Abstract
Currently, no reported studies have evaluated intraoperative handover among anesthesia providers. Studies on anesthetic handover in the US recovery room setting observed that handover processes are insufficient and, in many instances, significant intraoperative events are disregarded. An online survey tool was sent to anesthesia providers at US anesthesia residency programs nationwide (120 out of the 132 US programs encompassing around 4500 residents and their academic MDAs) and a smaller survey selection of CRNAs (10 institutions about 300 CRNAs in the metropolitan area of Detroit, MI, USA) to collect information on handover practices. The response rate to this survey (n = 216) was comprised of approximately 5% (n = 71) of the resident population in US anesthesia programs, 5% (n = 87) of MDAs , and 20% (n = 58) of the CRNAs. Out of all respondents (n = 212), 49.1 % had no hand-over protocol at their institution and 88% of respondents who did have institutional handover protocols believed them insufficient for effective patient handover. In addiiton, 84.8% of all responders reported situations where there was insufficient information received during a patient handover. Only 7% of the respondents reported never experiencing complications or mismanagement due to poor or incomplete hand-overs. In contrast, 60% reported rarely having complications, 31% reported sometimes having complications, and 3% reported frequent complications. In conclusion, handover transition of patient care is a vulnerable and potentially life-threatening event in the operating room. Our preliminary study suggests that current intraoperatvive handover practices among anesthesia providers are suboptimal and that national patient handover guidelines are required to improve patient safety.
Keywords: patient handover, anesthesiology, postoperative care, patient safety, health care surveys
INTRODUCTION
Healthcare and anesthesiology practices have undergone marked changes over recent years. Patient acuity has been increasing, patient turnover is higher, and patients are frequently of advanced age with several comorbid disorders. Limited resources and the pressure for higher efficiency can result in the suboptimal delivery of healthcare. During treatment within the healthcare system, a significant percentage of patients (3–16%) suffer from adverse events through system errors[1]-[3] with 15–65% of adverse patient events being attributed to communication failure[4].
Patient care can involve several health care providers with several transfers between providers. In this transition, poor or incomplete relay of patient data may result in errors, near misses and adverse events. Standardized and thorough communication of critical information is an essential component of patient safety[5],[6]. National handover policies exist in Europe[7], the UK[8] and Australia[9]. Although individual US based handover guidelines[10],[11] and handover tools [12] have been developed, these practices are not widespread. A previous survey study observed that 31% of MDs experienced daily clinical problems which they believed avoidable if provided with adequate hand-over processes[13]. Widespread US practice of verbal hand-over has been observed to be highly inefficient[14].
Need for improvement in the patient handover process has clearly become a worldwide issue. The World Health Organization listed “Communication during Patient Care Handovers” as one of its High 5 patient safety initiatives[15]. The Joint Commission International listed their 2nd national patient safety goal as to “Improve the effectiveness of communication among caregivers”[16]. There is a lack of studies on how anaesthesiologists hand over their patients, which is surprising given that anesthesiology is a specialty that has always aimed at placing patient safety as its top priority[17].
The standards of postoperative care issued by the American Society of Anesthesiology does not state how handover should be performed nor what information it should include, leaving the handover process decision up to the individual clinician[18]. Studies analyzing anesthetic team handover in the recovery room observed that the majority of handovers were remarkably brief and insufficient[19]-[21]. In these studies, critical details such as the preoperative state of the patient, type of operation performed, amount and kinds of analgesics given and problems encountered during the case were either barely mentioned or underplayed. In some instances significant intraoperative events were completely disregarded. Additionally, there were frequent distractions present at the time of the hand-over. There are no reported studies on handover practices performed by anesthesia providers when transition of care occurs intraoperatively.
This preliminary pilot study was a qualitative rather than quantitative survey to highlight the scope of the current US intraoperative handover of patient information.
SUBJECTS AND METHODS
This study had institutional approval (Wayne State University IRB). Due to the anonymity of the suvey content, the requirement for written informed consent was waived by the IRB. This study used an online questionnaire format with 8 survey questions created using a computerized online survey program (Survey Monkey , Palo Alto, CA, USA,). An e-mail with a link to the questionnaire was sent to anesthesia providers at all anesthesia residency programs nationwide (120 out the 132 US programs encompassing around 4500 residents and their attending academic MDAs) and a smaller survey selection of CRNAs (10 institutions about 300 CRNAs in the metropolitan area of Detroit, MI). All questionnaires were anonymous and were only sent to US anesthesia providers working in an academic hospital setting with an associated residency program in anesthesiology. The only demographics of surveyed anesthesia health care providers obtained were for medical training level (Certified Registered Nurse Anesthetist -CRNA, Medical Doctor of Anesthesiology Resident MDAR, or Medical Doctor of Anesthesiology MDA). All responses were gathered during a 2 month survey period.
RESULTS
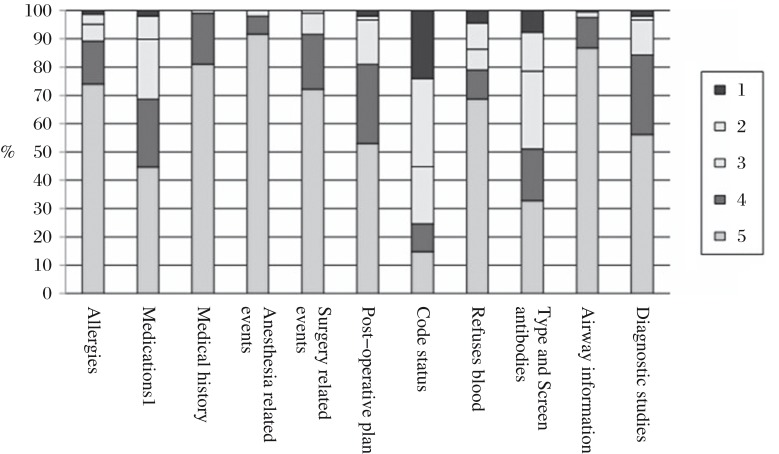
From all questionnaires received (n = 216), 87 (40.3%) of respondents were MDAs, 71 (32.9%) were MDAR, and 58 were CRNAs (26.9%; Table 1). The response rate to this survey was low with a response from approximately 5% of the resident population in US anesthesia programs and approximately 20% of the CRNAs surveyed in the metropolitan Detroit area. Of all respondents, 108 (49.1 %) stated that they did not have a handover protocol at the institution where they practiced (Table 1). Of the respondents who did have an institutional handover policy, 11.2% stated that that protocol included the necessary elements for effective handover. Furrthermmore, 85.7% respondents reported not having a departmental standardized handover form (Table 2). Of all responders, 84.8% (173/204) had an experience where they had not received sufficient information during a patient handover. Only 7.4% (15/203) of respondents had never experienced complications or mismanagement due to poor or incomplete handover. In comparison, 59.6% (121/203) reported rarely having complications, 30.5% (62/203) reported sometimes having complications and 2.5% (5/203) reported frequently having complications (Table 3). Based on the informal prelimanary survey, the specific handover information has been developed. Respondents were asked to respond on the frequency in which they addressed the specific handover information such as allergies and medications, past medical history, intraoperative events (anesthesia related and surgery related), postoperative plans (extubation/ICU, etc.), special concerns (code status, Jehovah's witness, type and screen antibodies, airway information (ie. h/o difficult intubation) and significant diagnostic studies (e.g Blood lab, EKG, Chest X-ray, Stress tests, Pulmonary Function Tests, etc.). For this specific handover information, the majority of providers frequently or always relayed information regarding patient allergies (89.2%), past medical history (99%), anesthesia related intraoperative events (99%), surgery related intraoperative events (91.7%), airway information (97.5%) and significant diagnostic studies (84.2%; Fig. 1). However, information about medications (31.4%), postoperative plan (19.1%), code status (75.4%), information about refusal of blood (21.1%) and type and screen antibodies (49%) were either sometimes, rarely or never included during handover. From the specific list of patient handover information factors, 80.5% (165/204) of responders stated that these factors would be sufficient for an effective, complete handover.
Table 1. Survey responses from question 8 of the intraoperative handover questionnaire.
| Survey question | MDAR | CRNA | MDA |
| Which group of anesthesia providers do you belong to? | 40.3% | 32.9% | 26.9% |
MDAR-Medical Doctor of Anesthesiology Resident, CRNA- Certified Registered Nurse Anesthetist, MDA-Medical Doctor of Anesthesiology.
Table 2. Survey responses from questions 1, 2, 3 and 6 of the intraoperative handover questionnaire.
| Survey question | Yes | No |
| Does your Department have a hand over protocol? | 50.9% | 49.1% |
| Does this Departmental handover policy define the necessary elements that you believe should be included during hand overs? | 11.2% | 88.2% |
| Do you use a standardized hand over form when taking over a case from another provider? | 14.3% | 85.7% |
| Have you ever felt that you have not received enough patient hand over information when taking over a case? | 15.2% | 84.8% |
Table 3. Survey responses from question 7 of the intraoperative handover questionnaire.
| Survey question | Never | Rarely | Sometimes | Frequently |
| How often have you experienced complications or mismanagement due to poor or incomplete hand-overs? | 7.4% | 59.6% | 30.5% | 2.5% |
Fig. 1. Survey question 4.
On a scale from 1–5, how frequently do you cover the following patient information during the hand-over? Key - (1 = Never, 2 = Rarely, 3 = Sometimes, 4 = Frequently, 5 = Always. Patient information factors expressed as a % proportion of total survey response.
Table 4. Additional patient information that survey respondants suggested for an effective handover; responses from survey question 5 (n = 39 responses/216 total survey responses).
| Suggested additional patient information | Responses/total responses |
| Anesthesiologist covering room | 3/39 |
| Baseline vital signs | 2/39 |
| Previous anesthesia related complications (i.e. PONV, MH, etc.) | 2/39 |
| Important family and psycho-social elements | 12/39 |
| IV access / lines | 15/39 |
| Total IV fluids | 11/39 |
| Antibiotics re-dosing time | 3/39 |
| Patient positioning | 2/39 |
| Anticipated time until end of surgery | 4/39 |
| Post-op pain management / concerns | 6/39 |
PONV: post-operative nauseaand vommitting; MH: malignant hyperthermia; IV: intravenous.
DISCUSSION
This pilot study was a qualitative rather than quantitative survey to highlight the scope of the current problem of US intraoperative handover of patient information. Poor transition of patient care from the operating room has a high potential for adverse patient outcomes. Our study indicates that the current intraoperatvive handover processes among anesthesia providers do not have standard uniform practices, and there may be a high proportion of insufficient patient handover practices. These findings are surprising given that the anesthesiology specialty places patient safety as one of its top objectives[17] and that all survey respondents practiced in an academic institution. Major limitations of this study were the low response rate of 216 respondents and that due to annonymous nature of this survey the number of individual academic institutitions could not be determined. Additionally, there is the possibility that there was a bias towards an increased proportion of responses from anesthesia providers who had prior poor handover experiences and were unsatisified with current practice. Regardless of these potential limitations, there are no current US standard handover practices. The lack of standardized handover process has resulted in substandard patient care in US healthcare setting[13],[14]. Standardized and rigorous implementation of handover practices improves quality of healthcare[6],[11].
In conclusion, we hope that our study will stimulate a discussion of US handover practices in the anesthesia field. Increased awareness in handover practices will hopefully encourage action in improving potential patient safety issues. We believe that patient handover practices should be discussed and an optimal response would be the formation of an expert consortium with the aim to develop and implement standardized protocols.
References
- 1.Wilson RM, Runciman WB, Gibberd RW, Harrison BT, Newby L, Hamilton JD. The Quality in Australian Health Care Study. Med J Aust. 1995;163:458–71. doi: 10.5694/j.1326-5377.1995.tb124691.x. [DOI] [PubMed] [Google Scholar]
- 2.Vincent C, Neale G, Woloshynowych M. Adverse events in British hospitals: a preliminary retrospective record review. BMJ. 2001;322:517–9. doi: 10.1136/bmj.322.7285.517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kohn LT, Corrigan JM, Donaldson MS. To Err Is Human: Building a Safer Health System. Washington, DC: The National Academies Press; p. 2000. [PubMed] [Google Scholar]
- 4.Gawande AA, Zinner MJ, Studdert DM, Brennan TA. Analysis of errors reported by surgeons at three teaching hospitals. Surgery. 2003;133:614–21. doi: 10.1067/msy.2003.169. [DOI] [PubMed] [Google Scholar]
- 5.Kalkman CJ. Handover in the perioperative care process. Curr Opin Anesthesiol. 2010;23:749–53. doi: 10.1097/ACO.0b013e3283405ac8. [DOI] [PubMed] [Google Scholar]
- 6.Catchpole KR, de Leval MR, McEwan A, Pigott N, Elliott MJ, Mcquillan A, et al. Patient handover from surgery to intensive care: using Formula 1 pit-stop and aviation models to improve safety and quality. Paediatr Anaesth. 2007;17:470–8. doi: 10.1111/j.1460-9592.2006.02239.x. [DOI] [PubMed] [Google Scholar]
- 7.Philibert I, Barach P.The European HANDOVER Project: a multi-nation program to improve transitions at the primary care–inpatient interface BMJ Qual Saf 2012(Suppl 1), i1–6.doi: 10.1136/bmjqs-2012-001598. [DOI] [PubMed] [Google Scholar]
- 8.BMA, Junior Doctors Committee, National Patient Safety Agency, NHS Modernisation Agency. Safe handover: safe patients. Guidance on clinical handover for clinicians and managers. London: British Medical Association; 2005. [Google Scholar]
- 9.Safe Handover: Safe Patients. Guidance on clinical handover for clinicians and managers (2006). Australia Medical Association. Url: http://ama.com.au/system/files/node/4064/Clinical_Handover.pdf. [Google Scholar]
- 10.Wohlauer MV, Arora VM, Horwitz LI, Bass EJ, Mahar SE, Philibert I. Handoff Education and Assessment for Residents (HEAR) Computer Supported Cooperative Workgroup The patient handoff: a comprehensive curricular blueprint for resident education to improve continuity of care. Acad Med. 2012;87:411–8. doi: 10.1097/ACM.0b013e318248e766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Arriaga AF, Elbardissi AW, Regenbogen SE, Greenberg CC, Berry WR, Lipsitz S, et al. A policy-based intervention for the reduction of communication breakdowns in inpatient surgical care: results from a Harvard surgical safety collaborative. Ann Surg. 2011;253:849–54. doi: 10.1097/SLA.0b013e3181f4dfc8. [DOI] [PubMed] [Google Scholar]
- 12.Petrovic MA, Martinez EA, Aboumatar H. Implementing a perioperative handoff tool to improve postprocedural patient transfers. Jt Comm J Qual Patient Saf. 2012;38:135–42. doi: 10.1016/s1553-7250(12)38018-5. [DOI] [PubMed] [Google Scholar]
- 13.Borowitz SM, Waggoner-Fountain LA, Bass EJ, Sledd RM. Adequacy of information transferred at resident sign-out (in-hospital handover of care): a prospective survey. Qual Saf Health Care. 2008;17:6–10. doi: 10.1136/qshc.2006.019273. [DOI] [PubMed] [Google Scholar]
- 14.Bhabra G, Mackeith S, Monteiro P, Pothier DD. An experimental comparison of handover methods. Ann R Coll Surg Engl. 2007;89:298–300. doi: 10.1308/003588407X168352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.World Health Organization. Communication during Patient Care Hand-Overs. Patient Safety Solutions May 2007;Volume 1,Solution 3. [Google Scholar]
- 16.The Joint Commission releases Improving America's Hospitals: The Joint Commission's Annual Report on Quality and Safety, 2008. Jt Comm Perspect. 2009:99–103. [PubMed] [Google Scholar]
- 17.Gaba DM. Anaesthesiology as a model for patient safety in health care. BMJ. 2000;320:785–8. doi: 10.1136/bmj.320.7237.785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.American Society of Anesthesiologists. Standards for Postanesthesia Care. Available at: http://www.asahq.org/ForMembers/~/media/For%20Members/documents/Standards%20Guidelines%20Stmts/Postanesthesia%20Care%20Standards%20For.ashx. [Google Scholar]
- 19.Smith AF, Pope C, Goodwin D, Mort M. Interprofessional handover and patient safety in anaesthesia: observational study of handovers in the recovery room. Br J Anaesth. 2008;101:332–7. doi: 10.1093/bja/aen168. [DOI] [PubMed] [Google Scholar]
- 20.Smith AF, Pope C, Goodwin D, Mort M. Communication between anesthesiologists, patients and the anesthesia team: a descriptive study of induction and emergence. Can J Anaesth. 2005;52:915–20. doi: 10.1007/BF03022051. [DOI] [PubMed] [Google Scholar]
- 21.Nagpal K, Arora S, Abboudi M, Vats A, Wong HW, Manchanda C, et al. Postoperative handover: problems, pitfalls, and prevention of error. Ann Surg. 2010;252:171–6. doi: 10.1097/SLA.0b013e3181dc3656. [DOI] [PubMed] [Google Scholar]