Abstract
Background: The prevalence and severity of cancer pain in the outpatient palliative care (PC) setting have not been explored previously in Saudi Arabia (SA). Exploration of this basic information may help in evaluating pain severity in patients new to PC as compared to those with previous PC exposure. Objective: This paper aims to determine the prevalence and severity of cancer pain among new and follow-up patients attending a PC outpatient clinic. Methods: In a PC outpatient setting in a major tertiary hospital in SA, we interviewed adult patients with cancer during their attendance to the clinic. Patients were requested to score the severity of their pain on a 0 to 10 numerical scale. Results: A total of 124 patients were interviewed, of whom 73 (59%) were females. The majority of patients (82.3%) had metastatic disease. The most common cancers were breast (27.4%) and head and neck (15.3%). The majority of patients (85.5%) reported pain, with a median intensity score of 5 and a mean of 4.6. Of those who reported pain, 54 (51%) scored above 4. The mean pain score did not differ between groups of patients according to various characteristics such as age, sex, performance status, type of cancer or encounter type. Conclusion: Pain is a prevalent symptom in new and follow-up cancer patients seen in a PC outpatient setting in SA. Further research on a larger scale is needed to evaluate the magnitude of the problem more comprehensively with emphasis on detailed pain assessment and exploration of the adopted management approaches.
Keywords: cancer pain, palliative care, Saudi Arabia
Introduction
Cancer pain impacts all aspects of patient's wellbeing and is often cited as the most significant among the multiple cancer-related symptoms. (1) Although the treatment of cancer pain has improved in recent decades, prevalence remains unacceptably high worldwide, hence the World Health Organization (WHO) consideration of cancer pain a global health problem. (2)
The total population of Saudi Arabia (SA) is more than 27 million, of which 69% are Saudi nationals. (3) The reporting of more than 12,000 new cancer cases per year in SA is believed to reflect under-reporting. (4,5) In SA, the cancer crude incidence rate is 52.3 per 100,000 and the overall age-standardized incidence is 82.1 per 100,000 population. In males, the five most prevalent malignancies are colorectal followed by non-Hodgkin lymphoma, leukemia, lung and liver. In females, breast cancer is most prevalent, followed by thyroid, colorectal, non-Hodgkin lymphoma and leukemia. In most of the cases the disease is advanced, with regional or distant spread and at this stage treatment is given with palliative intent and the main emphasis placed on palliative care (PC). (4)
Once a provisional diagnosis of cancer is made in a local hospital, the patient is usually referred to a tertiary center for further management. King Faisal Specialist Hospital and Research Center (KFSHRC) in Riyadh, SA, is the country's oldest and largest cancer care center. Patients treated at KFSHRC and other governmental cancer centers receive treatment free of charge including hospital stay, investigations, procedures, outpatient services and cost of prescribed medications.
The PC program at KFSHRC, Riyadh, was the first of its kind in the country and is now more than two decades old. An interdisciplinary team of PC professionals deliver inpatient, outpatient and home care services. The PC program accepts inpatient and outpatient referrals of all age groups, with children being a very small minority of the PC patient population. Although the PC program accepts non-cancer referrals, the great majority of patients referred to the PC program are those with significant burden of malignancy-related symptoms. The PC outpatient clinic at KFSHRC is run by consultants in palliative medicine who have extensive experience working full-time in PC. A postgraduate fellowship program has been established at KFSHRC for more than ten years to provide family physicians and internists with one-year structured training in palliative medicine.
A variety of opioids and adjuvant analgesics are readily available at KFSHRC and the standard approach of managing cancer pain follows the WHO analgesic ladder. (6) The prevalence and severity of cancer pain in the outpatient PC setting have not been explored previously in SA. Exploration of this basic information may help in evaluating pain severity in patients new to PC as compared to those with previous PC exposure. The aim of this paper is to determine the prevalence and severity of cancer pain among new and follow-up patients attending a PC outpatient clinic in a tertiary hospital in SA.
Methods
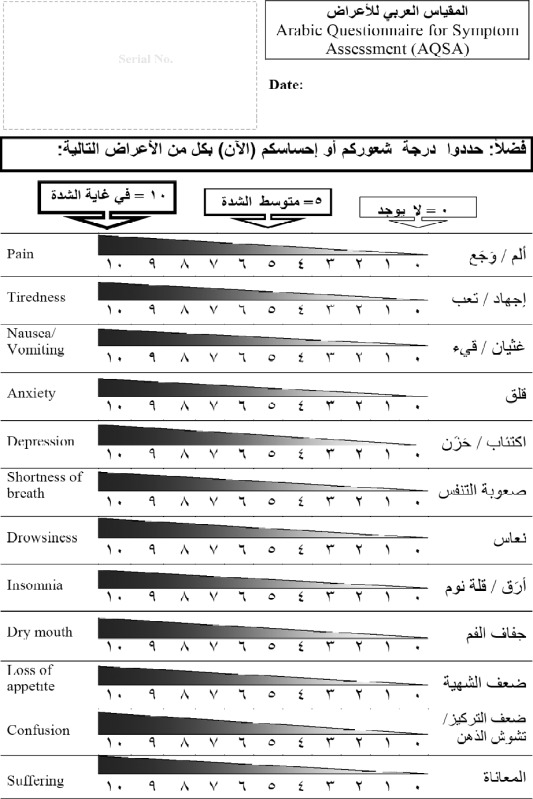
This is a cross-sectional survey exploring the prevalence and intensity of pain in an outpatient PC setting. The target population consisted of cancer patients older than 18 years of age who attended the PC clinic over a period of five months. Patients visiting the PC outpatient for the first time were considered “new” and those returning to clinic after one or more previous visits were labeled as “follow-ups”. For patients visiting the clinic more than once during the study period, only the first visit was included in the study. Enrolled patients had to be oriented to place, time and person, for them to be considered mentally competent to participate in the study. The performance status of patients was assessed using the Palliative Performance Scale (PPS) [Appendix I]. (7) The presence and severity of pain during the outpatient encounter were assessed using the Arabic Questionnaire for Symptom Assessment (AQSA) which is a one page tool designed to detect the presence and quantify the intensity of pain and suffering as well as ten additional symptoms known to be common in cancer patients with advanced disease [Appendix II]. The content of AQSA was unanimously declared valid by three PC experts from SA and the United States of America. The criterion and construct validity of the AQSA as a self-administered tool for assessing symptom severity is currently being tested by an ongoing study lead by the author of this paper (MZA). Although the AQSA was designed to be used as a simple self-administered tool, patients were interviewed and requested to select the scores of their pain severity using the AQSA as a guide. The pain intensity at the time of the clinic visit was determined by every patient according to a 0–10 scoring system, with 0 being no pain at all and 10 being the greatest severity of pain imaginable. Based on this scoring, pain severity was categorized as mild for scores of 1–4, moderate for scores of 5–6 and severe for scores of 7–10. (8) Interviews were all conducted by one of the authors (OA) in order to avoid the possibility of inter-rater variations. The study protocol was approved by the research ethics committee at KFSHRC. Data analysis was performed using the software package SAS version 9.2 (Statistical Analysis System, SAS Institute Inc., Cary, NC, USA). Descriptive data were presented in the form of frequencies and percentages. The statistical tests used to compare means included ANOVA or Student's t-test as appropriate. The level of statistical significance was set at a P value of less than 0.05.
Results
All approached patients accepted to participate in the study. However, a few illiterate elderly patients needed more effort on the part of the interviewer to explain to them the concept of numerically scoring the severity of pain. Of the 124 patients interviewed, 73 (59%) were females. Two thirds of the participants (67%) had not been seen before in the PC clinic while 33% were follow-ups. The youngest patient was 20 years old and the oldest 92 years old, with equal mean and median values (56 years). The majority of patients (102; 82.3%) had metastatic disease. None of the patients who were receiving anti-cancer therapy at the time of the study were treated with curative intent. The most common types of cancer included breast (27.4%), head and neck (15.3%), and genitourinary (12.9%). Most of the patients had a fair performance status at the time of interview, with a median PPS of 70%. Details of patients' characteristics are shown in Table 1.
Table 1.
Patients' demographics
| Mean | Median | Range | |
|
| |||
| Age (in years) | 56 | 56 | 20–92 |
|
| |||
| Palliative Performance Scale (%) | 72 | 70 | 40–100 |
|
| |||
| Frequency | % | ||
|
| |||
| Sex | |||
|
| |||
| Male | 51 | 41 | |
|
| |||
| Female | 73 | 59 | |
|
| |||
| Type of clinic visit | |||
|
| |||
| New | 83 | 67 | |
|
| |||
| Follow-up | 41 | 33 | |
|
| |||
| Cancer type | |||
|
| |||
| Breast | 34 | 27.4 | |
|
| |||
| Head & Neck | 19 | 15.3 | |
|
| |||
| Genitourinary | 16 | 12.9 | |
|
| |||
| Gastrointestinal | 12 | 9.7 | |
|
| |||
| Gynecology | 12 | 9.7 | |
|
| |||
| Lung | 8 | 6.5 | |
|
| |||
| Hematological | 4 | 3.2 | |
|
| |||
| Others | 19 | 15.3 | |
|
| |||
| Total | 124 | 100 | |
|
| |||
Only 18 patients (14.5%) reported no pain while the remaining 106 (85.5%) gave scores ranging from 1 to 10, with a median score of 5. The mean score and standard deviation (SD) were 4.6 and 2; respectively. Of the 106 patients experiencing pain, 54 (51%) scored their pain severity above 4, denoting moderate to severe pain intensity. Figure 1 shows the distribution of pain scores for the study population. The average pain score was not statistically different from one group to another according to various characteristics such as sex, age, type of encounter, performance status or cancer category.
Figure 1.
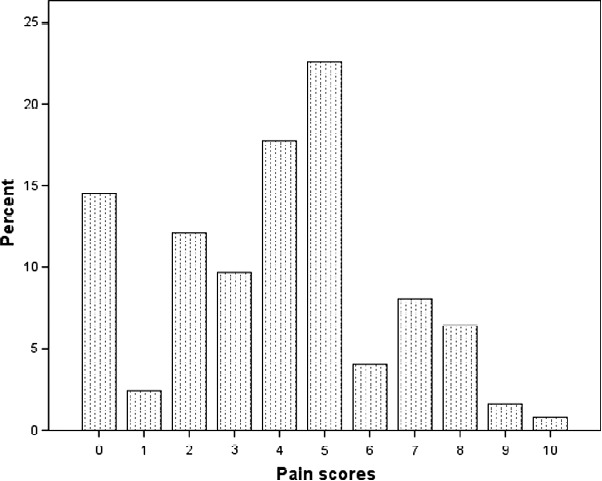
Distribution of pain scores.
Discussion
The relatively young age of the PC population in this study is in agreement with previous reports on PC populations in SA but is not consistent with reports from Western countries. (9–11) This could be due to the fact that less than 3% of the population in SA is above 65 years of age. (12) The finding that the majority of the study population had metastatic disease may be explained by the known trend of delayed referrals to PC at KFSHRC. (9,13) The rules of the PC outpatient clinic require patients to be physically present at the clinic for assessment by the physician at the first encounter. However, for follow-up visits, patients are given the choice to send a relative to get a medication refill on their behalf if they so wish. The extended family structure is the norm for Saudi families. This makes it easy for most patients to send a relative to attend the PC clinic on their behalf. Therefore, patients' relatives commonly attend the PC outpatient clinic at KFSHRC on behalf of patients for the sake of medication refills, hence the lower proportion of follow-up patients as compared to new patients in our study. For patients who are on opioid analgesics, as is the case for most PC patients, clinic appointments are arranged on a monthly basis because the prescription of opioids for outpatients is currently allowed for only a 30-day supply at a time. However, the rules are currently in the process of being possibly changed to allow for a 60-day supply at a time.
Cancer pain is common worldwide and its control is believed to be far from optimal at both the global and local levels. Little is known about cancer pain prevalence in SA. (14) Similar to the findings in our PC clinic, a survey conducted on adult cancer patients in an oncology unit of a teaching hospital in Riyadh without a PC service, found 50% of patients reported moderate to severe cancer pain. (15) A study from Lebanon on cancer inpatients referred to PC showed that more than 95% had cancer pain and about 77% reported severe pain. (16) Internationally speaking, in a systematic review covering a period of four decades, the prevalence of pain in patients with advanced cancer was reported to be 64%. (17) More recently, a Canadian PC survey showed a prevalence of moderate to severe cancer pain approaching 34%. (18) These significant variations in the findings of different studies may be attributable to various factors including variations in the stage of disease, type of cancer, assessment methods and type of healthcare settings in addition to cultural factors. (19–23)
Some Muslim patients may express stoicism and underreport pain, assuming that reporting pain may echo impatience that questions their acceptance of God's will. Based on our experience, this phenomenon is not common. In fact, Islam allows for moderate expression of pain in a way that calls for help but does not reflect impatience and dissatisfaction, such as voicing statements like “why me?”. (24)
Another factor that may have an impact on the reporting as well as the treatment of cancer pain among some Muslim patients is the fact that using substances with sensorium-altering potential is considered religiously prohibited. This is despite the fact that the permissibility of reporting suffering and seeking treatment as well as the use of opioids for medical purposes has been emphasized by Muslim scholars. (25) That being said, we believe that a major obstacle preventing optimal management of cancer pain in SA is the lack of PC services in most hospitals. In fact, PC is available in only a few of the many hospitals treating cancer patients. Acknowledging the scarcity of specialized personnel in PC worldwide, it has been proposed to develop a Saudi nationwide PC program using KFSHRC as a training center and a source of support to other institutions all over the country. (26) Over the last several years, physicians who received training at KFSHRC were able to initiate PC programs in several health institutions in SA.
One limitation in our study is the relatively small number of patients which may have contributed to the fact that our data did not match findings of other reports that have suggested significant association between cancer pain and some correlates. For instance, previous reports have suggested that certain cancer types may be associated with greater prevalence and (or) severity of pain. (17) Kirkova et al., from the Cleveland Clinic have reported significant association between pain prevalence and the performance status of patients. (27) Another shortcoming of our study is that pain assessment was not detailed to include various characteristics of pain and the management modalities implemented. In future research, it may be worthwhile comparing cancer pain prevalence and severity between cancer care facilities with and without PC services. It may also be worth auditing the cancer pain management approach adopted at our PC clinic. Temporal trend of pain severity over sequential visits to the PC clinic may also need to be studied.
Conclusion
Although pain might be less prevalent and (or) severe in our sample than reported elsewhere, it is still a common symptom (and often of significant severity) among cancer patients visiting our PC clinic. Patients seen previously in the PC clinic did not seem to have lower pain scores than those visiting the clinic for the first time. There is an emergent need for more comprehensive research to explore the magnitude and management approaches of cancer pain in Saudi Arabia.
Appendix I
Appendix II
| PPS (%) | Ambulation | Activity &evidence of disease | Self-care | Intake | Conscious level |
|
| |||||
| 100 | Full | Normal activity & work No evidence of disease | Full | Normal | Full |
|
| |||||
| 90 | Full | Normal activity & work Some evidence of disease | Full | Normal | Full |
|
| |||||
| 80 | Full | Normal activity with effort Some evidence of disease | Full | Normal or reduced | Full |
|
| |||||
| 70 | Reduced | Unable to work Significant disease | Full | Normal or reduced | Full |
|
| |||||
| 60 | Reduced | Unable to do hobby/housework Significant disease | Occasional assistance necessary | Normal or reduced | Full or confusion |
|
| |||||
| 50 | Mainly sit/lie | Unable to do hobby/housework Significant disease | Considerable assistance required | Normal or reduced | Full or drowsy or confusion |
|
| |||||
| 40 | Mainly in bed | Unable to do most activities Extensive disease | Mainly assistance | Normal or reduced | Full or drowsy ± confusion |
|
| |||||
| 30 | Totally bed Bound | Unable to do any activity Extensive disease | Total care | Reduced | Full or drowsy ± confusion |
|
| |||||
| 20 | Totally bed Bound | Unable to do any activity Extensive disease | Total care | Minimal to sips | Full or drowsy ± confusion |
|
| |||||
| 10 | Totally bed Bound | Unable to do any activity Extensive disease | Total care | Mouth care only | Drowsy or coma |
|
| |||||
| 0 | Death | – | – | – | – |
|
| |||||
References
- 1.Paice JA, Ferrell B. The management of cancer pain. CA Cancer J Clin. 2011;61(3):157–182. doi: 10.3322/caac.20112. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Access to Controlled Medications Programme: Framework. Geneva, Switzerland: World Health Organization; 2007. Available at: http://www.who.int/medicines/areas/quality_safety/Framework_ACMP_withcover.pdf. Accessed March 28, 2012. [Google Scholar]
- 3. Central department of statistics and information. Key indicators. Available at: http://www.cdsi.gov.sa/english/. Accessed March 28, 2012.
- 4. Ministry of Health. Cancer incidence and survival report, Saudi Arabia. Riyadh: Ministry of Health, National Cancer Registry; 2007. Available at: www.scr.org.sa/reports/SCR2007.pdf. Accessed March 28, 2012.
- 5.Al-Zahrani A, Baomer A, Al-Hamdan N, Mohamed G. Completeness and validity of cancer registration in a major public referral hospital in Saudi Arabia. Ann Saudi Med. 2003;23(1-2):6–9. doi: 10.5144/0256-4947.2003.6. [DOI] [PubMed] [Google Scholar]
- 6.WHO. Cancer Pain Relief. 2nd ed. Geneva: WHO; 1996. [Google Scholar]
- 7.Anderson F, Downing GM, Hill J, Casorso L, Lerch N. Palliative performance scale (PPS): a new tool. J Palliat Care. 1996;12(1):5–11. [PubMed] [Google Scholar]
- 8.Palos GR, Mendoza TR, Mobley GM, Cantor SB, Cleeland CS. Asking the community about cutpoints used to describe mild, moderate and severe pain. J Pain. 2006;7(1):49–56. doi: 10.1016/j.jpain.2005.07.012. [DOI] [PubMed] [Google Scholar]
- 9.Al-Shahri MZ, Sroor MY, Alsirafy SA. The impact of implementing referral criteria on the pattern of referrals and admissions to a palliative care program in Saudi Arabia. J Support Oncol. 2010;8(2):78–81. [PubMed] [Google Scholar]
- 10.Astradsson E, Granath L, Heedman PA, Starkhammar H. Cancer patients hospitalized for palliative reasons: symptoms and needs presented at a university hospital. Support Care Cancer. 2001;9:97–102. doi: 10.1007/s005200000209. [DOI] [PubMed] [Google Scholar]
- 11.Kuuppelomäki M, Lauri S. Cancer patients' reported experiences of suffering. Cancer Nurs. 1998;21(5):364–369. doi: 10.1097/00002820-199810000-00008. [DOI] [PubMed] [Google Scholar]
- 12. Population and Housing Characteristics in the Kingdom of Saudi Arabia. Demographic Survey 1428 H. (2007). Ministry of Economy & Planning, Central Department of Statistics & Information, Kingdom of Saudi Arabia. www.cdsi.gov.sa/pdf/demograph1428.pdf. Accessed March 28, 2012.
- 13.Alsirafy SA, Sroor MY, Al-Shahri MZ. Referral timing of in-hospital cancer deaths to palliative care in a Saudi tertiary care hospital. Progr Palliat Care. 2010;18(2):58–88. [Google Scholar]
- 14.Al-Shahri MZ. Cancer Pain: progress and ongoing issues in Saudi Arabia. Pain Res Manag. 2009;14(5):359–360. [PMC free article] [PubMed] [Google Scholar]
- 15.Al-Rowaili A, Al-aqeel SA, Al-Naim LS, Al-Diab AI. Appropriateness of cancer pain management in Saudi teaching hospital. Gulf J Oncolog. 2009;(5):37–43. [PubMed] [Google Scholar]
- 16.Ghosn M, Boutros C, Geara S, Kattan J, Nasr F, Chahine G. Experience with palliative care in patients with advanced cancer at a tertiary care hospital in a developing country. Support Care Cancer. 2011;19(4):573–575. doi: 10.1007/s00520-010-1056-x. [DOI] [PubMed] [Google Scholar]
- 17.van den Beuken-van Everdingen MH, de Rijke JM, Kessels AG, Schouten HC, van Kleef M, Patijn J. Prevalence of pain in patients with cancer: a systematic review of the past 40 years. Ann Oncol. 2007;18(9):1437–1449. doi: 10.1093/annonc/mdm056. [DOI] [PubMed] [Google Scholar]
- 18.Wilson KG, Chochinov HM, Allard P et al. Prevalence and correlates of pain in the Canadian National Palliative Care Survey. Pain Res Manag. 2009;14(5):365–370. doi: 10.1155/2009/251239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cleeland CS, Gonin R, Hatfield AK, Edmonson JH, Blum RH. Pain and its treatment in outpatients with metastatic cancer. N Engl J Med. 1994;330:592–596. doi: 10.1056/NEJM199403033300902. [DOI] [PubMed] [Google Scholar]
- 20.Bonica JJ. Management of Cancer pain. Recent Results Cancer Res. 1984;89:13. doi: 10.1007/978-3-642-82028-1_2. [DOI] [PubMed] [Google Scholar]
- 21.Daut RL, Cleeland CS. The prevalence and severity of pain in cancer. Cancer. 1982;50:1913–1918. doi: 10.1002/1097-0142(19821101)50:9<1913::aid-cncr2820500944>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- 22.Mumford JW, Mumford SP. The care of cancer patients in a rural South Indian hospital. Pall Med. 1988;2:157. [Google Scholar]
- 23.Portenoy RK. Cancer pain: epidemiology and syndromes. Cancer. 1989;63(11 Suppl):2298–2307. doi: 10.1002/1097-0142(19890601)63:11<2298::aid-cncr2820631140>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 24.Al-Shahri MZ. Historical perspectives on end-of-life care in global context Middle East and North Africa. In: Lazenby M, McCorkle R, Sulmasy D, editors. Safe passage: a global spiritual sourcebook for care at the end of life. New York: Oxford University Press; 2014. pp. 71–79. [Google Scholar]
- 25.Al-Shahri MZ, Al-Khenaizan A. Palliative care for Muslim patients. J Support Oncol. 2005;3(6):432–436. [PubMed] [Google Scholar]
- 26.Al-Shahri MZ, Brown SM, Bruera ED. Palliative care: proposal for a national program in Saudi Arabia. Saudi Med J. 2004;25(12):1791–1795. [PubMed] [Google Scholar]
- 27.Kirkova J, Rybicki L, Walsh D, Aktas A. Symptom prevalence in advanced cancer: age, gender, and performance status interactions. Am J Hosp Palliat Care. 2012;29(2):139–145. doi: 10.1177/1049909111410965. [DOI] [PubMed] [Google Scholar]


