Abstract
Epidermoid cysts, true dermoid cysts and teratoid cysts compose the spectrum of cystic teratomas, which are defined as neoplasms whose tissue are derivatives of more than one germ layer, foreign to that part of the body from which the tumor arises. Epidermoid cysts of the floor of the mouth are rare lesions and are much less common than dermoid cysts in the head and neck. This case reports a 43-year-old male patient who presented with a longstanding midline swelling in the submental region. Initial imaging was done using ultrasound followed by computed tomography (CT) scan. Biopsy was taken and revealed a cyst wall lined with epidermal squamous epithelium along with areas of focal ulceration suggesting chronic inflammatory changes of the wall of the epidermoid cyst.
There are characteristic and even pathognomonic imaging features of epidermoid cysts at the floor of the mouth in ultrasound and CT scan. Imaging has an important role in the surgical management plan according to the size and location of the cyst in relation to geniohyoid and mylohyoid muscles.
Keywords: Epidermoid cyst, cystic teratoma, floor of mouth
Introduction
Epidermoid cysts are classified as one type of the spectrum of cystic teratomas, (1) this spectrum describes three closely related histologic cysts including dermoid cysts, epidermoid cysts, and teratoid cysts. (1) These cysts are very rare and represent 0.01% of all oral cavity cysts. (2–4) They constitute 1.6–6.9% of all cysts in the head and neck region. The epidermoid cysts in the neck region are less common than dermoid cysts. (5) Those cysts were reported to occur more frequently in patients between 15 and 35 years, (4,6) but can be seen in all age groups.
Because of their rarity, they are unfamiliar to most radiologists and not well covered in radiologic literature. A patient recently presented to Hamad General Hospital with a large epidermoid cyst arising from the floor of the mouth. Ultrasound and CT scan were performed for this patient and were of significant help in establishing the diagnosis.
Case presentation
We are reporting a 43 year old Pakistani male patient who presented to Hamad General Hospital with multiple known co-morbidities including diabetes mellitus and chronic kidney disease on dialysis. The patient was referred from emergency department to the radiology department because of a large submental swelling. Inspection and palpation of the head and neck revealed a large smooth, doughy and compressible swelling measuring approximately 8 × 7 cm, occupying the submental region and extending to both submandibular regions, giving the double chin appearance. The lesion was painless on palpation, not mobile on tongue protrusion and there was no significant compromise on the oral cavity. The intraoral examination was unremarkable. The history disclosed that the lesion had been slowly progressing over the years. His white blood cell count (WBC) was 12 × 103/ul (normal from 4 to 11 × 103/ul), hemoglobin was 12.3 g/dl (normal from 13 to 17 g/dl), serum glucose was 15.42 mmol/L (normal from 3.3 to 6 mmol/L), serum creatinine was 813 umol/L (normal from 62 to 124 umol/L). The clinical differential diagnosis was abscess collection, cystic hygroma, cystic teratoma and giant ranula.
Ultrasound was initially requested to rule out any collection or abscess formation. Ultrasound was done using 10 MHz linear transducer (Figure 1). The ultrasound was done through a submental approach in the axial and sagittal planes. It showed a relatively well circumscribed midline cystic structure measuring approximately 8.3 × 7.7 × 5 cm with multiple rounded lobulated echogenic structures within. No significant vascularity was noted. No associated enlarged cervical lymph nodes were seen.
Figure 1.

Ultrasound showing well-circumscribed midline cystic structure, measuring 8.3 × 7.7 cm with multiple rounded lobulated echogenic structures within.
A CT scan was subsequently performed in axial sections followed by reconstruction of images into sagittal and coronal sections. This showed a well-defined encapsulated cystic mass lesion in the floor of the mouth occupying the submental region containing low attenuation rounded structures of fat density (Figure 2).
Figure 2.
Computed tomography of the neck in coronal (a) sagittal (b) and axial (c) planes showing a well-defined encapsulated cystic mass lesion in the floor of the mouth occupying the submental and submandibular regions and containing rounded fat density structures.
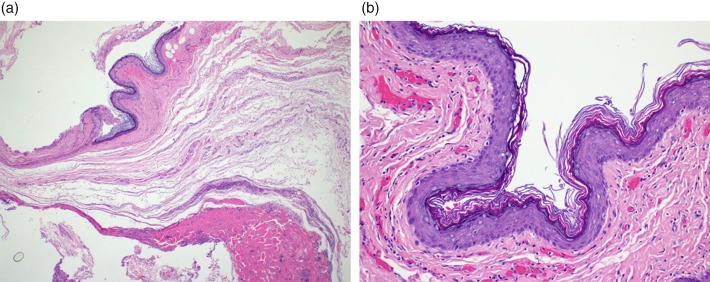
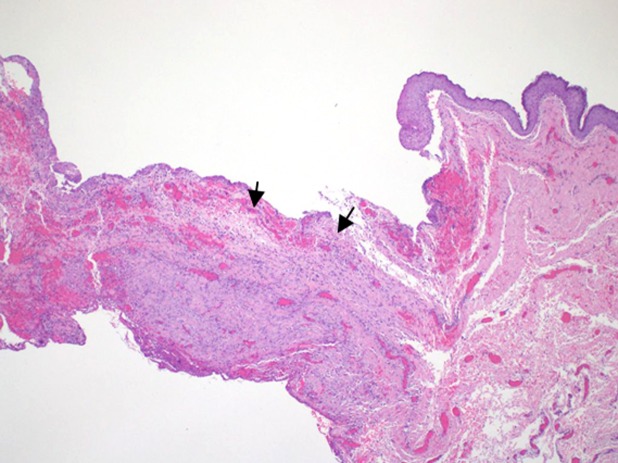
Incisional biopsy through an extraoral approach was done. Histopathology revealed portions of a cyst lined by multilayered epidermal-type benign squamous epithelium (Figures 3). There was focal ulceration with organizing fibrosis and chronic inflammation in the cyst wall (Figure 4). No adnexal structures were seen in the cyst wall, nor evidence of malignancy. Diagnosis was made as an epidermoid cyst complicated by chronic inflammation of the wall. The patient refused to do any surgery but consented for marsupialization. Follow-up after one year showed no recurrence.
Figure 3 (a&b).
Specimen from the midline submental lesion histopathology. Hematoxylin and eosin (a) and magnified view (b) showing fragmented cyst lined by keratinizing multilayered benign squamous epithelium.
Figure 4.
Focal ulceration (black arrows) in the cyst wall with organizing fibrosis and chronic inflammation in the cyst wall.
Discussion
Epidermoid cysts are classified as one type of the spectrum of cystic teratomas. Histologically all cystic teratomas are lined by an epidermal-type squamous epithelium; consequently, the lumen of the cyst is filled with a mixture of keratin and sebaceous material. The cyst lining determines the histological category of the cyst: epidermoid, if only epidermal-type squamous epithelium lines the cyst; dermoid, if skin adnexa exist; or teratoid, if there are tissue derivatives from other (mesodermal and endodermal) germinal layers. (2) Although dermoid cysts represent a separate entity, the term “dermoid cysts” is sometimes used to indicate all the three categories. (2) The gross pathological/surgical features of epidermoid cysts are oily or cheesy, tan, yellow, white material and the cyst wall is a fibrous capsule usually 2–6 mm in thickness. The cyst that was presented in this case was lined by epidermal-type squamous epithelium with no adnexal structures identified and therefore the diagnosis was an epidermoid cyst.
Epidermoid cysts develop as a slowly growing mass over years; several theories have been proposed to explain the development of these cysts. They may result from entrapment of ectodermal tissue of the first and second branchial arches during fetal development. They could represent a variant from the thyroglossal cyst. Also, prior surgical or accidental events may result in traumatic implantation of epithelial cells into deeper tissue. (7) In our case, there was no identified trauma history noted.
Imaging has an important role in raising the primary diagnosis and also for classification of those cysts according to its relation to the muscles.
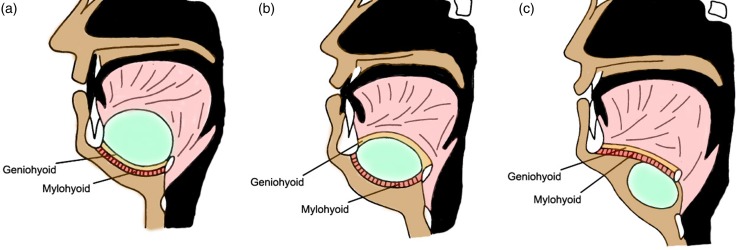
Ultrasound is the initial diagnostic modality; the epidermoid cysts are seen as well-defined cysts with multiple well-defined dependent, echogenic nodules within the cyst. (5) CT scan shows a unilocular cyst with homogenous, hypo-attenuating (0–18 HU) fluid material that contains multiple hypo-attenuating fat density nodules giving a “sack of marbles” appearance; a feature virtually pathognomonic for a dermoid cyst in this location. (1,8) On MRI, it shows fluid signal character in the form of high signal in tbl2WI and low signal in tbl1WI however, diffuse high tbl1 signal can be due to high protein content, and the areas of fat component will show low signal on fat suppressed images. MR imaging facilitates exact visualization of the location and extent of cystic lesions in the floor of the mouth and is useful for determining their relationship to the surrounding muscles (Figure 5). The mylohyoid muscle, which separates the sublingual spaces from the submental and submandibular spaces, is the key structure in the floor of the mouth. Depending on the topographic relationship between a lesion and the mylohyoid muscle, either an intraoral or cervical surgical approach is used. Axial and coronal images are used to optimize visualization of this relationship. (9) A sagittal orientation is helpful for cysts located in the midline. (9)
Figure 5.
Diagram of the topographic relationship between a cyst and muscles of the floor of the mouth. (a) cyst located above the geniohyoid and mylohyoid muscle (b), cyst located between genihyoid and mylohyoid muscles (c) cyst located beneath geniohyoid and mylohyoid muscles [Modified from reference (9)].
The differential diagnosis includes developmental lesions (such as lymphangioma, ranula and thyroglossal cyst), infectious lesions (cellulitis of the floor of the mouth, necrotizing lymphadenitis, and abscess formation), tumors (such as salivary gland tumors) and others such as hemangioma and lipoma, are also to be considered. Lymphangioma usually is a multilocular trans-spatial insinuating cystic mass. Thyroglossal cysts are usually a midline unilocular cystic mass that can mimic an epidermoid cyst if it is in a supra-hyoid location and in the posterior root of the tongue; however, it has no complex elements (no fat or calcifications). Simple ranula is a unilocular cystic mass with non-enhancing wall which may exactly mimic epidermoid cysts if there is fluid only. Diving ranula is a simple ranula that ruptures from the subligual to subamandibular space; it has comet tail shape with the tail in the collapsed sublingual space (tail sign) and head in the submandibular space. Oral cavity abscess is usually diagnosed clinically and on CT scan. There will be a cystic mass surrounded by a rim of enhancement in addition to extensive soft tissue cellulitis-edema. (7,10) Minor salivary gland malignancies such as sublingual gland tumors will appear as an enhancing mass with irregular borders in contrast enhanced CT; on MRI it shows inhomogenous signal intensity in tbl1WI and tbl2WI with heterogeneous enhancement after gadolinium-based contrast injection. (7,10)
The expected treatment includes complete surgical enucleation (3–6,8) without rupturing the cyst as the intraluminal contents may act as irritants to fibrovascular tissues, producing postoperative inflammation. (1,5,8) However, marsupialization is another alternative for management of large cysts. (11)
Lesions above the mylohyoid muscles are operated on intraorally, whereas those below the muscle are removed via an incision in the neck. (9) However, if there is a very large sublingual cyst above the mylohyoid muscle, an extraoral approach may be preferred. An intraoral approach avoids a conspicuous scar, and the recovery time is shorter. (9)
Complications of epidermoid cysts of the floor of the mouth include disfigurement, occasionally difficulty in swallowing if it reaches huge proportions and airway compromise. Also, it can be secondarily infected. (12) Malignant changes are rare, a five percent rate of malignant transformation of oral dermoid cysts have been reported by some authors, but only for the teratoid type. (3)
Prognosis is good after excision with a very low incidence of relapse. (3,4)
Conclusion
Ultrasound and CT scan have an important role in establishing the diagnosis of epidermoid cysts of the floor of the mouth and help differentiation from other floor of the mouth cystic lesions.
Imaging also has an important role in guiding surgeons when choosing the best surgical approach for epidermoid cysts of the floor of the mouth.
References
- 1.Mammen S, Korulla A, Paul MJ. An epidermal cyst in the floor of the mouth: a rare presentation. J Clin Diagn Res. 2013;7:381–382. doi: 10.7860/JCDR/2013/4165.2776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kandogan T, Koç M, Vardar E, Selek E, Sezgin O. Sublingual epidermoid cyst: a case report. J Med Case Rep. 2007;1:87. doi: 10.1186/1752-1947-1-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tsirevelou P, Papamanthos M, Chlopsidis P, Zourou I, Skoulakis C. Epidermoid cyst of the floor of the mouth: two case reports. Cases J. 2009;2:9360. doi: 10.1186/1757-1626-2-9360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Seah TE, Sufyan W, Singh B. Case report of a dermoid cyst at the floor of the mouth. Ann Acad Med Singapore. 2004;33(4):77–79. [PubMed] [Google Scholar]
- 5.Hiremath R, Chandrashekarayya SH, Manswini Pol TJ, Anegundi KR. A rare case of a submental epidermoid cyst: a case report. J Clin Diagn Res. 2011;5:1452–1453. [Google Scholar]
- 6.Jha AK, Sahoo NK. An unusual case of submental epidermoid cyst in a ten years old child: a case report. Int J Case Rep Image. 2011;2(10):10–13. [Google Scholar]
- 7.Yousem D, Grossman R. Neuroradiology: The Requisites. 3rd ed. Philadelphia, PA: Mosby; 2010. ISBN: 978-0323045216. [Google Scholar]
- 8.Chaturvedi J, Hegde K, Ananthamurthy A, Nayar R. Submental epidermoid cyst- a case report. Internet J Head Neck Surg. 2009;4(2) [Google Scholar]
- 9.Vogl TJ, Steger W, Ihrler S, Ferrera P, Grevers G. Cystic masses in the floor of the mouth: value of MR imaging in planning surgery. AJR Am J Roentgenol. 1993;161(1):183–186. doi: 10.2214/ajr.161.1.8517299. [DOI] [PubMed] [Google Scholar]
- 10.Harnsberger H, Glastonbury C. Diagnostic Imaging: Head and Neck. 2nd ed. Philadelphia, PA: Amirsys; 2011. ISBN: 978-1931884785. [Google Scholar]
- 11.Jham BC, Duraes GV, Jham AC, Santos CR. Epidermoid cyst of the floor of the mouth: a case report. J Can Dent Assoc. 2007;73(6):525–528. [PubMed] [Google Scholar]
- 12.Cortezzi W, De Albuquerque EB. Secondarily infected epidermoid cyst in the floor of the mouth causing a life-threatening situation: report of a case. J Oral Maxillofac Surg. 1994;52(7):762–764. doi: 10.1016/0278-2391(94)90496-0. [DOI] [PubMed] [Google Scholar]