubMed] [Google Scholar]
- 12.Argo JL, Vick CC, Graham LA, Itani KM, Bishop MJ, Hawn MT. Elective surgical case cancellation in the Veterans Health Administration system: identifying areas for improvement. Am J Surg. 2009;198(5):600–606. doi: 10.1016/j.amjsurg.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 13.Ferschl MB, Tung A, Sweitzer B, Huo D, Glick DB. Preoperative clinic visits reduce operating room cancellations and delays. Anesthesiology. 2005;103(4):855–859. doi: 10.1097/00000542-200510000-00025. [DOI] [PubMed] [Google Scholar]
- 14.Rai MR, Pandit JJ. Day of surgery cancellations after nurse-led pre-assessment in an elective surgical centre: the first 2 years. Anaesthesia. 2003;58(7):692–699. doi: 10.1046/j.1365-2044.2003.03189_3.x. [DOI] [PubMed] [Google Scholar]
- 15.van Klei WA, Moons KG, Rutten CL, Schuurhuis A, Knape JT, Kalkman CJ, Grobbee DE. The effect of outpatient preoperative evaluation of hospital inpatients on cancellation of surgery and length of hospital stay. Anesth Analg. 2002;94(3):644–649. doi: 10.1097/00000539-200203000-00030. [DOI] [PubMed] [Google Scholar]
- 16.Pollard JB, Olson L. Early outpatient preoperative Anaesthesia assessment: does it help to reduce operating room cancellations? Anesth Analg. 1999;89(2):502–505. doi: 10.1097/00000539-199908000-00048. [DOI] [PubMed] [Google Scholar]
- 17.Kleinfeldt AS. Preoperative phone calls. Reducing cancellations in pediatric day surgery. AORN J. 1990;51(6):1559–1564. doi: 10.1016/s0001-2092(07)66908-7. [DOI] [PubMed] [Google Scholar]
- 18.Tung A, Dexter F, Jakubczyk S, Glick D. The limited value of sequencing cases based on their probability of cancellation. Anesth Analg. 2010;111(3):749–756. doi: 10.1213/ANE.0b013e3181e661e8. [DOI] [PubMed] [Google Scholar]
- 19.Dexter F, Shi P, Epstein R. Descriptive study of case scheduling and cancellations within 1 week of the day of surgery. Anesth Analg. 2012;115(5):1188–1195. doi: 10.1213/ANE.0b013e31826a5f9e. [DOI] [PubMed] [Google Scholar]
- 20.Dexter F, Marcon E, Epstein RH, Ledolter J. Validation of statistical methods to compare cancellation rates on the day of surgery. Anesth Analg. 2005;101(2):465–473. doi: 10.1213/01.ANE.0000154536.34258.A8. table of contents. [DOI] [PubMed] [Google Scholar]
- 21.Goldratt EM, Cox J. The Goal – A Process of Ongoing Improvement. Croton-on-Hudson, NY: North River Press; 1984. [Google Scholar]
- 22.Breen AM, Burton-Houle T, Aron DC. Applying the theory of constraints in health care: Part 1–The philosophy. Qual Manag Health Care. 2002;10(3):40–46. doi: 10.1097/00019514-200210030-00010. [DOI] [PubMed] [Google Scholar]
- 23.Schuster M, Neumann C, Neumann K, Braun J, Geldner G, Martin J, Spies C, Bauer M, for the CASCAES Study Group The effect of hospital size and surgical service on case cancellation in elective surgery: results from a prospective multicenter study. Anesth Analg. 2011;113(3):578–585. doi: 10.1213/ANE.0b013e318222be4d. [DOI] [PubMed] [Google Scholar]
- 24.Grosfeld A, Ronen B, Kozlovsky N. The Pareto managerial principle: when does it apply? Int J Prod Res. 2007;45(10):2317–2325. [Google Scholar]
- 25.Keranen J, Soini EJ, Ryynanen OP, Hietaniemi K, Keranen U. Economic evaluation comparing from home to operation same day admission and preoperative admission one day prior to the surgery process: a randomized, controlled trial of laparoscopic cholecystectomy. Curr Med Res Opin. 2007;23(11):2775–2784. doi: 10.1185/030079907x233223. [DOI] [PubMed] [Google Scholar]
- 26.Povysil J. [One-day surgery] Osterr Krankenpflegez. 1986;39:78–81. [PubMed] [Google Scholar]
- 27.Ranieri E, Caprio G, Fobert MT, Civitelli L, Ceccarelli F, Barberi S, Virno F. One-day surgery in a series of 150 breast cancer patients: efficacy and cost-benefit analysis. Chir Ital. 2004;56(3):415–418. [PubMed] [Google Scholar]
- 28.Gilliard N, Eggli Y, Halfon P. A methodology to estimate the potential to move inpatient to one day surgery. BMC Health Serv Res. 2006;6:78. doi: 10.1186/1472-6963-6-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dervin JV, Stone DL, Beck CH. The no-show patient in the model family practice unit. J Fam Pract. 1978;7(6):1177–1180. [PubMed] [Google Scholar]
- 30.Taylor PJ. The no-show patient never has the last appointment of the day. CMAJ. 1991;144(7):916–917. [PMC free article] [PubMed] [Google Scholar]
- 31.Mantyjarvi M. No-show patients in an ophthalmological out-patient department. Acta Ophthalmol (Copenh) 1994;72(3):284–289. doi: 10.1111/j.1755-3768.1994.tb02760.x. [DOI] [PubMed] [Google Scholar]
- 32.Stickney P. What works. Telephone reminder system works with patient software to reduce no-show rate. Health Manag Technol. 1997;18(6):46. [PubMed] [Google Scholar]
- 33.Guse CE, Richardson L, Carle M, Schmidt K. The effect of exit-interview patient education on no-show rates at a family practice residency clinic. J Am Board Fam Pract. 2003;16(5):399–404. doi: 10.3122/jabfm.16.5.399. [DOI] [PubMed] [Google Scholar]
- 34.Izard T. Managing the habitual no-show patient. Fam Pract Manag. 2005;12(2):65–66. [PubMed] [Google Scholar]
- 35.Goldstein A. Are your patient no-show strategies robbing you blind? Dent Today. 2009;28(11):146. 48-49. [PubMed] [Google Scholar]
- 36.Rittersma J, Casparie AF, Reerink E. Patient information and patient preparation in orthognathic surgery: a medical audit study. J Maxillofac Surg. 1980;8(3):206–209. doi: 10.1016/s0301-0503(80)80102-0. [DOI] [PubMed] [Google Scholar]
- 37.Reading AE. Psychological preparation for surgery: patient recall of information. J Psychosom Res. 1981;25(1):57–62. doi: 10.1016/0022-3999(81)90084-2. [DOI] [PubMed] [Google Scholar]
- 38.Baskerville PA, Heddle RM, Jarrett PE. Preparation for surgery: information tapes for the patient. Practitioner. 1985;229(1405):677–678. [PubMed] [Google Scholar]
- 39.Rittersma J. Patient information and patient preparation in orthognathic surgery. The role of an information brochure a medical audit study. J Craniomaxillofac Surg. 1989;17(6):278–279. doi: 10.1016/s1010-5182(89)80096-4. [DOI] [PubMed] [Google Scholar]
- 40.Phipps CG. Effectiveness of the clinical nurse specialist in preadmission testing. Health Matrix. 1987;5(4):23–27. [PubMed] [Google Scholar]
- 41.Koay CB, Marks NJ. A nurse-led preadmission clinic for elective ENT surgery: the first 8 months. Ann R Coll Surg Engl. 1996;78(1):15–19. [PMC free article] [PubMed] [Google Scholar]
- 42.Gilmartin J. Day surgery: patients' perceptions of a nurse-led preadmission clinic. J Clin Nurs. 2004;13(2):243–250. doi: 10.1046/j.1365-2702.2003.00836.x. [DOI] [PubMed] [Google Scholar]
- 43.Ferguson J, Alpert JJ. A study of hospital admission rules during pediatric residency training. J Med Educ. 1980;55(10):876–878. doi: 10.1097/00001888-198010000-00011. [DOI] [PubMed] [Google Scholar]
- 44.Siegel SH. How OBRA admission rules affect nursing facilities. Healthc Financ Manage. 1990;44(9):52–53. 56-59. [PubMed] [Google Scholar]
- 45.Walker BC, Haslett T. The dynamics of local rules in hospital admission processes. Aust Health Rev. 2003;26(3):98–106. doi: 10.1071/ah030098. [DOI] [PubMed] [Google Scholar]
- 46.Dombi WA. Patient admission, service, and discharge: rules to survive by. Caring. 2004;23(4):18–21. [PubMed] [Google Scholar]
- 47.Farasatkish R, Aghdaii N, Azarfarin R, Yazdanian F. Can preoperative anaesthesia consultation clinic help to reduce operating room cancellation rate of cardiac surgery on the day of surgery? Middle East J Anesthesiol. 2009;20(1):93–96. [PubMed] [Google Scholar]
- 48.Stepaniak S, Mannaerts G, de Quelerij M, de Vries G. The effect of the operating room coordinator's risk appreciation on operating room efficiency. Anesth Analg. 2009;108(4):1249–1256. doi: 10.1213/ane.0b013e318195e109. [DOI] [PubMed] [Google Scholar]
- 49.Tessler M, Kleiman S, Huberman M. A “zero tolerance for overtime” increases surgical per case costs. Can J Anaesth. 1997;44(10):1036–1041. doi: 10.1007/BF03019223. [DOI] [PubMed] [Google Scholar]