Abstract
The outcome differences between Chinese male and female patients within one-year follow-up after percutaneous coronary intervention (PCI) with stent remain unclear. The present study was aimed to compare clinical outcomes in such two populations. From May 1999 to December 2009, 4,334 patients with acute myocardial infarction (MI), unstable angina, stable angina, or silent ischemia, who underwent PCI, were registered at our centers. Among these, 3,089 were men and 1,245 were women. We compared these groups with respect to the primary outcomes of MI and secondary outcomes including a composite of major adverse cardiac events (MACE) including cardiac death, MI, target lesion revascularization, target vessel revascularization (TVR), stent thrombosis (ST), definite ST and probable ST at one-year follow-up. Chinese male patients had a higher MACE rate (13% vs. 10.7%, P = 0.039), mainly led by TVR (9.09% vs. 6.98%, P = 0.024) at one year, which was significantly different than female patients. Chinese male and female patients showed a significant difference on MACEs. However, there was no significant difference with respect to MI between these groups.
Keywords: interventional cardiology, ischemic heart disease, drug-eluting stent, major adverse cardiac event, coronary stenting, gender difference
INTRODUCTION
Percutaneous coronary intervention (PCI), first introduced as percutaneous transluminal coronary angioplasty (PTCA) by Andreas Gruntzig in 1997, is a catheter-based therapy alternative to open heart surgery. After several decades of explosive development in this field, PCI has become the most effective approach to rescue patients with coronary heart disease, leading to successful and safe advances of heart disease treatment. However, PCI still needs to be perfected and numerous issues remain to be resolved[1]. PCI has developed from PTCA to bare-metal stents (BMS) and drug-eluting stents (DES). With the use of DES, the use of PCI dominates over coronary bypass operations and results in reduced rates of restenosis and mortality[2],[3]. In the quest for perfection, there have been many studies on gender outcome differences after PCI procedure. Many studies have suggested that female patients are more likely to have postoperative complications than male patients[3],[4]. However, large scale data are lacking for analyzing and understanding the relationship between genders and outcome differences after the implantation of stents in Chinese patients. Therefore, this study attempts to compare differences in one-year outcomes between genders after PCI by using a large cohort of patients.
PATIENTS AND METHODS
We included symptomatic patients older than 18 years, from May 1999 to December 2009. A total of 4,334 patients with acute myocardial infarction (AMI), unstable angina, stable angina, or silent ischemia who had PCI in our centers were registered. Among these, 3,089 patients were men and 1,245 patients were women.
PCI procedures
All PCI procedures and peri-procedure medications followed the American Heart Association/American College of Cardiology (AHA/ACC) guidelines. Coronary angiography and PCI with stent implantation were performed through a transfemoral or transradial approach. The use of intravascular ultrasound and the selection of stents were totally dependent on an experienced operating physician. All patients were pretreated with 300 mg clopidogrel and 100 mg aspirin. Life-long aspirin therapy was recommended to all patients. Clopidrogrel was prescribed for at least 9–12 months according to clinical guidelines. Angiographic success was defined as a residual stenosis ≤ 30% by visual estimation in the presence of thrombolysis in myocardial infarction (TIMI) flow grade of 3. Procedural success was defined as the achievement of angiographic success in the absence of in-hospital events. The primary endpoint was myocardial infarction (MI) at one-year follow-up. Secondary endpoints included composite major adverse cardiac events (MACE), such as cardiac deaths, MI, target lesion revascularization (TLR), target vessel revascularization (TVR), stent thrombosis (ST), definite ST and probable ST at one-year follow-up. Cardiac death was diagnosed for any unexplained death unless a non-cardiac cause was identified. The diagnosis of MI was based on the ACC/AHA guideline[5],[6]. TLR was defined as a repeat intervention of the stented segment, including the 5-mm segments proximal or distal to the stent. TVR was defined as a repeat revascularization of the same vessel that was treated in the index procedure. ST was defined according to ARC definition[7]. Definite ST was diagnosed by angiographic or pathologic confirmation of partial or total thrombotic occlusion within the peri-stent region and at least one of the additional criteria, including acute ischemia symptoms, ischemic ECG changes and elevated cardiac enzymes. Probable ST was defined as any unexplained death within 30 days of stent implantation and any MI related to documented acute ischemia in the territory of the implanted stent without angiographic confirmation of ST and any other obvious causes.
Follow-up
All patients were followed-up at one month and 12 months after discharge. Follow-up was done on an outpatient clinic basis either through telephone contact or through patients' relatives. If patients had visited other medical centers, the records from those centers were also recorded. All clinical and imaging data were recorded in our database. Patients were advised to repeat angiography once within a year of the procedure but angiography was not done routinely for every patient. Earlier angiographic surveillance was performed if clinically indicated. Clinically driven TLR or TVR was performed if there was at least > 50% in-stent restenosis coupled with the presence of typical angina or a new onset of exertional dyspnea.
Statistical analysis
Continuous variables were expressed as mean ± standard deviation (SD) and were compared with the use of two-tailed Student's t test. Categorical variables were expressed as percentages and compared using chi-square test or Fisher's exact test. All statistical analyses were two-tailed, and a P value < 0.05 was considered statistically significant. MACE-free survival was calculated using the Kaplan-Meier curve and compared by log-rank test. Binary regression was conducted by applying variables including age, gender, hypertension, diabetes, heart failure, stable angina, unstable angina, non-ST segment elevation myocardial infarction (NSTEMI), ST segment elevation myocardial infarction (STEMI), hyperlipidemia, left ventricle ejection fraction (LVEF), creatinine, renal function, diseased vessel numbers, stent number, stent length, transradial approach, chronic total occlusion (CTO) lesions, LMcto, LADcto, RCActo, left circumflex artery (LCXcto), post PCI TIMI flow, presence of bifurcation, presence of thrombus and complete revascularization. Statistical analysis was performed using SPSS version 16.0 for Windows.
RESULTS
Baseline characteristics
Of the 4,334 patients, 3,089 were men and 1,245 were women (71.2% vs. 28.7%). Baseline characteristics of both patient groups are shown in Table 1. Women were older than men but were shorter in height, lower in body weight, and had increased blood pressure, blood glucose level and increased serum cholesterol levels (P< 0.05) for all the values. Male patients were found to have a greater incidence of STEMI (P < 0.05) and NSTEMI, whereas stable angina and unstable angina incidence was found to be greater in female patients (P < 0.05). Other characteristics like LVEF, renal function and the use of medicine were not significantly different between the two groups.
Table 1. Baseline demographic and clinical characteristics.
| Baseline levels | Men (n = 3,089) | Women (n = 1,245) | P value |
| Age (year) | 63.93±10.75 | 66.41±9.29 | 0.000 |
| Height (cm) | 167.55±5.97 | 159.67±3.69 | 0.000 |
| Weight (kg) | 67.93±10.80 | 60.80±9.01 | 0.000 |
| Hypertension, n (%) | 2108(68.2) | 931(74.8) | 0.000 |
| Systolic blood pressure | 134.11±20.72 | 136.90±20.71 | 0.291 |
| Diastolic blood pressure | 81.14±12.71 | 80.12±11.38 | 0.000 |
| Diabetes mellitus, n (%) | 612(19.8) | 316(25.38) | 0.000 |
| Insulin | 112(3.6) | 62(4.9) | 0.400 |
| Oral medication | 420(13.59) | 225(18.0) | 0.000 |
| Hyperlipidemia, n (%) | 543(17.57) | 305(24.49) | 0.000 |
| CHF, n (%) | 429(13.88) | 117(14.21) | 0.778 |
| Presentation, n (%) | |||
| Stable angina | 475(15.37) | 266(21.36) | 0.000 |
| Unstable angina | 1,652(53.4) | 759(60.96) | 0.000 |
| STEMI | 735(23.79) | 154(12.36) | 0.000 |
| NSTEMI | 230(7.4) | 63(5.06) | 0.150 |
| LVEF (%) | 56.53±11.94 | 61.36±32.26 | 0.342 |
| Creatinine | 98.59±49.73 | 79.93±40.94 | 0.537 |
| Renal dysfunction, n (%) | 48(4.8) | 11(2.7) | 0.700 |
| Medication, n (%) | |||
| Statin | 311(10.06) | 120(9.6) | 0.669 |
| Beta-blocker | 374(12.10) | 171(13.73) | 0.144 |
| Diuretics | 122(3.94) | 56(4.49) | 0.410 |
| CCB | 620(20.0) | 282(22.65) | 0.138 |
| ACEI | 357(11.55) | 131(10.5) | 0.281 |
| ARB | 167(5.40) | 78(6.26) | 0.268 |
CHF: congestive heart failure, STEMI: ST-elevation myocardial infraction, NSTEMI: non-ST-elevation myocardial infraction, LVEF: left ventricular ejection fraction, ACEI: angiotensin converting enzyme inhibitor, ARB: angiotensin receptor blocker, CCB: calcium channel blocker.
Angiographic and procedural features
A higher prevalence of diseased vessel was seen in male patients than in female patients (P<0.000). A higher incidence of CTO of LCXcto (P = 0.007) with an increased stent length (P = 0.000), stent number (P = 0.000) and thrombus (P = 0.000) was seen in male patients whereas complete revascularization was higher in female patients (P = 0.013). PCI was performed through the trans-radial approach in 1,501 male patients and 585 female patients without a difference in the rate between male and female patients (48.5% vs. 47.0%, P = 0.339). The two groups did not differ with respect to infarct-related artery, bifurcation lesion or TIMI flow (Table 2).
Table 2. Angiographic and procedural features.
| Angiographic and PCI | Men (n = 3,089) | Women (n = 1,245) | P value |
| No. of diseased vessel (n) | 1.35±0.59 | 1.30±0.56 | 0.000 |
| 1-vessel disease no, n (%) | 2,191(70.9) | 923(74.13) | |
| 2-vessel disease no, n (%) | 712(23.04) | 256(20.56) | |
| 3-vessel disease no, n (%) | 181(5.85) | 65(5.22) | |
| Infarct related artery, n (%) | |||
| LAD | 2,062(66.75) | 854(68.5) | 0.419 |
| LCX | 860(27.84) | 339(27.22) | 0.684 |
| RCA | 919(29.75) | 326(26.18) | 0.190 |
| LM | 343(11.1) | 117(9.4) | 0.099 |
| Chronic total obstruction (cto), n (%) | 247(8.10) | 76(6.10) | 0.320 |
| LAD cto | 99(3.2) | 33(3.0) | 0.337 |
| LCX cto | 78(2.52) | 15(1.20) | 0.007 |
| RCA cto | 107(3.50) | 35(3.00) | 0.275 |
| LM cto | 1 | - | 0.525 |
| TIMI flow after PCI, n (%) | 0.469 | ||
| 0 | 26(0.84) | 5(0.40) | |
| 1 | 5(0.16) | 2(0.16) | |
| 2 | 28(0.90) | 10(0.80) | |
| 3 | 3,030(98.0) | 1,228(99.0) | |
| Bifurcation lesion, n (%) | 963(31.1) | 340(27.30) | 0.120 |
| Thrombus, n (%) | 267(8.64) | 63(5.06) | 0.000 |
| Complete-revascularization, n (%) | 2,184(71.0) | 927(74.4) | 0.0130 |
| Stent number | 2.26±1.51 | 2.01±1.39 | 0.000 |
| Stent diameter | 3.02±0.73 | 3.00±0.695 | 0.650 |
| Stent length | 55.03±4.20 | 47.78±36.81 | 0.000 |
| Transradial approach, n (%) | 1,501(48.5) | 585(47.0) | 0.339 |
PCI: percutaneous coronary intervention, LAD: left anterior descending artery, LCX: left circumflex artery, RCA: right coronary artery, LM: left main artery.
One-year follow-up
Approximately 63.1% of all patients received repeat angiography. There was a significant difference in the rate of repeat angiography between male and female patients (65.1% vs. 61.1%, P = 0.012) (Table 3). Although there was no statistical significance in MI between the two groups during in-hospital follow-up (0.64% in men vs. 0.24% in women, P = 0.096), the rate of MI at one-month follow-up was significantly higher in male patients than female patients (0.87% in men vs. 0.24% in women, P = 0.023) and was seen still increasing at one-year follow-up, but was not significantly different between the two groups (1.23% in men vs. 0.72% in women, P = 0.145).
Table 3. Cumulative major adverse cardiac events during one-year follow-up.
| Parameters | Men (n = 3,089) | Women (n = 1,245) | P value |
| Repeat angiography, n (%) | 2,013(65.1) | 761(61.1) | 0.012 |
| In hospital, n (%) | |||
| Myocardial infarction | 20(0.64) | 3(0.24) | 0.096 |
| Cardiac death | 34(1.10) | 14(1.12) | 0.946 |
| Target lesion revascularization | 8(0.25) | - | 0.072 |
| Target vessel revascularization | 25(0.80) | 6(0.48) | 0.247 |
| Coronary artery bypass graft | 16(0.51) | 6(0.48) | 0.880 |
| Stent thrombosis | 9(0.29) | 3(0.24) | 0.775 |
| Major adverse cardiac event | 65(2.10) | 23(1.84) | 0.587 |
| One month, n (%) | |||
| Myocardial infarction | 27(0.87) | 3(0.24) | 0.023 |
| Cardiac death | 66(2.1) | 26(2.0) | 0.921 |
| Target lesion revascularization | 10(0.32) | - | 0.044 |
| Target vessel revascularization | 30(0.97) | 7(0.56) | 0.185 |
| Coronary artery bypass graft | 16(0.51) | 7(0.56) | 0.856 |
| Stent thrombosis | 14(0.45) | 3(0.24) | 0.312 |
| Definite | 10(0.32) | 1(0.08) | 0.150 |
| Probable | 4(0.12) | 2(0.16) | 0.803 |
| Major adverse cardiac event | 99(3.20) | 35(2.81) | 0.498 |
| 12 months, n (%) | |||
| Myocardial infarction | 38(1.23) | 9(0.72) | 0.145 |
| Cardiac death | 95(3.07) | 36(2.89) | 0.749 |
| Target lesion revascularization | 198(6.40) | 68(5.4) | 0.239 |
| Target vessel revascularization | 281(9.09) | 87(6.98) | 0.024 |
| Coronary artery bypass graft | 24(0.77) | 11(0.88) | 0.723 |
| Stent thrombosis | 26(0.84) | 5(0.40) | 0.120 |
| Definite | 10(0.32) | 1(0.08) | 0.150 |
| Probable | 4(0.12) | 2(0.16) | 0.803 |
| Major adverse cardiac event | 403(13.0) | 134(10.7) | 0.039 |
The rate of MACE during in-hospital follow-up was not significantly different in the two groups (2.10% in men vs. 1.84% in women, P = 0.587), with a slight increase in the one-month follow-up in the two groups (3.20% in men vs. 2.81% in women, P = 0.498). However, a significant difference was detected between the two groups in the one-year follow-up (13.0% in men vs. 10.7% in women, P = 0.039). There was a significant difference in TLR between the two groups at one-month follow-up (0.32% in men vs. 0% in women, P = 0.044) and TVR at the one-year follow-up (9.09% in men vs. 6.98% in women, P = 0.024). Definite and probable ST was comparable in the two groups. On the other hand, there was no significant difference in cardiac death, coronary artery bypass grafting (CABG) and stent thrombosis between male and female patients. However, there was a trend for an increase in MACE in one-year follow-up, with greater significant increase in male patients.
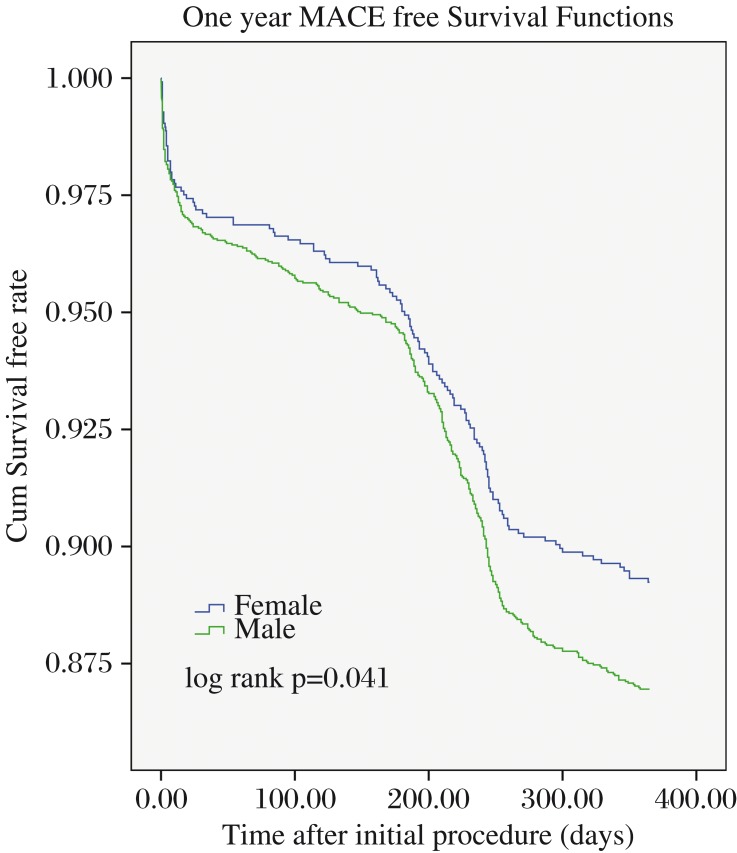
Binary regression analysis revealed that diabetes (odds ratio [OR] = 0.22, 95% confidence interval [CI] = 0.06–0.75, P = 0.01) and the presence of bifurcation (OR = 0.30, 95% CI = 0.08–1.02, P = 0.05) were significantly associated with the occurrence of MI at one-year. Conversely, LVEF (OR = 0.97, 95% CI = 0.95–0.99, P = 0.02) and LADcto (OR = 0.29, 95% CI = 0.09–0.85, P = 0.02) were significantly associated with occurrence of MACE at one-year post PCI (Fig. 2) .
Fig. 2. One-year major adverse cardiac events MACE free survival functions. Kaplan-Meier free survival curves for one-year MACE between male and female patients undergoing percutaneous coronary intervention.
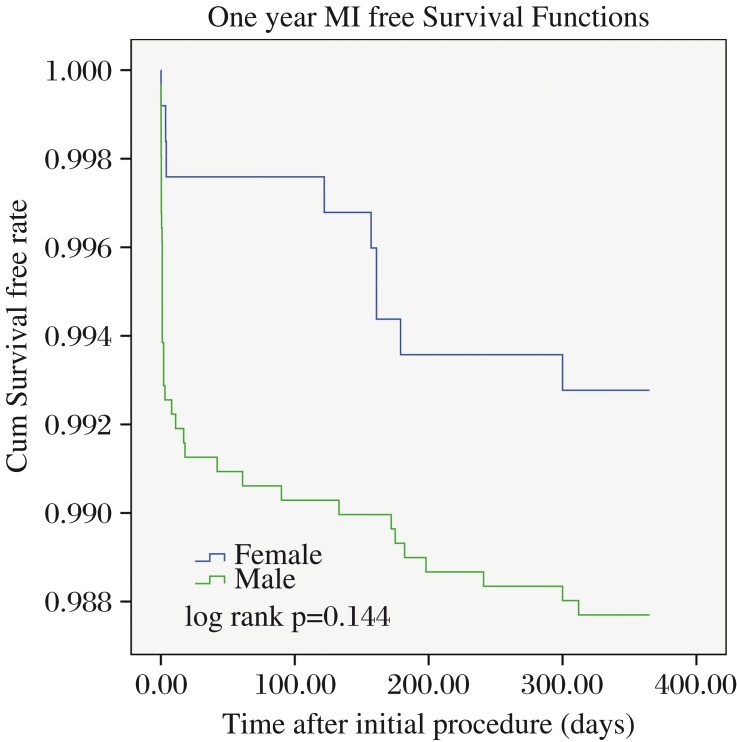
Survival
Kaplan-Meier analysis is shown in Fig. 1 for MI patients at the one-year follow-up after PCI by using Log rank test. It was determined that there was no significant difference between male and female patients (P = 0.144). However, there was a significant difference between the two groups with respect to one-year MACE during the follow-up period (P = 0.041).
Fig. 1. One-year myocardial infarction free survival functions. Kaplan-Meier free survival curves for one-year MI between male and female patients undergoing percutaneous coronary intervention.
DISCUSSION
We were able to derive several major findings from the present study. Chinese female patients were found to be older and have a lower body weight than male patients. They also had more risk factors including hypertension, diabetes and high cholesterol levels, but were found to have lower rates of thrombosis and MI than male patients. However, there was no significant difference between male and female patients during the hospital stay in the rates of MI, mortality or MACE. There was a significant difference in MI and TLR between male and female patients during one-month follow-up. A significant difference in MACE between male and female patients was found during one-year follow-up. There was a slight increase in definite ST and MI in men rather than women, and there was also a significant difference in TVR between male and female patients during one-year follow-up.
Many studies have shown a higher prevalence for female patients with these risk factors than male patients because women are older than men at the time of presentation of ACS[8],[9] and female patients have a higher incidence of postoperative MACE than male patients[10]. Some studies[11],[12],[13] showed that patients with risk factors, such as diabetes, are most likely to have negative outcomes than patients without risk factors. Mehilli et al.[14],[15] suggested that diabetes may have a greater adverse impact on female patients than male patients. The study by Ogita et al.[16] on diabetic patients post DES showed no significant difference between patients of different genders after elective PCI. In our present study, many female patients were older than male patients and had diabetes with other risk factors including hypertension and high cholesterol, but their follow-up results were totally opposite and showed that male patients had a higher incidence of MACE than female patients. In our study, Chinese male patients having a higher incidence of MACE at one-year due to their LVEF, renal function and creatinine levels were much worse in outcome than Chinese female patients, although they were not statistically significantly different. Spinler [17] reported that, from a large database of the SYNERGY trial, chronic kidney disease derived from estimated glomerular filtration rate was predictive of 30-day mortality, myocardial infarction and bleeding.
Lansky [18] reported that women have increased in-hospital mortality after both elective and primary PCI compared to men in the majority of reports, but that such differences are smaller after adjustment for women's greater age, smaller body surface area and comorbidities at the time of presentation. In our study, we did not find any difference between female and male patients during the in-hospital stay, which can be explained by the improvement in the PCI technique and in-hospital management. KAMIR[19] investigators suggested that one-month MACE was higher in female patients although there was no gender difference for invasive treatment. Welty[20] did not find any difference between genders for the procedural outcome of PCI and both genders had a similar success rate in their study. Schuhlen et al.[21] also found that female gender had no excess risk for MACE after PCI. Our study showed that there was a gender difference, but male patients were having a higher rate of MACE than female patients. MI and TLR were found to be significantly higher in male patients. This can be explained as there were a higher number of male patients who had longer and a higher number of stents. The increase in the number and length of stents contributed to an increase in TLR and in stent restenosis causing MI and an increase in MACE[22]. The other main reasons for all MACE at one-year follow-up are discontinuation of dual antiplatelet therapy by patients themselves. The study of Brener et al.[23] suggested that prolonged dual antiplatelet therapy reduces MACE after PCI. We know many male patients discontinued dual antiplatelet therapy from our data. Another study reported by Harmsze et al.[24] concluded that many patients are resistant to anti-coagulation medication. This can be the major cause of MACE after PCI and patient's reaction to stents. In our study, there are more male patients than female patients, like the study reported by Nguyen et al.[25], who suggested that there may be a gender bias for referral of patients for coronary angiography.
This study is subject to the limitations of a non-randomized study. The significant difference between genders in terms of baseline demographics and the smaller female patient population may result in bias in the interpretation of the data. Further studies of DES and BMS need to be performed to clarify difference in gender-based outcomes in Chinese patients.
Acknowledgments
We appreciate Professor Baoxiang Duan who worked as the Director of the Event Committee. We also acknowledge Ms. Ling Lin, Ms. Haimei Xu, Ms. Yinyin Zhao and Ms. Lingling Liu for contributing to data collection and remote monitoring.
References
- 1.Song ZY, Zhang ZY, Xu ZS. Brief history of percutaneous coronary intervention. Zhonghua Yi Shi Za Zhi (in Chinese) 2010;40:180–3. [PubMed] [Google Scholar]
- 2.Yeh RW, Chandra M, McCulloch CE, Go AS. Accounting for the mortality benefit of drugeluting stents in percutaneous coronary intervention: a comparison of methods in a retrospective cohort study. BMC Med. 2011;9:78. doi: 10.1186/1741-7015-9-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yang PC, Clancy CE. Gender-based differences in cardiac diseases. Biomed Res. 2011;25:81–9. doi: 10.1016/S1674-8301(11)60010-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ma J, Yang W, Singh M, Peng T, Fang N, Wei M. Meta-analysis of long-term outcomes of drug-eluting stent implantations for chronic total coronary occlusions. Heart Lung. 2011;40:32–40. doi: 10.1016/j.hrtlng.2010.07.009. [DOI] [PubMed] [Google Scholar]
- 5.Liu Y, Wang LF, Yang XF, Ge YG, Xu L, Li WM, et al. Gender differences in efficacy of primary percutaneous coronary intervention in patients with ST-elevation myocardial infarction. Chin Med J. 2008;121:2374–8. [PubMed] [Google Scholar]
- 6.Braunwald E, Antman EM, Beasley JW, Califf RM, Cheitlin MD, Hochman JS, et al. ACC/AHA 2002 guideline update for the management of patients with unstable angina and non-ST-segment elevation myocardial infraction-summary article: a report of the American College of Cardiology/American Heart Association task force on practice guidelines (Committee on the management of patients with Unstable angina). J Am Coll Cardiol. 2002;40:1366–74. doi: 10.1016/s0735-1097(02)02336-7. [DOI] [PubMed] [Google Scholar]
- 7.Antman EM, Anbe DT, Armstrong PW, Bates ER, Green LA, Hand M, et al. ACC/AHA guidelines for the management of patient with ST-elevation myocardial infarction; a report of the American College of Cardiology/American Heart Association task force on practice guidelines (Committee to Revise the 1999 Guidelines for the Management of patients with acute myocardial infraction). J Am Coll Cardiol. 2004;44:E1–E211. doi: 10.1016/j.jacc.2004.07.014. [DOI] [PubMed] [Google Scholar]
- 8.Laura M, Wen-hua H, Joseph M. M, Kalon KL, Ralph DA, Donald EC. Stent Thrombosis in Randomized Clinical Trials of Drug-Eluting Stents. N Engl J Med. 2007;356:1020–9. doi: 10.1056/NEJMoa067731. [DOI] [PubMed] [Google Scholar]
- 9.Berger JS, Elliott L, Gallup D, Roe M, Granger CB, Armstrong PW, et al. Sex differences in mortality following acute coronary syndromes. JAMA. 2009;302:874–82. doi: 10.1001/jama.2009.1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Elizabeth AJ, Mauro M, Dean ES, David S, Simon D, Adam G, et al. The association of sex with outcomes among patients undergoing primary percutaneous coronary intervention for ST elevation myocardial infarction in the contemporary era: Insights from the Blue Cross Blue Shield of Michigan Cardiovascular Consortium (BMC2). Am Heart J. 2011;161:106–12. doi: 10.1016/j.ahj.2010.09.030. [DOI] [PubMed] [Google Scholar]
- 11.Chen Z, Qian J, Ma J, Ge L, Ge J. Effect of gender on repeated coronary artery revascularization after intra-coronary stenting: a meta-analysis. Int J Cardiol. 157:381–5. doi: 10.1016/j.ijcard.2010.12.082. 2012 14. [DOI] [PubMed] [Google Scholar]
- 12.Sabaté M, Jiménez-Quevedo P, Angiolillo DJ, Gomez-Hospital JA, Alfonso F, Hernandez-Antolin R, et al. Randomized comparison of sirolimus-eluting stent versus standard stent for percutaneous coronary revascularization in diabetic patients: the diabetes and sirolimus-eluting stent (DIABETES) trial. Circulation. 2005;112:2175–83. doi: 10.1161/CIRCULATIONAHA.105.562421. [DOI] [PubMed] [Google Scholar]
- 13.Niles NW, McGrath PD, Malenka D, Quinton H, Wennberg D, Shubrooks SJ, et al. Survival of patients with diabetes and multivessel coronary artery disease after surgical or percutaneous coronary revascularization: results of a large regional prospective study. Northern New England Cardiovascular Disease Study Group. J Am Coll Cardiol. 2001;37:1008–15. doi: 10.1016/s0735-1097(00)01205-5. [DOI] [PubMed] [Google Scholar]
- 14.Lincoff AM. Important triad in cardiovascular medicine: diabetes, coronary intervention, and platelet glycoprotein IIb/IIIa receptor blockade. Circulation. 2008;107:1556–9. doi: 10.1161/01.cir.0000055653.52489.e9. [DOI] [PubMed] [Google Scholar]
- 15.Mehilli J, Kastrati A, Bollwein H, Dibra A, Schuhlen H, Dirschinger J, et al. Gender and restenosis after coronary artery stenting. Eur Heart J. 2003;24:1523–30. doi: 10.1016/s0195-668x(03)00320-8. [DOI] [PubMed] [Google Scholar]
- 16.Mehilli J, Kastrati A, Dirschinger J, Bollwein H, Neumann FJ, Schomig A. Differences in prognostic factors and outcomes between women and men undergoing coronary artery stenting. J Am Med Assoc. 2000;284:1799–805. doi: 10.1001/jama.284.14.1799. [DOI] [PubMed] [Google Scholar]
- 17.Ogita M, Miyauchi K, Dohi T, Wada H, Tuboi S, Miyazaki T, et al. Gender-based outcomes among patients with diabetes mellitus after percutaneous coronary intervention in the drug-eluting stent era. Int Heart J. 2011;52:348–52. doi: 10.1536/ihj.52.348. [DOI] [PubMed] [Google Scholar]
- 18.Spinler SA, Mahaffey KW, Gallup D, Levine GN, Ferguson JJ, Rao SV, et al. Relationship between renal function and outcomes in high-risk patients with non-ST-segment elevation acute coronary syndromes: Results from SYNERGY. Int J Cardiol. 2010;144:36–41. doi: 10.1016/j.ijcard.2009.03.119. [DOI] [PubMed] [Google Scholar]
- 19.Lansky AJ, Hochman JS, Ward PA, Mintz GS, Fabunmi R, Berger PB, et al. Percutaneous coronary intervention and adjunctive pharmacotherapy in women. A statement for Healthcare Professionals from the American Heart Association. Circulation. 2005;111:940–53. doi: 10.1161/01.CIR.0000155337.50423.C9. [DOI] [PubMed] [Google Scholar]
- 20.Lee KH, Jeong MH, Ahn YK, Kim JH, Chae SC, Kim YJ, et al. Gender differences of success rate of percutaneous coronary intervention and short term cardiac events in Korea Acute Myocardial Infarction Registry. Int J Cardiol. 2008;130:227–34. doi: 10.1016/j.ijcard.2007.08.044. [DOI] [PubMed] [Google Scholar]
- 21.Welty FK, Mittleman MA, Healy RW, Muller JE, Shubrooks SJ. Similar results of percutaneous transluminal coronary angioplasty for women and men with post myocardial infarction ischemia. J Am Coll Cardiol. 1994;23:35–9. doi: 10.1016/0735-1097(94)90499-5. [DOI] [PubMed] [Google Scholar]
- 22.Schuhlen H, Kastrati A, Dirschinger J, Hausleiter J, Elezi S, Wehinger A, et al. Intracoronary stenting and risk for major adverse cardiac events during the first month. Circulation. 1998;98:104–11. doi: 10.1161/01.cir.98.2.104. [DOI] [PubMed] [Google Scholar]
- 23.Zhang QY, Li Y, Guan SY, Wang XZ, Jing QM, Ma YY, et al. Incidence and predictors of definite stent thrombosis after coronary stent implantation. Chin Med J (Engl) 2012;125:1547–51. [PubMed] [Google Scholar]
- 24.Brener SJ, Steinhubl SR, Berger PB, Brennan DM, Topol EJ CREDO Investigators. Prolonged dual antiplatelet therapy after percutaneous coronary intervention reduces ischemic events without affecting the need for repeat revascularization: insights from the CREDO trial. J Invasive Cardiol. 2007;19:287–90. [PubMed] [Google Scholar]
- 25.Harmsze AM, van Werkum JW, Ten Berg JM, Zwart B, Bouman HJ, Breet NJ, et al. CYP2C19*2 and CYP2C9*3 alleles are associated with stent thrombosis: a case-control study. Eur Heart J. 2010;31:3046–53. doi: 10.1093/eurheartj/ehq321. [DOI] [PubMed] [Google Scholar]
- 26.Nguyen JT, Berger AK, Duval S, Luepker RV. Gender disparity in cardiac procedures and medication use for acute myocardial infarction. Am Heart J. 2008;155:862–68. doi: 10.1016/j.ahj.2007.11.036. [DOI] [PMC free article] [PubMed] [Google Scholar]