Low back pain affects a considerable proportion of the population and can significantly decrease quality of life. Radiofrequency ablation is an emerging technique that may offer relief from pain for patients experiencing chronic low back pain. This systematic review of the procedure aimed to summarize its efficacy in the treatment of pain in different regions of the low back.
Keywords: Chronic low back pain, Low back pain, Radiofrequency ablation, Visual analogue scale
Abstract
BACKGROUND:
Radiofrequency ablation (RFA), a procedure using heat to interrupt pain signals in spinal nerves, is an emerging treatment option for chronic low back pain. Its clinical efficacy has not yet been established.
OBJECTIVE:
To determine the efficacy of RFA for chronic low back pain associated with lumbar facet joints, sacroiliac joints, discogenic low back pain and the coccyx.
METHODS:
A systematic review was conducted. Medline, EMBASE, PubMed, SPORTDiscus, CINAHL and the Cochrane Library were searched up to August 2013. Abstracts and full-text articles were reviewed in duplicate. Included articles were sham-controlled randomized controlled trials (RCTs), assessed the efficacy of RFA, reported at least one month of follow-up and included participants who had experienced back pain for at least three months. Data were extracted in duplicate and quality was assessed using the Cochrane Risk of Bias tool. Due to heterogeneity, as well as a lack of reported mean differences and SDs, meta-analysis was not possible using these data.
RESULTS:
The present systematic review retrieved 1063 abstracts. Eleven sham-controlled RCTs were included: three studies involving discogenic back pain; six studies involving lumbar facet joint pain; and two studies involving sacroiliac joint pain. No studies were identified assessing the coccyx. The evidence supports RFA as an efficacious treatment for lumbar facet joint and sacroiliac joint pain, with five of six and both of the RCTs demonstrating statistically significant pain reductions, respectively. The evidence supporting RFA for the treatment of discogenic pain is mixed.
CONCLUSIONS:
While the majority of the studies focusing on lumbar facet joints and sacroiliac joints suggest that RFA significantly reduces pain in short-term follow-up, the evidence base for discogenic low back pain is mixed. There is no RCT evidence for RFA for the coccyx. Future studies should examine the clinical significance of the achieved pain reduction and the long-term efficacy of RFA.
Abstract
HISTORIQUE :
L’ablation par radiofréquence (ARF), une intervention faisant appel à la chaleur pour interrompre les signaux de douleur dans les nerfs rachidiens, est un traitement émergent dont l’efficacité n’est pas encore établie pour soulager les douleurs lombaires chroniques.
OBJECTIF :
Déterminer l’efficacité de l’ARF pour soulager les douleurs lombaires chroniques associées aux facettes articulaires lombaires, aux articulations sacro-iliaques, aux articulations discales et au coccyx.
MÉTHODOLOGIE :
Les chercheurs ont effectué une analyse systématique dans Medline, EMBASE, PubMed, SPORTDiscus, CINAHL et la Bibliothèque Cochrane jusqu’en août 2013. Ils ont examiné deux fois les résumés et les articles intégraux. Ils ont inclus les essais aléatoires et contrôlés (EAC) contre placebo, évalué l’efficacité de l’ARF, rendu compte d’au moins un mois de suivi et inclus les participants qui avaient souffert de douleurs lombaires pendant au moins trois mois. Ils ont extrait les données deux fois et évalué la qualité au moyen de l’outil de risque de biais de Cochrane. En raison de l’hétérogénéité et du manque de différences moyennes et d’ÉT déclarés, il n’a pas été possible d’effectuer de méta-analyse.
RÉSULTATS :
La présente analyse systématique a permis d’extraire 1 063 résumés. Onze EAC contre placebo ont été conservés : trois sur les douleurs aux articulations discales dorsales, six sur les douleurs aux facettes articulaires lombaires et deux sur les articulations sacro-iliaques. Aucune ne portait sur le coccyx. Cinq des six EAC sur les facettes articulaires lombaires et les deux EAC sur les articulations sacro-iliaques démontraient une réduction statistiquement significative de la douleur grâce à l’ARF. Les données probantes en appui à l’ARF pour traiter les douleurs discales sont mitigées.
CONCLUSIONS :
D’après la majorité des études sur les facettes articulaires lombaires et les articulations sacro-iliaques, l’ARF réduit considérablement la douleur au suivi à court terme, mais les données probantes sont mitigées à l’égard des douleurs des disques lombaires. Aucun EAC ne présente de résultats sur l’ARF appliqué au coccyx. D’autres études devraient porter sur l’importance clinique de la réduction de la douleur obtenue et sur l’efficacité à long terme de l’ARF.
More than 80% of the global population will experience low back pain at least once in their life (1). At any one time, it is prevalent in 4% to 33% of the population (2). One-half of the adult population in the United States report having experienced low back pain within the previous year, and one-quarter report experiencing low back pain in the previous three months (3). Low back pain is responsible for significant resource utilization; it has been estimated that this condition costs more than $100 billion per year in the United States, primarily due to lost productivity and wages (4).
Low back pain can originate from the lumbar facet joints, the sacroiliac joint, the intervertebral discs (discogenic low back pain) and the coccyx. While there is no standardized definition (5), chronic low back pain is typically defined as pain in the low back that persists for ≥3 months, while acute low back pain is typically defined as pain lasting for <3 months (6). Of the population with acute low back pain, approximately 2% to 34% will eventually experience chronic low back pain (7).
Conservative treatment options for chronic low back pain may include pharmaceuticals, manual therapy (eg, massage, physiotherapy, spinal manipulation), exercise therapy (eg, aerobic activity, muscle strengthening), and educational or psychological therapies (eg, cognitive behavioural therapy, support groups, educational sessions) (8,9). A systematic review of randomized controlled trials, which assessed conservative treatment options for low back pain, found strong evidence for the use of muscle relaxants, manipulation, education (‘back school’) and exercise therapy (10). If conservative treatments are unsuccessful, more invasive methods, such as steroid injections, nerve blocks, cryoablation, radiofrequency ablation (RFA) or surgery, can be attempted (11).
First used to treat low back pain by Shealy (12) in 1975, RFA is a procedure that may offer low back pain relief for patients without a known pathology (infection, tumour, fracture or osteoporosis). During the procedure, a high-frequency electrical current runs through an insulated needle. At the tip of the needle, the electric field causes molecule movement which, in turn, produces thermal energy. The heat from the tip of the RFA device is targeted to create a small lesion within a nerve, which disrupts the pain signal. Numerous randomized controlled trials (RCTs) and observational studies have been completed assessing the ability of RFA to treat low back pain.
To our knowledge, there is no current systematic review on RFA that summarizes the available evidence to determine the efficacy of RFA for all four clinical conditions associated with chronic low back pain. Therefore, the objective of the present study is to determine the efficacy of RFA for the treatment of chronic low back pain associated with the lumbar facet joints, the sacroiliac joint, discogenic low back pain and the coccyx.
METHODS
A systematic review was completed. Medline, EMBASE, PubMed, SPORTDiscus, CINAHL and the Cochrane Central Registry of Controlled Trials (CENTRAL), Cochrane Database of Systematic Reviews, and University of York Centre for Reviews and Dissemination Databases were searched from inception to August 2013. Terms aimed at capturing the target diagnosis, such as “low back pain” and “back pain” were combined using the Boolean operator “or”. These terms were then combined, using the Boolean operator “and”, with terms describing the technology, such as “radiofrequency”, “radio-frequency”, “medial branch”, “RF”, “ablation” and “denervation”. Results were limited to human studies and RCT designs. No other limitations were used. Details of the search are available from the authors on request.
All abstracts were screened in duplicate. Abstracts proceeded to full-text review if they: reported original data; were a sham-controlled RCT study design; assessed the efficacy of RFA; included adult participants with low back pain for >3 months before the intervention; and reported at least one month follow-up data using a visual analogue scale or numerical rating scale (Table 1). Abstracts were excluded if they failed to meet the criteria above or if they included animals, reported nonoriginal data or included pediatric populations. There were no restrictions on the type (cooled, pulsed or continuous), temperature or duration of RFA used. Abstracts selected for inclusion by either reviewer proceeded to full-text review. This initial abstract screen was intentionally broad to ensure that all relevant literature was captured.
Table 1.
Inclusion and exclusion criteria
| Inclusion criteria | Exclusion criteria |
|---|---|
| Pulsed or continuous radiofrequency ablation | Not radiofrequency ablation technology |
| Sham-controlled RCT | Not sham-controlled RCT design |
| Original data | Animals |
| Adult population | Nonoriginal data |
| Pain persistent for ≥3 months before intervention | Pediatric population Pain persistent for <3 months before intervention |
| ≥1 month follow-up reporting using either a visual analogue scale or a numerical rating scale | Research only available in poster or abstract form |
RCT Randomized controlled trial
Studies included after abstract review proceeded to full-text review in duplicate. Studies were included in the present review if they met all inclusion criteria and failed to meet any of the exclusion criteria presented in Table 1. Any discrepancy between reviewers during full-text review was resolved through discussion and consensus. Reference lists of included studies were hand-searched to ensure all relevant studies were captured in the literature search.
For all studies, patient selection, study inclusion and exclusion criteria, patient characteristics, procedure protocol and outcomes measured were extracted using standardized data extraction forms. Pain outcomes (mean and SD) for intervention and control groups, as measured by visual analogue or numerical rating scales, were also extracted from each study.
During data extraction, each included study was assessed for quality using the Cochrane Risk of Bias Checklist (13). Using this checklist, each included study was assessed for seven areas of bias (random assignment generation; allocation concealment; blinding of participants and personnel; blinding of outcome assessment; incomplete outcome data; selective reporting; and any additional potential sources of bias) (13). Each of these seven potential areas of bias were assigned a ‘low’, ‘high’ or ‘unclear’ risk of bias (13). Quality assessment was completed in duplicate, with discrepancies being resolved through discussion and consensus.
RESULTS
The literature search identified 1063 abstracts (Figure 1). Of these, 922 were excluded during abstract review and 141 proceeded to full-text review. During full-text review, an additional 130 studies were excluded. A total of 11 studies met the inclusion criteria when assessed during full-text review and were included in the present systematic review (14–24). Hand-searching the references of the 11 included studies did not identify any additional articles.
Figure 1).
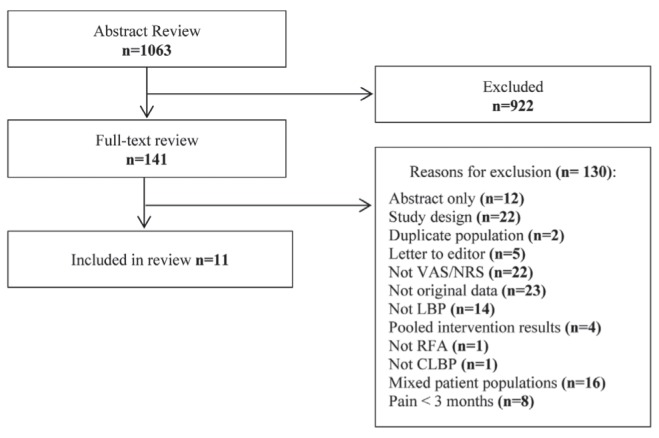
Flow chart of included and excluded studies. CLBP Chronic low back pain (LBP); NRS Numerical rating scale; RFA Radiofrequency ablation; VAS Visual analogue scale
The final 11 studies were allocated into three categories based on location of low back pain: discogenic low back pain (14,17,18); lumbar facet joint pain (16,19,20,22–24); and sacroiliac back pain (15,21) (Table 2). No RCTs addressing the efficacy of RFA for treating pain in the coccyx region were found in the literature.
Table 2.
Characteristics of randomized controlled trials reporting the efficacy of radiofrequency ablation (RFA)
| Author (reference), year; country | Patient selection | Comparators | Outcomes | |
|---|---|---|---|---|
| Discogenic | ||||
| Barendse et al (14), 2001; The Netherlands | Patient selection: Patients were recruited from one teaching hospital between July 1994 and September 1996. Participants were randomly assigned by a computer program to receive the intervention or sham procedure Inclusion criteria: Chronic low back pain for >1 year, nonresponsive to conservative treatment, 30 to 65 years of age, positive response to discography Exclusion criteria: Spinal stenosis, spondylolithesis, multilevel burnt out disc lesions, coagulation disturbances, pregnancy, diabetes mellitus, >1 pain syndrome Patient characteristics: 13 participants (8 women and 5 men) with a mean age of 40.8±7.5 years were randomly assigned to receive the intervention. 15 participants (10 women and 5 men) with a mean age of 45.2±8.4 years were randomly assigned to receive the sham procedure. There were no statistically significant differences in patient characteristics between the sham and intervention groups |
Type of intervention: Continuous conventional RFA, with a 20-gauge cannula and 10 mm tip length, for 90 s using a temperature of 70°C Type of control: Sham procedure with the same placement as intervention, but no current applied |
Outcomes measured: VAS, Oswestry Disability Index, number of analgesic tablets taken, COOP/WONCA quality of life questionnaire, Impairment (Waddell) Outcome ascertainment: Baseline, 2 months Type of analysis: Intention-to-treat |
|
| Kapural et al (17), 2013; United States | Patient selection: Patients were recruited from the authors’ medical practices between September 2007 and October 2011. Participants were randomly assigned using a computer program to receive either the intervention or sham procedure Inclusion criteria: Age ≥18 years, chronic low back pain for >6 months, resistant to conservative treatment, no surgery in the previous 3 months, response to discography, disc height 50% compared with adjacent disc Exclusion criteria: Lumbar surgery, nucleus pulposus herniation, disc bulges >5 mm, free disc fragments, three or more discs degenerated on MRI, structural abnormality, compressive radiculopathy, cervical or thoracic pain, lumbar canal stenosis, chronic sever conditions, immunosuppression, history of coagulopathy, neurological deficits, traumatic spinal fracture, workers compensation, psychological issues, pregnancy, infection, allergies to medication used, body mass index >30 kg/m2 Patient characteristics: 27 participants (15 women and 12 men) with a mean age of 40.4±10.3 years were randomly assigned to receive the intervention. 30 participants (15 women and 15 men) with a mean age of 38.4±10.4 years were randomly assigned to receive the sham procedure. There were no statistically significant differences in patient characteristics between the sham and intervention groups |
Type of intervention: Continuous cooled RFA was used for 150 s in monopolar configuration (60°C) and 15 min in bipolar configuration (45°C to 50°C) Type of control: Sham procedure with the same placement as the intervention, but no current applied |
Outcomes measured: Numerical rating scale, Oswestry Disability Index, health care utilization questionnaire, Short-Form 36 Health Survey Outcome ascertainment: Baseline,1 month, 3 months, 6 months Type of analysis: Not reported |
|
| Kvarstein et al (18), 2009; Norway | Patient selection: Patients were recruited between August 2003 and January 2006 based on referrals. Participants were randomly assigned in 1:1 sex-stratified blocks, using random numbers Inclusion criteria: 20 to 65 years of age, back pain for >6 months, pain >5 on a NRS scale, pain worsened by sitting, no neurological deficits, no history of surgical interventions, no response to conservative treatment, disc degeneration, positive response to diagnostic discography Exclusion criteria: Acute infection, history of drug abuse, psychological disorder that could affect outcome, abnormal neurological examination, radicular pain, spinal deformity, disc herniation >4 mm, pregnancy, allergy to medication used in procedure Patient characteristics: 10 participants (7 women and 3 men) with a mean age of 44.7±10.1 years were randomly assigned to receive the intervention. 10 participants (7 women and 3 men) with a mean age of 39.6±8.9 years were randomly assigned to receive the sham procedure. There were no statistically significant differences in patient characteristics, pain duration or pain medication between the sham and intervention groups |
Type of intervention: Continuous conventional RFA, with a 17-gauge cannula, for 240 s using a temperature of 50°C to 65°C Type of control: Sham procedure with the same placement as the intervention, but no current applied |
Outcomes measured: Brief Pain Inventory, Short Form-36, Oswestry Disability Index, relative change in pain Outcome ascertainment: Baseline, 6 months,12 months Type of analysis: Intention-to-treat and per-protocol |
|
| Lumbar facet | ||||
| Gallagher et al (16), 1994; United Kingdom | Patient selection: Not reported Inclusion criteria: Low back pain for >3 months, positive or neutral response to diagnostic block, 25 to 55 years of age, diagnosis of facet joint pain Exclusion criteria: General ill health, pending compensation claims, mental illness or personality disorder, previous back operation Patient characteristics: 24 participants were randomly assigned to receive the intervention (18 with good response to diagnostic blocks, 6 with poor response to diagnostic blocks), 17 were randomly assigned to receive the sham procedure (12 with good response to diagnostic blocks and 5 with poor response to diagnostic blocks). No patient characteristics were reported |
Type of intervention: Continuous conventional RFA, for 90 s using a temperature of 80°C Type of control: Sham procedure with the same placement as the intervention, but no current applied |
Outcomes measured: VAS and McGill Pain Questionnaire Outcome ascertainment: Baseline, 1 month, 6 months Type of analysis: Not reported |
|
| Leclaire et al (19), 2001; Canada | Patient selection: Patients were recruited from physiatrist referral between October 1993 and December 1996. Participants were randomly assigned in blocks of four Inclusion criteria: 18 to 65 years of age, relief from intra-articular facet injections Exclusion criteria: Allergy to medications used in procedure, blood coagulation disorder, cardiac pace-maker, sciatic pain, low back pain not related to mechanical disorder, previous back surgery Patient characteristics: 36 participants (24 women and 12 men) with a mean age of 46.7±9.3 years were randomly assigned to receive the intervention. 34 participants (21 women and 13 men) with a mean age of 46.4±9.7 years were randomly assigned to receive the sham procedure. There were no statistically significant differences in patient characteristics between the sham and intervention groups |
Type of intervention: Continuous conventional RFA, with a 22-gauge cannula and 5 mm tip length, for 90 s using a temperature of 80°C Type of control: Sham procedure with the same placement as the intervention, but no current applied |
Outcomes measured: Roland-Morris Questionnaire, Oswestry Scale, VAS, spinal mobility and strength, return to work Outcome ascertainment: Baseline, 3 months Type of analysis: Intention-to-treat |
|
| Nath et al (20), 2008; Sweden | Patient selection: Not reported Inclusion criteria: Back pain for >2 years, no response to conservative treatment, positive response to diagnostic block Exclusion criteria: Pregnancy, coagulopathies, malignancy, infection, mental handicap, psychiatric disorder, patients living too far away to complete follow-up Patient characteristics: 20 participants (14 women and 6 men) with a mean age of 56 years were randomly assigned to receive the intervention. 20 participants, 21 women and 13 men with a mean age of 53 years were randomly assigned to receive the sham procedure. There were no statistically significant differences in patient characteristics between the sham and intervention groups. However, the intervention group reported more generalized pain, low back pain, referred pain in the leg and had worse hip movement |
Type of intervention: Continuous conventional RFA, with a 22-gauge cannula and 5 mm tip length, for 60 s using a temperature of 85°C Type of control: Sham procedure with the same placement as the intervention, but no current applied |
Outcomes measured: Global perception of improvement, low back pain, lower limb pain and relief of generalized pain Outcome ascertainment: Baseline, 6 months Type of analysis: Not reported |
|
| Tekin et al (22), 2007; Turkey | Patient selection: Participants were randomly assigned using a random number generator. Inclusion criteria: >17 years of age, symptoms indicative of lumbar facet pain for >6 months, no response to conservative treatment Exclusion criteria: Allergy to medication used in procedure, blood coagulation disorder, language problems, pregnancy Patient characteristics: 20 participants, 9 women and 11 men with a mean age of 60.5±8.5 years, were randomly assigned to receive the continuous intervention. 20 participants (8 women and 12 men) with a mean age of 59.6±7.7 years, were randomly assigned to receive the pulsed intervention. 20 participants, 9 women and 11 men with a mean age of 57.9±9.3 years, were randomly assigned to receive the sham procedure. There were no statistically significant differences in patient characteristics between the sham and intervention groups |
Type of intervention: Pulsed and continuous heated RFA, with a 22-gauge cannula. Pulsed RFA used 2 mm tip length and a temperature of 42°C for 240 s. Continuous RFA used 10 mm tip length and a temperature of 80°C for 90 s Type of control: Sham procedure with the same placement as the intervention, but no current applied |
Outcomes measured: VAS, and Oswestry Disability Index Outcome ascertainment: Baseline, 6 months,12 months Type of analysis: Not reported |
|
| Van Kleef et al (24), 1999; The Netherlands | Patient selection: Patients who had been referred by a medical specialist to a pain management centre due to lack of response to conservative therapies for low back pain were recruited between June 1994 and April 1996 Inclusion criteria: Chronic low back pain, no response to conservative therapy, positive response to diagnostic block Exclusion criteria: Previous back surgery, known cause of back pain, diabetes mellitus, >1 pain syndrome Patient characteristics: 15 participants (10 women and 5 men) with a mean age of 46.6±7.4 years, were randomly assigned to receive the intervention. 16 participants (10 women and 6 men) with a mean age of 41.4±7.5 years were randomly assigned to receive the sham procedure. There were no statistically significant differences in patient characteristics between the sham and intervention groups |
Type of intervention: Continuous conventional RFA, with a 22-gauge cannula and 5 mm tip length, for 60 s using a temperature of 80°C Type of control: Sham procedure with the same placement as the intervention, but no current applied |
Outcomes measured: VAS, global perceived effect, Impairment evaluation (Waddell), Oswestry Disability Index, and the COOP-WONCA quality of life questionnaire Outcome ascertainment: Baseline, 2 months Type of analysis: Not reported |
|
| Van Wijk et al (23), 2005; The Netherlands | Patient selection: Patients were recruited from 4 pain clinics between May 1996 and January 1999 Inclusion criteria: Older than 117, chronic low back pain for >6 months, no radicular syndrome or indication for back surgery Exclusion criteria: Prior RFA treatment, coagulation disturbances, allergies to medications used in procedure, language problems, malignancy, mental handicap, psychiatric condition, pregnancy Patient characteristics: 40 participants (30 women and 10 men) with a mean age of 46.9±11.5 years were randomly assigned to receive the intervention. 41 participants (28 women and 13 men) with a mean age of 48.1±12.6 years were randomly assigned to receive the sham procedure. There were no statistically significant differences in patient characteristics between the sham and intervention groups |
Type of intervention: Continuous conventional RFA, with a 22-gauge cannula and 5 mm tip length, for 60 s using a temperature of 80°C Type of control: Sham procedure with the same placement as the intervention, but no current applied |
Outcomes measured: VAS, daily activities, analgesic intake, global perceived effect, Short Form-36 Health Survey, Zung Self Rating Depression Scale and Multidimensional Pain Inventory Outcome ascertainment: Baseline, 3 months Type of analysis: Not reported |
|
| Sacroiliac | ||||
| Cohen et al (15), 2008; United States | Patient selection: Patients were recruited between May 2005 and August 2006, and randomly assigned in a 1:1 ratio, using blocks of 4 Inclusion criteria: >18 years of age, pain for ≥6 months, no response to conservative treatment, pain relief from sacroiliac joint injections Exclusion criteria: Herniated disc, spondyloarthropathy, untreated coagulopathy, unstable medical or psychological illness Patient characteristics: 14 participants (9 women and 5 men) with a mean age of 51.9±13.6 years were randomly assigned to receive the intervention; 14 participants (8 women and 6 men) with a mean age of 51.8±13.1 years were randomly assigned to receive the sham procedure. There were no statistically significant differences in patient characteristics between the sham and intervention groups, with the exception of military duty status, and baseline Oswestry Disability Index Scores |
Type of intervention: Continuous cooled RFA, with a 17-gauge cannula and 4 mm tip length, for 90 s using a temperature of 80°C Type of control: Sham procedure with the same placement as the intervention, but no current applied |
Outcomes measured: Global perceived effect, NRS, Oswestry Disability Index Outcome ascertainment: Baseline, 1 month, 3 months, 6 months Type of analysis: Not reported |
|
| Patel et al (21), 2012; United States | Patient selection: Patients were recruited by the authors, the authors’ colleagues and using advertisements between July 2008 and July 2010. Participants were randomly assigned in a 2:1 ratio Inclusion criteria: Axial pain below the L5 vertebrae lasting >6 months, 3-day average NRS score rating between 4 and 8, >18 years of age, no response to conservative treatment Exclusion criteria: History of intervertebral disc disease or zygopophyseal joint pain, Beck’s Depression Inventory score >20, psychological barriers to recovery, spinal pathology, infection, cervical or thoracic pain >2/10 on NRS, acute illness, pregnancy, radicular pain, immunosuppression, allergy to medications used, smokers, high narcotics use Patient characteristics: 34 participants (23 women and 11 men) with a mean age of 56±13 years, were randomly assigned to receive the intervention. 17 participants (14 women and 3 men) with a mean age of 64±14 years, were randomly assigned to receive the sham procedure. There were no statistically significant differences in patient characteristics between the sham and intervention groups |
Type of intervention: Continuous cooled RFA, with a 17-gauge cannula and 4 mm tip length, for 150 s using a temperature of 60°C Type of control: Sham procedure with the same placement as the intervention, but no current applied |
Outcomes measured: NRS, Oswestry Disability Index, Short Form-36, bodily pain subscale and Short From-36 physical functioning subscale Outcome ascertainment: Baseline, 3 months, 6 months, 9 months Type of analysis: Not reported |
|
CRF Continuous radiofrequency; MRI Magnetic resonance imaging; NR Not reported; NRS Numerical rating scale; VAS Visual analogue scale
The number of participants in each study ranged from 20 (18) to 81 (23). In the control groups, the mean age ranged from 38.4 years (17) to 64 years (21), and in the intervention groups, the mean age ranged from 40.4 years (17) to 59.6 years (22). Three studies were from the United States (15,17,21), three from the Netherlands (14,23,24), and the remaining were from Norway (18), Canada (19), Sweden (20), United Kingdom (16) and Turkey (22).
Of the included studies, seven used a visual analogue scale to measure reduction in pain (14,16,19,20,22–24), three used a numerical rating scale (15,17,21) and one used the Brief Pain Inventory (18). Studies measured pain outcomes at various times, with all studies measuring a baseline, or zero time point, and some recording outcomes up to one year later (18,22). RFA procedure protocol varied within the included studies, with eight using conventional RFA (14,16,18–20,22–24) and three using cooled RFA (15,17,21). All of the included studies used continuous RFA, with the exception of one study, which assessed the efficacy of both pulsed and continuous RFA (22).
Broadly, the included studies are of moderate to high quality as assessed by the Cochrane Risk of Bias (13) (Table 3). Only two studies were assessed as having a high risk of bias in one of the seven areas; Leclaire et al (19) had ‘high’ risk of bias in selective reporting (19), and Patel et al (21) had ‘high’ risk of bias in blinding of participants (21). All of the included studies used some type of randomization to allocate patients to either the sham or treatment arms. However, some did not report the method of randomization; therefore, it was not possible to assess random sequence generation in these studies. Five of the included studies did not report sufficient information for allocation concealment to be assessed (14,16,20,22,24). Generally, blinding of participants, personnel and outcome assessors was clearly reported and with a low risk of bias. Because it is unknown whether other biases influenced the results of these studies, ‘unclear risk of bias’ was assigned to all under the final category ‘other bias’.
Table 3.
Cochrane Risk of Bias quality assessment
| Random sequence generation | Allocation concealment | Blinding of participants and personnel | Blinding of outcome assessment | Incomplete outcome data | Selective reporting | Other bias | |
|---|---|---|---|---|---|---|---|
| Discogenic | |||||||
|
| |||||||
| Barendse et al (14), 2001; The Netherlands | Low | Unclear | Low | Low | Low | Low | Low |
| Kapural et al (17), 2013; United States | Low | Low | Low | Low | Low | Low | Low |
| Kvarstein et al (18), 2009; Norway | Low | Low | Low | Low | Low | Low | Low |
| Lumbar facet | |||||||
|
| |||||||
| Gallagher et al (16), 1994; United Kingdom | Unclear | Unclear | Unclear | Low | Unclear | Low | Unclear |
| Leclaire et al (19), 2001; Canada | Unclear | Low | Low | Unclear | Low | High | Unclear |
| Nath et al (20), 2008; Sweden | Low | Unclear | Low | Unclear | Unclear | Low | Low |
| Tekin et al (22), 2007; Turkey | Low | Unclear | Low | Low | Low | Low | Low |
| van Kleef et al (24), 1999; The Netherlands | Low | Unclear | Low | Low | Low | Low | Low |
| van Wijk et al (23), 2005; The Netherlands | Low | Low | Low | Low | Low | Low | Low |
| Sacroiliac | |||||||
|
| |||||||
| Cohen et al (15), 2008; United States | Low | Low | Unclear | Low | Low | Low | Low |
| Patel et al (21), 2012; United States | Low | Low | High | Low | Low | Low | Low |
Low, Unclear and High indicate risk of bias
Due to heterogeneity in outcome measures, location of pain and follow-up times, as well as a lack of reported mean differences and standard deviations, meta-analysis was not possible with these data. The results of the included studies are summarized in Table 4. A discussion of the key findings, according to area of pain, follows.
Table 4.
Results of included studies
| Author (reference), year; country | Type of pain outcome measure | Scale of pain outcome measure | Time after RFA | Intervention group pain rating (mean ± SD) | Control group pain rating (mean ± SD) | Findings |
|---|---|---|---|---|---|---|
| Discogenic | ||||||
| Barendse et al (14), 2001; The Netherlands | VAS | 0–10 | Baseline | 6.5±1.3 | 5.5±1.1 | No evidence of statistically significant benefit |
| 2 months | 5.89 | 4.36 | ||||
| Kapural et al (17), 2013; USA | NRS | 0–10 | Baseline | 7.13±1.61 | 7.18±1.98 | A statistically significant reduction in pain was found in the intervention group, compared with the control group six months after treatment (P=0.006) |
| 1 month | 5.31±2.04 | 5.72±2.29 | ||||
| 3 months | 4.94±2.05 | 5.98±2.36 | ||||
| 6 months | 4.94±2.15 | 6.58±2.11 | ||||
| Kvarstein et al (18), 2009; Norway | BPI | 0–10 | Baseline | 4.6±1.8 | 5.5±2 | No evidence of statistically significant benefit |
| 6 months | 3.7±2.2 | 5.3±1.8 | ||||
| 12 months | 3.2±2.3 | 4.9±2.1 | ||||
| Lumbar facet | ||||||
| Gallagher et al (16), 1994; United Kingdom | VAS | 0–100 | Baseline | 58±4.2 | 72±5.6 | For participants who experienced good response to diagnostic blocks: a statistically significant reduction in pain was found in the intervention group, compared with the control group six months after treatment (P<0.05) |
| 1 month | 34±6.9 | 60±9.8 | ||||
| 6 months | 44±7.2 | 70±8.5 | ||||
| Leclaire et al (19), 2001; Canada | VAS | 0–100 | Baseline | 51.9 | 51.5 | No evidence of statistically significant benefit |
| 3 months | 52.3 | 44.4 | ||||
| Nath et al (20), Sweden 2008; | VAS | 0–10 | Baseline | 5.98 | 4.38 | A statistically significant reduction in pain was found in the intervention group, compared with the control group six months after treatment (P=0.004) |
| 6 months | 3.88 | 3.68 | ||||
| Tekin (22), et al 2007; Turkey | VAS | NR | Baseline | PRF: 6.6±1.6 | 6.8±1.6 | A statistically significant reduction in back pain was found when comparing post-procedure are preprocedure scores for PRF (P<0.001), CRF (P<0.001) and control groups (P<0.001) |
| CRF: 6.5±1.5 | ||||||
| 6 months | PRF: 2.9±1.6 | 3.1±0.8 | ||||
| CRF: 2.3±1.3 | ||||||
| 12 months | PRF: 3.5±1.3 | 3.9±1.2 | ||||
| CRF: 2.4±1.1 | ||||||
| Van Kleef et al (24), 1999; The Netherlands | VAS | 0–10 | Baseline | 5.2±1.7 | 5.2±1.6 | A statistically significant reduction in pain was found in the intervention group, compared with the control group two months after treatment (P<0.005) |
| 2 months | 2.83±2.24 | 4.77±2.5 | ||||
| Van Wijk et al (23), 2005; The Netherlands | VAS | 0–10 | Baseline | 5.8±1.8 | 6.5±1.8 | A statistically significant reduction in back pain was found for both those treated with RFA (P=0.001) and in those who received sham (P=0.0003) |
| 3 months | 3.7 | 3.7 | ||||
| Sacroiliac | ||||||
| Cohen et al (15), 2008; United States | NRS | 0–10 | Baseline | 6.1±1.8 | 6.5±1.9 | Statistically significant reduction in pain was found in the treatment group, compared with the control group (at one month, P<0.001) |
| 1 month | 2.4±2 | 6.3±2.4 | ||||
| 3 months | 2.4±2.3 | 6±0 | ||||
| 6 months | 2.6±2.2 | NR | ||||
| Patel et al (21), 2012; United States | NRS | 0–10 | Baseline | 6.1±1.3 | 5.8±1.3 | Statistically significant reduction in pain was found in the treatment group, compared with the control group three months post-treatment |
| 1 month | 3.4 | 4.1 | ||||
| 3 months | NR | NR | ||||
| 6 months | NR | NR | ||||
| 9 months | NR | NR |
BPI Brief Pain Inventory; CRF Conventional radiofrequency NR Not reported; NRS Numerical rating scale; PRF Pulsed radiofrequency; RFA Radiofrequency ablation; VAS Visual analogue scale
Discogenic back pain
Three studies assessed the use of RFA for treating discogenic back pain using a variety of methods. Two of the included studies used conventional RFA (14,18) and one used cooled RFA (17). The study using cooled RFA, used a bipolar configuration which was then followed by the standard monopolar configuration (17).
All three studies used diagnostic discography to confirm diagnosis of discogenic low back pain, and only participants with a positive response to this procedure were included in the studies.
Studies used RFA at a temperature between 50°C and 70°C to create the lesion. The three studies reported that the characteristics of patients were not significantly different between the control and intervention groups, with the exception of Barendse et al (14), who reported that those in the intervention group had higher pain and had a longer duration of pain than the control group. Although all three studies used different outcome measures to assess change in pain, all used a 0 to 10 scale.
The two studies, Barendse et al (14) and Kvarstein et al (18), that assessed the efficacy of conventional RFA found no evidence of statistically significant benefit when the intervention group was compared with the control group. A study conducted by Kapural et al (17), which assessed the efficacy of cooled RFA, found evidence of a statistically significant benefit. This study reported a 2.19-point reduction in pain within the intervention group and a 0.6-point reduction in pain in the control group six months postprocedure (P=0.006) (17).
Lumbar facet joint pain
Six studies included in the present systematic review assessed the efficacy of RFA in reducing chronic lumbar facet back pain (16,19,20,22–24). Five studies used continuous RFA (16,19,20,23,24), and one used a combination of pulsed and continuous RFA (22). All six included studies used conventional RFA, and used diagnostic blocks to confirm diagnosis of lumbar facet joint pain (16,19,20,22–24). Five of the six studies used 22-gauge cannulas (19,20,22–24), and one study did not report these data (16). All six studies assessed pain reduction using a visual analogue scale; three used a 0 to 10 scale (20,23,24), two used a 0 to 100 scale (16,19) and one study did not report the scale used (22). Five studies reported that there were no statistically significant differences in patient characteristics between the intervention and control groups at baseline (16,19,22–24). Nath et al (20) reported that those who received RFA had more general pain, low back pain and referred pain than those in the control group.
Results from the included studies were mixed as to the efficacy of RFA. Five of the included studies found evidence of statistically significant reductions in pain when comparing RFA with sham (16,20,22–24). One of these studies found a significant effect only in participants who experienced a positive response to diagnostic block (P<0.05); for participants who experienced equivocal response to diagnostic blocks, statistically significant benefit was not found (16). One of the six included studies did not find any evidence of statistically significant improvement; this study found a 0.5 point reduction in pain within the intervention group and a 0.6 point reduction in pain in the control group (19).
Sacroiliac joint pain
Two studies assessed the efficacy of RFA for treating sacroiliac pain (15,21). Both used continuous, cooled RFA procedures (15,21). These studies used a 17-gauge cannula and a 4 mm tip length. Cohen et al (15) heated the device to 80°C for 90 s, while Patel et al (21) used 60°C heat for 150 s. Both studies used a numerical rating scale, with a range of 0 to 10 to assess change in pain. Cohen et al (15) followed participants for six months. Patel et al (21) followed participants for nine months postprocedure, but only presented data for the control group up to three months. Both of these studies reported that there were no statistically significant differences in patient characteristics at baseline between the intervention and controls groups.
These two studies assessing the efficacy of RFA for treating sacroiliac joint pain studies found statistically significant reduction in pain for the intervention group, when compared with the control group (15,21). Three months postprocedure, Cohen et al (15) found a 3.7-point reduction in pain within the intervention group, while the control group experienced only a 0.5-point reduction in pain. Three months postprocedure, Patel et al (21) found a 2.4-point pain reduction in the intervention group, and a 0.8-point pain reduction in the control group.
DISCUSSION
Eleven sham-controlled RCTs were found, assessing the efficacy of RFA for discogenic back pain (14,17,18), lumbar facet joint pain (16,19,20,22–24) and sacroiliac joint pain (15,21). There were no RCTs investigating the use of RFA for pain in the coccyx region found in the literature.
The efficacy of RFA for discogenic back pain remains unclear. Of the three included studies, two studies assessed conventional RFA and found no statistically significant benefit over sham at two (14) and 12 months (18), while one study assessed cooled RFA and did find a statistically significant benefit compared with sham (17). The contradicting results may be attributable to the procedural differences between these three studies. However, the clinical relevance of these findings is unclear.
Five of the six studies assessing RFA for treating lumbar facet joint pain found statistically significant results (16,20,22–24), and one found no evidence of statistically significant benefit (19). The methods used in these studies were similar, with all using continuous, conventional RFA and diagnostic blocks to confirm diagnosis. This number of similar, high-quality sham-controlled RCTs on lumbar facet joints provides a robust evidence base that suggests that continuous, conventional RFA is efficacious in reducing lumbar facet joint pain. However, the longest follow-up time point within these studies was one year (22), with the majority of the studies only following patients for two (24), three (19,23) or six months (16,20). The long-term pain relief associated with RFA is unclear. In addition, the clinical relevance of the pain relief achieved is unknown. The studies reporting improvement reported modest reductions in pain scores with no predefined clinically relevant pain reduction reported. A large high-quality RCT in this patient population measuring predefined clinically meaningful pain reduction following patients for at least one year is now required to understand the efficacy of RFA for treating lumbar facet joint low back pain.
Both of the RCTs assessing the efficacy of RFA for treating sacroiliac joint pain found statistically significant reductions in pain for the treatment group compared with the control group (15,21). The procedures used in these two studies were similar in that they both used continuous, cooled RFA (15,21). These two studies suggest that continuous cooled RFA is efficacious in reducing sacroiliac joint pain; however, with only two available RCTs, more data on the efficacy of RFA for sacroiliac joint pain would strengthen this conclusion. In addition, as with the lumbar facet joint literature, the clinical significance of the modest pain reduction is unclear.
The lack of literature on the efficacy of RFA to treat the coccyx is surprising because this topic has been studied using non-RCT study designs (25). A sham-controlled RCT on the efficacy of RFA for the treatment of pain in the coccyx area would be a positive addition to the literature and could impact clinical practice.
The present systematic review had several limitations that merit comment, including limitations of the literature, inability to conduct a meta-analysis and using statistical significance as a surrogate for clinical significance.
As with all systematic reviews, the key limitation of the present review was that it reflects the literature and data available on this subject. In this case, the literature on sacroiliac joint pain was limited, the literature on discogenic pain used heterogeneous RFA methods and no literature was found on coccyx pain. This incomplete literature base limits the conclusions that can be drawn in the present systematic review.
Of the included studies, very few reported mean differences and SDs of these mean differences. Therefore, quantitative pooling through meta-analysis was not possible; the present study was limited to narrative synthesis. Future work should be encouraged to report data such that pooling is possible, thus enabling conclusions based on the entire body of work assessing RFA for low back pain.
In the present review, pain was the primary outcome assessed. This outcome was used because it was frequently reported and gave a broad sense of improvement or worsening. Many of the included studies only reported statistically significant differences as opposed to predefined clinical improvement. However, in clinical practice, the end goal is for the patient to experience pain relief such that they can return to their daily tasks; a level of pain relief that may differ from the level of pain reduction required to achieve statistical significance. However, these clinically relevant outcomes were not reported in any of the studies identified.
The evidence supports RFA as an efficacious treatment for lumbar facet joint and sacroiliac joint pain with five of six and both of the RCTs demonstrating statistically significant pain reductions, respectively. The evidence supporting RFA for treatment for discogenic pain is mixed and no RCT evidence exists for treatment of the coccyx. However, all the RCT data are short-term (<1 year) and do not report clinically meaningful pain reduction or outcomes such as ability to complete daily tasks or return to work. Further evidence should be generated before RFA is widely integrated into evidence-based clinical guidelines.
OTHER ACKNOWLEDGEMENTS:
This work was supported by a grant from Alberta Health. The research herein does not reflect their views or opinions.
Footnotes
FUNDING/SUPPORT: None.
CONTRIBUTIONS OF AUTHORS: Design of the study (LL, DLL, RS, TN, FC); collection of data (LL, LS, DLL); management of data (LL, LS, FC), analysis of data (LL,LS, FC); interpretation of the data (LL, LS, FC); preparation of manuscript (LL, LS, DLL, TN, RS, ST, FC); review of manuscript (LL, LS, DLL, TN, RS, ST, FC); approval of manuscript (LL, LS, DLL, TN, RS, ST, FC).
DISCLOSURES: The authors have no financial disclosures or conflicts of interest to declare.
REFERENCES
- 1.World Health Organization WHO Technical Report Series: The Burden of Musculoskeletal Conditions at the Start of the New Millenium. World Health Organization. 2003 < http://whqlibdoc.who.int/trs/WHO_TRS_919.pdf> (Accessed September 1, 2013) [PubMed] [Google Scholar]
- 2.World Health Organization Chronic Diseases and Health Promotion. World Health Organization. 2013. < www.who.int/chp/topics/rheumatic/en/> (Accessed September 1, 2013)
- 3.Lawrence R, Felson D, Helmick C, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States: Part II. Arthritis Rheum. 2008;58:26–35. doi: 10.1002/art.23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Katz JN. Lumbar disc disorders and low-back pain: Socioeconomic factors and consequences. J Bone Joint Surg Am. 2006;88(Suppl 2):21–4. doi: 10.2106/JBJS.E.01273. [DOI] [PubMed] [Google Scholar]
- 5.Andersson GB. Epidemiological features of chronic low-back pain. Lancet. 1999 Aug 14;354:581–5. doi: 10.1016/S0140-6736(99)01312-4. [DOI] [PubMed] [Google Scholar]
- 6.Office of Communication and Public Liaison. Low Back Pain Fact Sheet. National Institute of Neurological Disorders and Stroke. 2013. < www.ninds.nih.gov/disorders/backpain/detail_backpain.htm>.
- 7.Steenstra IA, Verbeek JH, Heymans MW, et al. Prognostic factors for duration of sick leave in patients sick listed with acute low back pain: A systematic review of the literature. Occup Environ Med. 2005;62:851–60. doi: 10.1136/oem.2004.015842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Haldeman S, Dagenais S. A supermarket approach to the evidence-informed management of chronic low back pain. Spine J. 2008;8:1–7. doi: 10.1016/j.spinee.2007.10.009. [DOI] [PubMed] [Google Scholar]
- 9.Savigny P, Watson P, Underwood M. Early management of persistent non-specific low back pain: Summary of NICE guidance. BMJ. 2009;338:61805. doi: 10.1136/bmj.b1805. [DOI] [PubMed] [Google Scholar]
- 10.Van Tulder MW, Koes BW, Bouter LM. Conservative treatment of acute and chronic nonspecific low back pain: A systematic review of randomized controlled trials of the most common interventions. Spine. 1997;22:2128–56. doi: 10.1097/00007632-199709150-00012. [DOI] [PubMed] [Google Scholar]
- 11.Towards Optimized Practice Program. Guideline for the Evidence-Informed Primary Care Management of Low Back Pain. Toward Optimized Practice Program. 2011 < http://nationalpaincentre.mcmaster.ca/documents/LowerBackPainGuidelineNov2011.pdf> (Accessed September 1, 2013) [Google Scholar]
- 12.Shealy CN. Percutaneous radiofrequency denervation of spinal facets: Treatment for chronic back pain and sciatica. J Neurosurg. 1975;43:448–51. doi: 10.3171/jns.1975.43.4.0448. [DOI] [PubMed] [Google Scholar]
- 13.Higgins J, Altman D, Gotzsche P, et al. The Cochrane Collaborations tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Barendse GA, van Den Berg SG, Kessels AH, et al. Randomized controlled trial of percutaneous intradiscal radiofrequency thermocoagulation for chronic discogenic back pain: Lack of effect from a 90-second 70 C lesion. Spine. 2001;26:287–92. doi: 10.1097/00007632-200102010-00014. [DOI] [PubMed] [Google Scholar]
- 15.Cohen SP, Hurley RW, Buckenmaier CC, et al. Randomized placebo-controlled study evaluating lateral branch radiofrequency denervation for sacroiliac joint pain. Anesthesiology. 2008;109:279–88. doi: 10.1097/ALN.0b013e31817f4c7c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gallagher J, Petriccione DVPL, Wedley JR, et al. Radiofrequency facet joint denervation in the treatment of low back pain: A prospective controlled double-blind study to assess its efficacy. Pain Clin. 1994;7:193–8. [Google Scholar]
- 17.Kapural L, Vrooman B, Sarwar S, et al. A randomized, placebo-controlled trial of transdiscal radiofrequency, biacuplasty for treatment of discogenic lower back pain. Pain Med. 2013;14:362–73. doi: 10.1111/pme.12023. [DOI] [PubMed] [Google Scholar]
- 18.Kvarstein G, Mawe L, Indahl A, et al. A randomized double-blind controlled trial of intra-annular radiofrequency thermal disc therapy – a 12-month follow-up. Pain. 2009;145:279–86. doi: 10.1016/j.pain.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 19.Leclaire R, Fortin L, Lambert R, et al. Radiofrequency facet joint denervation in the treatment of low back pain: A placebo-controlled clinical trial to assess efficacy. Spine. 2001;26:1411–6. doi: 10.1097/00007632-200107010-00003. [DOI] [PubMed] [Google Scholar]
- 20.Nath S, Nath CA, Pettersson K. Percutaneous lumbar zygapophysial (Facet) joint neurotomy using radiofrequency current, in the management of chronic low back pain: A randomized double-blind trial. Spine. 2008;33:1291–7. doi: 10.1097/BRS.0b013e31817329f0. [DOI] [PubMed] [Google Scholar]
- 21.Patel N, Gross A, Brown L, et al. A randomized, placebo-controlled study to assess the efficacy of lateral branch neurotomy for chronic sacroiliac joint pain. Pain Med. 2012;13:383–98. doi: 10.1111/j.1526-4637.2012.01328.x. [DOI] [PubMed] [Google Scholar]
- 22.Tekin I, Mirzai H, Ok G, et al. A comparison of conventional and pulsed radiofrequency denervation in the treatment of chronic facet joint pain. Clin J Pain. 2007;23:524–9. doi: 10.1097/AJP.0b013e318074c99c. [DOI] [PubMed] [Google Scholar]
- 23.van Wijk R, Geurts JWM, Wynne HJ, et al. Radiofrequency denervation of lumbar facet joints in the treatment of chronic low back pain: A randomized, double-blind, sham lesion-controlled trial. Clin J Pain. 2005;21:335–44. doi: 10.1097/01.ajp.0000120792.69705.c9. [DOI] [PubMed] [Google Scholar]
- 24.van Kleef M, Barendse GA, Kessels A, et al. Randomized trial of radiofrequency lumbar facet denervation for chronic low back pain. Spine. 1999;24:1937–42. doi: 10.1097/00007632-199909150-00013. [DOI] [PubMed] [Google Scholar]
- 25.Reig E, Abejon D, Del Pozo C, et al. Thermocoagulation of the ganglion impar or ganglion of Walther: Description of a modified approach. Preliminary results in chronic, nononcological pain. Pain Pract. 2005;5:103–10. doi: 10.1111/j.1533-2500.2005.05206.x. [DOI] [PubMed] [Google Scholar]


